Abstract
Purpose
It is broadly supposed that in total knee arthroplasty, the flexion/extension gap ratio is increased after resection of the posterior cruciate ligament (PCL). However, studies are rare and results are inconsistent. Therefore, this study was conducted to determine whether PCL release regularly increases the flexion gap.
Methods
Data from 50 consecutive posterior stabilised knee prostheses were analysed retrospectively. Using imageless computer navigation, the joint-gap width was measured over the entire range of motion before and after PCL release.
Results
PCL release had no effect on the extension gap, but it increased the flexion gap significantly. An increase of >3 mm occurred in 36% of patients and of >5 mm in 12%. No clinically relevant effect (<2 mm) was found in 44% of patients.
Conclusion
PCL release increased the flexion/extension gap ratio on average, but the individual effect could not be predicted. Therefore, we recommend PCL release before the femoral resections are performed, as this step mainly determines the ratio between extension and flexion gap.
Introduction
The debate concerning whether to retain or resect and substitute the posterior cruciate ligament (PCL) in total knee arthroplasty (TKA) is not new, and there is no clear consensus regarding the outcome [1]. Excellent clinical results have been reported for cruciate-retaining as well as cruciate-substituting prostheses [1–4]. In recent years, demand has increased for TKA to achieve deeper flexion, e.g. for kneeling or squatting [5–7]. It is generally agreed that the success of TKA depends on equally balanced extension and flexion gaps [8, 9]. Most publications indicate that PCL release substantially influences the joint-gap width. Authors of reviews state that sacrificing the PCL leads to an increased flexion gap [1, 10]. Different companies, in their operating manuals, advise a reduced tibial slope to compensate for an increased flexion gap if the PCL is resected [11]. If the flexion gap increase was constant, and therefore predictable, it would be adequate to depend on that and release the PCL through the bony femoral-box resection [1]. However, at that point of the procedure, the flexion/extension gap ratio has already been determined by the femoral distal and posterior resections. In contrast to this operative strategy, some studies indicate no effects of PCL release on the flexion/extension gap ratio [12, 13]. Therefore, it may be a better alternative to release the PCL prior to the femoral resections. In this case, the final flexion/extension gap ratio is known before femoral resections are performed. Unfortunately, sacrificing the PCL prior to femoral resection is often time-consuming, as the tibial insertion extends approximately 2.5 cm distal to the joint line and on the femoral side >20 mm in the anterior–posterior direction across the roof and medial side of the femoral intercondylar notch [2, 14]. Our study was designed to answer the following questions: Is the increase of the flexion/extension gap ratio after PCL release constant and therefore predictable? Is it therefore adequate to release the PCL after femoral distal and posterior cuts through the bony femoral box resection?
Materials and methods
Data from 50 posterior stabilised knee replacements (25 consecutive varus deformities; 25 consecutive valgus deformities) between July 2010 and January 2011 were retrospectively analysed. Details of the study population are shown in Table 1. Exclusion criteria were secondary gonarthrosis due to fracture or trauma, previous osseous or ligamentous operations on the knee joint, obvious PCL insufficiency and revision arthroplasties.
Table 1.
Details of the study population: mean (standard deviation; range)
| Valgus deformity | Varus deformity | Total | |
|---|---|---|---|
| Number of operative procedures | 25 | 25 | 50 |
| Age (years) | 66 (11; 40–87) | 68 (11; 42–83) | 67 (11; 40–87) |
| Gender (% female) | 92 | 46 | 69 |
| Side (% left) | 32 | 67 | 49 |
| Leg axis (° varus) | −6 (6; −1 to −15) | 10 (5; 2–20) | 1 (10, −15 to 20) |
All patients were operated upon by one surgeon (CS) using an imageless computer navigation device (CiKnee 2.1, Brainlab, Feldkirchen, Germany). All patients received the posterior stabilised cemented PFC sigma implant (DePuy, Leeds, UK) under general anaesthesia through a standardised medial parapatellar approach to the knee joint. After fixation of the reference arrays on Schanz screws in the tibial and femoral shafts, the anatomical landmarks of the knee joint and the joint surfaces were registered, as described in the literature [15]. Thereafter, the tibia was cut perpendicular to the mechanical tibial axis, with a 3° slope and 8 mm resection depth. PCL integrity was checked visually and by manual palpation. A tensor, distracting the medial and lateral joint gaps with a force of 150 Nm (Sensor Tensor, DePuy) was inserted into the joint gap (Fig. 1). If the joint-gap width was >12 mm, an additional 5 mm or 10 mm cap was fixed on the top of the medial or lateral site of the tensor to allow for adequate spring tension. The patella was placed in the anatomical position. Using the navigation device, ligament balancing was performed as described in the literature to achieve a balanced extension gap [10]. Depending on the severity of the deformity, a gradual release of the medial capsule, the pes anserinus and the superficial medial collateral ligament (varus deformity) or the lateral capsule, the iliotibial band and the lateral collateral ligament (valgus deformity) was performed. Thereafter, a dynamic measurement of the width of the joint gap was performed as follows: The tensor was fixed on the tibia plateau, and the patella was placed in the anatomical position. The knee was bent passively from 0° extension to 140° flexion by an electronic device, elevating the femur (Fig. 2). During knee flexion, the tibia movement was controlled by the surgeon’s hands, enabling physiological knee rotation. During this procedure, the navigation device continuously measured the width of the medial and lateral joint gaps, the mechanical knee axis and femoral rotation. Measurement procedures were repeated three times. The tensor was removed, and the PCL was resected at its femoral insertion. Completeness of the release was verified by manual palpation. Thereafter, the tensor was replaced into the joint gap, and the measurement procedure was repeated three times, as described above. All data were stored by the navigation device.
