There is considerable controversy over the protective effect of diets rich in fruit, vegetables and fibre, and the respective roles of the different components (including micronutrients such as folate). The report of the Committee on Medical Aspects of Food Nutrition Policy (COMA) (Department of Health, 1998) recommended increasing consumption of all of them, an advice that seems to have motivated the Department of Health in promoting its ‘5-a-day’ programme (Department of Health, 2005). The original consensus of the probable decrease in risk of several cancers of the gastrointestinal tract (oral cavity and pharynx, oesophagus, stomach and colorectum) associated with increased consumption of fruit and vegetables (WHO/FAO, 2003) was based on the results of multiple case–control studies and a few prospective studies. The IARC Handbook of Cancer Prevention (IARC, 2003) concludes its review of the evidence as follows:
There is limited evidence for cancer-preventive effect of consumption of fruit and vegetables for cancers of the mouth and pharynx, oesophagus, stomach, colorectum, larynx, lung, ovary (vegetables only), bladder (fruit only) and kidney. There is inadequate evidence for a cancer-preventive effect of consumption of fruit and vegetables for all other sites. More specifically, this evidence indicates that higher intake of fruit probably lowers the risk of cancers of the oesophagus, stomach and lung, while higher intake of vegetables probably lowers the risk of cancers of the oesophagus and colorectum. Likewise a higher intake of fruit possibly lowers the risk of cancers of the mouth, pharynx, colorectum, larynx, kidney and urinary bladder. An increase in consumption of vegetables possibly reduces the risk of cancers of the mouth, pharynx, stomach, larynx, lung, ovary and kidney.
The conclusions of the WCRF report (2007) are more or less in line with these, except with respect to large-bowel cancer, for which the evidence for protective effects of both vegetables and fruit was considered ‘limited’ (in contrast to ‘conclusive’ or ‘probable’ – implying that a causative relationship is uncertain). More emphasis was placed on the importance of the protective effects of consumption of foods containing dietary fibre than on vegetables per se. The summary conclusions were as follows:
Non-starchy vegetables probably protect against cancers of the mouth, pharynx, and larynx, and those of the oesophagus and stomach. There is limited evidence suggesting that they also protect against cancers of the nasopharynx, lung, colorectum, ovary, and endometrium. Fruit in general probably protects against cancers of the mouth, pharynx, and larynx, and those of the oesophagus, lung, and stomach. There is limited evidence suggesting that fruit also protects against cancers of the nasopharynx, pancreas, liver, and colorectum.
In this analysis, we follow the WCRF in considering ONLY the effect of a deficit of fruit and vegetables on cancers of the mouth and pharynx, oesophagus, stomach and larynx, and of a deficit of fruit on cancers of the lung.
The advice from the Department of Health (2005) is to increase the average consumption of a variety of fruit and vegetables to at least five portions per day, corresponding to 5 × 80 or 400 g per day. In this section, we estimate the population-attributable fraction (PAF) of these five cancers (and of all cancer) that results from consumption of fruit and vegetables lower than this target.
Methods
The risks associated with consumption of 1 g per day of fruit or of vegetables are shown in Table 1. As we are concerned with quantifying the effect of a deficit in consumption, they are presented as the risk associated with a decreased intake of 1 g per day.
Table 1. Estimated risks associated with a decreased consumption of 1 g per day of fruits and non-starchy vegetables.
|
Risks associated
with 1 g per day decrease in consumption
|
||
|---|---|---|
| Cancer type | Fruit | Vegetables a |
| Oral cavity and pharynx | 0.00488 | 0.00416 |
| Oesophagus | 0.00504 | 0.00266 |
| Stomach | 0.00234 | 0.00320 |
| Colon–rectum | 0 | 0 |
| Larynx | 0.00322 | 0.00370 |
| Lung | 0.00146 | 0 |
Non-starchy vegetables.
