Abstract
Objective
To assess the impact of gynecologic surgery on mobility and functional status in women ≥ 60 years of age using Life-Space Assessment (LSA).
Design
Observational prospective cohort study
Setting
Academic outpatient urogynecology and gynecologic oncology clinics
Participants
Women presenting for urogynecology (N=51) and gynecologic oncology (N=51) surgery.
Measurements
LSA scores six weeks, six months and one year after surgery. Participant demographics, preoperative diagnoses, surgical approach, and medical comorbidities were collected. Analyses utilized repeated measures.
Results
Mean age was 71 + 7 years. Urogynecology participants started and maintained a higher LSA (p-value=0.03) than oncology participants at all study intervals. At six weeks post-surgery, urogynecology and oncology participants’ mean decline was 13-points (95% CI 4, 21 p-value=.004) and 23-points (95% CI 13, 33 p-value < .001), respectively. At six months, the urogynecology and oncology participants’ scores increased by a mean of 9-points (95% CI 1, 17 p-value=.033), and 13-points (95% CI 5, 20 p-value=.001) points, respectively. No significant difference was found at one year from baseline within each group or between groups in LSA scores. Income, depression, Body Mass Index (BMI) and having an operative complication predicted a larger decline in life-space over time in both groups.
Conclusion
Gynecologic surgical interventions in older women limit physical and functional ability at six weeks postoperatively. Both the urogynecology and gynecologic oncology cohorts returned to baseline levels by six months which was sustained to one year.
Keywords: Life-space assessment, perioperative function and mobility, gynecologic surgery
INTRODUCTION
In 2006, 37 million people age 65 and over lived in the United States, which was 12 percent of the total population. By 2030, this age group is predicted to be 71.5 million, increasing to nearly 20 percent of the total population, double the size of this population in 2000 (1). The majority of this rapidly growing, older population is women. In 2006, 58% of people over 65 years were women, which increased to 68% for age 85 and over (1). It has been estimated that the demand for care of pelvic floor disorders will increase by 45%, paralleling the evolving U.S. demographic (2). The same is likely to be true with surgery for gynecologic malignancy (3, 4). There is limited data regarding the impact of gynecologic and other surgeries on mobility, functional status, and participation in society in the older patient.
In the older woman, participation in society is an important factor with respect to retaining quality of life. In order to remain active in society, overall functional status and physical ability following surgery is an important consideration (5). Almost all studies of function or disability have focused on specific functional activities and minimal research has been related to overall mobility status and social participation due to lack of appropriate measures. Traditional measures of physical ability include Activities of Daily Living (ADL) measurements (6), Instrumental ADL (IADL) assessments (7), and physical performance measures (8). The Life-Space Assessment (LSA) is a validated questionnaire that measures functional status and mobility by incorporating where a person goes, the frequency of going there, and the degree of dependence required to get there in the four weeks prior to the assessment (9, 10, 11, 12). Although current measures used to assess functional decline postoperatively in older women exist, measuring life-space may be a better instrument, reflecting a person’s mobility and participation in society.
The purpose of this study was to assess the impact of gynecologic surgery on mobility and functional status in older women by prospectively evaluating LSA over a one year postoperative time period in women aged 60 and older undergoing urogynecologic and gynecological oncology surgery. We wished to characterize these changes both within and between each group to provide some perspective in two different surgical cohorts.
METHODS
Institutional Review Board approval from the University of Alabama at Birmingham (UAB) and written informed consent was obtained. From July 2006 until March 2007, eligible consecutive women age 60 years and older, were enrolled. Women were excluded if they were unable to complete a self-administered questionnaire, if they were previously seen and treated with a prior surgery for the same complaint, or if they were involved in another research trial; otherwise, they were offered inclusion. The initial LSA questionnaire was self-administered at enrollment and subsequent LSA questionnaires were mailed to the participants. Demographic data, body mass index (BMI) measured in kg/m2, self-reported medical comorbidities (ever or current), and route of surgical procedure (laparotomy, laparoscopy, or transvaginal/vulvar) were collected at enrollment. Transportation difficulty was defined by the participant and self-reported as present or not present. The occurrence of a surgical complication was obtained from the operative notes, discharge summaries, and postoperative follow-up visit notes and was, therefore, defined by the surgeons. These included bladder injury, wound separation, wound dehiscence, blood transfusion, venous thromboembolism, ileus, and intensive care unit admissions. Urogynecology participants had procedures for incontinence and/or prolapse. Gynecologic oncology procedures included surgery for endometrial cancer, ovarian cancer, pelvic masses and vulvar disease. These surgeries were performed by trained urogynecologists and gynecologic oncology physicians on faculty, respectively. The surgeons used laparoscopy, laparotomy, vulvar and vaginal approaches for these procedures. Vulvar and vaginal approaches were combined into one group for comparison. The attending physician documented the surgical approach at the time of surgery. This data was collected prospectively and verified by retrospective chart review.