Fig. 1.

Tensor used in this study. The hand grip is used only to insert the tensor into the joint gap. This allows an anatomically appropriate position of the patella during knee flexion
Fig. 2.

Measurement setup. The tensor is positioned in the joint gap; the femur is elevated by an electronic leg holder. The patella remains in the anatomical position; the surgeon controls the tibia to allow physiological knee rotation during knee flexion
The following data were exported from the navigation device: mechanical leg axis in extension, rotation of the posterior femoral condyles referencing the tibial cut, width of the medial and lateral joint gap in 10° steps from 0° to 140° knee flexion. To check measurement accuracy of the navigation device and reproducibility of passive knee movements, measurements were repeated ten times in three patients, and differences between maximum and minimum values were calculated. This analysis resulted in differences <1 mm, or 1°; hence a measurement inaccuracy <1 mm or 1° was assumed for our measurement setup.
Statistical analysis Data was tested for normality using the Kolmogorov–Smirnov test. Depending on those test results, Student’s paired t test or Wilcoxon signed rank test were used to determine significance, which was set at 0.05. Correlations were evaluated using Pearson’s correlation coefficient. SPSS statistics 19.0 (IBM, Somers NY, USA) for windows was used for statistical analysis.
Results
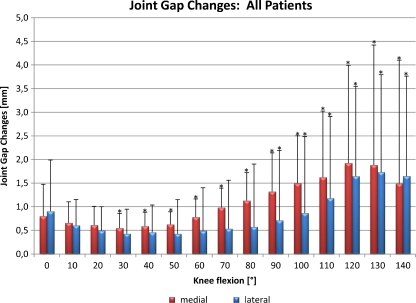
The analysis of all patients’ data showed that PCL release produced a significant increase in the medial and lateral flexion gap between 90° and 140° (Fig. 3). The biggest effect was measured in high flexion between 110° and 140°. PCL release had no significant effect on extension-gap width. The mean difference between the joint gap before and after PCL sacrifice averaged at 90°: 1.3 mm on the medial and 0.7 mm on the lateral site; and at 130°: 1.9 mm on the medial and 1.7 mm on the lateral site.
Fig. 3.
Differences in joint-gap width ([after sacrifice of the PCL] minus [before PCL release]) are shown for the entire range of knee flexion. Differences in the medial joint gap are represented by the red bars and in the lateral joint gap by the blue bars. Error bars standard deviation; asterisks significant differences. PCL posterior cruciate ligament
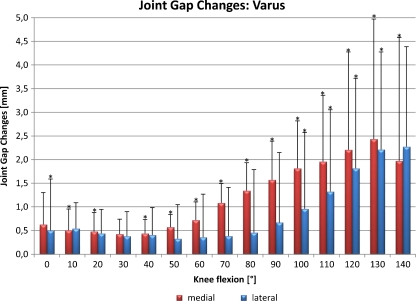
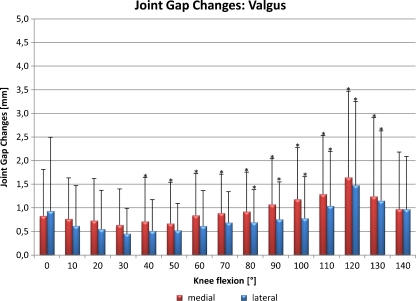
Measured increase in the flexion gap was greater in varus deformities (90°: medial 1.6 mm, lateral 0.7 mm; 130°: medial 2.4 mm, lateral 2.2 mm Fig. 4) than in valgus deformities (90°: medial 1.1 mm, lateral 0.8 mm; 130°: medial 1.2 mm, lateral 1.2 mm Fig. 5).