These risks derive from the simple means of the values from three meta-analyses: those of Riboli and Norat (2003), WCRF (2007) and, except for laryngeal cancer, Soerjomataram et al (2010). (The value for the protective effect of vegetables on cancers of the oral cavity and pharynx in the meta-analysis of Soerjomataram et al (2010) was quite implausible, implying a reduction in risk of 1.4% per gram per day. We substituted the value for upper aero-digestive tract cancers from the multi-centre European prospective study (EPIC) of 0.29% per gram per day (Boeing et al, 2006)). The values from the latter were reported as relative risk per gram increase in daily consumption of fruit and vegetables. For the others, the excess relative risk for a decrease of 1 g of vegetables or fruit consumed was estimated by assuming a log-linear relationship between exposure and risk, so that:
where x is the exposure level (in grams per day) and RRx the relative risk for x grams per day.
The latent period (or interval between ‘exposure’ to fruit and vegetables and the appropriate decrease in risk of these cancers) is not known. Prospective studies of diet and cancer (from which the estimates of relative risk are mostly drawn) involve follow-up periods (between estimated dietary intake and cancer onset) of several years. For the cohort studies contributing to the meta-analyses of WCRF, 10 studies of lung cancer and 6 of stomach cancer reported the mean duration of follow-up; the simple means were 15.2 and 10.3 years, respectively. There are a few cohort studies on upper GI cancers: the follow-up periods in the EPIC study (González et al, 2006) and Japanese JPHC studies (Yamaji et al, 2008) were 6.5 and 7.7 years, respectively. For the purposes of estimating attributable fraction, we assume a mean latency of 10 years, and thus examine the effects on cancers occurring in 2010 of sub-optimal levels of fruit and vegetable consumption in 2000. Consumption of fruit and vegetables, in grams per week, by age group and sex, is available for 2000–2001 from the National Diet & Nutrition Survey (FSA, 2004; Table 2.1). The mean consumption, by age group, is shown in Table 2. The target consumption of 400 g per day was not achieved at any age, and the young, in particular, had a low consumption of such items.
Table 2. Mean consumption of fruit and non-starchy vegetables by sex and age group, Great Britain 2000–2001.
| Vegetables |
Mean consumption
(grams per day) by age group (years)
|
||||
|---|---|---|---|---|---|
| or fruit | 19–24 | 25–34 | 35–49 | 50–64 | 19–64 |
| Men | |||||
| Vegetables | 95 | 122 | 144 | 162 | 137 |
| Fruit | 27 | 61 | 99 | 122 | 87 |
| Women | |||||
| Vegetables | 89 | 130 | 139 | 143 | 132 |
| Fruit | 54 | 74 | 98 | 151 | 103 |
| Persons | |||||
| Vegetables | 92 | 126 | 141 | 153 | 135 |
| Fruit | 40 | 68 | 99 | 137 | 95 |
The National Diet & Nutrition Survey also provides the distribution of intake of fruit and vegetables in the British population, in terms of the cumulative percentage of individuals (by sex and age group) consuming 0, <1, <2, …, >5 portions of fruit and vegetables daily (FSA, 2004; Table 2.3). The populations of each sex were dichotomised into two age groups (<50 and 50–64), and ‘portions’ were converted into grams (of fruit and vegetables), such that the mean daily intake corresponded to the values in Table 2. Table 3 shows the results in terms of the proportions of the population at seven different levels of consumption of fruit and vegetables.
Table 3. Proportions of the Great Britain population in seven categories of fruit and vegetable consumption in 2000–2001, and estimated deficit in consumption in each category from the recommended 400 g per day.