The primary outcome measure was the change in LSA score over time. LSA for older adults was validated to assess mobility and participation in society, with respect to activity in one’s home environment and surrounding community, over the previous four weeks (9, 10, 11, 12). Our study questionnaire specifically excluded visits to the physician’s office secondary to a large proportion of long distance participants traveling outside of one’s town for appointments. LSA is based on a conceptual model of actual mobility as a series of concentric rings with five levels (12). Level 1 is mobility beyond the room in which one sleeps. Level 2 is mobility outside of the home such as a porch or hallway. Level 3 is mobility within the neighborhood other than one’s yard or apartment. Level 4 is mobility outside of the neighborhood but within one’s town. Level 5 is mobility outside of town. At each level, frequency of mobility is also recorded as < 1 per week, 1–3 times per week, 4–6 times per week or daily. Independence at each level is also recorded as personal assistance, equipment alone, or neither. The questionnaire has a total of 15-questions (3 questions for each mobility level) and takes the average subject approximately one minute to complete. Each LSA level, frequency and independence is given an ordinal weighted score with better mobility given higher scores. Possible LSA level scores are 0, 1, 2, 3, 4, 5; frequency scores are 1, 2, 3, 4; and independence scores are 1, 1.5 and 2. Therefore, Level 5 is scored a 5, frequency of daily a 4, and complete independence a 2. At each level, the scores for level, frequency and independence are multiplied. These scores are then summed across all 5 levels. Scores can range from 0–120, with 0 being bed bound and 120 traveling out of town everyday without assistance (11, 12). Death is measured as −10. The LSA score was measured at baseline, six weeks, six months and one year post operation. LSA was obtained from all participants at baseline and deaths were included in the final analysis.
Based on a previous analysis of the psychometric properties of the LSA, test-retest reliability demonstrated an intraclass correlation coefficient of 0.96 (95 % Confidence Interval of 0.95–0.97) for the measure (10). The LSA is also sensitive to change over time. Using standard deviations reported from the UAB Study of Aging (9) and the clinically relevant between group difference for LSA of 10 points, a sample size of 50 per group was needed to achieve 80% power with 5% Type I error rate. We powered the study for the between group comparison knowing that within group differences, if present, would also be captured. Of note, a change of 10 points in LSA was considered clinically relevant because it correlates with transitioning from restricted to unrestricted life space in measures of activities of daily living (10).
Demographic and clinical variables were compared between groups using independent t-test, chi square, and Fisher’s Exact test where appropriate for continuous and categorical variables. Repeated measures analysis was used to measure the impact on LSA between and within the 2 groups over time at six weeks, six months, and one year post-operatively using a backward selection model to identify variables impacting LSA at the 0.05 significance level. The selection process started with all demographic and patient parameters listed in Table 1. Within the urogynecology and oncology groups, the amount of change and 95% confidence interval were generated using the dependent t-test. Income, transportation difficulty, and age were known parameters that impact LSA and maintained in the final multivariable linear regression model based on an a priori decision (9). Tukey’s Honestly Significant Difference (HSD) corrected for multiple testing. Additionally, we evaluated the surgical approach (laparoscopic vs transvaginal vs laparotomy) using a backwards selection repeated measures model. Analyses were performed with JMP IN 5.1 (SAS Institute, Cary, NC).
Table 1.
