Abstract
Progressive hemifacial atrophy, also known as Parry-Romberg syndrome, is an uncommon degenerative condition which is poorly defined. It is characterized by a slow and progressive atrophy affecting one side of the face. The onset usually occurs during the first two decades of life. Characteristically, the atrophy progresses slowly for several years, and then it becomes stable. Ophthalmic involvement is common, with progressive enophthalmos which is a frequent finding. Cutaneous pigmentation is common in such conditions, however its extension to the conjunctiva is rarely reported. We report a case of Parry Romberg syndrome with characteristic clinical and radiographic presentation accompanied with rare ocular findings. The clinical features, radiological findings, and differential diagnoses to be considered, and the available treatment options are discussed in this report.
Keywords: Facial Hemiatrophy, Parry-Romberg Syndrome, Pigmentation, Conjunctiva
Parry-Romberg syndrome, also known as "progressive facial hemiatrophy", is characterized by a unilateral, progressive, but self-limited atrophy of skin and subcutaneous tissue of face.1 It is a rare, acquired, neurocutaneous syndrome of unknown aetiology accounting 1 in 700,000 individuals.2 This condition was first reported by an English physician, Caleb Parry, in 1815, and subsequently elaborated in 1846 by Moritz Romberg.2 This syndrome occurs more in women and is frequently limited to one side of the face and cranium; however it may occasionally spread to the neck and one side of the body.3 Ocular involvement is common and the most frequent manifestation is enophthalmos.4 Most of the patients present with cutaneous hyperpigmentation of the affected side,3 however the extension of pigmentation into the conjunctiva are rarely reported.
We here present an uncommon case of Parry-Romberg syndrome with classical features associated with hyperpigmentation of conjunctiva.
Case Report
A 16-year old male patient reported to the Department of Oral Medicine and Radiology with a complaint of progressive flattening of left side of face since the age of 2 years which was continuous to date. Patient gave a history of pigmentation of his left face since birth which had been gradually fading over the years. No history of trauma or surgery was reported and there was no positive family history of facial atrophy. Neither was there a family history of consanguinity. His delivery was not assisted, per vagina. The medical history was not contributory, and he was not on any form of medication. Patient denied history of smoking or alcohol intake. Patient was moderately built and nourished.
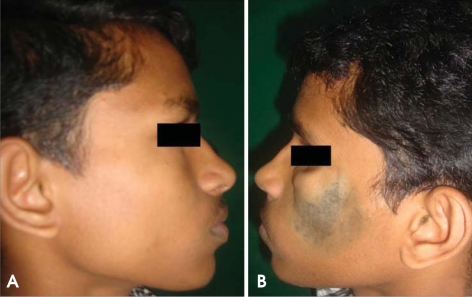
On physical examination, he was conscious, oriented, and afebrile. His general condition was fair with vital signs within normal limits. On extraoral examination, facial asymmetry was detected due to hypoplasia of left malar region (Fig. 1). There was atrophy of left masseter muscle and fat with prominence of the left infraorbital ridge and zygoma. The right face appeared normal. Examination of the face revealed no sensory or motor deficits on both sides. The left eye appeared depressed in the socket (enophthalmos) due to loss of periorbital fat with minimal drooping of the left eyelid (Figs. 2 and 3). Increased lacrimation was associated with enophthalmos. There was a deviation of mouth angle to the affected side at rest. Pigmentation was noticed on the left cheek which also involved the left palpebral conjunctiva (Fig. 4). Systemic examination of the central nervous system was normal. Fundus examination was also normal.
Fig. 1.
Clinical photograph of the patient shows marked hypoplasia of the left malar area with diffuse blackish pigmentation of the same region.
Fig. 2.
Photographs compare the normal and abnormal sides.
Fig. 3.
Photograph shows enophthalmos and flattening of zygomatic complex.
Fig. 4.
Photograph shows the pigmentation of the left palpebral conjunctiva.
Based on the clinical findings and history, a clinical diagnosis of Parry-Romberg syndrome was made. Routine blood investigations revealed all values within normal limits.