|
Consumption
categories in 2000–2001
|
|||||||
|---|---|---|---|---|---|---|---|
| Sex and age (years) | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Men 19–49 | |||||||
| Proportion of the population | 0.01 | 0.22 | 0.29 | 0.20 | 0.11 | 0.08 | 0.09 |
| Vegetables (g per day) | 0 | 27.8 | 83.3 | 138.8 | 194.3 | 249.8 | 305.3 |
| Deficit from 256 g per day | 256 | 228 | 172 | 117 | 61 | 6 | 0 |
| Fruit (g per day) | 0 | 15.8 | 47.3 | 78.8 | 110.3 | 141.8 | 173.3 |
| Deficit from 144 g per day | 144 | 129 | 97 | 66 | 34 | 3 | 0 |
| Men 50–64 | |||||||
| Proportion of the population | 0.01 | 0.06 | 0.22 | 0.16 | 0.15 | 0.16 | 0.24 |
| Vegetables (g per day) | 0 | 24.5 | 73.5 | 122.5 | 171.5 | 220.5 | 269.5 |
| Deficit from 228 g per day | 228 | 204 | 155 | 106 | 57 | 8 | 0 |
| Fruit (g per day) | 0 | 18.5 | 55.5 | 92.5 | 129.5 | 166.5 | 203.5 |
| Deficit from 172 g per day | 172 | 153 | 116 | 79 | 42 | 5 | 0 |
| Women 19–49 | |||||||
| Proportion of the population | 0.01 | 0.06 | 0.22 | 0.16 | 0.15 | 0.16 | 0.24 |
| Vegetables (g per day) | 0 | 25.8 | 77.3 | 128.8 | 180.3 | 231.8 | 283.3 |
| Deficit from 242 g per day | 242 | 217 | 165 | 114 | 62 | 11 | 0 |
| Fruit (g per day) | 0 | 16.8 | 50.3 | 83.8 | 117.3 | 150.8 | 184.3 |
| Deficit from 158 g per day | 158 | 141 | 107 | 74 | 40 | 7 | 0 |
| Women 50–64 | |||||||
| Proportion of the population | 0.01 | 0.19 | 0.26 | 0.21 | 0.12 | 0.08 | 0.12 |
| Vegetables (g per day) | 0 | 21 | 63 | 105 | 147 | 189 | 231 |
| Deficit from 195 g per day | 195 | 174 | 132 | 90 | 48 | 6 | 0 |
| Fruit (g per day) | 0 | 22.3 | 66.8 | 111.3 | 155.8 | 200.3 | 244.8 |
| Deficit from 205 g per day | 205 | 183 | 139 | 94 | 50 | 5 | 0 |
To calculate the deficit in consumption of fruit and vegetables relative to a target of 400 g per day for both, the deficit in each sex and age group (19–49, 50–64) was calculated from Table 2. For example, the deficit in older men (50–64) was, on average, 216 g per day (400−(162+122)). The total deficit is partitioned into deficits of fruit and vegetables, so that the same ratio of vegetables to fruit that was being eaten in 2000–1 is maintained. Thus, the 400 g per day target for consumption in men in the age group of 50–64 years is partitioned in the ratio of 162:122 (Table 2); i.e., 228 g per day vegetables and 172 g per day fruit (Table 3). The deficit of each in the different consumption categories in men and women aged <50 years and in the age group of 50–64 is shown in Table 3.
For each cancer, the relative risk in 2010 in the four age–sex strata is calculated from the deficit in consumption 10 years earlier (2000–2001), with the risk for fruit and vegetables calculated separately according to the following formula:
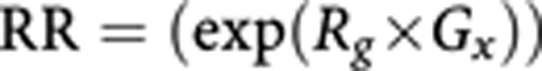 |
where Rg is the relative risk for a deficit of 1 g per day of fruit or vegetables (Table 1) and Gx is the deficit in consumption (as shown in Table 3) in consumption category x.
The benefits of fruit and vegetables are considered to be multiplicative in their effect, so that
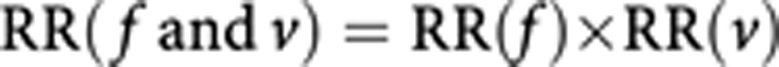 |
Population-attributable fractions were calculated for each of the four sex–age groups in Table 3 according to the following formula:
 |
where px is the proportion of population in consumption category x and ERRx the excess relative risk (RR(f and v)−1) in consumption category x.
