Abstract
Purpose
At present, the indications for femoral derotational osteotomy remain controversial due to the inconsistent findings in femoral neck anteversion in developmental dysplasia of the hip (DDH). Moreover, combined anteversion is not assessed in unilateral DDH using three dimensional-CT. Therefore, the purposes of our study were to observe whether the femoral neck anteversion (FA), acetabular anteversion (AA) and combined anteversion (CA) on the dislocated hips were universally presented in unilateral DDH according to the classification system of Tönnis.
Methods
Sixty-two patients with unilateral dislocation of hip were involved in the study, including 54 females and eight males with a mean age of 21.63 months (range, 18–48 months). The FA, AA and CA were measured and compared between the dislocated hips and the unaffected hips.
Results
Although no significant difference was observed in FA between the dislocated hips and the unaffected hips (P = 0.067, 0.132, respectively) in Tönnis II and III type, FA was obviously increased on the dislocated hips compared with the unaffected hips in Tönnis IV type. Increased AA on the dislocated hips was a universal finding in Tönnis II, III and IV types. Meanwhile, a wide safe range of CA from 24° to 62° was demonstrated on the unaffected hips.
Conclusion
Femoral derotational osteotomy seems not to be necessary in Tönnis II and III types in unilateral DDH. Femoral derotational osteotomy should be considered in DDH, especially in Tönnis IV type, if the CA is still above 62° and the hip joints present instability in operation after abnormal acetabular anteversion, acetabular index and acetabular coverage of the femoral head are recovered to normal range through pelvic osteotomy.
Introduction
Developmental dysplasia of the hip (DDH) is one of the most complex three-dimensional (3D) deformities, and is a leading cause of premature arthritis requiring total hip replacement [1]. The choice of the type of surgical procedure for surgeons in DDH mainly depends on the understanding of the morphologic insufficiencies of acetabulum and femur. Increased acetabular anteversion or femoral anteversion is related to hip instability [2, 3], and acetabular retroversion is associated with hip pain and osteoarthrosis of the hip [4, 5]. Bicanic et al. [6] observed that for every millimeter of lateral displacement of the acetabular cup, an increase of 0.7% in hip load should be expected during total hip arthroplasty. Therefore, exactly evaluating the anteversion of acetabulum and femur could be quite crucial before surgical decision-making for children with DDH to avoid complications. Several investigators have reported that anteversion of the acetabulum is significantly increased on the side involved in DDH [7–9], whereas others have failed to confirm those findings [10–13]. In the past, the widely held belief was that there was increased femoral anteversion on the involved side in DDH; and so femoral derotational osteotomy was believed to be required. However, several recent studies did not show any significant difference in femoral anteversion between the affected hips and unaffected hips [8, 14–16]. These authors thought femoral derotational osteotomy may not be necessary in DDH. Thus, at present, the indications for femoral derotational osteotomy remain controversial.
Combined anteversion (CA) or the ‘instability index’ of the hip means the sum of the anteversion of the acetabulum and the femur (CA = FNA + AA). McKibbin [17] employed, for the first time, the term in a study of infant cadavers for DDH and defined the normal instability index for anatomic hips. At present, the CA has been generally used in total hip arthroplasty (THA) [18, 19]. Komeno et al. thought that the dislocation rate after THA was not affected by the positioning of either the cup or the stem alone but was influenced by the CA [18]. However, currently, the CA is not analysed in the subgroup of unilateral DDH according to the classification system of Tönnis [20]. Moreover, the CA also is not considered as an index to assess whether femoral derotational osteotomy should be performed.
Although it is widely considered that two dimensional-CT scanning is an accurate method for the quantitative assessment on the anteversion of femoral neck and of acetabulum in children with DDH, its reliability and accuracy are limited by anatomical and positional variables [21, 22]. Previously, we have reported that the three dimensional-CT showed better intra- and inter-observer agreement than two dimensional-CT for assessing acetabular anteversion in DDH [9]. Therefore, in the present study, we employed three dimensional-CT assessing the femoral neck anteversion, acetabular anteversion and combined anteversion in DDH. Because wide-age range patient groups have been considered as underlying reasons for the inconsistent finding in acetabular and femoral anteversion [8, 11], the patients with unilateral DDH in an early walking age group (18–48 months) were involved in the present study to compare these data published in recent years.
