Abstract
Purpose
In contrast to bone cuts, soft-tissue releases cannot be planned sufficiently prior to total knee arthroplasty (TKA). Intra-operative evaluation of the extension gap after tibial or femoral resection may result in an unnecessarily excessive bone resection. The present study examines whether extension gap asymmetry can be calculated from the pre-operative long standing X-ray.
Methods
In this retrospective study, 32 patients with navigated unconstrained TKA were included. The pre-operative malalignment was measured on long standing X-rays and compared with the extension gap asymmetry that was documented by the navigation system intra-operatively.
Results
The mean pre-operative malalignment was 9.8° (20° valgus to 14.8° varus). The intra-operatively measured extension gap showed a mean asymmetry of 3.4 ± 2.4 mm. Both correlated following the equation: asymmetry [mm] = 0.35 * malalignment [°] (R = 0.855, P < 0.001).
Conclusions
We recommend planning the intra-operative release and tibial bone cut using long standing X-rays.
Introduction
The most difficult surgical step in primary total knee arthroplasty, but the one that is decisive for the outcome, is soft-tissue release [1–8] rather than implant design [9, 10]. However, in contrast to bone cuts and implant sizes, it cannot be planned sufficiently pre-operatively. In many cases, the flexion and extension gap are only evaluated intra-operatively after tibial or femoral resection, leading to the use of high inlays rather than a bone-sparing approach. It has recently been shown that the amount of necessary tibial resection to produce a well-balanced knee is less than the thinnest tibial plateau plus insert in most cases and depends on the pre-operative deformity [11]. Since the amount of ligamentous instability and necessary soft-tissue release cannot be sufficiently planned pre-operatively, an anatomical tibial resection height leads to higher than the smallest available insert in most cases. This is not only equivalent to unnecessary primary bone loss but may result in a component size smaller than the tibia based on the chalice shape of the tibia.
If the need for a semi-constrained implant is only ascertained intra-operatively, costs are incurred for additional instrumentation (set-up time, preparation and sterilization), which could be avoided through pre-operative planning.
The clinical examination at most provides an indication of the extent of an instability or contracture, without allowing precise quantification. Stress radiographs under varus and valgus conditions enable a better determination of the stability of the knee joint [12], but involve additional radiation exposure and greater costs and are therefore reserved for special questions [13]. In contrast to this, the pre-operative long standing X-ray is standard in most hospitals, as it is necessary for planning the tibial and femoral resection planes in relation to the mechanical axis [14–16]. Up to now, it has been unclear to what extent the axis deviation shown in this radiograph allows conclusions to be drawn about the ligamentous situation of the knee joint, since not just soft-tissue tension but also cartilage/bone defects and extra-articular deviations of the femur or tibia determine the leg axis. The objective of the present study was to find out whether pre-operative measurement of the leg axis in the long standing X-rays can be used to determine extension gap asymmetry in clinical practice.
Method
Thirty-two consecutive patients who had undergone navigated (Aesculap Orthopilot 4.2) unconstrained bicondylar surface replacement (Emotion, Aesculap, Tuttlingen, Germany) of the knee joint were included in this retrospective study. In order to find a representative correlation, no exclusion criteria were defined. Primary arthroses were distinguished from secondary ones, which were differentiated into post-traumatic, rheumatoid, post-infectious and other arthroses.
Radiological evaluation
In the pre-operative digital long standing X-rays, the coordinates of the hip, knee and ankle centres were determined by two investigators (G.M. and D.M.) and documented separately to check inter-observer variability. From this, the angles (alpha) between the mechanical tibial and femoral axis were determined, whereby varus malalignments produced a positive angle and valgus malalignments a negative angle.
Operation
The implantation method corresponds to the tibia first technique. After reading in the landmarks, a measured resection of the tibia perpendicular to the mechanical axis was performed. The knee joint was tensioned in extension by the instruments medially and laterally with the same force, and the distances between the tibial resection plane and the planned femoral resection plane were determined medially and laterally and documented. The difference in these distances corresponds to the asymmetry of the extension gap before any soft-tissue release.
