Abstract
The aim of the study was to determine the spatial distribution of methicillin-resistant Staphylococcus aureus [MRSA] at two marine and one fresh water recreational beaches in the Seattle area. Fifty-six marine water, 144 fresh water, and 96 sand samples were collected from June through August 2010. Isolates were biochemically verified as MRSA. Staphylococcal cassette chromosome mec (SCCmec) typing, multilocus sequence typing [MLST], pulse field gel electrophoresis [PFGE] and the presence of other antibiotic resistance genes were determined. Twenty-two fresh water [15.3%; n = 144], one dry sand [1.9%; n = 53], six wet sand [14%; n = 43], and 2 marine water samples [3.6%; n = 56] were MRSA positive. Of the 27 fresh water stream sites sampled multiple times, 37% of the sites were positive for MRSA and/or S. aureus ≥ 2 times. Twenty-one (67.7%) of 31 MRSA were SCCmec type IV, fifteen (48.4%) of the isolates had MLST types not previously associated with humans, and 29 (93.5%) of the isolates carried other antibiotic resistance genes. This study is the first to report and characterize repeated MRSA positive samples from fresh water drainages and creeks surrounding popular recreational beaches.
Keywords: MRSA, SCCmec type IV, S. aureus
Introduction
Community-acquired MRSA [CA-MRSA] has become a major cause of skin and soft tissue infection in the general population which do not have classic risk factors such as healthcare exposure (King et al., 2006) with the morbidity and mortality per 100,000 people estimated at 4.6 and 0.5, respectively (Klevens et al., 2007). Contact with seawater has been associated with a fourfold increase in the risk of S. aureus skin infections in children (Charoenca & Fujioka, 1995) suggesting that recreational marine beaches may be potential sources of MRSA exposure in the community. Several potential sources of S. aureus and MRSA contamination in the marine environment have been examined including shedding from recreational bathers, untreated wastewater, and urban runoff (Börjesson et al., 2009; Elmir et al., 2007; Plano et al., 2011; Selvakumar & Borst, 2006).
Over the past several years S. aureus and MRSA have been isolated from marine water, stream water, and intertidal sand samples from beaches in California (Goodwin & Pobuda 2009), Florida (Abdelzaher et al., 2010), Hawaii (Tice et al., 2010; Viau et al., 2011) and the Pacific Northwest (Soge et al., 2009). MRSA spatial distribution or strain characterization was not addressed in the studies by Goodwin & Pobuda (2009) in California and Tice et al. (2010) in Hawaii. A more recent study sampled fresh water streams draining into coastal beaches on O'ahu Hawaii found that 63.6% of the stream water sites [n = 22] repeatedly sampled were positive for S. aureus (Viau et al., 2011). Temporal and spatial distribution of pathogenic microorganisms including S. aureus was examined in a Florida study (Abdelzaher et al., 2010), however none of the presumptive S. aureus isolates were biochemically confirmed as S. aureus. The study by Soge et al. (2009) identified MRSA and/or S. aureus from six of ten marine beaches from the Pacific Northwest, however the number of samples taken was limited. That study found that the MRSA isolates were related to strains previously associated with hospital-acquired MRSA, and the S. aureus isolates were related to widespread clones.
In the current study we conduct multiple sampling of two marine water beaches and one fresh water beach in the Seattle metro area to assess the spatial distribution of MRSA between June and August 2010. All MRSA isolates were molecularly characterized using SCCmec typing, pulse field gel electrophoresis [PFGE], and multilocus sequence typing [MLST] to determine the potential sources of the isolates.
Materials and Methods
Site Descriptions
Water and sand samples were collected from two marine water beaches [A and B] and one freshwater beach [C] in the Seattle WA area. Marine beach A is a public beach located in a 0.36 km2 park along the east side of the Puget Sound. The marine water on beach A is the receiving water for several upland drainage streams and a natural creek that traverse a steep slope boarding the beach to the west. At the top of this slope is an 8,903 m2 off-lease dog park and immediately south of the beach is a full-service marina and boat launch. There are two combined sewer overflows [CSO] one 1.6 km south of beach A and one between Beach A and Beach B. Marine beach B, 3 km north of beach A, is also a public beach located in a 0.9 km2 park and is the receiving water for a natural stream, a county CSO, and a pump station. Despite the numerous potential point and non-point source of fecal contamination, beaches A and B have been compliant with seasonal regulatory monitoring criteria for enterococci from 2004 –2010 (WA Dept. of Ecology, 2011). Beach C is a fresh water beach located on the west side of Lake Washington in an 89,031 m2 park. This beach is the receiving point in Lake Washington for a natural creek and a county CSO. Beach C intermittent high fecal coliform counts are believed to be caused by bacterial contamination from the natural creek. During summer 2010, beach C did not exceed seasonal regulatory monitoring criteria for fecal coliform counts (King County, 2011).