The purpose of our study was to observe whether the femoral neck anteversion, acetabular anteversion and combined anteversion on the dislocated hips were universally presented in unilateral DDH using three dimensional-CT.
Patients and methods
Patients
We retrospectively reviewed the medical records, plain anteroposterior pelvic radiographs and CT images of 485 patients with a primary diagnosis of unilateral DDH treated at our institution between 2005 and 2010. Since non-operative or operative treatment can alter the acetabular anatomy, patients with a history of prior treatment were excluded. Thus, 62 patients (124 hips) with unilateral DDH were involved in the study, including 54 females and eight males with a mean age 21.63 months (range, 18–48 months). The left hip was involved in 35 cases, the right hip in 27 cases. According to the classification system of Tönnis based on the level of dislocation of the femoral head [20], by using plain anteroposterior pelvic radiographs, 11 hips were classified as grade II, 37 hips as grade III and 14 hips as grade IV, but the patients with subluxation of hip were not involved in the study. This research had been approved by the Medical Ethics Committee of Shengjing Hospital, China Medical University.
Scanning procedures and measurements
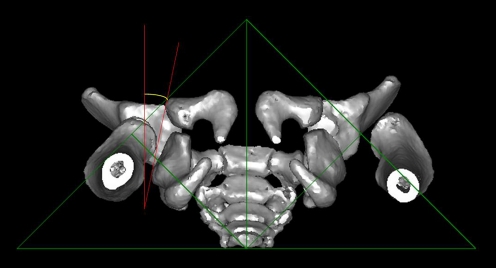
The three dimensional-CT scans were performed using a Philips Brilliance 64 scanner (Marconi Medical Systems, Netherlands). The scanning technique used was 120 kV, 70–120 mA (depending on the patient’s size), with a 0.5-s rotation time. Contiguous slices (1.5 mm) were obtained from the upper rim of the acetabulum to the lesser trochanter. Another scan went through the distal femur which included bilateral inner and outer condyles of the femur. The patients were placed in a supine position with hips extended and thighs horizontal and parallel. The images were retrospectively reconstructed at a CT workstation (Extended Brilliance™ Workspace V3.5.0.2250) to produce the three dimensional images. Once the data were acquired, the images could be observed and measured from any angle. After proximal and distal femur were reconstructed, the three dimensional image of proximal femur and the three dimensional image of medial and lateral condle of femur were overlapped on an image (Fig. 1). The lowest point of the medial and lateral condle and the lowest point of the greater trochanter located in the middle between medial and lateral condle were connected by a horizontal line (red line, Fig. 2). The femoral neck anteversion (FA) was the angle formed by the horizontal line (red line) and the tangential line (red line) connecting the point of centricity of the femoral head with the midpoint of the narrowest femoral neck (Fig. 2). If the epiphysis of the femoral head was extremely small or disappeared or decentered, the axial line of the femoral neck was considered as the tangential line. The acetabular anteversion was measured on the inferior view of the three-dimensional computed tomography reconstruction of the pelvis. Acetabular anteversion angle (AA) was the angle formed by a line connecting the anterior and posterior margins of the acetabulum (red line) and the sagittal line (red line, Fig. 3). Acetabular index (AI) and centre–edge angle of every patient on the unaffected hips were measured to evaluate whether the unaffected hips were normal.
Fig. 1.

Reconstructed three dimensional image of the proximal femur and distal femur
Fig. 2.