Statistics
The inter-observer variability was defined as the difference in the measured angle and is stated as the mean, standard deviation and maximum. The correlation between the pre-operative malalignment angle and the intra-operative imbalance of the extension gap was tested by Pearson correlation with a level of significance of P = 0.05. The mean deviation with standard deviation of the beta measurements from the predicted angles was determined.
Results
Of the ten men and 22 women, 28 patients had primary gonarthrosis. The secondary arthroses were differentiated into two post-traumatic arthroses after lateral tibia head fracture and one case each of a post-infectious arthrosis and arthrosis secondary to rheumatoid arthritis. One female patient was excluded who showed rapid destruction of the medial tibia head within a few months, due to rheumatoid arthritis, with a varus malalignment of 39°.
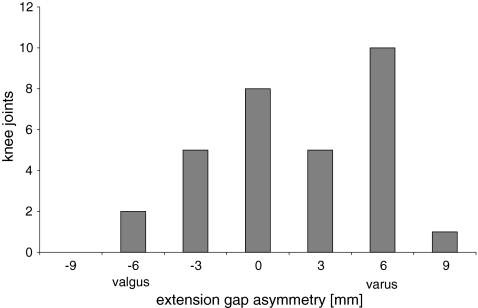
The inter-observer variability produced a mean of 0.4° ± 0.3°, with a maximum of 1.0°. The average pre-operative malalignment in the patient population investigated was 9.8° (20.0° valgus to 14.8° varus; Fig. 1). The intra-operatively determined extension gap showed an average asymmetry of 3.4 mm ± 2.4 mm (8 mm medially unstable to 9 mm laterally unstable; Fig. 2). This correlated significantly with the pre-operative malalignment, following the equation: asymmetry [mm] = 0.35 * malalignment [°] (R = 0.855, P < 0.001; Fig. 3).
Fig. 1.
Pre-operative malalignment determined on the basis of the long standing X-ray
Fig. 2.
Asymmetry of the extension gap measured by the navigation device intra-operatively after tibial resection and insertion of a tensioning device
Fig. 3.
Correlation between preoperative malalignment and asymmetry of the extension gap
When this formula was applied, it produced an average deviation in the actual from the predicted asymmetry of the extension gap of 1.9 mm ± 1.1 mm.
Discussion
The pre-operative long standing X-ray enables an objective planning of the necessary extension gap release, which is sufficiently accurate for use in clinical practice. Per degree of axial malalignment, an asymmetry of the extension gap of 0.35 mm is to be expected.
This result is surprising, since the malalignment of the leg axis is dependent on intra- and extra-articular osseous deformities and ligamentous insufficiencies or contractures. The nevertheless good correlation suggests that osseous malalignments, hypoplasias and defects interact with the capsulo-ligamentous stabilizers during the genesis of arthrosis [17].
One limitation of this study is the impreciseness in determination of the mechanical axes and angles on the long standing X-ray that can be flawed by deviations of the AP path of rays, especially in flexion contracture. Another limitation is the fact that ligamentous instability might not be seen in long standing X-rays in some cases (e.g. medial instability in severe varus deformity or lateral instability in severe valgus deformity).
The ability to plan the expected extension gap release pre-operatively opens up the objective choice between a medial or a lateral approach within a differentiated surgical strategy. If the prognosis is a considerable extension gap asymmetry, the use of a semi-constrained implant can be planned, so that intra-operative changes in system can be avoided.
Independently of the surgical method (tibia or femur first), the possibility to pre-operatively plan the extension gap release and thus estimate the amount of tibial resection will minimize the need for high inlays and spare proximal tibial bone [11]. Regarding the chalice shape of the tibial head this may allow additional bony release through downsizing and lateralization of the tibial component in some cases.
In light of the potential advantages and the minimal effort involved in measurement, we recommend the planning of release and tibial resection on the basis of a long standing X-ray.