Sample Collection
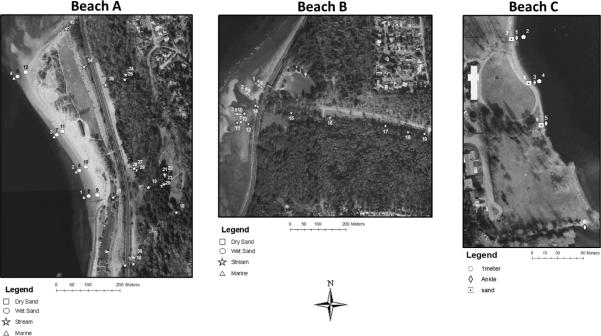
A total of 296 samples of marine water [n = 56], fresh water from the drainage and natural creeks at beaches A and B and Lake Washington water at beach C [n = 144], and sand samples [n = 96] were collected from June 24 to August 31, 2010 (Table 1). The MRSA distribution over time was assessed by repeatedly sampling 30 sites over 6 sampling events, 19 sites over 4 sampling events, and 9 sites over 3 sampling events from beach A, B and C, respectively (Table 1, Figure 1). Differences in the number of sampling events at the three sites, was due to additional convenient sampling at site A. For beaches A and B, marine water samples were taken at ankle level [5 cm] at regular intervals along the beach. Wet sand samples from the water line and dry sand samples from the high tide line were collected along a vertical transect from the location of the marine water sample collection. The locations of the wet and dry samples varied based on the tideline, however, the location of the vertical transect was consistent between sampling events. Fresh water samples from the natural stream and various drainage points were also collected. From beach C, water samples were taken at 5 cm and 1-meter deep depths and sand was collected along a horizontal mid-beach transect. Water and sand samples were collected in sterile 1-L bottles and 50 ml tubes, respectively, stored at 4 °C and processed within 24 h of collection.
Table 1.
Sampling distribution of water and sand samples in Beach A, B and C.
| Water |
Sand |
|||||
|---|---|---|---|---|---|---|
| No. of Sampling Events | Marine | Fresha | Wetb | Dryc | Total | |
| Beach A | 6 | 38 | 87 | 24 | 27 | 176 |
| Beach B | 4 | 18 | 37 | 19 | 15 | 89 |
| Beach C | 3 | NAd | 20 | 0 | 11 | 31 |
|
| ||||||
| Total | 13 | 56 | 144 | 43 | 53 | 296 |
For beaches A and B, fresh water refers to samples collected from natural streams and drainage points. For beach C, fresh water refers to samples collected from Lake Washington.
Wet: sand collected along the water line
Dry: sand collected along the hightide line
NA: not applicable.
Figure 1.
Fresh water, marine water and sand sampling locations and numeric designation of sites repeatedly surveyed between June and August, 2010 at beaches A, B, and C. Aerial photography courtesy of the City of Seattle [1993].
Sample Processing
Prior to processing, marine, and fresh water samples were vigorously shaken for 30 sec and a 25 ml sample transferred to a sterile glass bottle. Water samples were diluted 1:1 with 1.5× Bacto® m Staphylococcus broth (Difco Laboratories, Becton Dickinson & Co, Sparks, MD, USA), supplemented with a final concentration of 75 μg mL−1 polymyxin B (Sigma, St. Louis, MO, USA), and 0.01% potassium tellurite (Sigma). For each sand sample, 10 g [wet weight] was transferred to a sterile 50 ml tube. Twenty-five mL of supplemented 1.0× m Staphylococcus broth was added to the sand samples, vigorously shaken for 2 min, and decanted into a sterile glass bottle. After initial processing, both water and sand broth mixtures were incubated at 36.5 °C with 5% CO2 until the samples became turbid with black precipitate indicating Staphylococcus spp. growth (Soge et al., 2009). Samples that were not turbid or did not have a black precipitate were considered negative for Staphylococcus spp. after 7 days. Sampling events on August 2 [marine water n = 4; fresh water n = 21] and August 30 [marine water n = 4; fresh water n = 18; dry sand n = 4; wet sand n = 4] for beach A and July 22 [marine water n = 3; fresh water n = 9; wet sand n = 4; dry sand n = 3] fresh water and for August 16 [marine water n = 3; fresh water n = 8; wet sand n = 4; dry sand n = 3] for beach B, were quantified using the most-probable number [MPN] technique as previously described (Levin-Edens et al., 2011a).
S. aureus and MRSA Biochemical Verification
Positive enrichments were serially diluted and plated onto Mannitol Salt Agar (Difco) and incubated at 36.5 °C with 5% CO2 for 48 h. Yellow colonies from the Mannitol Salt Agar were considered presumptive positive for S. aureus and a maximum of 10 yellow colonies were streaked on to Brucella agar (Difco) supplemented with 5% sterile sheep blood to test for β-hemolysis. Positive isolates were coagulase tested using the Remel Staphaurex rapid latex kit (Thermo Fisher Scientific Remel Products, Lenexa, KS, USA). Isolates that were both β-hemolytic and coagulase positive were confirmed S. aureus and subsequently streaked onto Bacto® Staphylococcus Medium 110 (Difco) supplemented with 0.01% potassium tellurite and 10 μg mL−1 methicillin (Sigma) and incubated at 36.5 °C with 5% CO2 for a maximum of seven days to screen for MRSA. β-hemolytic, coagulase-positive S. aureus that grew on Bacto® Staphylococcus Medium 110 supplemented with methicillin were considered presumptive MRSA and the presence of the mecA gene was determined by PCR (see next section). For the sampling events that were quantitatively processed, presumptive MRSA isolates were isolated as previously described (Levin-Edens et al., 2011).