Results
Table 4 shows the PAFs and the estimated number of cases ‘caused’ in 2010 by these deficits in consumption of fruit and vegetables 10 years earlier. The cancers for which the greatest proportion of cases may be related to low intake of fruit and vegetables are the oral cavity and pharynx (56%), oesophagus (46%) and larynx (45%). Although only 9% of lung cancer cases may be related to low intake of fruit (there is no excess risk of lung cancer from low intake of vegetables), the actual number of cases (3567) represents almost one-quarter of the total number of cancers attributable to low intake of fruit and vegetables (14 902: Table 5).
Table 4. Cancer cases in 2010 at six sites caused by deficient intake of fruit and vegetables in 2000–2001.
|
Age (years)
|
Oral cavity and pharynx
|
Oesophagus
|
Stomach
|
Colon–rectum
|
Larynx
|
Lung
|
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| At exposure | At outcome (+10 years) | PAF | Obs. | Excess attributable cases | PAF | Obs. | Excess attributable cases | PAF | Obs. | Excess attributable cases | PAF | Obs. | Excess attributable cases | PAF | Obs. | Excess attributable cases | PAF | Obs. | Excess attributable cases |
| Men | |||||||||||||||||||
| 19–49 | 29–59 | 0.65 | 1874 | 1223 | 0.56 | 1064 | 596 | 0.49 | 587 | 285 | 0 | 3410 | 0 | 0.56 | 443 | 249 | 0.11 | 2839 | 300 |
| 50–64 | ⩾60 | 0.52 | 2656 | 1393 | 0.45 | 4643 | 2067 | 0.35 | 3875 | 1367 | 0 | 18 643 | 0 | 0.43 | 1358 | 578 | 0.08 | 19 417 | 1584 |
| Total (%) | 4571 | 2616 (57.2%) | 5713 | 2663 (46.6%) | 4467 | 1651 (37.0%) | 22 127 | 0 (0.0%) | 1803 | 827 (45.9%) | 22 273 | 1884 (8.5%) | |||||||
| Women | |||||||||||||||||||
| 19–49 | 29–59 | 0.64 | 786 | 503 | 0.55 | 332 | 184 | 0.47 | 325 | 151 | 0 | 2791 | 0 | 0.54 | 113 | 61 | 0.11 | 2550 | 280 |
| 50–64 | ⩾60 | 0.50 | 1521 | 762 | 0.44 | 2482 | 1088 | 0.32 | 2243 | 722 | 0 | 14 926 | 0 | 0.40 | 269 | 106 | 0.09 | 15 562 | 1403 |
| Total (%) | 2359 | 1265 (53.6%) | 2819 | 1272 (45.1%) | 2577 | 874 (33.9%) | 17 787 | 0 (0.0%) | 386 | 168 (43.5%) | 18 132 | 1683 (9.3%) | |||||||
| Persons | |||||||||||||||||||
| 19–49 | 29–59 | 2660 | 1725 | 1396 | 779 | 912 | 436 | 6201 | 0 | 556 | 310 | 5389 | 579 | ||||||
| 50–64 | ⩾60 | 4177 | 2155 | 7125 | 3155 | 6118 | 2089 | 33 569 | 0 | 1627 | 684 | 34 979 | 2987 | ||||||
| Total (%) | 6930 | 3881 (56.0%) | 8532 | 3935 (46.1%) | 7044 | 2525 (35.8%) | 39 914 | 0 (0.0%) | 2189 | 995 (45.4%) | 40 405 | 3567 (8.8%) | |||||||
Abbreviations: Obs=observed cases; PAF=population-attributable fraction.
Table 5. Number of all cancer cases in 2010 caused by deficient intake of fruit and vegetables in 2000–2001.
|
Age group (years)
|
All cancersa
|
|||
|---|---|---|---|---|
| At exposure | At outcome (+10 years) | Observed cases | Excess attributable cases | PAF (%) |
| Men | ||||
| 19–49 | 29–59 | 27 845 | 2651 | 9.5 |
| 50–64 | 60+ | 128 192 | 6990 | 5.5 |
| Total | 158 667 | 9641 | 6.1 | |
| Women | ||||
| 19–49 | 29–59 | 42 499 | 1179 | 2.8 |
| 50–64 | 60+ | 110 403 | 4082 | 3.7 |
| Total | 155 584 | 5261 | 3.4 | |
| Persons | ||||
| 19–49 | 29–59 | 70 344 | 3830 | 5.4 |
| 50–64 | 60+ | 238 595 | 11 071 | 4.6 |
| Total | 314 251 | 14 902 | 4.7 | |
Abbreviations: PAF=population-attributable fraction.