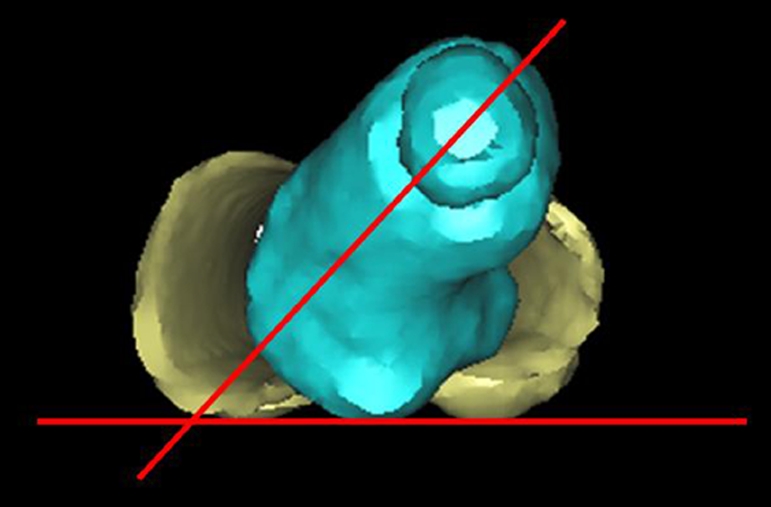
The femoral neck anteversion (FA) was the angle formed by the horizontal line (red line) and the tangential line (red line) connecting the point of centricity of the femoral head with the midpoint of the narrowest femoral neck
Fig. 3.
Acetabular anteversion angle (AA) was the angle formed by a line connecting the anterior and posterior margins of the acetabulum (red line) and the sagittal line (red line). The triangle ruler was regarded as the marker to prevent the pelvic obliquity
To determine intra-observer variation, the measurement was repeated two weeks later by one of the paediatric orthopaedic surgeons (observer A). For evaluation of inter-observer variation, we randomly selected 36 patients with 72 hips and the measurements were taken by three experts, including two paediatric orthopaedic surgeons (observers A and B) and one radiologist (observe C).
Statistical analysis
Statistical analysis was performed using SPSS version 11.5 (SPSS Inc, Chicago, IL, USA) for Windows. The paired sample t-test was used to assess the difference in the AA, FA, CA and AI between the dislocated hips and the unaffected hips in unilateral DDH. The correlation of AA with FA was assessed using Pearson correlation analysis. We considered p < 0.05 to be significant.
Intra-observer agreements between the two sets of measurements of observer A and inter-observer agreements between the three sets of measurements of observers A, B and C were analysed using Pearson correlation coefficient and the intra-class correlation coefficient (ICC). An ICC > 0.75 was regarded as excellent, ICC 0.40–0.75 was fair to good, and ICC < 0.40 was poor.
Results
The average AA, FA, CA and AI (acetabular index) between the dislocated hips and the unaffected hips in unilateral DDH were shown in Table 1. Significant differences in AA, CA and AI were detected between the dislocated hips and the unaffected hips. No significant difference was observed in FA between the two sides (Table 1). However, after the 62 patients of unilateral dislocation of hip were divided into three subgroups according to the classification system of Tönnis, the result indicated the FA was obviously increased on the dislocated hips (35.97 ± 10.24°) compared with the unaffected hips (30.46 ± 7.51°) in the grade IV group (P = 0.028), but significant difference in FA was not shown in the grades II and III (Table 2). In the groups of grades II, III and IV, the AA and AI were larger on the dislocated hips than on the unaffected hips (Tables 3 and 4). Although the CA was increased on the dislocated hips compared with the unaffected hips in the group of grade III and IV, it did not differ between the two sides in the group of grade II (Table 5). The correlation was not shown between FA and AA in DDH (r = −0.028, P = 0.828 on the dislocated hips and r = −0.129, P = 0.316 on the unaffected hips).
Table 1.
The average AA, FA, CA and AI were shown between the dislocated hips and the unaffected hips in unilateral DDH
| Measurement | Dislocated hips | Unaffected hips | P-value | ||
|---|---|---|---|---|---|
| Mean±SD | Range | Mean±SD | Range | ||
| AA | 17.72 ± 3.35° | (12–26°) | 12.54 ± 2.93° | (5–18°) | 0.001 |
| FA | 34.66 ± 7.77° | (19–57°) | 32.60 ± 8.15° | (16–48°) | 0.071 |
| CA | 52.37 ± 8.37° | (36–83°) | 45.14 ± 9.01° | (24–62°) | 0.001 |
| AI | 33.21 ± 4.70° | (22–45°) | 21.47 ± 3.60° | (14–28°) | 0.001 |
AA acetabular anteversion, FA femoral neck anteversion, CA combined anteversion, AI acetabular index, DDH developmental dysplasia of the hip, SD standard deviation
Table 2.
