Abstract
Purpose
The American College of Radiologists (ACR) recognises the value of magnetic resonance imaging (MRI) as the investigation of choice in patients with a clinically suspected scaphoid fracture but normal plain radiographs. The Royal College of Radiologists (RCR) in the UK produces no similar guidelines, as evidenced by the inconsistent management of such cases in hospitals around the UK. In discussion with our musculoskeletal radiologists, we implemented new guidelines to standardise management of our patients and now report our findings.
Methods
A consecutive series of 137 patients referred to the orthopaedic department with clinically suspected scaphoid fracture but normal series of plain radiographs were prospectively followed up over a two-year period. We implemented the use of early MRI for these patients and determined its incidence of detected scaphoid injury in addition to other occult injuries. We then prospectively examined results of these findings on patient management.
Results
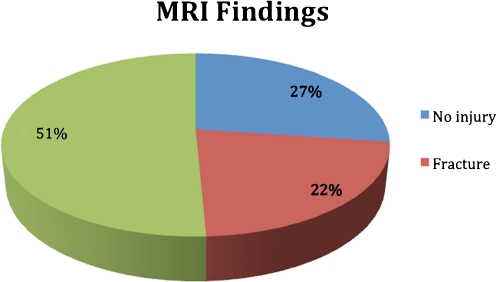
Thirty-seven (27%) MRI examinations were normal with no evidence of a bony or soft-tissue injury. Soft-tissue injury was diagnosed in 59 patients (43.4%). Of those, 46 were triangular fibrocartilage complex (TFCC) tears (33.8%) and 18 were intercarpal ligament injuries (13.2 %). Bone marrow oedema with no distinct fracture was discovered in 55 cases (40.4%). In 17 (12.5%) cases, this involved only the scaphoid. In the remainder, it also involved the other carpal bones or distal radius. Fracture(s) were diagnosed on 30 examinations (22.0%).
Conclusions
MRI should be regarded as the gold standard investigation for patients in whom a scaphoid fracture is suspected clinically. It allows the diagnosis of occult bony and soft-tissue injuries that can present clinically as a scaphoid fracture; it also helps exclude patients with no fracture. We believe that there is a need to implement national guidelines for managing occult scaphoid fractures.
Introduction
Scaphoid fracture is the most common carpal bone fracture [1]. Of particular clinical relevance is the risk of nonunion and its association with avascular necrosis (AVN) in 5–12% of cases [2]. Scaphoid fracture can remain radiographically occult for up to six weeks [3] and is initially occult in 16% of cases [4]. Traditional practice has been to immobilise the wrist when there is clinical suspicion of a scaphoid fracture but normal radiographs. The patient then undergoes serial radiographs and clinical review at intervals until a diagnosis is made or symptoms resolve. This can result in unnecessary overtreatment of many patients, with further implications for work, daily activities and health care resources. There has been much discussion about the most appropriate investigation of patients with a clinically suspected scaphoid injury but normal plain radiographs. Developments in radiological investigations have increased the options for obtaining such a diagnosis. Recent literature variably suggests that nuclear bone scintigraphy (NBS), computed tomography (CT) and magnetic resonance imaging (MRI) can all be used as the investigation of choice in patients with a clinically suspected scaphoid fracture but normal plain radiographs [5, 6].
The American College of Radiologists (ACR) recognises the value of MRI and recommends it as the first-choice, second-line investigation [7, 8]. The Royal College of Radiologists (RCR) in the UK has no similar guidelines as evidenced by the inconsistent management of these cases in hospitals around the country [9]. At our institution, we had no guidelines in place for such patients. Patients were therefore investigated and managed with various methods, including immobilisation with serial plain radiographs and clinical review, NBS, MRI and CT. In discussion with our musculoskeletal radiologists, we implemented guidelines to standardise patient management, and we now report our findings.
Materials and methods
A consecutive series of patients referred to the orthopaedic department with clinically suspected scaphoid fracture but normal scaphoid plain radiographs were prospectively followed up over a two-year period. All patients were treated with a scaphoid immobilisation splint or plaster and were seen in fracture clinic within one week of the injury. At that review, all patients with clinical signs of a scaphoid fracture were referred for a wrist MRI, which was performed within seven days of request, with a GE Excite Echospeed/Twinspeed 1.5 T scanner with a GE high-resolution wrist array coil. Routine protocol included sagittal T1 spin echo (SE), axial and coronal T2 fast spin echo with fat saturation (FSE FSAT), coronal proton-density fast-recovery FSE (PD FR-FSE) and coronal 3D fast spoiled-gradient recalled acquisition in steady state (F-SPGR). Our consultant musculoskeletal radiologists independently reported on the MRI scans, and patients were then reviewed.
Results
One hundred and thirty-six patients in whom scaphoid fracture was clinically suspected but not demonstrated on initial scaphoid radiographs underwent an MRI within seven days of their first fracture-clinic appointment. There were 79 male (58%) and 57 female (42%) patients, with an average age of 34.6 (n = 136) years. Injury mode was sporting or accidental falls in all cases.
MRI results
Thirty-seven (27%) MRI examinations were normal with no evidence of a bony or soft-tissue injury (Fig. 1).
