The evaluation by IARC (1992) concluded that ‘There is sufficient evidence in humans for the carcinogenicity of solar radiation. Solar radiation causes cutaneous malignant melanoma and non-melanocytic skin cancer. There is limited evidence in humans for the carcinogenicity of exposure to ultraviolet (UV) radiation from sunlamps and sun beds’.
In assessing the quantitative contribution of different exposures to cancer in the UK, we are not concerned with non-melanoma skin cancers. This is because there is no agreed method of enumerating such tumours, which may occur at multiple skin sites throughout life, and, because of their generally trivial nature, are in any case under-enumerated in registration systems.
Evaluation of the proportion of total cases of malignant melanoma that is related to solar (UV) exposure poses many problems. Clearly, the method of estimation based on prevalence of exposure and relative risk is inappropriate, given that there is no ‘unexposed’ population, and the distribution of relevant types of exposure is unknown.
We have therefore estimated the UV-attributable cases occurring in 2010 as the difference between the number observed and those that would have been expected with a theoretical-minimum-risk exposure distribution, based on historical data from UK. These historical data are the estimated incidence rates for the generation of individuals born in 1903, resident in the South Thames region of England.
Methods
Over the last 30 years, the incidence of malignant melanoma has increased more than for any other common cancer in the UK; in males the age-standardised (European standard) rate rose from 2.5 in 1975 to 14.6 in 2007, and it is projected to be 17.0 in 2010; the female age-standardised rate has increased fourfold – from 3.9 to 15.4 – over the same period, with a projected value of 18.0 in 2010.
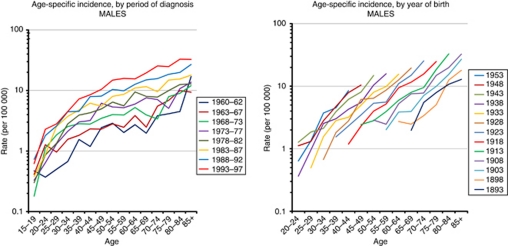
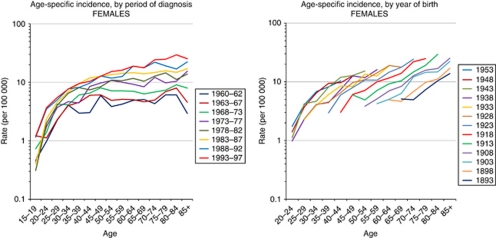
The longest series of high-quality incidence data in the UK, with incidence rates from 1960 onwards, is from the South Thames region (Parkin et al, 2005). Figures 1 and 2 show the trends in incidence between 1960 and 1997 in males and females, respectively.
Figure 1.
Trends in incidence of malignant melanoma in the South Thames region, 1960–1997, males.
Figure 2.
Trends in incidence of malignant melanoma in South Thames region, 1960–1997, females.
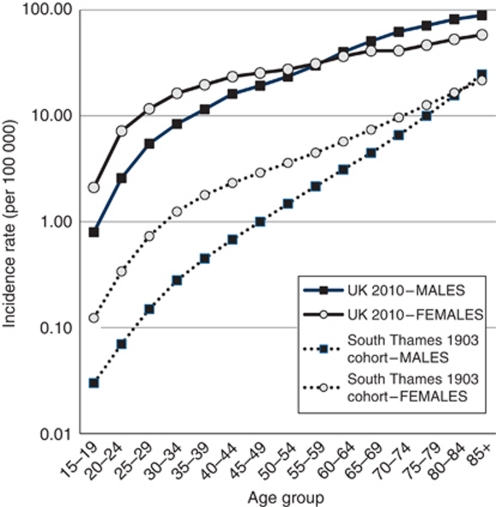
We fitted an age-cohort model to the South Thames data to reconstruct age-specific incidence rates for age groups without actual observations, and selected the estimated incidence rates in the cohort born in 1903 as our ‘reference’, with which to calculate expected numbers of cases in 2010, if solar exposure had been as modest as in the 1903 cohort. Age-standardised incidence rates in this generation are some 10-fold lower in males and 6-fold lower in females than those estimated for 2010, but the disparity is considerably greater in the young than in the elderly (Figure 3).
Figure 3.
Malignant melanoma: incidence in UK 2010 and South Thames 1903 birth cohort.
Results
Table 1 shows the projected numbers of cases of melanoma in the UK in 2010 (6096 in men and 6822 in women), and the number expected in the same year if the rates in the 1903 South Thames cohort had been applied. Overall, some 90% of melanoma cases in men and 82% in women are estimated to be attributed to ‘excess’ solar irradiation, although the attributable fractions are very much greater at younger ages. The overall attributable fraction (85.9% of melanoma) is equivalent to 3.5% of all new cancer cases in the UK in 2010.