Baseline Demographics and Clinical Characteristics
| Urogynecology (N=51) | Gyn Oncology (N=51) | P‡ | Overall | |
|---|---|---|---|---|
| Age* (years) | 70 ± 7 | 71 ± 8 | 0.791 | 71 ± 7 |
| BMI* (kg/m2) | 28 ± 5 | 31 ± 9 | 0.052 | 29 ± 7 |
| Race | 0.001 | |||
| African American | 1 (2) | 15 (29) | 16 (16) | |
| Non-Hispanic White | 49 (96) | 35 (69) | 84 (82) | |
| Hispanic | 1 (2) | 1 (2) | 2 (2) | |
| Income | 0.028 | |||
| <$7,999 | 4 (8) | 14 (27) | 18 (18) | |
| $8,000–15,999 | 9 (19) | 16 (31) | 25 (26) | |
| $16,000–29,999 | 13 (28) | 7 (14) | 20 (20) | |
| $30,000–49,999 | 7 (15) | 6 (12) | 13 (13) | |
| >$50,000 | 14 (30) | 8 (16) | 22 (22) | |
| Transportation Difficulty | 2 (4) | 6 (12) | 0.141 | 8 (8) |
| Tobacco | 5 (10) | 10 (20) | 0.162 | 15 (15) |
| Surgical Approach | <0.001 | |||
| Laparoscopy | 1 (2) | 6 (12) | 7 (7) | |
| Laparotomy | 2 (4) | 40 (78) | 42 (42) | |
| Transvaginal/Vulvar | 48 (94) | 5 (10) | 52 (52) | |
| Congestive Heart Failure | 3 (6) | 5 (10) | 0.461 | 8 (8) |
| Lung Disease | 4 (8) | 3 (6) | 0.781 | 7 (7) |
| Difficulty with Vision | 5 (10) | 5 (10) | 0.630 | 10 (10) |
| Hearing Difficulty | 9 (18) | 10 (20) | 0.694 | 19 (19) |
| Diabetes Mellitus | 4 (8) | 13 (26) | 0.016 | 17 (17) |
| Asthma | 7 (14) | 6 (12) | 0.723 | 14 (13) |
| Gastrointestinal Diagnoses | 5 (10) | 12 (24) | 0.055 | 17 (17) |
| Rheumatoid Arthritis or Osteoarthritis | 34 (67) | 30 (59) | 0.270 | 64 (63) |
| Back Problems | 4 (18) | 15 (29) | 0.121 | 24 (24) |
| Headaches | 15 (29) | 7 (14) | 0.045 | 22 (22) |
| Depression | 6 (12) | 10 (20) | 0.207 | 16 (16) |
| Anxiety | 5 (10) | 4 (8) | 0.756 | 9 (9) |
| Hypertension | 32 (63) | 43 (84) | 0.012 | 75 (74) |
| Angina | 3 (6) | 5 (10) | 0.358 | 8 (8) |
| History of Myocardial Infarction | 5 (10) | 5 (10) | 0.630 | 10 (10) |
| History of Cerebrovascular Accident | 3 (6) | 7 (14) | 0.159 | 10 (10) |
| Kidney Disease | 2 (4) | 0 (0) | 0.248 | 2 (2) |
| Prior Cancer (other than current diagnosis) | 10 (20) | 27 (53) | 0.001 | 37 (37) |
| Ever GERD | 15 (30) | 24 (47) | 0.051 | 39 (38) |
| High Cholesterol | 25 (49) | 23 (45) | 0.724 | 48 (47) |
| Operative Complication | 5 (10) | 17 (33) | <0.001 | 22 (22) |
All values represent N (%) unless otherwise noted.
Mean ± standard deviation
P is for the difference between urogynecology and gyn oncology
RESULTS
Forty-nine of 51 (96%) urogynecology and 43 of 51 (84%) oncology participants completed the six week LSA and 48/51 (94%) urogynecology and 43/51 (84%) oncology participants completed the six month LSA. Forty-two of 51 (82%) urogynecology and 39 of 51 (76%) oncology participants completed the one year LSA. There was one death in the urogynecology group at one year LSA follow up. There were three deaths in the oncology group at six weeks, one death at six months, and one death at one year LSA follow up. Total data at one-year follow up, which includes deceased participants, was obtained in 42/51 (82%) urogynecology and 39/51 (76%) oncology participants.