Compared the FA between the dislocated hips and unaffected hips in the group of grade II, III and IV according to the classification of Tönnis
| Tönnis grade | Dislocated hips | Unaffected hips | P-value | ||
|---|---|---|---|---|---|
| Mean±SD | Range | Mean±SD | Range | ||
| II | 32.53 ± 6.86° | (23–42°) | 35.81 ± 8.24° | (23–48°) | 0.067 |
| III | 34.79 ± 7.02° | (19–51°) | 32.45 ± 8.27° | (15–48°) | 0.132 |
| IV | 35.97 ± 10.24° | (26–57°) | 30.46 ± 7.51° | (17–43°) | 0.028 |
FA femoral neck anteversion, SD standard deviation
Table 3.
Compared the AA between the dislocated hips and unaffected hips in the group of grade II, III and IV according to the classification of Tönnis
| Tönnis grade | Dislocated hips | Unaffected hips | P-value | ||
|---|---|---|---|---|---|
| Mean±SD | Range | Mean±SD | Range | ||
| II | 16.57 ± 3.08° | (12–22°) | 12.65 ± 2.83° | (9–18°) | 0.008 |
| III | 17.94 ± 3.20° | (13–23°) | 12.61 ± 3.38° | (5–18°) | 0.001 |
| IV | 18.03 ± 3.96° | (12–26°) | 12.26 ± 1.55° | (10–15°) | 0.001 |
AA acetabular anteversion, SD standard deviation
Table 4.
Compared the AI between the dislocated hips and unaffected hips in the group of grade II, III and IV according to the classification of Tönnis
| Tönnis grade | Dislocated hips | Unaffected hips | P-value | ||
|---|---|---|---|---|---|
| Mean±SD | Range | Mean±SD | Range | ||
| II | 33.36 ± 3.70° | (29–41°) | 22.21 ± 1.70° | (19–25°) | 0.001 |
| III | 32.79 ± 5.17° | (22–45°) | 21.22 ± 4.28° | (14–28°) | 0.001 |
| IV | 34.21 ± 4.15° | (28–42°) | 21.54 ± 2.64° | (16–25°) | 0.001 |
AI acetabular index, SD standard deviation
Table 5.
Compared the CA between the dislocated hips and unaffected hips in the group of grade II, III and IV according to the classification of Tönnis
| Tönnis grade | Dislocated hips | Unaffected hips | P-value | ||
|---|---|---|---|---|---|
| Mean±SD | Range | Mean±SD | Range | ||
| II | 49.10 ± 6.56° | (40–59°) | 48.47 ± 8.88° | (32–62°) | 0.734 |
| III | 52.73 ± 7.59° | (36–67°) | 45.06 ± 9.57° | (24–62°) | 0.001 |
| IV | 54.01 ± 11.14° | (39–83°) | 42.72 ± 7.14° | (33–57°) | 0.001 |
CA combined anteversion, SD standard deviation
The three dimensional-CT-based measurement of AA and FA revealed excellent intra-observer agreement and inter-observer agreement across the three observers (Table 6).
Table 6.
Comparison of intra-observer and inter-observer agreement in the measurement of three dimensional acetabular angle (AA) and femoral anteversion (FA) as calculated by the intra-class correlation coefficient (ICC)
| Observer | AA | FA | ||
|---|---|---|---|---|
| ICC | P-value | ICC | P-value | |
| A-A | 0.934 | 0.000 | 0.947 | 0.000 |
| A-B | 0.864 | 0.000 | 0.815 | 0.000 |
| A-C | 0.805 | 0.000 | 0.881 | 0.000 |
| B-C | 0.895 | 0.000 | 0.826 | 0.000 |
Discussion
In the present study, the reliability of three dimensional-CT in measuring acetabular anteversion was further confirmed. Meanwhile, similar results were also observed in measuring femoral anteversion. Our data indicated that excessive anteversion of the acetabulum was universally presented on the dislocated hips in grades II, III and IV in unilateral DDH.