Excluding non-melanoma skin cancer.
Table 5 sums the excess numbers of cases at the five sites, caused by low consumption of fruit and vegetables, and expresses these numbers as a fraction of the total burden of (incident) cancer. The estimate is 6.1% cancers in men and 3.4% in women, or 4.7% of cancers overall.
Discussion
As we note in the Introduction, the protective role of the consumption of fruit and vegetables against cancer is controversial. The first report of the World Cancer Research Fund (WCRF)/AICR Panel (1997) considered that the evidence for a protective effect of fruit and/or vegetables against cancers of the upper aero-digestive tract, stomach and lung was ‘convincing’. As we describe, although the preventive recommendation remains to ‘eat at least five portions/servings (at least 400 g) of a variety of non-starchy vegetables and of fruits every day’, this evaluation had been downgraded to ‘probable’ in the latest report (WCRF, 2007). This is because of the subsequent publication of some cohort studies that failed to find statistically significant associations. Key (2011) suggests that, as all of the relevant cancers are also caused by smoking, and that smokers have a lower intake of fruit and vegetables than non-smokers, the observed associations could be due to residual confounding (failure to control adequately for this risk factor in the analysis, generally due to the use of rather broad groups for categorising smoking status). With respect to lung cancer (the malignancy with the strongest smoking-associated risk), for example, recent cohort studies show conflicting results: no association (Wright et al, 2008) or protective effects of fruit (and vegetables) in all subjects or in smokers only (Büchner et al, 2010). Miller et al (2004) have even suggested that the strength of the association between smoking and lung cancer can overwhelm a real, but much smaller, association with diet. Fruit and vegetables are the main dietary source of many micronutrients and other metabolically active chemicals. The types and quantities of these compounds vary between items, which may explain why most studies measuring cancer risk in relation to overall intake tend to show only a weak association (McCullough and Giovannucci, 2004).
In any case, in this section, we have followed the results of the current consensus reviews by WHO/FAO (2003), IARC (2003) and WRCF (2007) with respect to those cancers that might reasonably be caused, in part, by a deficient intake of these dietary elements. The latter report considered that the evidence for a protective effect of vegetables (and, even more so, fruit) on the risk of colon cancer was ‘limited’, and placed more emphasis on the importance of the protective effects of consumption of foods containing dietary fibre than on vegetables per se. This concurs with more recent reviews of the evidence from epidemiological studies (Koushik et al, 2007; Huxley et al, 2009), and in this section, therefore, we consider that no cases of colorectal cancer are attributable to sub-optimal consumption of vegetables or fruit.
An estimate of the fraction of cancer in UK attributable to low intake of fruit and vegetables was recently published by the WCRF (2009) (Table 6). There are several reasons for the differences in results from the current estimates. WCRF selected ‘representative’ studies from which to take the relative risks, rather than those from their own meta-analyses. Exposure prevalence was taken from data for the same year as outcome (2002). Finally, the baseline category (optimum consumption) varied by site – ⩾160 g vegetables per day for oesophagus and stomach cancer; ⩾120 g per day for upper aero-digestive cancers; ⩾57.1 g fruit per day for stomach cancer; and ⩾160 g fruit per day for lung cancer. Given the estimates by site in Table 6, the overall AF (for all cancers) due to low consumption of vegetables and fruits would be 7.1% – of which almost 60% are lung cancers, because of the large attributable fraction (33%) and high incidence of this cancer.