Patient demographics and other clinical characteristics are presented in Table 1. The overall mean age was 71 ± 7 years, and BMI was 29 ± 7 g/m2. Oncology participants in comparison to the urogynecology participants trended to a higher mean BMI (31 kg/m2 versus 28 kg/m2, p=0.052) and were less likely to be Non-Hispanic Whites (69% versus 96%, p =0.001). Oncology participants also underwent more laparotomies (78% versus 4%, p<0.001), and were more likely to have a surgical complication (33% versus 10%, p<0.001) than the urogynecology participants. Medical co-morbidities, diabetes (26% versus 8%, p=0.016), hypertension (84% versus 63%, p =0.012), and a prior cancer (53% versus 20%, p =0.001), were more common among the oncology than the urogynecology participants while the oncology participants were less likely to have headaches (14% versus 29%, p=0.045) than the urogynecology participants.
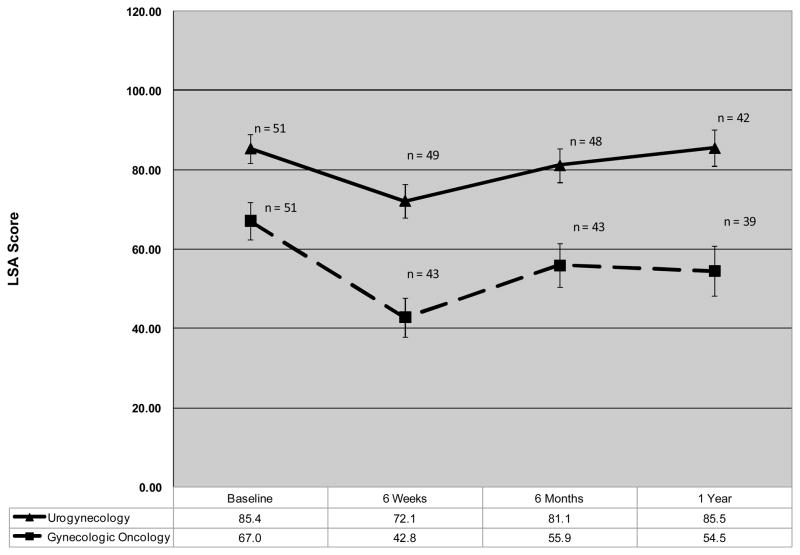
From the repeated measures model, change in LSA score for the two groups is shown in Figure 1 (vertical bars represent mean standard error at each time point). In addition to a priori including income, transportation difficulty, and age (variables known to impact LSA) (9), the backward model selection also included BMI, current diagnosis of depression and having an operative complication. The other variables listed in Table 1, including those that differed between groups did not significantly impact on LSA (except for BMI and having a complication) were dropped from the model. The model accounted for 69% of the variance, implying an acceptable fit. Urogynecology participants started and maintained a higher LSA (p=0.034) than the oncology participants at all time points. From the dependent t-test, the amount of change in mean LSA score between time points (mean, 95% Confidence Interval [CI]) for both the urogynecology and oncology groups is shown in Table 2. Both groups had significant within group reductions in life-space at six weeks after surgery followed by improvement at six months, which were sustained at one year. Change in mean LSA scores between urogynecology and oncology participants at the follow up time points were not statistically different: baseline-six weeks P= 0.118, six weeks-six months P= 0.476, and six months-one year P=0.546. Accounting for multiple testing with Tukey’s HSD, there was no difference between baseline, six month and one year time points within each group. When we evaluated the surgical approach (laparoscopic vs transvaginal vs laparotomy), no statistical differences were seen among the group by surgical type.
Figure 1.
Baseline and Postsurgical LSA Scores
Table 2.
Change in LSA Score between Time Points after Surgery
| Life-Space Assessment Points* | ||||
|---|---|---|---|---|
| Urogyn | P | Gyn Oncology | P | |
| Mean (95%CI) | Mean (95%CI) | |||
| Baseline-Six Weeks‡ | −12.5 (−4.2, −20.8) | 0.004 | −22.6 (−12.6, −32.6) | <0.001 |
| N=49 | N=40 | |||
| Six Weeks-Six Months | 8.8 (0.7, 16.8) | 0.033 | 12.7 (5.5, 19.9) | 0.001 |
| N=48 | N=40 | |||
| Six Months-One Year | 3.0 (−2.2, 9.7) | 0.213 | 0.4 (−9.1, 10.0) | 0.929 |
| N=42 | N=39 | |||
| Baseline-One Year† | 1.6 (−6.3, 9.4) | 0.688 | 9.5 (0.1, 18.9) | 0.048† |
| N=42 | N=38 | |||
Data from dependent t-test for within group changes.