Fig. 1.
Magnetic resonance imaging findings
Soft-tissue injury was diagnosed in 59 patients (43.4%). Of these, 46 were triangular fibrocartilage complex (TFCC) tears (33.8%), and 18 were intercarpal ligament injuries (13.2 %). Bone marrow oedema with no distinct fracture was discovered in 55 cases (40.4%). In 17 (12.5%) cases, this involved only the scaphoid. In the remainder, it also involved the other carpal bones or distal radius. Fractures were diagnosed on 30 examinations (22.0%). A scaphoid fracture was found in 16 (11.7%) patients, of whom two also had fractures of other carpal bones; 14 (10.3%) patients did not have a scaphoid fracture but were found to have occult fractures of the other carpal bones or the distal radius. These fractures consisted of seven distal radial, three hamate, three lunate, three triquetral, two trapezoid and one capitate.
Result of findings on patient management
Following MRI and review, the 30 fractures were immobilised appropriately and reviewed clinically and radiologically. The 37 cases in which injury was excluded were discharged with no further follow-up. Patients with soft-tissue injury and/or bone bruising were managed conservatively with soft-splint immobilisation and further clinic follow-up. Of these, ten TFCC tears were persistently symptomatic and were subsequently referred for an upper-limb-specialist opinion.
Discussion
There has been much discussion about the most appropriate investigation of patients with a clinically suspected scaphoid injury but normal plain radiographs. Developments in radiological investigations have increased the options for obtaining a diagnosis. Recent literature has variably suggested that NBS, CT and MRI can all be used as the investigation of choice in patients with a clinically suspected scaphoid fracture but normal plain radiographs. Isotope bone scanning is highly sensitive but has a lower specificity, thus leading to a high false positive rate [5, 10, 11]. CT also has similar specificity issues in addition to exposing the patient to ionising radiation [12–14]. MRI is an effective method for diagnosing occult fractures, having excellent sensitivity, specificity and reliability [4, 6, 12, 14, 15]. MRI also allows detection not only of occult fractures of the scaphoid but occult fractures of the other carpal bones [15], bone oedema indicating trabecular injury and soft-tissue injuries to ligamentous structures around the wrist [12]. MRI diagnosis of these injuries allows implementation of early definitive treatment and can thus prevent the need for multiple reviews and immobilisation. Although soft-tissue injuries may not require active treatment, diagnosis can allay patient fears and, again, allow early mobilisation and patient discharge. MRI can be used to exclude a fracture and thus prevent overtreatment. MRI excluded fracture in 106 of 136 cases (78%), which implies a potential cost and resource benefit by reducing the clinic time required to manage these cases, the period of immobilisation and subsequent patient days off work. Although we did not perform a formal cost analysis, several studies show that the use of early MRI is cost effective in managing occult scaphoid fractures [16–19]. Dorsay et al. concluded that MRI costs were equal to those of the traditional protocol due to the reduced number of patients undergoing unnecessary treatment and follow-up [18]. Their study did not, however, quantify the indirect benefit of earlier return to work. Hansen et al. found that although there was a minor increase in the cost of hospital treatment with MRI scanning, there was a significant reduction in immobilisation time and time off work; they concluded that MRI significantly reduces the cost to society without reducing treatment effectiveness [17]. We feel that the use of a dedicated small-extremity scanner with faster scanning protocols would further reduce costs, and we are looking to implement this in our unit.
There is a wide variation in the choice of investigation and management of occult scaphoid fractures, as revealed in a number of studies, which indicates that only a small percentage of surgeons are aware of local protocols [9, 20]. In the UK, the RCR produces no specific guidelines to assist in these cases, which could explain the widespread variability, as local preferences and resources dictate management. However, the ACR recognises the need for an evidence-based approach and produced national guidelines for these cases. They advise that MRI be used as the gold-standard, second-line investigation in preference to CT and NBS [7, 8].
Conclusion
MRI should be regarded as the gold-standard investigation for patients in whom a scaphoid fracture is suspected clinically. It allows the diagnosis of occult bony and soft-tissues injuries that can present clinically as a scaphoid fracture in addition to excluding patients with no fracture. This ensures that appropriate management can be implemented and thus prevent over- and undertreatment. Although guidelines for managing this common problem exist in the USA, there are none in the UK We believe there is a need to implement national guidelines for managing occult scaphoid fractures.
Acknowledgments
Conflict of interest statement There are no conflicts of interest.