Fig. 4.
Differences in medial and lateral joint gaps in different knee flexions for varus deformities. Error bars standard deviation; asterisks significant differences
Fig. 5.
Joint-gap changes for valgus deformities. Error bars standard deviation; asterisks significant differences
Correlation analysis detected a significant relationship between flexion-gap increase and absolute value of the preoperative leg axis for the medial joint gap between 100° and 140° (100°: Pearson’s correlation coefficient 0.302, p = 0.035; 110°: 0.342, p = 0.016; 120°: 0.361, p = 0.011; 130°: 0.434, p = 0.005, 140°: 0.439, p = 0.041). No correlation was detected between the preoperative leg axis and the lateral joint gap. Substantial differences were noted in the study population: in about half of the patients, PCL resection provoked a clinically relevant increase in the flexion gap: in 28 patients (56%), the flexion gap increased >2 mm; in 18 patients (36%), >3 mm; in six patients (12%), >5 mm. By contrast, in 22 patients (44%), PCL sacrifice had no clinically relevant effect on the flexion gap (<2 mm). In addition, the effect of PCL release on extension- and flexion-gap symmetry was analysed. PCL sacrifice had no constant effect on extension-gap symmetry (mean change of the leg axis 0°; standard deviation (SD) 1°, range −3°to 5°; p = 0.1). By contrast, in 49 of the 50 patients, PCL release reduced the femoral component’s external rotation, which was required to produce a balanced flexion gap (mean −1°; SD 1°, range −5 to 1°; p < 0.001).
Discussion
Analysing combined patient data, our study demonstrates that PCL release significantly increases the flexion gap without a detectable effect on the extension gap. These results are generally in line with the majority of existing studies [9, 16–20]. In this context, we investigated high flexion grades and found that the biggest joint-gap increase was between 110° and 140°. To our knowledge, all other studies focused only on the joint gap between full extension and 90° [9, 12, 13, 16–21]. The proven increase in high flexion grades might be the reason for the higher range of motion that was frequently detected after posterior stabilised prostheses in comparison with posterior cruciate-retaining prostheses [22–24].
In our study, the increase in the joint-gap width in 90° flexion averaged only 1.3 mm on the medial site and 0.7 mm on the lateral site. Individual analysis showed that in 44% of patients, PCL release had no clinically significant effect on the flexion gap. On the other hand, in 36% of patients, the flexion gap increased >3 mm and in 12% >5 mm. Further analysis showed that the effect was more pronounced in varus than in valgus deformities. Furthermore, correlation analysis detected a bigger flexion-gap increase after PCL sacrifice if the preoperative deformity was more severe. However, of the 18 patients responding with a flexion-gap increase >3 mm, nine had a varus and nine a valgus deformity.
Comparison between our results and cadaver studies shows that those experiments demonstrated constant flexion-gap increases after PCL release of 6.4 mm [19] and 6.9 mm [18]. Those studies used knee joints without arthritis or deformity. Lüring et al. performed an extensive medial capsule ligament release with complete displacement of the medial collateral ligament; Mihalko and coworkers transected femur and tibia in the midshaft. Furthermore, it is proven that the PCL shows histological degeneration in the osteoarthritic knee and has less stiffness compared with the normal PCL [10, 25]. Those limitations make comparison of cadaver experiments and our clinical study difficult. Besides the cadaver studies, five in vivo studies measuring the flexion gap after PCL sacrifice showed more heterogeneous results: Kadoya et al. studied 30 patients with a varus deformity and found no effect of a PCL release on the extension gap but found a 4.8-mm medial and 4.4-mm lateral increase of the 90° flexion gap [17]. A significant flexion-gap increase was detected in 90% of patients. Park et al. studied 30 patients with severe varus arthritis with a deformity >20° varus or 15° flexion contracture [20]. They detected no effect of PCL release on the extension gap but an increase of 4.5-mm medial and 3.4-mm lateral joint gap at 90°. Chaiyakit et al. studied 16 patients with a varus deformity and measured a flexion gap increase at 90° of 1.3 mm on the medial and 2.1 mm on the lateral side [16]. The latter two studies included no information on how many patients reacted with a relevant flexion-gap increase. Baldini and coworkers reported on 50 patients with varus and valgus deformity and found a symmetrical effect from the PCL release of 1.3 mm on the joint gap in extension and 90° flexion [12]. A flexion-gap increase >2 mm was measured in 26% of patients. Matziolis et al. measured a symmetrical extension and flexion gap after PCL sacrifice in 92 patients [13]. With regard to preoperative deformities or rate of flexion-gap increases, no further information was included in that manuscript. In summary, three studies involving 76 patients with varus arthritis demonstrated an increase solely of the flexion gap after PCL release; two studies involving 142 patients with varus and valgus deformities found no effect or a similar effect on extension and flexion gap. It should be noted that each study used a different spreader to distract the joint gap, a fact that may further complicate comparison between studies. In 49 of 50 patients in our study, a bigger effect on the flexion gap after PCL release was seen on the medial than on the lateral joint gap. If the gap-balanced procedure is used, PCL release leads to a constant reduction of the femoral component’s external rotation. Similarly, Park et al. measured a reduced external rotation of the femoral component of 1.6° after PCL resection [20].