Negative values represent a decrease in life-space points; positive values represent an increase.
Baseline-One Year differences not significant with repeated measures model.
In the repeated measures models, increased BMI, lower income level, the presence of depression and having an operative complication were variables significantly associated with change of mean LSA scores in both groups over the one year postoperative period. With every one year increase in age, LSA score decreased by 0.9 (95% CI 0.3, 1.6 P=0.006). Every one unit increase in BMI was associated with a 0.80 unit decrease in LSA (95% CI 0.04, 1.56 P=0.039). Having an income >$30,000–50,000 or >$50.000 increased LSA (P=0.004) above those with an income <$7,000 by a mean of 28.1 (95% CI 3.8, 52.4) and 27.2 (95% CI 5.5, 48.8), respectively. Having a current diagnosis of depression decreased LSA score by 19.4 (95% CI 5.3, 33.5 p-value=0.007) and having an operative complication decreased LSA score by 16.6 points (95% CI 4.5, 28.6).
DISCUSSION
In this prospective cohort of older women undergoing surgery, the life-space assessment measuring mobility and functional status pre- and post-surgery declined at six weeks, returned to baseline at six months and was sustained at one year in both groups. Compared to gynecologic oncology participants, urogynecology participants undergoing more elective types of surgery maintained a higher LSA before and after surgery. Continued improvement in life-space between six months and one year after gynecologic surgery was not found for urogynecology or gynecologic oncology participants, both maintaining levels that were statistically unchanged from baseline. Incorporating life-style and functional ability, the LSA score reflects a global functional change that other functional status measures may not detect in the perioperative period.
In comparison to other studies assessing pre- and post-operative mobility and functional status in older surgical patients, Lawrence et al evaluated change in post-operative outcomes after abdominal surgery in 372 older adults using ADLs and IADLs and other functional measures such as a timed walk, functional reach, and grip strength (13). Findings were a significant decline one week post-operation in all functional measures with the majority of the participants having continued disability in the functional measures at 6 months post-operatively. In a separate study of patients during acute hospitalization, factors such as physician-rated life expectancy and baseline bed mobility levels affected ability to regain ambulatory function during the acute hospital stay (14). In a study by Brown et al, life-space mobility was retrospectively evaluated pre- and post- hospitalization from prior medical and surgical admissions. In this community-based, longitudinal study of participants who were hospitalized for different types of major surgery (n = 44), LSA scores decreased by 23 points (95% CI −29.9 to −15.0) and also returned to baseline after one year, unlike participants admitted for medical conditions (n = 167) who only had a 9-point decline in LSA score and did not have a return in LSA scores to baseline values up to two years after admission (12). In comparison to this study, we had similar rates of decline after surgery in the gynecologic oncology participants (23-point decline with a 95% CI −32.6 to −12.6) and a close approximation to baseline LSA scores by 6 months, which was maintained in both groups after one year. The wide 95% CI seen in both studies may be due to the small sample sizes, n = 44 in the study by Brown et al and n = 51 for the gynecologic oncology participants (12). In counseling patients regarding outcomes after surgery, much of the discussion usually involves the immediate postoperative period and 6 week recovery time. Given above findings, clinicians should consider modifying their traditional counseling beyond the standard 6-week recovery time when caring for the older woman undergoing surgery.
Several studies in older adults have targeted treatments around hospitalization and the perioperative period. One study found that a preoperative geriatric assessment did not improve quality of life postoperatively in older women undergoing pelvic floor surgery (15). Two studies have showed improvements in functional status and mobility (IADLs and walking status) through rehabilitation and home physical therapy in older adults after hospitalization (16, 17). Using life-space mobility as an assessment tool in the perioperative setting may be a more sensitive measure than ADLs and IADLs to identify older adults at risk for further decline in functional capacity and mobility after more elective and indicated surgeries.