At present, the indications for femoral derotational osteotomy in DDH remain controversial due to the inconsistent findings in femoral neck anteversion (FA) [3, 8, 14–16, 23–25]. It has generally been accepted that DDH is associated with increased FA in the past. However, recently, several researches did not observe any significant difference in FA between the affected hips and the unaffected hips in early walking-age patients with DDH using two dimensional-CT and MRI [8, 14–16]. Thus, these authors thought femoral derotational osteotomy is not necessary in DDH. Sezgin et al. [8] compared the difference of FA between 44 affected hips and ten unaffected hips in DDH using two-dimensional computed tomography. They found an FA of 32.9° ± 6.4° in the affected group and 30.7° ± 6.1° in the unaffected group. The difference was insignificant (P = 0.378). Similar results were observed in our study. The average FA on the 62 dislocated hips and 62 unaffected hips were, respectively, 34.66 ± 7.77°and 32.60 ± 8.15°, and no significant difference was found between the two sides (P = 0.071). However, in the present research, it is notable that after the 62 patients of unilateral dislocation of hip were divided into three subgroups according to classification system of Tönnis, we found the FA was obviously increased on the dislocated hips compared with the unaffected hips in the grade IV group (P = 0.028); although a significant difference in FA was not shown in grades II and III (P = 0.067 and 0.132, respectively). To date, this finding was not reported in the published literature.
Combined anteversion (CA) or the ‘instability index’ of the hip means the sum of the anteversion of the acetabulum and the femur (CA = FNA + AA). In 1970, McKibbin [17] employed, for the first time, the term in a study of infant cadavers for DDH. The CA of 45° was presented in infant cadavers of DDH. The average instability index for normal anatomic hips was 35.25° (range, 20–58°). The CA in DDH was less than that from some completely stable hips. Therefore, they thought the dislocation could not be blamed on this alone. We totally agree with their views because, in addition to the CA, insufficient acetabular coverage of the femoral head (such as decreased centre–edge angle) and increased acetabular index were also closely associated with the dislocation of hip. Thus, only when the two indexes are completely normal, the CA could be viewed as a meaning index to assess the stability of hip joint. In the present study, we observed the CA was increased on the dislocated hips compared with the unaffected hips in unilateral DDH. However, after the 62 patients of unilateral dislocation of hip were divided into three subgroups according to the classification system of Tönnis, no significant difference in CA between the dislocated hips and unaffected hips was observed in the grade II group. Though no significant difference was found in CA in the group of grade II, the patients presented unilateral dislocation of hip. This suggests that in addition to normal acetabular index and acetabular coverage of the femoral head, normal angle of acetabular anteversion is also quite crucial to keep the stability of hip joint because acetabular anteversion is obviously increased on the dislocated hips compared with the unaffected hips. Significant difference in CA was observed between the dislocated hips and unaffected hips in grade III and IV groups. In the grade III group, increased CA on the dislocated hips was mainly induced by excessive acetabular anteversion because no significant difference in femoral anteversion was found between the dislocated hips and the unaffected hips. In the grade IV group, the increased CA could be induced by excessive acetabular and femoral anteversion because the two indexes were larger on the dislocated hips than on the unaffected hips.
In our study, a wide safe range of CA from 24° to 62° was demonstrated on the unaffected hips. Thus, we recommend that femoral derotational osteotomy should be considered in DDH in the early walking age (18–48 months), especially in the grade IV group, if the CA still is above 62° and the hip joint presents instability in operation after abnormal acetabular anteversion, acetabular index and acetabular coverage of the femoral head were recovered to normal range through pelvic osteotomy. For example, if abnormal acetabular index and acetabular coverage of the femoral head are recovered to the normal range through pelvic osteotomy and acetabular anteversion is 12°, femoral derotational osteotomy may not be necessary when femoral anteversion is less than 50° (62°CA − 12°AA = 50°FA). If acetabular anteversion is 8°, femoral derotational osteotomy may not be necessary when femoral anteversion is less than 54° (62°CA − 8°AA = 54°FA). Berkeley et al. [23] advised performing a concomitant femoral derotational osteotomy if anteversion exceeded 60°. Sankar et al. [3] generally performed a derotational osteotomy for anteversion that exceeded 50°, with the final goal being 20–30° of femoral anteversion. Because Wenger et al. [24] found that femoral anteversion was often increased to 40–60°, they usually derotated 30° to avoid posterior hip dislocation. Zadeh et al. [25] described a “test of stability” to determine when to do derotational osteotomy, which is based on intraoperative analysis. Herein, the authors speculated that the CA and “test of stability” working together may be a more meaningful index to evaluate whether femoral derotational osteotomy should be performed in DDH. Of course, this needs be further confirmed in future research.