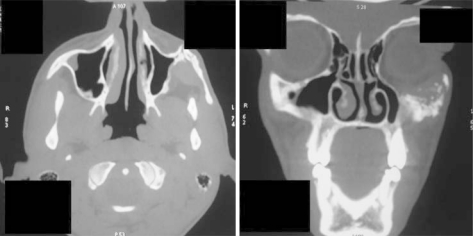
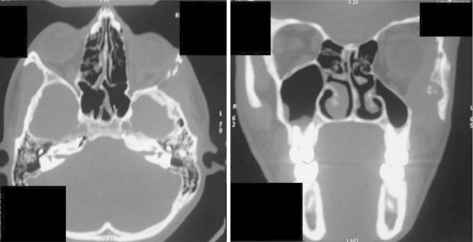
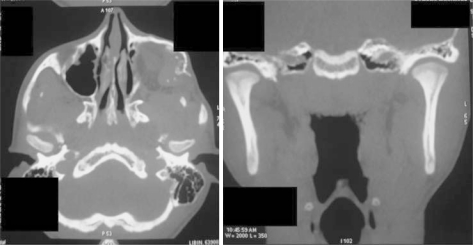
As a part of radiographic investigations, a panoramic radiograph was taken. The radiograph revealed no significant findings (Fig. 5). Axial and coronal computed tomographic (CT) images revealed hypoplasia of the left zygomatic complex, maxillary sinus, and lateral orbital wall. It also revealed left enophthalmos when levels of eyeballs were compared on the axial image (Figs. 6 and 7). Minimal condylar change was noted on the left side when compared to the right side (Fig. 8). Three-dimensional reconstruction CT image revealed deviated nasal septum, tilt in the occlusal table, and zygomatic complex, and hypoplastic orbital wall on the left side (Fig. 9).
Fig. 5.
Panoramic radiograph shows shorter crowns and roots of teeth on the left side compared with the right side.
Fig. 6.
Axial and coronal CT images reveal the hypoplastic left zygomatic complex and maxillary sinus.
Fig. 7.
Axial CT image shows the left eye ball at a lower level when compared to right side. Also observe the hypoplastic lateral orbital wall. Also coronal CT image reveals the shrunken left eyeball, hypoplastic maxillary sinus and lateral orbital wall.
Fig. 8.
Coronal and axial CT images show the minimal condylar changes on the right side compared with the left side.
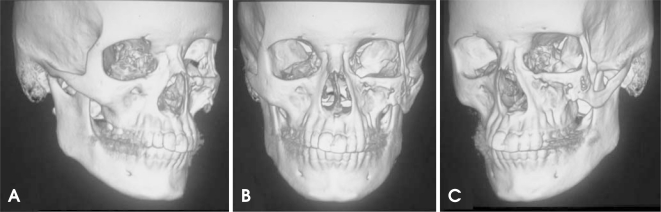
Fig. 9.
3D CT images show the normal anatomical features on the right side (A), deviated nasal septum and tilt in the occlusal table in the frontal view (B), hypoplastic zygomatic complex and orbital wall on left side (C).
Discussion
Progressive hemifacial atrophy is a rare pathology of unknown cause, whose degenerative condition affects the face unilaterally.1,3 It is characterized by a slow and progressive unilateral atrophy of the facial tissues including muscles, bones, and skin.1 The extension of atrophy is frequently limited to one side of the face, and the ipsilateral involvement of the body is rare (20% of cases were described as being bilateral).2 In the present case, there was involvement of only one side of the face. Clinically, the skin can be dry with a dark pigmentation.3 An early sign may be a well demarcated furrow on the forehead, which marks the boundary between the normal and atrophic tissue known as "coup de sabre" (French term which means "cut of the sword").4 This condition is found more often in female population and has predilection for the left side of the face,2 which is seen in the presented herein case. The disease manifests in the first or second decade of life with a slow progression over many years showing atrophy and then becomes stable.5 The etiology of the disease is unidentified. A cerebral disturbance on fat metabolism has been proposed as a primary cause.6 Trauma, viral infections, endocrine disturbances, auto-immunity, and heredity are also believed to be associated to the pathogenesis of the disease.7
Ocular involvement is common and the most frequent manifestation is the enophthalmos due to the fat loss around the orbit, as was observed in our patient. The eye usually works normally.1 Thinning of the ear due to atrophy of the fat around it and alopecia on the involved side are also frequent manifestations.1 Migraine and facial pain are the most common neurological symptoms in this patient group. Occasionally, epilepsy may occur and can sometimes be related directly to a brain abnormality ipsilateral to the skin lesion.2 However, these findings were not found in our case. Mouth and nose are deviated to the affected side, deviating also facial and dental midlines. Atrophy of the upper lip can lead the anterior teeth to be exposed.3 Atrophy of the tongue on the affected side is a consistent findings in patients with Parry-Romberg syndrome as mentioned by Pinheiro et al.3