Variables found to significantly impact LSA in our study included: age, income, BMI, depression, and occurrence of operative complications. Participants with a current diagnosis of depression had a significant decline in LSA. Depression also affected post surgical outcomes in the prospective cohort study of Lawrence et al (13). Mental health disease impacts participation in society and therefore limits life-space. This deserves a priori preoperative consideration in discussing post-surgical recovery and regaining of functional status with patients who suffer from depression. Additionally, Lawrence et al found that operative complications affected postoperative recovery (13). Similarly our participants with an operative complication in the postoperative period had decreased life-space. Consideration should be given to aggressive rehabilitation and assistance with patients identified as having these factors in the perioperative period.
There are several limitations of this study. The sample size is small with regards to estimating the impact of patient characteristics on LSA, although numbers were sufficient per power analysis to detect statistical and clinical significance in LSA. Further, while a validation study of Life-Space Assessment in a surgical population was not performed, it was previously validated in the community from which our study was performed including subjects with recent hospitalizations (10). This descriptive study includes two populations of women receiving surgery for different underlying pathologies. We measured within and between cohorts to account for this. Women presenting for gynecologic oncology complaints had more medical co-morbidities than the urogynecology group, which may have contributed to lower LSA scores at baseline, even though statistical modeling attempted to adjust for this. Also, the gynecologic oncology group had significantly more African American women than the urogynecology patient group. It is unknown whether racial/ethnic differences existed in care-seeking for pelvic floor disorders, including incontinence, in this study (18). It is possible that specific postoperative restrictions placed on the women varied by provider in the six-week postoperative period thus having an impact on LSA scores at this time point; however, this may be related to the type of surgery the patient had rather than the specific surgeon as all patients were managed according to standardized postoperative orders and guidelines. Even though surgical approach did not correlate with LSA, we were likely underpowered to detect any difference between the groups according to type of surgery performed. Also, identification of a surgical complication was at the discretion and documentation of the surgeon. Post-operative delirium was not reported in any participants. If present, it may have had marked impact on functional status and recovery.
We explored several covariants including depression and opted for self-reported assessments (yes/no) as opposed to quantative assessments to relieve patients’ burden with participation in the study. Future studies would certainly warrant quantifying the impact of depression with the Geriatric Depression Scale or other validated tool for use in an older population. We believe that depression may differ between groups, and we controlled for self-reported depression (along with baseline LSA level) in the repeated measures model. Unfortunately, a measure of co-morbid disease burden or severity was not captured in this study and would be important to include in future research. We did not assess if there was a change in health status at each time point from the initial surgery. Other health factors could have affected LSA. Additionally, many gynecologic oncology participants received adjuvant or neoadjuvant therapies such as chemotherapy and/or radiation. We did not capture this information, but further characterizing LSA in a gynecology oncology cohort who will prospectively receive adjuvant or neoadjuvant treatments is an important area of future research. Finally, attrition in questionnaire completion at six month and one year follow up occurred in both cohorts, but was marked in the oncology participants. It is plausible these participants had worsening performance, prognosis, or depression; therefore, the final LSA might have bias in that the patient’s who were clinically improved were more likely to complete the questionnaires.
There are several strengths of this study. The research is prospective and longitudinal with one year follow up. LSA is a sensitive measure of change over time in women having surgery. LSA may be a better measure of functional status in older adults in comparison to other studies as it documents a patient’s mobility and participation in society over time and space. This gives us information not only regarding what a patient can do, but what they are actually doing. In addition, data from this study may be used to power other studies using LSA as an outcome measure in specific groups.
In general, post-surgical gynecologic counseling considers a six week recovery time. Patients are instructed on limitations during this time and expectations for mobility. However, in our study population of older women, their mobility and overall functional status was still decreased at the six-week time point. Evaluating our current routine post-operative counseling and potential screening of women that may be at risk for further declines in functional status after surgery would be important. Interventions aimed at recognizing and treating depression in the pre- and post-operative period may also improve functional status. In addition, gynecological surgery patients with increased BMI, low income and post-operative complications are at increased risk for life-space loss after surgery and may benefit from more aggressive rehabilitation and additional support with discharge after hospitalization. Targeting overall functional status pre- and post-operatively by utilizing life-space assessment could improve patient-centered outcomes and long-term participation of these older women in society.