Table 1. Malignant melanoma cases diagnosed in 2010, estimated to be due to exposure to solar (ultraviolet) radiation.
|
Malignant melanoma
|
All cancera
|
||||
|---|---|---|---|---|---|
| Age (years) | Relative risk | Observed cases | Excess attributable cases (PAF) | Observed cases | Excess attributable cases (PAF) |
| Males | |||||
| <25 | 33.50 | 78 | 75.7 (97.0) | 1853 | 75.7 (4.1) |
| 25–34 | 32.37 | 284 | 275.2 (96.9) | 2109 | 275.2 (13.0) |
| 35–49 | 21.98 | 1042 | 994.6 (95.4) | 8359 | 994.6 (11.9) |
| 50–64 | 13.88 | 1717 | 1593.3 (92.8) | 37 617 | 1593.3 (4.2) |
| ⩾65 | 6.81 | 2975 | 2538.4 (85.3) | 108 729 | 2538.4 (2.3) |
| Total | 6096 | 5477 (89.8) | 158 667 | 5477.2 (3.5) | |
| Females | |||||
| <25 | 19.31 | 199 | 188.7 (94.8) | 1646 | 188.7 (11.5) |
| 25–34 | 14.18 | 561 | 521.4 (92.9) | 3284 | 521.4 (15.9) |
| 35–49 | 9.72 | 1551 | 1391.4 (89.7) | 16 877 | 1391.4 (8.2) |
| 50–64 | 6.89 | 1816 | 1552.4 (85.5) | 41 338 | 1552.4 (3.8) |
| ⩾65 | 3.69 | 2695 | 1965.6 (72.9) | 92 439 | 1965.6 (2.1) |
| Total | 6822 | 5620 (82.4) | 155 584 | 5619.6 (3.6) | |
| Persons | |||||
| <25 | 277 | 264 (95.4) | 3500 | 264 (7.6) | |
| 25–34 | 845 | 797 (94.3) | 5393 | 797 (14.8) | |
| 35–49 | 2593 | 2386 (92.0) | 25 236 | 2386 (9.5) | |
| 50–64 | 3533 | 3146 (89.0) | 78 955 | 3146 (4.0) | |
| ⩾65 | 5670 | 4504 (79.4) | 201 167 | 4504 (2.2) | |
| Total | 12 918 | 11 097 (85.9) | 314 251 | 11097 (3.5) | |
Abbreviations: PAF, population-attributable fraction (%).
Excluding non-melanoma skin cancer.
Discussion
With respect to malignant melanoma the evidence for carcinogenicity of solar radiation is derived from various sources. Descriptive studies (in white populations) show a positive association between incidence of and mortality from melanoma and residence at lower latitudes. Studies of migrants suggest that the risk of melanoma is related to solar radiant exposure at the place of residence in early life. The body-site distribution of melanoma favours sites usually exposed to the sun. Evidence from a large number of case–control studies is generally consistent with positive associations with residence in sunny environments throughout life, in early life and even for short periods in early adult life. Positive associations are generally seen between measurements of cumulative sun damage, expressed biologically as microtopographical changes or history of keratoses or non-melanocytic skin cancer, and measures of intermittent exposure to the sun (such as particular sun-intensive activities, outdoor recreation or vacations) and with a history of sunburn. In contrast, chronic exposure, as assessed through occupational exposure, appears to reduce the melanoma risk, an observation consistent with the descriptive epidemiology of the condition, which shows lower risks in groups that work outdoors.
Previous evaluations of the proportion of total cases of malignant melanoma that is related to solar (UV) exposure have also relied on the direct method of estimating attributable risk: the difference between observed incidence in the population and incidence in an ‘unexposed’ reference group. In a widely quoted study, Armstrong and Kricker (1993) used three different estimates of incidence in ‘unexposed’ populations to compare with the observed rates in Australia:
The incidence of melanoma at body sites unexposed to the sun (buttocks and (in women) the scalp, from the Queensland Cancer Registry in 1987; Green et al, 1993).
The incidence from areas of lower sun exposure in migrants to Australia.
A comparison of US Whites and US Blacks, in which the incidence in Blacks was taken as the incidence in unexposed Whites.
In the evaluation of avoidable cancers in the Nordic countries, Winther et al (1997) used the crude incidence rates of melanoma at unexposed sites from the above study as the baseline ‘unexposed’ and estimated attributable fraction in Nordic countries from this study. The IARC's assessment of causes of cancer in France (IARC, 2007) simply took the attributable fraction calculated by Armstrong and Kricker (1993) for Australia as relevant to France in the year 2000. In the evaluation in this section, we chose to use rates from an ‘unexposed’ reference population that is relevant to UK – the generation born in 1903 in the South Thames region of England.