Conclusion
In the present study, the results of this study indicated that increased acetabular anteversion on the dislocated hips was a universal finding in unilateral DDH. Femoral derotational osteotomy seems not to be necessary in the groups of grades II and III in unilateral DDH after abnormal acetabular anteversion, acetabular index and acetabular coverage of the femoral head were recovered to normal range through pelvic osteotomy. This was because no significant difference was found in FA between the dislocated hips and the unaffected hips in the two groups. A wide safe range of CA from 24° to 62° was demonstrated on the unaffected hips. Thus, we recommend that femoral derotational osteotomy should be considered in DDH, especially in the group of grade IV, if the CA still is above 62° and the hip joint present instability in operation after abnormal acetabular anteversion, acetabular index and acetabular coverage of the femoral head are recovered to normal range through pelvic osteotomy. In the present study, we also observed a few cases in which the femoral neck anteversion was obviously increased on the unaffected hips compared to the dislocated hips even with careful and repeated evaluations. Consequently, the authors think that an individualized treatment plan based on the exact assessment for acetabular anteversion, femoral anteversion and combined anteversion through CT should be considered before surgical decision-making for children with DDH to avoid the complications. Our study did not observe the correlation between FA and AA. Further study should be performed because the sample size is small in the group of grades II and IV. A safe range of CA should be further researched at different ages and different populations.
Acknowledgments
Conflict of interest The authors declare that we have no conflict of interest.
References
- 1.Sewell MD, Eastwood DM (2011) Screening and treatment in developmental dysplasia of the hip—where do we go from here? Int Orthop. doi:10.1007/s00264-011-1257-z [DOI] [PMC free article] [PubMed]
- 2.Buckley SL, Sponseller PD, Magid D. The acetabulum in congenital and neuromuscular hip instability. J Pediatr Orthop. 1991;11:498–501. doi: 10.1097/01241398-199107000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Sankar WN, Neubuerger CO, Moseley CF. Femoral anteversion in developmental dysplasia of the hip. J Pediatr Orthop. 2009;29:885–888. doi: 10.1097/BPO.0b013e3181c1e961. [DOI] [PubMed] [Google Scholar]
- 4.Kim WY, Hutchinson CE, Andrew JG, Allen PD. The relationship between acetabular retroversion and osteoarthritis of the hip. J Bone Joint Surg Br. 2006;88:727–729. doi: 10.2106/JBJS.E.00550. [DOI] [PubMed] [Google Scholar]
- 5.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:263–269. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 6.Bicanic G, Delimar D, Delimar M, Pecina M. Influence of the acetabular cup position on hip load during arthroplasty in hip dysplasia. Int Orthop. 2009;33:397–402. doi: 10.1007/s00264-008-0683-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Browning WH, Rosenkrantz H, Tarquino T. Computed tomography in congenital hip dislocation. The role of acetabular anteversion. J Bone Joint Surg Am. 1982;64:27–31. [PubMed] [Google Scholar]
- 8.Sarbana S, Ozturkb A, Tabura H, Isikan UE. Anteversion of the acetabulum and femoral neck in early walking age patients with developmental dysplasia of the hip. J Pediatr Orthop B. 2005;14:410–414. doi: 10.1097/01202412-200511000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Li LY, Zhang LJ, Zhao Q, Wang EB. Measurement of acetabular anteversion in developmental dysplasia of the hip in children by two- and three-dimensional computed tomography. J Int Med Res. 2009;37:567–575. doi: 10.1177/147323000903700234. [DOI] [PubMed] [Google Scholar]