PCR Assay for mecA, SCC mec Typing, Multilocus Sequence Typing [MLST], and Pulse Field Gel Electrophoresis [PFGE]
All presumptive MRSA isolates were confirmed using a mecA PCR assay, as previously described (Soge et al., 2009). Isolates that were mecA negative were labeled S. aureus. SCCmec typing was done as previously described by multiplex PCR assay for types I – V using positive controls (Soge et al., 2009). Isolates that were negative were categorized as non-typeable [NT]. MLST was determined with previously described primers and PCR conditions for seven housekeeping genes: arc, carbamate kinase; aro, shikimate dehydrogenase; glp, glycerol kinase; gmk, guanylate kinase; pta, phosphate acetyltransferase; tpi, triosephosphate isomerase; and ygi, acetyl coenzyme A acetyltransferase (Enright et al., 2000), and bi-directionally sequenced at the University of Washington High Throughput Sequencing Facility. For each locus, alleles were characterized based on comparison with previously described alleles in the S. aureus MLST database (www.mlst.net). New alleles were confirmed unique by bi-directionally re-sequencing three times and assigned a new identification number and new MLST type.
Nineteen selected isolates were analyzed by PFGE and the 14 different PFGE patterns were labeled A – N as previously described (Soge et al., 2009). Isolates were considered to be identical if the banding patterns differed by ≤ 3 bands (Roberts et al., 2009). The percent similarity of each isolate analyzed by PFGE was compared against a clinical USA300 control strain to calculate the percent similarity using UPGMA method and DICE cluster analysis on GelComprII software (Applied Maths, Inc., Austin, TX, USA). PCR assays for tetracycline resistance genes, tet(M), tet(K), and macrolide resistance genes erm(A), erm(B) and erm(C), and msr(A) were done as previously described (Soge et al., 2009). The presence of the aminoglycoside resistance gene aadD was assayed by PCR assay as previously described (van Asselt et al., 1992).
Statistical Analysis
The chi-squared test was used to test the strength of association between sample type and MRSA and was calculated in Stata11 I.C (StataCorp LP, College Station, TX, USA). P < 0.05 was considered statistically significant.
Results
MRSA and S. aureus Distribution and Quantification
From the 296 water and sand samples collected, 31 [10.4%] samples were MRSA positive (Table 2). For marine beaches A and B, fresh water refers to samples collected from natural streams and drainage points. The highest percentage of MRSA positive samples [19.4%] was from the fresh water recreational beach, while the marine beaches ranged between 7.9% and 11.4%. Twenty-two [15.3%] of the 144 fresh water samples, one [1.9%] of the 53 dry sand, six [14%] of the 43 wet sand, and two [3.6%] of the 56 marine water samples were MRSA positive. MRSA was dependent on sample type and fresh water and wet sand samples were the most frequently contaminated [P = 0.01]. Twenty MRSA strains were isolated from beach A and were from sand [n = 4], marine water [n = 2] and fresh water [n = 14]. All five of the MRSA isolates were isolated from fresh water samples from beach B. Six MRSA isolates were found from sand [n = 3] and from the fresh lake water [n = 3] from beach C. This study was focused on the identification of MRSA and as a result most likely underestimated the frequency and distribution of S. aureus in the three recreational beaches surveyed.
Table 2.
Overall distribution of MRSA and S. aureus isolates by beach and sample type.
| No. Samples | No. MRSA | % MRSA [95% CI] | No. S. aureus | % S. aureus [95% CI] | ||
|---|---|---|---|---|---|---|
| Beach | A | 176 | 20 | 11.4 [6.7 – 16.1] | 9 | 5.1 [1.9 – 8.4] |
| B | 89 | 5 | 5.6 [0.8 –10.4] | 5 | 5.6 [0.8 – 10.4] | |
| C | 31 | 6 | 19.4 [5.4 – 33.3] | 0 | 0 | |
|
| ||||||
| Water | Marine | 56 | 2 | 3.6 [0.0 – 8.4] b | 1 | 1.8 [0.0 – 5.3]b |
| Fresha | 144 | 22 | 15.3 [9.4 – 21.2] | 12 | 8.3 [3.8 – 12.8] | |
| Sand | Dry | 53 | 1 | 1.9 [0.0 – 5.5]b | 1 | 1.0 [0.0 – 3.1]b |
| Wetb | 43 | 6 | 14.0 [3.6 – 24.3] | 0 | 0 | |
|
| ||||||
| Total | 296 | 31 | 10.5 [7.0 – 14.0] | 14 | 4.7 [2.3 – 7.1] | |
MRSA: methicillin-resistant Staphylococcus aureus; MRSA isolates are mecA positive; S. aureus isolates are mecA negative.
Fresh water refers to water collected from the streams and drainage points on beaches A and B and lake water collected from beach C.
Wet sand includes sand collected at the waterline at marine beaches A [n = 3] and sand collected from fresh water beach C [n = 3].
Lower 95% confidence interval truncated at 0.0.