Acknowledgments
Partially supported by the National Institute of Diabetes and Digestive and Kidney Diseases DK068389 to HER and a Dennis W. Jahnigen Career Development Scholar Award to TLW
Footnotes
Poster Presentation, American Urogynecological Society 28th Annual Meeting, September 27–29, 2007, Hollywood, Florida; Presidential Poster Session, American Geriatrics Society Annual Meeting, April 30-May 4, 2008, Washington, DC
References
- 1.Federal Interagency Forum on Aging-Related Statistics. Federal Interagency Forum on Aging-Related Statistics. Washington DC: U.S. Government Printing Office; Mar, 2008. Older Americans 2008: Key Indicators of Well-Being. [Google Scholar]
- 2.Lawrence JM, Lukacz ES, Nager CW, et al. Prevalence and co-occurrence of pelvic floor disorders in community-dwelling women. Obstet Gynecol. 2008;111:678–85. doi: 10.1097/AOG.0b013e3181660c1b. [DOI] [PubMed] [Google Scholar]
- 3.National Cancer Institute. [Accessed August 24, 2008]; Available at: http://www.cancer.gov/statistics/
- 4.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2007. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 5.US Department of Health and Human Services. Physical Activity and Health: A Report of the Surgeon General. Atlanta: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996. [Google Scholar]
- 6.Katz S, Ford A, Moskowitz R, et al. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 7.Lawton MP. Instrumental activities of daily living (IADL) scale: Self reported version. Psychopharmacol Bull. 1988;24:789–91. [PubMed] [Google Scholar]
- 8.Mathias S, Nayak U, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil. 1986;67:387–9. [PubMed] [Google Scholar]
- 9.Allman RM, Baker P, Maisiak R, et al. Racial Similarities and Differences of Mobility Change over 18 Months. J Gen Intern Med. 2004;19:1118–26. doi: 10.1111/j.1525-1497.2004.30239.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baker P, Bodner E, Allman R. Measuring Mobility in Community-Dwelling Older Adults. J Am Geriatr Soc. 2003;51:1610–4. doi: 10.1046/j.1532-5415.2003.51512.x. [DOI] [PubMed] [Google Scholar]
- 11.Peel C, Baker P, Roth D, et al. Assessing Mobility in Older Adults: The UAB Study of Aging Life-Space Assessment. Physical Therapy. 2005;85:1008–19. [PubMed] [Google Scholar]
- 12.Brown CJ, Roth DL, Allman RM, et al. Trajectories of Life-Space Mobility after Hospitalization. Ann Intern Med. 2009;150:372–378. doi: 10.7326/0003-4819-150-6-200903170-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lawrence VA, Hazuda HP, Cornell JE, et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg. 2004;199:762–72. doi: 10.1016/j.jamcollsurg.2004.05.280. [DOI] [PubMed] [Google Scholar]
- 14.Brown CJ, Roth DL, Peel C, et al. Predictors of regaining ambulatory ability during hospitalization. J Hosp Med. 2006;1:277–84. doi: 10.1002/jhm.104. [DOI] [PubMed] [Google Scholar]
- 15.Richter HE, Redden DT, Duxbury AS, et al. Pelvic floor surgery in the older woman: Enhanced compared with usual preoperative assessment. Obstet Gynecol. 2005;105:800–7. doi: 10.1097/01.AOG.0000154920.12402.02. [DOI] [PubMed] [Google Scholar]
- 16.Melin AL, Bygren LO. Efficacy of the rehabilitation of elderly primary health care patients after short-stay hospital treatment. Med Care. 1992;30:1004–15. doi: 10.1097/00005650-199211000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Nikolaus T, Specht-Leible N, Bach M, et al. A randomized trial of comprehensive geriatric assessment and home intervention in the care of hospitalized patients. Age Aging. 1999;28:543–50. doi: 10.1093/ageing/28.6.543. [DOI] [PubMed] [Google Scholar]
- 18.Harris SS, Link CL, Tennstendt SL, et al. Care seeking and treatment for urinary incontinence in a diverse population. J Urol. 2007;77:680–84. doi: 10.1016/j.juro.2006.09.045. [DOI] [PubMed] [Google Scholar]