Table 6. Percentage of cancers in UK in 2002 attributable to low consumption of fruits and vegetables.
| Oesophagus | Mouth, pharynx, larynx | Lung | Stomach | |
|---|---|---|---|---|
| Non-starchy vegetables | 21 (4–40) | 34 (2–57) | 21 (0–41) | |
| Fruits | 5 (2–9) | 17 (0–43) | 33 (17–51) | 18 (3–33) |
From WCRF/AICR (2009).
See acknowledgements on page Si.
Footnotes
The authors declare no conflict of interest.
References
- Boeing H, Dietrich T, Hoffmann K, Pischon T, Ferrari P, Lahmann PH, Boutron-Ruault MC, Clavel-Chapelon F, Allen N, Key T, Skeie G, Lund E, Olsen A, Tjonneland A, Overvad K, Jensen MK, Rohrmann S, Linseisen J, Trichopoulou A, Bamia C, Psaltopoulou T, Weinehall L, Johansson I, Sánchez MJ, Jakszyn P, Ardanaz E, Amiano P, Chirlaque MD, Quirós JR, Wirfalt E, Berglund G, Peeters PH, van Gils CH, Bueno-de-Mesquita HB, Büchner FL, Berrino F, Palli D, Sacerdote C, Tumino R, Panico S, Bingham S, Khaw KT, Slimani N, Norat T, Jenab M, Riboli E (2006) Intake of fruits and vegetables and risk of cancer of the upper aero-digestive tract: the prospective EPIC-study. Cancer Causes Control 17: 957–969 [DOI] [PubMed] [Google Scholar]
- Büchner FL, Bueno-de-Mesquita HB, Linseisen J, Boshuizen HC, Kiemeney LA, Ros MM, Overvad K, Hansen L, Tjonneland A, Raaschou-Nielsen O, Clavel-Chapelon F, Boutron-Ruault MC, Touillaud M, Kaaks R, Rohrmann S, Boeing H, Nöthlings U, Trichopoulou A, Zylis D, Dilis V, Palli D, Sieri S, Vineis P, Tumino R, Panico S, Peeters PH, van Gils CH, Lund E, Gram IT, Braaten T, Martinez C, Agudo A, Arriola L, Ardanaz E, Navarro C, Rodríguez L, Manjer J, Wirfält E, Hallmans G, Rasmuson T, Key TJ, Roddam AW, Bingham S, Khaw KT, Slimani N, Bofetta P, Byrnes G, Norat T, Michaud D, Riboli E (2010) Fruits and vegetables consumption and the risk of histological subtypes of lung cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC). Cancer Causes Control 21: 357–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of Health (1998) Nutritional Aspects of the Development of Cancer. Report of the Working Group on Diet and Cancer. Committee on Medical Aspects of Food Nutrition Policy. HMSO: UK [PubMed] [Google Scholar]
- Department of Health (2005) Choosing a Better Diet: A Food and Health Action Plan. Available at www.bda.uk.com/Downloads/ChoosingBetterDiet.pdf
- Food Standards Agency (FSA) (2004) National Diet and Nutrition Survey: Adults Aged 19 to 64, Vol. 5. Summary Report. Available at www.food.gov.uk/multimedia/pdfs/ndns5full.pdf
- González CA, Pera G, Agudo A, Bueno-de-Mesquita HB, Ceroti M, Boeing H, Schulz M, Del Giudice G, Plebani M, Carneiro F, Berrino F, Sacerdote C, Tumino R, Panico S, Berglund G, Simán H, Hallmans G, Stenling R, Martinez C, Dorronsoro M, Barricarte A, Navarro C, Quiros JR, Allen N, Key TJ, Bingham S, Day NE, Linseisen J, Nagel G, Overvad K, Jensen MK, Olsen A, Tjønneland A, Büchner FL, Peeters PH, Numans ME, Clavel-Chapelon F, Boutron-Ruault MC, Roukos D, Trichopoulou A, Psaltopoulou T, Lund E, Casagrande C, Slimani N, Jenab M, Riboli E (2006) Fruit and vegetable intake and the risk of stomach and oesophagus adenocarcinoma in the European Prospective Investigation into Cancer and Nutrition (EPIC-EURGAST). Int J Cancer 118: 2559–2566 [DOI] [PubMed] [Google Scholar]