Ninety-two samples, 55 samples from beach A [August 2 and 30] and 37 samples from beach B [July 22 and August 16], were quantitatively processed. Six [6.5%] of the samples were positive for MRSA and as defined by a positive mecA PCR assay with the median MRSA MPN 100 mL−1 of 3.5 with a range between 2.0 and 66.2 MPN 100 mL−1.
Fourteen [4.7%] of the 296 samples were S. aureus positive, nine from marine beach A and five from marine beach B. This included one [1.8%] S. aureus positive marine water sample, one [1.9%] S. aureus positive dry sand sample and 12 [9.7%] S. aureus positive samples from the fresh water streams draining into the marine beaches. No S. aureus samples were identified from the fresh water beach C (Table 2).
Sites Repeatedly Sampled for MRSA and/or S. aureus
There were 30 marine water, fresh water, and sand sampling sites on beach A, 19 marine water, fresh water, and sand sampling sites on beach B, and nine fresh water and sand sites from beach C that were repeatedly sampled during six, four and three sampling events, respectively. On beach A, two marine water sites [sites 2 and 4] and three sand sites [sites 6, 2, 11] were MRSA or S. aureus positive once. There was no positive marine water or sand sites for beach B. In contrast, there were 27 fresh water stream sites samples repeatedly from marine beaches A and B of which ten (37%) sites, six on beach A [sites 16, 17, 27, 28, 29 and 30] and four [sites 12, 14, 17, and 19] on beach B, were MRSA or MRSA/ S. aureus positive between two and four different sampling events. Of the six fresh water sites and three sand sites repeatedly sampled at beach C, one sand site was MRSA positive twice [site 7] and three sites [sites 1,4 and 5] were MRSA positive once over the three sampling events (Figure 1 and 2).
Figure 2.
Distribution of methicillin-resistant S. aureus [MRSA] and methicillin-susceptible S. aureus [MSSA] isolates in beaches A, B and C. Site numbering corresponds to Figure 1. Sites positive for MRSA/MSSA ≥2 days are sites 16, 17, 27, 28, 29, and 30 for beach A, sites 12, 14, 17, and 19 for beach B, and site 7 for beach C.
MRSA Molecular Characterization
Thirty-one MRSA isolates were characterized and included 21 isolates that were SCCmec type IV [67.7%], three were SCCmec type I [9.7%], one was SCCmec type II [3.2%], and six were NT [18.2%]. All nine MRSA strains isolated from marine [n = 1] and sand [n = 8] samples were SCCmec type IV, while the 22 fresh water samples were a mixture of SCCmec type IV [n = 12], SCCmec type I [n = 3], SCCmec type II [n = 1], and SCCmec type NT [n = 6] (Table 3). None of the SCCmec type IV isolates were related to USA300, the most common CA-MRSA strain associated with outbreaks in the USA, by PFGE [homologies < 50%; data not shown].
Table 3.
Genotypic characterization of 31 MRSA isolates collected during summer 2010.
| Date | Isolate | Sample Type | Sitea | SCCmec Typeb | MLSTc | PFGE Type | Genotype | |
|---|---|---|---|---|---|---|---|---|
| Beach A [n = 20 strains] | 24Jun | 111 | Sand | 11 | IV | 8 | K | erm(C), msr(A), aadD |
| 118 | Fresh | NA | IV | 15 | tet(M), tet(K), erm(C), msr(A), aadD | |||
| 125 | Fresh | NA | IV | 133 | C | tet(K), erm(C), msr(A), aadD | ||
| 07Jul | 302 | Marine | NA | IV | 109 | F | tet(M), tet(K), erm(A), msr(A), aadD | |
| 308 | Marine | 2 | IV | 109 | F | tet(M), erm(A), erm(C), msr(A), aadD | ||
| 361 | Sand | 11 | IV | 109 | F | tet(M), erm(A), erm(C), msr(A), aadD | ||
| 08Jul | 401 | Fresh | NA | IV | 5 | L | tet(M), tet(K), erm(C), msr(A), aadD | |
| Seep1 | Sand | NA | IV | 88 | tet(M), tet(K), msr(A), aadD | |||
| 3mid | Sand | NA | IV | 15 | G | tet(M), tet(K), msr(A), aadD | ||
| 12Jul | 512 | Fresh | 27 | IV | 133 | E | tet(K), erm(C), msr(A), aadD | |
| 515 | Fresh | 28 | IV | 1875 | tet(K), erm(C), msr(A), aadD | |||
| 526 | Fresh | 30 | IV | 1875 | tet(M), tet(K), msr(A), aadD | |||
| 19Jul | 813 | Fresh | 17 | IV | 1875 | tet(M), tet(K), erm(C), msr(A), aadD | ||
| 823 | Fresh | 27 | NT | 1875 | tet(M), tet(K), erm(C), msr(A), aadD | |||
| 824 | Fresh | 28 | NT | 133 | tet(K), erm(C), msr(A), aadD | |||
| 827 | Fresh | 30 | IV | 1956 | I | tet(K), erm(C), msr(A), aadD | ||
| 02Aug | 1112 (1) | Fresh | 16 | I | 133 | B | none | |
| 1112 (2) | Fresh | 16 | II | 45 | M | erm(A), aadD | ||
| 1113 | Fresh | 17 | I | 1956 | J | none | ||
| 1124 | Fresh | 28 | I | 1956 | aadD | |||
|
| ||||||||
| Beach B [n =5 | 02Jul | 252 | Fresh | 19 | IV | 133 | B | tet(K), erm(C), msr(A), aadD |