The pattern of increasing incidence of malignant melanoma in this population over time is a feature of many fair-skinned populations (Lens and Dawes, 2004). In Europe, the increases began first with Scandinavia and the UK and then spread to western, southern and eastern Europe (de Vries et al, 2003). The increase has been mainly for thin melanomas (Lipsker et al, 1999; Mackie et al, 2002). Some of the increase may be due to increased surveillance and early detection, as well as changes in diagnostic criteria, but much of the increase is considered to be real (van der Esch et al, 1991) and linked to changes in sun behaviour (Dennis, 1999; de Vries and Coebergh, 2004; de Vries and Coebergh, 2005). Although the trends observed in South Thames could equally well be related to an increase in risk by period of diagnosis, or by birth cohort, we assume that they are in fact due to changes in exposure to solar UV exposure because of altered patterns of behaviour (in choice of clothing and recreational sunshine), producing an increase in incidence that is cohort-specific. This Edwardian generation almost certainly had little bodily exposure to sunlight in their childhood, and even as young adults opportunities for vacations in sunny climates would have been very limited (Figure 4). Nevertheless, exposure was not zero, so that, even at almost 86%, an estimate of PAF will be something of an underestimate.
Figure 4.
Holiday makers on the beach around 1919–1921.
In a recent update to its evaluation of the carcinogenicity of UV irradiation, IARC reaffirmed the carcinogenicity of solar radiation, but the classification of the use of UV-emitting tanning devices was raised to Group 1, ‘carcinogenic to humans’ (El Ghissassi et al, 2009). A part of the increase in incidence rates in contemporary UK may well be due to use of sunlamps, but since these devices will almost certainly not have been used by any of the 1903-born generation, the estimate of total UV-attributable cancers based on the differences in incidence rates remains a valid approach.
See acknowledgements on page Si.
Footnotes
The authors declare no conflict of interest.
References
- Armstrong BK, Kricker A (1993) How much melanoma is caused by sun exposure? Melanoma Res 3: 395–401 [DOI] [PubMed] [Google Scholar]
- Dennis LK (1999) Analysis of the melanoma epidemic, both apparent and real: data from the 1973 through 1994 surveillance, epidemiology, and end results program registry. Arch Dermatol 135: 275–280 [DOI] [PubMed] [Google Scholar]
- de Vries E, Bray FI, Coebergh JW, Parkin DM (2003) Changing epidemiology of malignant cutaneous melanoma in Europe 1953–1997: rising trends in incidence and mortality but recent stabilizations in Western Europe and decreases in Scandinavia. Int J Cancer 107: 119–126 [DOI] [PubMed] [Google Scholar]
- de Vries E, Coebergh JW (2004) Cutaneous malignant melanoma in Europe. Eur J Cancer 40: 2355–2366 [DOI] [PubMed] [Google Scholar]
- de Vries E, Coebergh JW (2005) Melanoma incidence has risen in Europe. Br Med J 331: 698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Ghissassi F, Baan R, Straif K, Grosse Y, Secretan B, Bouvard V, Benbrahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V (2009) WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens – part D: radiation. Lancet Oncol 10: 751–752 [DOI] [PubMed] [Google Scholar]
- Green A, MacLennan R, Youl P, Martin N (1993) Site distribution of cutaneous melanoma in Queensland. Int J Cancer 53: 232–236 [DOI] [PubMed] [Google Scholar]
- IARC (1992) IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. Vol. 55. Solar and Ultraviolet Radiation. IARC: Lyon [PMC free article] [PubMed] [Google Scholar]
- IARC (2007) Attributable causes of cancer in France in the year 2000. IARC Working Group Reports 3.
- Lens MB, Dawes M (2004) Global perspectives of contemporary epidemiological trends of cutaneous malignant melanoma. Br J Dermatol 150: 179–185 [DOI] [PubMed] [Google Scholar]
- Lipsker DM, Hedelin G, Heid E, Grosshans EM, Cribier BJ (1999) Striking increase of thin melanomas contrasts with stable incidence of thick melanomas. Arch Dermatol 135: 1451–1456 [DOI] [PubMed] [Google Scholar]
- MacKie RM, Bray CA, Hole DJ, Morris A, Nicolson M, Evans A, Doherty V, Vestey J, Scottish Melanoma Group (2002) Incidence of and survival from malignant melanoma in Scotland: an epidemiological study. Lancet 360: 587–591 [DOI] [PubMed] [Google Scholar]
- Parkin DM, Whelan S, Ferlay J, Storm H (2005) Cancer Incidence in Five Continents, Vol. I to VIII. IARC Cancer Base No. 7: Lyon [Google Scholar]
- van der Esch EP, Muir CS, Nectux J, Macfarlane G, Maisonneuve P, Bharucha H, Briggs J, Cooke RA, Dempster AG, Essex WB, Hofer PA, Hood AF, Ironside P, Larsen TE, Little H, Philipps R, Pfau RS, Prade M, Pozharisski KM, Rilke F, Schafler K (1991) Temporal change in diagnostic criteria as a cause of the increase of malignant melanoma over time is unlikely. Int J Cancer 47: 483–489 [DOI] [PubMed] [Google Scholar]
- Winther JF, Ulbak K, Dreyer L, Pukkala E, Osterlind (1997) Avoidable cancers in the Nordic countries. Radiation. APMIS Suppl 76: 83–99 [PubMed] [Google Scholar]