In conclusion, our results show that PCL release has no effect on the extension gap but increases the flexion gap, with a maximum effect between 110° and 140°. This finding might be one reason for the frequently detected higher range of motion after posterior stabilised prostheses. However, the enormous scatter range of our results, reaching from 0 mm to 9 mm flexion-gap increase, indicates that the effect of PCL release cannot be predicted. As a consequence of our results, we recommend a PCL release before femoral resections are performed, as this step mainly determines the ratio between extension and flexion gaps.
Acknowledgments
Conflict of interest The authors state that they have no conflict of interest.
References
- 1.Sierra RJ, Berry DJ. Surgical technique differences between posterior-substituting and cruciate-retaining total knee arthroplasty. J Arthroplasty. 2008;23:20–23. doi: 10.1016/j.arth.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 2.Lombardi AV, Jr, Berend KR. Posterior cruciate ligament-retaining, posterior stabilized, and varus/valgus posterior stabilized constrained articulations in total knee arthroplasty. Instr Course Lect. 2006;55:419–427. [PubMed] [Google Scholar]
- 3.Swanik CB, Lephart SM, Rubash HE. Proprioception, kinesthesia, and balance after total knee arthroplasty with cruciate-retaining and posterior stabilized prostheses. J Bone Joint Surg Am. 2004;86(A):328–334. doi: 10.2106/00004623-200402000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Sumino T, Gadikota HR, Varadarajan KM, Kwon YM, Rubash HE, Li G (2011) Do high flexion posterior stabilised total knee arthroplasty designs increase knee flexion? A meta analysis. Int Orthop. doi:10.1007/s00264-011-1228-4 [DOI] [PMC free article] [PubMed]
- 5.Tsuji S, Tomita T, Hashimoto H, Fujii M, Yoshikawa H, Sugamoto K. Effect of posterior design changes on postoperative flexion angle in cruciate retaining mobile-bearing total knee arthroplasty. Int Orthop. 2011;35:689–695. doi: 10.1007/s00264-010-1060-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharkey PF, Miller AJ (2011) Noise, Numbness, and Kneeling Difficulties After Total Knee Arthroplasty Is the Outcome Affected? J Arthroplasty. doi:10.1016/j.arth.2010.10.009 [DOI] [PubMed]
- 7.Tanavalee A, Ngarmukos S, Tantavisut S, Limtrakul A (2010) High-flexion TKA in patients with a minimum of 120 degrees of pre-operative knee flexion: outcomes at six years of follow-up. Int Orthop. doi:10.1007/s00264-010-1140-3 [DOI] [PMC free article] [PubMed]
- 8.Lombardi AV, Jr, Berend KR, Aziz-Jacobo J, Davis MB. Balancing the flexion gap: relationship between tibial slope and posterior cruciate ligament release and correlation with range of motion. J Bone Joint Surg Am. 2008;90(Suppl 4):121–132. doi: 10.2106/JBJS.H.00685. [DOI] [PubMed] [Google Scholar]
- 9.Luring C, Oczipka F, Grifka J, Perlick L. The computer-assisted sequential lateral soft-tissue release in total knee arthroplasty for valgus knees. Int Orthop. 2008;32:229–235. doi: 10.1007/s00264-006-0314-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yercan HS, Ait Si Selmi T, Sugun TS, Neyret P. Tibiofemoral instability in primary total knee replacement: a review, Part 1: Basic principles and classification. Knee. 2005;12:257–266. doi: 10.1016/j.knee.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Shakespeare D. Conventional instruments in total knee replacement: what should we do with them? Knee. 2006;13:1–6. doi: 10.1016/j.knee.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 12.Baldini A, Scuderi GR, Aglietti P, Chalnick D, Insall JN. Flexion-extension gap changes during total knee arthroplasty: effect of posterior cruciate ligament and posterior osteophytes removal. J Knee Surg. 2004;17:69–72. doi: 10.1055/s-0030-1248201. [DOI] [PubMed] [Google Scholar]