| 11Jul | PC3 | Fresh | NA | NT | 6 | tet(M), tet(K), msr(A), aadD | ||
| 22Jul | 1012 | Fresh | 12 | NT | 6 | tet(M), tet(K), msr(A), aadD | ||
| 1017 | Fresh | 17 | NT | 2049 | erm(C), aadD | |||
| 1019 | Fresh | 19 | NT | 2049 | tet(K), erm(C), msr(A), aadD | |||
|
| ||||||||
| Beach C [n = 6 strains] | 01Jul | 244 | Fresh | 1 | IV | 133 | A | erm(C), msr(A), aadD |
| 248 | Fresh | 4 | IV | 133 | A | tet(K), msr(A), aadD | ||
| 257 | Sand | 7 | IV | 97 | N | tet(K), erm(C), msr(A), aadD | ||
| 14Jul | 603 | Sand | 7 | IV | 30 | H | tet(M), tet(K), erm(C), msr(A), aadD | |
| 21Jul | 909 | Fresh | 5 | IV | 133 | D | tet(K), erm(C), msr(A), aadD | |
| 910 | Sand | 9 | IV | 133 | D | tet(K), erm(C), msr(A), aadD | ||
Isolates with the same SCCmec type, MLS and PFGE type were considered to be genetically related and based on these the 31 isolates represent 21 different strains
Site number corresponds with figure 1; NA: not applicable
SCCmec type: I – V, NT [non-typable]. No SCCmec type IV related to USA300 [homology < 50%]
MLST type determined by the allelic profile of seven housekeeping gene arc, aro, glp, gmk, pta, tpi, and ygi.
ST5, ST6, ST8, ST15, ST30, ST45, ST88, ST97, ST109 have all been found in humans and animals; ST133 has been found in livestock; ST1956 has been found in squirrels; ST1875 and ST2049 are new MLST types isolated in the study.
Fourteen different MLST types were identified including two new ST types, ST1875 and ST2049. Five of the ST types were found once [ST 8, 30, 45, 88 and 97], while ST133 was identified from five different fresh water samples from marine beach A [n = 4] and beach B [n = 1] and three fresh water samples and one sand sample from beach C (Table 3). Eighteen (58.1%) of the isolates were ST types that had not been previously associated with humans including ST133 [n = 9] which have previously been isolated in cows, sheep, and goats (Smyth et al., 2009), ST1956 [n = 3] isolated from squirrels [www.mlst.net] and the new ST1875 [n = 4] and ST2049 [n = 2] (Table 3).
Fourteen distinct PFGE patterns [A-N] were identified from the 19 isolates analyzed. Nine isolates represented four PFGE groups (patterns A, B, D, and F) with each group having the same ST type and identical or very similar combination of antibiotic resistance genes (Table 3). Among the ST133 isolates, three isolates [125, 512, and 824] gave different PFGE patterns and carried a different number and combination of the antibiotic resistance genes. Isolates 909 and 910, isolated from different samples taken the same day, had indistinguishable PFGE patterns (D), were SCCmec IV and carried the same antibiotic resistance genes were most likely genetically related. Isolates 244 and 248 carried SCCmec type IV, had a common PFGE pattern (A) and had similar but not identical antibiotic resistance genes and may be related to each other but not the other ST133 isolates in the study. The isolates 1112(1) and 252, both ST133 had indistinguishable PFGE pattern (B), but carried different SCCmec elements (I vs IV) and different antibiotic resistance gene carriage patterns. Both isolates were from the fresh water samples isolated in beach A in August [1112(1)] and beach B in July [252] however their genetic relationship to each other is unclear.
MRSA isolates 308 and 361, isolated from marine water on beach A on the same date from different samples, have the same ST type, carry SCCmec type IV, had a common PFGE pattern (F), and carried the same combination of other antibiotic resistance genes. Thus they most likely represent a single strain. The isolate 302 collected from sand on beach A on the same date as isolates 308 and 361, was also ST109, SCCmec type IV and PFGE pattern F, but differed in some of the antibiotic resistance genes carried. These three isolates most likely are genetically related and represent a single clone.
In addition to ST133 and ST109, four MRSA isolates collected from beach A on two different dates were ST1875, SCCmec type IV, and carried identical or very similar antibiotic resistance genes. Isolates 1012 and PC3, isolated on different dates from beach C, were both SCCmec NT and ST6 with the same antibiotic resistance gene combination. Two MRSA isolates collected from beach B on the same date from two different fresh water sites carried the new MSLT ST2049 and SCCmec NT and may be genetically related. One fresh water sample from beach A had 2 different MRSA strains isolated, 1112(1) and 1112(2), which differed in all measured characteristics and were genetically unrelated (Table 3).