Acknowledgments
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Asano H, Muneta T, Sekiya I. Soft tissue tension in extension in total knee arthroplasty affects postoperative knee extension and stability. Knee Surg Sports Traumatol Arthrosc. 2008;16:999–1003. doi: 10.1007/s00167-008-0591-1. [DOI] [PubMed] [Google Scholar]
- 2.Whiteside LA. Soft tissue balancing: the knee. J Arthroplasty. 2002;17:23–27. doi: 10.1054/arth.2002.33264. [DOI] [PubMed] [Google Scholar]
- 3.Peters CL. Soft-tissue balancing in primary total knee arthroplasty. Instr Course Lect. 2006;55:413–417. [PubMed] [Google Scholar]
- 4.Bottros J, Gad B, Krebs V, Barsoum WK. Gap balancing in total knee arthroplasty. J Arthroplasty. 2006;21:11–15. doi: 10.1016/j.arth.2006.02.084. [DOI] [PubMed] [Google Scholar]
- 5.Unitt L, Sambatakakis A, Johnstone D, Briggs TW. Short-term outcome in total knee replacement after soft-tissue release and balancing. J Bone Joint Surg Br. 2008;90:159–165. doi: 10.1302/0301-620X.90B2.19327. [DOI] [PubMed] [Google Scholar]
- 6.Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res. 1985;192:13–22. [PubMed] [Google Scholar]
- 7.Higuchi H, Hatayama K, Shimizu M, Kobayashi A, Kobayashi T, Takagishi K. Relationship between joint gap difference and range of motion in total knee arthroplasty: a prospective randomised study between different platforms. Int Orthop. 2009;33(4):997–1000. doi: 10.1007/s00264-009-0772-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Schnurr C, Nessler J, König DP. Is referencing the posterior condyles sufficient to achieve a rectangular flexion gap in total knee arthroplasty? Int Orthop. 2009;33(6):1561–1565. doi: 10.1007/s00264-008-0656-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sumino T, Gadikota HR, Varadarajan KM, Kwon YM, Rubash HE, Li G (2011) Do high flexion posterior stabilised total knee arthroplasty designs increase knee flexion? A meta analysis. Int Orthop. March 16. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 10.Moynihan AL, Varadarajan KM, Hanson GR, Park SE, Nha KW, Suggs JF, Johnson T, Li G. In vivo knee kinematics during high flexion after a posterior-substituting total knee arthroplasty. Int Orthop. 2010;34(4):497–503. doi: 10.1007/s00264-009-0777-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schnurr C, Csécsei G, Nessler J, Eysel P, König DP (2010) How much tibial resection is required in total knee arthroplasty? Int Orthop. May 9. [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 12.Ishii Y, Noguchi H, Matsuda Y, Kiga H, Takeda M, Toyabe S. Preoperative laxity in osteoarthritis patients undergoing total knee arthroplasty. Int Orthop. 2009;33:105–109. doi: 10.1007/s00264-007-0467-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Song EK, Seon JK, Yoon TR, Park SJ, Cho SG, Yim JH. Comparative study of stability after total knee arthroplasties between navigation system and conventional techniques. J Arthroplasty. 2007;22:1107–1111. doi: 10.1016/j.arth.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Sailer J, Scharitzer M, Peloschek P, Giurea A, Imhof H, Grampp S. Quantification of axial alignment of the lower extremity on conventional and digital total leg radiographs. Eur Radiol. 2005;15:170–173. doi: 10.1007/s00330-004-2436-8. [DOI] [PubMed] [Google Scholar]
- 15.Heyse TJ, Decking R, Davis J, Boettner F, Laskin RS. Varus gonarthrosis predisposes to varus malalignment in TKA. HSS J. 2009;5:143–148. doi: 10.1007/s11420-009-9118-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rauh MA, Boyle J, Mihalko WM, Phillips MJ, Bayers-Thering M, Krackow KA. Reliability of measuring long-standing lower extremity radiographs. Orthopedics. 2007;30:299–303. doi: 10.3928/01477447-20070401-14. [DOI] [PubMed] [Google Scholar]
- 17.Fishkin Z, Miller D, Ritter C, Ziv I. Changes in human knee ligament stiffness secondary to osteoarthritis. J Orthop Res. 2002;20:204–207. doi: 10.1016/S0736-0266(01)00087-0. [DOI] [PubMed] [Google Scholar]