Radiographically, the teeth of the patients with Parry-Romberg syndrome have short roots and appear small, when compared to the uninvolved side.3 Cranial CT and magnetic resonance image findings in Parry-Romberg syndrome are usually ipsilateral to the facial hemiatrophy, and intracranial calcifications as well as cerebral hypodensities are found.8 Occasionally, there may be some neurological complications, such as trigeminal neuralgia, facial paresthesia, severe headache, and contra lateral epilepsy. Contra lateral epilepsy is the most common complication as reported by Chbicheb et al.9
The treatment is usually based on the reposition of the atrophied adipose tissue. Autogenous fat grafts, cartilage grafts, silicon injections and prostheses, bovine collagen, and inorganic implants are some alternatives to the aesthetic correction of the atrophy.10 The treatment modalities mentioned, improve aesthetic appearance momentarily, whereas all the structure projected in the cosmetic surgery is lost with time, due to the gravity action, and the patient usually requires new intervention.3 Panfacial volumisation with autologous fat is an excellent tool for replacing volume and restoring contour to the aging face.11 Treatment using alloplastic implants was suggested to our patient to improve the facial appearance, however, this type of treatment was not performed due to financial and logistical reasons.
References
- 1.Stone J. Parry-Romberg syndrome. Pract Neurol. 2006;6:185–188. [Google Scholar]
- 2.Rangare AL, Babu SG, Thomas PS, Shetty SR. Parry-Romberg syndrome: a rare case report. J Oral Maxillofac Res. 2011;2:e5. doi: 10.5037/jomr.2011.2205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pinheiro TP, Silva CC, Silveira CS, Botelho PC, Pinheiro MG, Pinheiro Jde J. Progressive hemifacial atrophy - case report. Med Oral Patol Oral Cir Bucal. 2006;11:E112–E114. [PubMed] [Google Scholar]
- 4.Hakin KN, Yokoyama C, Wright JE. Hemifacial atrophy: an unusual cause of enophthalmos. Br J Ophthalmol. 1990;74:496–497. doi: 10.1136/bjo.74.8.496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar AA, Kumar RA, Shantha GP, Aloogopinathan G. Progressive hemi facial atrophy - Parry Romberg syndrome presenting as severe facial pain in a young man: a case report. Cases J. 2009;2:6776. doi: 10.4076/1757-1626-2-6776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller MT, Sloane H, Goldberg MF, Grisolano J, Frenkel M, Mafee MF. Progressive hemifacial atrophy (Parry-Romberg disease) J Pediatr Ophthalmol Strabismus. 1987;24:27–36. doi: 10.3928/0191-3913-19870101-07. [DOI] [PubMed] [Google Scholar]
- 7.Mazzeo N, Fisher JG, Mayer MH, Mathieu GP. Progressive hemifacial atrophy (Parry-Romberg syndrome). Case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;79:30–35. doi: 10.1016/s1079-2104(05)80069-1. [DOI] [PubMed] [Google Scholar]
- 8.Cory RC, Clayman DA, Faillace WJ, McKee SW, Gama CH. Clinical and radiologic findings in progressive facial hemiatrophy (Parry-Romberg syndrome) AJNR Am J Neuroradiol. 1997;18:751–757. [PMC free article] [PubMed] [Google Scholar]
- 9.Chbicheb M, Gelot A, Rivier F, Roubertie A, Humbertclaude V, Coubes P, et al. Parry-Romberg's syndrome and epilepsy. Rev Neurol. 2005;161:92–97. doi: 10.1016/s0035-3787(05)84980-x. [DOI] [PubMed] [Google Scholar]
- 10.de la Fuente A, Jimenez A. Latissimus dorsi free flap for restoration of facial contour defects. Ann Plast Surg. 1989;22:1–8. doi: 10.1097/00000637-198901000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Donofrio LM. Panfacial volume restoration with fat. Dermatol Surg. 2005;31:1496–1505. doi: 10.2310/6350.2005.31234. [DOI] [PubMed] [Google Scholar]