Twenty-nine (93.5%) of the MRSA strains carried ≥ 1 of the other antibiotic resistance genes with 24 (77.4%) carrying one or both of the tetracycline resistance genes [tet(K), tet(M)]; 28 (90.3%) carrying ≥ 1 of the macrolide resistance genes [erm(A), erm(C), msr(A)] and 29 (93.5%) carrying the aminoglycoside resistance gene [aadD] (Table 3).
Discussion
In the current study, 31 MRSA isolates were characterized with the majority (71%) isolated from the fresh water drainages and creeks surrounding marine beach A and B and/or fresh water beach C. The concentration of MRSA in the positive samples ranged from 2.0–66.2 MPN 100 mL−1, however, the level of risk to beach visitors at these levels are unknown. In addition, 37% of the fresh water sites at beach A and B sampled repeatedly were positive for MRSA and/or MRSA/S. aureus ≥ 2 times. There was no clear indication why these sites were consistently positive compared to other fresh water sites that were positive once for MRSA and S. aureus negative. Fresh water drainages sites were not sampled in our previous study (Soge et al., 2009) or in most other studies making it difficult to directly compare the current study to these studies (Abdelzaher et al., 2010; Goodwin & Pobuda, 2009; Tice et al., 2010). The recent study by Viau et al. (2011) repeatedly surveyed fresh water drainage sites from O'ahu and found that 14 [64%] of 22 streams were positive for S. aureus at least twice but only one [4.5%] of the 22 sites was MRSA positive from the December sampling. Differences of MRSA detection frequency between the Viau et al., 2011 study and the current study may be due to differences in sampling frequency, isolation methodology, and/or extrinsic factors such as water and air temperature differences found between Hawaii and Washington State.
Based on the combination of the SCCmec type, MLST type, and PFGE pattern the 31 MRSA isolates most likely represent 21 different strains. Some of the related isolates from a single strain were isolated from different samples on the same day, collected on different days and/or identified on different beaches suggesting that certain strains persisted in this environment. These results support our sterile laboratory microcosm studies which found that MRSA had a 1-log drop at 5–10 days in both marine and fresh water at 13 °C (Levin-Edens et al., 2011b). It is also possible that some of these strains, such as ST133 are widely distributed because they are associated with the wildlife found in this urban environment.
In the current study MRSA isolates were more often (67.7%) SCCmec IV, while in our previous study 83.3% of the isolates were SCCmec type I (Soge et al., 2009). This difference could be due to small sample sizes in the first study, changes to the community/environmental MRSA between 2008 and 2010, or the addition of fresh water samples in the current study which yield the majority [71%] of the MRSA isolates in the current study. The high prevalence of SCCmec type IV was also found in a recent study that found the SCCmec type IV predominated among MRSA from untreated wastewater (Börjesson et al., 2009). MRSA isolates from other recreational beaches studies have not been molecularly characterized and it is therefore difficult to know how the MRSA strains in the current study compare to other locations such as California and Hawaii (Goodwin & Pobuda 2009; Tice et al., 2010) where the beach environment is significantly warmer than in the Washington State. Characterization of MRSA from recreational beach environments from a variety of geographical locations is needed to verify whether the MRSA distribution and strains found in the Pacific Northwest is representative of the broader environment.
Two novel MLST types ST1875 and ST2049 were identified from samples taken from fresh water drainage and creek samples at beaches A and B. Including the novel ST types, > 50% of the isolates have not been previously associated with humans (Smyth et al., 2009; www.mlst.net). It was of interest that the most common ST type was ST133 which have been previously associated with cows, sheep and goats, animals not normally part of the Seattle urban environment. However, it is possible that MRSA ST133 is adaptive to wildlife such as squirrels or seagulls and/or with other unknown environmental reservoirs. Three isolates with ST1959 were taken from beach A, and have been previously found in squirrels from the UK and all three beaches have indigenous squirrel populations. The remaining isolates have been previously found in humans (ST109), humans and animals (ST15, ST45, ST88, ST97), or humans and meat products (ST5, ST6, ST8, ST30) (Armand-Lefevre et al., 2005; Boyl-Vavra and Daum 2010; Collery et al., 2008; Cuny et al., 2010; Deleo et al., 2010; Graveland et al., 2010; Hata et al., 2010; Kawaguchiya et al., 2011; Lin et al., 2011; Waters et al., 2011).
This study found MRSA most often contaminating samples of fresh water streams running into the marine beaches where we frequently observed children playing during sampling and at the fresh water beach on Lake Washington. The diversity of MRSA isolates found in this study concurs with the previous hypothesis that MRSA is increasingly disseminated throughout the environment via multiple different potential sources including humans and wildlife (Seifried et al., 2007).
This study is the first to isolate and molecularly characterize repeated MRSA positive samples from fresh water drainages and creeks surrounding popular recreational marine beaches and from a fresh water recreational beach. Approximately half of the MRSA strains from the study have MLST types traditionally associated with humans and the remaining associated with animal sources suggesting multiple reservoirs may be important in the Pacific Northwest. The distribution of MLST types may have important implications for recreational beach visitors in colder climates Further studies are needed to determine the source of MRSA contamination and potential differences in reservoirs for MRSA in colder vs warmer climates for both marine and fresh water beaches.