- 10.Edelson JG, Hirsch M, Weinberg H, Attar D, Barmeir E. Congenital dislocation of the hip and computerised axial tomography. J Bone Joint Surg Br. 1984;66:472–478. doi: 10.1302/0301-620X.66B4.6746676. [DOI] [PubMed] [Google Scholar]
- 11.Kim SS, Frick SL, Wenger DR. Anteversion of the acetabulum in developmental dysplasia of the hip: analysis with computed tomography. J Pediatr Orthop. 1999;19:438–442. doi: 10.1097/00004694-199907000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Fujii M, Nakashima Y, Yamamoto T. Acetabular retroversion in developmental dysplasia of the hip. J Bone Joint Surg Am. 2010;92:895–903. doi: 10.2106/JBJS.I.00046. [DOI] [PubMed] [Google Scholar]
- 13.Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88:372–379. doi: 10.2106/JBJS.D.02385. [DOI] [PubMed] [Google Scholar]
- 14.Mootha AK, Saini R, Dhillon M. Do we need femoral derotation osteotomy in DDH of early walking age group? A clinico-radiological correlation study. Arch Orthop Trauma Surg. 2010;130:853–858. doi: 10.1007/s00402-009-1020-8. [DOI] [PubMed] [Google Scholar]
- 15.Catherine M, Taylor FN, Lee C, Graham HK, Nattrass GR. MRI evaluation of surgical management in developmental dysplasia of hip in childhood. J Pediatr Orthop. 2002;22:92–97. [PubMed] [Google Scholar]
- 16.Mootha AK, Saini R, Dhillon MS, Aggarwal S, Kumar V, Tripathy SK. MRI evaluation of femoral and acetabular anteversion in developmental dysplasia of the hip. A study in an early walking age group. Acta Orthop Belg. 2010;76:174–180. [PubMed] [Google Scholar]
- 17.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52:148–159. [PubMed] [Google Scholar]
- 18.Komeno M, Hasegawa M, Sudo A, Uchida A. Computed tomographic evaluation of component position on dislocation after total hip arthroplasty. Orthopedics. 2006;29:1104–1108. doi: 10.3928/01477447-20061201-05. [DOI] [PubMed] [Google Scholar]
- 19.Dorr LD, Malik A, Dastane M, Wan Z. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009;467:119–127. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tönnis D. Die angeborene Hüftdysplasie und Hüftluxation im Kindes-und Erwachsenenalter. Berlin: Springer; 1984. Nomenklatur der angeborenen Hüftluxation; p. 86. [Google Scholar]
- 21.Zilber S, Lazennec JY, Gorin M, Saillant G. Variations of caudal, central, and cranial acetabular anteversion according to the tilt of the pelvis. Surg Radiol Anat. 2004;26:462–465. doi: 10.1007/s00276-004-0254-y. [DOI] [PubMed] [Google Scholar]
- 22.Bosse HJ, Lee D, Henderson ER, Sala DA, Feldman DS. Pelvic positioning creates error in ct acetabular measurements. Clin Orthop Relat Res. 2011;469:1683–1691. doi: 10.1007/s11999-011-1827-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Berkeley ME, Dickson JH, Cain TE, Donovan MM. Surgical therapy for congenital dislocation of the hip in patients who are twelve to thirty-six months old. J Bone Joint Surg Am. 1984;66:412–420. [PubMed] [Google Scholar]
- 24.Wenger DR, Lee CS, Kolman B. Derotational femoral shortening for developmental dislocation of the hip: special indications and results in the child younger than 2 years. J Pediatr Orthop. 1995;15:768–779. doi: 10.1097/01241398-199511000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Zadeh HG, Catterall A, Hashemi-Nejad A, Perry RE. Test of stability as an aid to decide the need of osteotomy in association with open reduction in developmental dislocation of hip. J Bone Joint Surg Br. 2000;82:12–19. doi: 10.1302/0301-620X.82B1.9618. [DOI] [PubMed] [Google Scholar]