- 13.Matziolis G, Perka C. Primary resection of the posterior cruciate ligament does not produce a gap mismatch in the navigated gap technique. Orthopedics. 2010;33:68–70. doi: 10.3928/01477447-20100510-50. [DOI] [PubMed] [Google Scholar]
- 14.Amis AA, Gupte CM, Bull AM, Edwards A. Anatomy of the posterior cruciate ligament and the meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2006;14:257–263. doi: 10.1007/s00167-005-0686-x. [DOI] [PubMed] [Google Scholar]
- 15.Schnurr C, Nessler J, Konig DP. Is referencing the posterior condyles sufficient to achieve a rectangular flexion gap in total knee arthroplasty? Int Orthop. 2009;33:1561–1565. doi: 10.1007/s00264-008-0656-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chaiyakit P, Meknavin S, Hongku N. Effects of posterior cruciate ligament resection in total knee arthroplasty using computer assisted surgery. J Med Assoc Thai. 2009;92(Suppl 6):80–84. [PubMed] [Google Scholar]
- 17.Kadoya Y, Kobayashi A, Komatsu T, Nakagawa S, Yamano Y. Effects of posterior cruciate ligament resection on the tibiofemoral joint gap. Clin Orthop Relat Res. 2001;391:210–217. doi: 10.1097/00003086-200110000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Luring C, Hufner T, Perlick L, Bathis H, Krettek C, Grifka J. The effectiveness of sequential medial soft tissue release on coronal alignment in total knee arthroplasty: using a computer navigation model. J Arthroplasty. 2006;21:428–434. doi: 10.1016/j.arth.2005.05.031. [DOI] [PubMed] [Google Scholar]
- 19.Mihalko WM, Krackow KA. Posterior cruciate ligament effects on the flexion space in total knee arthroplasty. Clin Orthop Relat Res. 1999;360:243–250. doi: 10.1097/00003086-199903000-00029. [DOI] [PubMed] [Google Scholar]
- 20.Park SJ, Seon JK, Park JK, Song EK. Effect of PCL on flexion-extension gaps and femoral component decision in TKA. Orthopedics. 2009;32:22–25. doi: 10.3928/01477447-20090915-54. [DOI] [PubMed] [Google Scholar]
- 21.Mihalko WM, Whiteside LA, Krackow KA. Comparison of ligament-balancing techniques during total knee arthroplasty. J Bone Joint Surg Am. 2003;85(A Suppl 4):132–135. doi: 10.2106/00004623-200300004-00018. [DOI] [PubMed] [Google Scholar]
- 22.Jacobs WC, Clement DJ, Wymenga AB (2005) Retention versus sacrifice of the posterior cruciate ligament in total knee replacement for treatment of osteoarthritis and rheumatoid arthritis. Cochrane.Database.Syst.Rev.CD004803 [DOI] [PubMed]
- 23.Arbuthnot JE, Wainwright O, Stables G, Rathinam M, Rowley DI, McNicholas MJ (2010) Dysfunction of the posterior cruciate ligament in total knee arthroplasty. Knee.Surg.Sports Traumatol.Arthrosc. doi:10.1007/s00167-010-1234-x [DOI] [PubMed]
- 24.Maruyama S, Yoshiya S, Matsui N, Kuroda R, Kurosaka M. Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty. 2004;19:349–353. doi: 10.1016/j.arth.2003.09.010. [DOI] [PubMed] [Google Scholar]
- 25.Laskin RS. The Insall Award. Total knee replacement with posterior cruciate ligament retention in patients with a fixed varus deformity. Clin Orthop Relat Res. 1996;331:29–34. doi: 10.1097/00003086-199610000-00005. [DOI] [PubMed] [Google Scholar]