References
- Abdelzaher AM, Wright ME, Ortega C, Solo-Gabriele HM, Miller G, Elmir S, Newman X, Shih P, Bonilla JA, Bonilla TD, Palmer CJ, Scott T, Lukasik J, Harwood VJ, McQuaig S, Sinigalliano C, Gidley M, Plano LR, Zhu X, Wang JD, Fleming LE. Presence of pathogens and indicator microbes at a non-point source subtropical recreational marine beach. Appl Environ Microbiol. 2010;76:724–732. doi: 10.1128/AEM.02127-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armand-Lefevre L, Ruimy R, Andremont A. Clonal comparison of Staphylococcus aureus isolates from healthy pig farmers, human controls, and pigs. Emerg Infect Dis. 2005;11:711–714. doi: 10.3201/eid1105.040866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Börjesson S, Matussek A, Melin S, Löfgren S, Lindgren PE. Methicillin-resistant Staphylococcus aureus (MRSA) in municipal wastewater: an uncharted threat? J Appl Microbiol. 2009;108:1244–1251. doi: 10.1111/j.1365-2672.2009.04515.x. [DOI] [PubMed] [Google Scholar]
- Boyl-Vavra S, Daum RS. Reliability of the BD GeneOhm methicillin-resistant Staphylococcus aureus (MRSA) assay in detecting MRSA isolates with a variety of genotypes from the United States and Taiwan. J Clin Microbiol. 2010;48:4546–4551. doi: 10.1128/JCM.02519-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collery MM, Smyth DS, Twohig JM, Shore AC, Coleman DC, Smyth CJ. Molecular typing of nasal carriage isolates of Staphylococcus aureus from an Irish university student population based on toxin gene PCR, agr locus types and multiple locus, variable number tandem repeat analysis. J Med Microbiol. 2008;57:348–358. doi: 10.1099/jmm.0.47734-0. [DOI] [PubMed] [Google Scholar]
- Cuny C, Friedrich A, Kozytska S, Layer F, Nübel U, Ohlsen K, Strommenger B, Walther B, Wieler L, Witte W. Emergence of methicillin-resistant Staphylococcus aureus (MRSA) in different animal species. Int J Med Microbiol. 2010;300:109–117. doi: 10.1016/j.ijmm.2009.11.002. [DOI] [PubMed] [Google Scholar]
- Charoenca N, Fujioka RS. Assessment of Staphylococcus bacteria in Hawaii recreational waters. Water Sci Technol. 1995;31:11–17. [Google Scholar]
- Deleo FR, Otto M, Kreiswirth BN, Chambers HF. Community-associated methicillin-resistant Staphylococcus aureus. Lancet. 2010;375:1557–1568. doi: 10.1016/S0140-6736(09)61999-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elmir SM, Wright ME, Abdelzaher A, Solo-Gabriele HM, Fleming LE, Miller G, Rybolowik M, Peter Shih MT, Pillai SP, Cooper JA, Quaye EA. Quantitative evaluation of bacteria released by bathers in marine water. Water Res. 2007;41:3–10. doi: 10.1016/j.watres.2006.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enright MC, Day NPJ, Davies CE, Peacock SJ, Spratt BG. Multilococus sequence typing for characterization of methicillin-resistant and methicillin-susceptible clones of Staphylococcus aureus. J Clin Microbiol. 2000;38:1008–1015. doi: 10.1128/jcm.38.3.1008-1015.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin KD, Pobuda M. Performance of CHROMagar Staph aureus and CHROMagar MRSA for detection of Staphylococcus aureus in seawater and beach sand – Comparison of culture, agglutination, and molecular analysis. Water Res. 2009;43:4802–4811. doi: 10.1016/j.watres.2009.06.025. [DOI] [PubMed] [Google Scholar]
- Graveland H, Wagenaar JA, Heesterbeek H, Mevius D, van Duijkern E, Heederik D. Methicillin resistant Staphylococcus aureus ST398 in veal calf farming: human MRSA carriage related with animal antimicrobial usage and farm hygiene. PLoS One. 2010;5:e10990. doi: 10.1371/journal.pone.0010990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hata E, Katsuda K, Kobayashi H, Uchida I, Tanaka K, Eguchi M. Genetic variation among Staphylococcus aureus strains from bovine milk and their relevance to methicillin-resistant isolates from humans. J Clin Microbiol. 2010;48:2130–2139. doi: 10.1128/JCM.01940-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawaguchiya M, Urushibara N, Kuwahara O, Ito M, Mise K, Kobayashi N. Molecular characteristics of community-acquired methicillin-resistant Staphylococcus aureus in Hokkaido, northern main island of Japan: Identification of sequence types 6 and 59 Panton-Valentine leucocidin-positive community-acquired methicillin-resistant Staphylococcus aureus. Microb Drug Resist. 2011;17:241–251. doi: 10.1089/mdr.2010.0136. [DOI] [PubMed] [Google Scholar]