References
- 1.Sonin AH, Rogers LF. Skeletal Trauma. In: Grainger RG, Allison DJ, editors. Diagnostic Radiology. 3. New York: Churchill Livingston; 1997. pp. 1573–1628. [Google Scholar]
- 2.Leslie JJ, Dickson RA. The fractured carpal scaphoid. Natural history and factors influencing outcome. J Bone Joint Surg (Br) 1981;63-B:225–230. doi: 10.1302/0301-620X.63B2.7217146. [DOI] [PubMed] [Google Scholar]
- 3.Waizenegger M, Barton NJ, Davis TR, Wastie ML. Clinical signs in scaphoid fractures. J Hand Surg (Br) 1994;19:743–747. doi: 10.1016/0266-7681(94)90249-6. [DOI] [PubMed] [Google Scholar]
- 4.Hunter J, Escobedo E, Wilson AJ, Hanel DP, Zink-Brody GC, Mann FA. MR imaging of clinically suspected scaphoid fractures. AJR Am J Roentgenol. 1997;168:1287–1293. doi: 10.2214/ajr.168.5.9129428. [DOI] [PubMed] [Google Scholar]
- 5.Tiel-van Buul MMC, Beek EJR, Broekhuizen AH, et al. Radiography and scintigraphy of suspected scaphoid fracture. J Bone Joint Surg (Br) 1993;75:61–65. doi: 10.1302/0301-620X.75B1.8421037. [DOI] [PubMed] [Google Scholar]
- 6.Yao L, Lee JK. Occult intraosseous fracture: detection with MR imaging. Radiology. 1988;167:749–751. doi: 10.1148/radiology.167.3.3363134. [DOI] [PubMed] [Google Scholar]
- 7.Rubin DA et al. (2007) American College of Radiologists Practice Guidelines for the performance of magnetic resonance imaging (MRI) of the wrist. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/guidelines/dx/musc/mri_wrist.aspx
- 8.Rubin DA et al. (2008) American College of Radiologists Appropriateness Criteria. http://www.acr.org/SecondaryMainMenuCategories/quality_safety/app_criteria/pdf/ExpertPanelonMusculoskeletalImaging/AcuteHandandWristTraumaDoc1.aspx
- 9.Brookes-Fazakerley SD, Kumar AJ, Oakley J. Survey of the initial management and imaging protocols for occult scaphoid fractures in UK hospitals. Skeletal Radiol. 2009;38(11):1045–1048. doi: 10.1007/s00256-008-0640-3. [DOI] [PubMed] [Google Scholar]
- 10.Beeres FJ, Hogervorst M, Rhemrev SJ, Hollander P, Jukema GN. A prospective comparison for suspected scaphoid fractures: bone scintigraphy versus clinical outcome. Injury. 2007;38(7):769–774. doi: 10.1016/j.injury.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 11.Beeres FJ, Rhemrev SJ, Hollander P, et al. Early magnetic resonance imaging compared with bone scintigraphy in suspected scaphoid fractures. J Bone Joint Surg Br. 2008;90(9):1205–1209. doi: 10.1302/0301-620X.90B9.20341. [DOI] [PubMed] [Google Scholar]
- 12.Jenkins PJ, Slade K, Huntley JS, Robinson CM. A comparative analysis of the accuracy, diagnostic uncertainty and cost of imaging modalities in suspected scaphoid fractures. Injury. 2008;39(7):768–774. doi: 10.1016/j.injury.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 13.Adey L, Souer JS, Lozano-Calderon S, Palmer W, Lee SG, Ring D. Computed tomography of suspected scaphoid fractures. J Hand Surg Am. 2007;32(1):61–66. doi: 10.1016/j.jhsa.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Yin ZG, Zhang JB, Kan SL, Wang XG. Diagnosing suspected scaphoid fractures: a systematic review and meta-analysis. Clin Orthop Relat Res. 2010;468(3):723–734. doi: 10.1007/s11999-009-1081-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Breitenseher MJ, Metz VM, Gilula LA, et al. Radiographically occult scaphoid fractures: value of MR imaging in detection. Radiology. 1997;203:245–250. doi: 10.1148/radiology.203.1.9122402. [DOI] [PubMed] [Google Scholar]
- 16.Gooding A, Coates M, Rothwell A. Accident Compensation Corporation. Cost analysis of traditional follow-up protocol versus MRI for radiographically occult scaphoid fractures: a pilot study for the Accident Compensation Corporation. N Z Med J. 2004;117(1201):U1049. [PubMed] [Google Scholar]
- 17.Hansen TB, Petersen RB, Barckman J, Uhre P, Larsen K. Cost-effectiveness of MRI in managing suspected scaphoid fractures. J Hand Surg Eur. 2009;34(5):627–630. doi: 10.1177/1753193409105322. [DOI] [PubMed] [Google Scholar]
- 18.Dorsay TA. Cost-effectiveness of immediate MR imaging versus traditional follow-up for revealing radiographically occult scaphoid fractures. AJR Am J Roentgenol. 2001;177:1257–1263. doi: 10.2214/ajr.177.6.1771257. [DOI] [PubMed] [Google Scholar]
- 19.Brooks S, Cicuttini FM, Lim S, Taylor D, Stuckley SL, Wluka AE. Cost effectiveness of adding magnetic resonance imaging to the usual management of suspected scaphoid fractures. Br J Sports Med. 2005;39:75–79. doi: 10.1136/bjsm.2003.007435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Groves AM, Kayani I, Syed R, Hutton BF, Bearcroft PP, Dixon AK, Ell PJ. An international survey of hospital practice in the imaging of acute scaphoid trauma. AJR Am J Roentgenol. 2006;187(6):1453–1456. doi: 10.2214/AJR.05.0686. [DOI] [PubMed] [Google Scholar]