- King MD, Humphrey BJ, Wang YF, Kourbatova EV, Ray SM, Blumberg HM. Emergence of community-acquired methicillin-resistant Staphylococcus aureus USA 300 clone as the predominant cause of skin and soft-tissue infections. Ann Intern Med. 2006;144:309–17. doi: 10.7326/0003-4819-144-5-200603070-00005. [DOI] [PubMed] [Google Scholar]
- King County Swimming Beach Monitoring. http://green.kingcounty.gov/swimbeach/BeachData.aspx?locator=0818SB&CurrentYear=tre (viewed on April 30, 2011)
- Klevens RM, Morrison MA, Nadle J, Petit S, Gersham K, Ray S, Harrison LH, Lynfield R, Dumyati G, Townes JM, Craig AS, Zell ER, Fosheim GE, McDougal LK, Carey RB, Fridken SK. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–1771. doi: 10.1001/jama.298.15.1763. [DOI] [PubMed] [Google Scholar]
- Levin-Edens E, Meschke JS, Roberts MC. Quantification of methicillin-resistant Staphylococcus aureus (MRSA) using most probable number (MPN) in marine and fresh waters samples. Appl Environ Microbiol. 2011a;77:3541–3543. doi: 10.1128/AEM.00015-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levin-Edens E, Bonilla N, Meschke JS, Roberts MC. Survival of environmental and clinical strains of methicillin-resistant Staphylococcus aureus [MRSA] in Pacific Northwest and fresh waters. Water Res. 2011b;45:5681–5686. doi: 10.1016/j.watres.2011.08.037. [DOI] [PubMed] [Google Scholar]
- Lin Y, Barker E, Kislow J, Kaldhone P, Stemper ME, Pantrangi M, Moore FM, Hall M, Fritsche TR, Novicki T, Foley SL, Shukla SK. Evidence of multiple virulence subtypes in nosocomial and community-associated MRSA genotypes in companion animals from the upper Midwestern and northeastern United States. Clin Med Res. 2011;9:7–16. doi: 10.3121/cmr.2010.944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Plano LRW, Garza AC, Shibata T, Elmir SM, Kish J, Sinigalliano CD, Gidley ML, Miller G, Withum K, Fleming LE, Solo-Gabriele HM. Shedding of Staphylococcus aureus and methicillin-resistant Staphylococcus aureus from adult and pediatric bathers in marine waters. BMC Microbiol. 2011;11:5. doi: 10.1186/1471-2180-11-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts MC, Soge OO, Giardino MA, Mazengia E, Ma G, Meschke JS. Vancomycin-resistant Enterococcus spp. in marine environments from the West Coast of the USA. J Appl Microbiol. 2009;107:300–307. doi: 10.1111/j.1365-2672.2009.04207.x. [DOI] [PubMed] [Google Scholar]
- Seifried SE, Tice AD, Eischen M. Diversity of community-associated strains of methicillin-resistant Staphylococcus aureus in Hawaii. J Infect Dis. 2007;195:305–307. doi: 10.1086/510252. [DOI] [PubMed] [Google Scholar]
- Selvakumar A, Borst M. Variation of microorganism concentrations in urban stormwater runoff with land use and seasons. J Water Health. 2006;4:109–124. [PubMed] [Google Scholar]
- Smyth DS, Feil EJ, Meaney WJ, Hartigan PJ, Tollersrud T, Fitzgerald JR, Enright MC, Smyth CJ. Molecular genetic typing reveals further insights into the diversity of animal-associated Staphylococcus aureus. J Med Microbiol. 2009;58:1343–1353. doi: 10.1099/jmm.0.009837-0. [DOI] [PubMed] [Google Scholar]
- Soge OO, Meschke JS, No DB, Roberts MC. Characterization of methicillin-resistant Staphylococcus aureus and methicillin-resistant coagulase-negative Staphylococcus spp. isolated from US West Coast public marine beaches. J Antimicrob Chemother. 2009;64:1148–1155. doi: 10.1093/jac/dkp368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tice AD, Pombo D, Hui J, Kurano M, Bankowski MJ, Seifried SE. Quantification of Staphylococcus aureus in seawater using CHROMagar SA. Hawaii Med J. 2010;69:8–12. [PMC free article] [PubMed] [Google Scholar]
- van Asselt GJ, Vliegenthart JS, Petit PL, van de Klundert JA, Mouton RP. High-level aminoglycoside resistance among enterococci and group A streptococci. J Antimicrob Chemother. 1992;30:651–659. doi: 10.1093/jac/30.5.651. [DOI] [PubMed] [Google Scholar]
- Viau EJ, Goodwin KD, Yamahara KM, Layton BA, Sassoubre LM, Burns SL, Tong H, Wong SHC, Lu Y, Boehm AB. Bacterial pathogens in Hawaiian coastal streams – Associations with fecal indicators, land cover, and water quality. Water Res. 2011;45:3279–3290. doi: 10.1016/j.watres.2011.03.033. [DOI] [PubMed] [Google Scholar]
- Washington State Department of Ecology BEACH Program. http://www.ecy.wa.gov/programs/eap/beach/data.html (viewed April 30, 2011)
- Waters AE, Contente-Cuomo T, Buchhagen J, Liu CM, Watson L, Pearce K, Foster JT, Bowers J, Driebe EM, Engelthaler DM, Keim PS, Price LB. Multidrug-resistant Staphylococcus aureus in US meat and poultry. Clin Infect Dis. 2011;52:1227–1230. doi: 10.1093/cid/cir181. [DOI] [PMC free article] [PubMed] [Google Scholar]