- Huxley RR, Ansary-Moghaddam A, Clifton P, Czernichow S, Parr CL, Woodward M (2009) The impact of dietary and lifestyle risk factors on risk of colorectal cancer: a quantitative overview of epidemiological evidence. Int J Cancer 125: 171–180 [DOI] [PubMed] [Google Scholar]
- International Agency for Research on Cancer (IARC) (2003) Handbooks of Cancer Prevention: Vol. 8. Fruit and Vegetables. IARC Press: Lyon [Google Scholar]
- Key TJ (2011) Fruit and vegetables and cancer risk. Br J Cancer 104: 6–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koushik A, Hunter DJ, Spiegelmann D, Beeson WL, van den Brandt PA, Buring J, Calle EE, Cho EFraser GE, Fraudenheim JL, Fuchs CS, Giovannucci EL, Goldbohm RA, Harnack L, Jacobs Jr DR, Kato I, Krogh V, Larsson SC, Leitzmann MF, Marshall JR, McCullough ML, Miller AB, Pietien P, Rohan TE, Schatzkin A, Sieri S, Virtanen MJ, Wolk A, Zeleniuch-Jacquotte A, Zhang SM, Smith-Warner SA (2007) Fruits, vegetables and colon cancer risk in a pooled analysis of 14 cohort studies. J Natl Cancer Inst 99: 1471–1483 [DOI] [PubMed] [Google Scholar]
- McCullough ML, Giovannucci EL (2004) Diet and cancer prevention. Oncogene 23: 6349–6364 [DOI] [PubMed] [Google Scholar]
- Miller AB, Altenburg HP, Bueno-de-Mesquita B, Boshuizen HC, Agudo A, Berrino F, Gram IT, Janson L, Linseisen J, Overvad K, Rasmuson T, Vineis P, Lukanova A, Allen N, Amiano P, Barricarte A, Berglund G, Boeing H, Clavel-Chapelon F, Day NE, Hallmans G, Lund E, Martinez C, Navarro C, Palli D, Panico S, Peeters PH, Quirós JR, Tjønneland A, Tumino R, Trichopoulou A, Trichopoulos D, Slimani N, Riboli E (2004) Fruits and vegetables and lung cancer: Findings from the European Prospective Investigation into Cancer and Nutrition. Int J Cancer 108: 269–276 [DOI] [PubMed] [Google Scholar]
- Riboli E, Norat T (2003) Epidemiologic evidence of the protective effect of fruit and vegetables on cancer risk. Am J Clin Nutr 78(Suppl): 559S–569S [DOI] [PubMed] [Google Scholar]
- Soerjomataram I, Oomen D, Lemmens V, Oenema A, Benetou V, Trichopoulou A, Coebergh JW, Barendregt J, de Vries E (2010) Increased consumption of fruit and vegetables and future cancer incidence in selected European countries. Eur J Cancer 46: 2563–2580 [DOI] [PubMed] [Google Scholar]
- WHO/FAO (2003) Diet, Nutrition and The Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation. WHO Technical Report Series 916 WHO: Geneva [PubMed] [Google Scholar]
- World Cancer Research Fund (WCRF)/American Institute for Cancer Research (AICR) (1997) Food, Nutrition, Physical Activity and the Prevention of Cancer: A Global Perspective. AIRC: Washington, DC [Google Scholar]
- World Cancer Research Fund (WCRF)/American Institute for Cancer Research (AICR) (2009) Policy and Action for Cancer Prevention. Food, Nutrition and Physical Activity: A Global Perspective. American Institute for Cancer Research: Washington, DC [Google Scholar]
- World Cancer Research Fund (WCRF) Panel (2007) Food, Nutrition, Physical Activity, and the Prevention of Cancer: A Global Perspective. World Cancer Research Fund: Washington, DC [Google Scholar]
- Wright ME, Park Y, Subar AF, Freedman ND, Albanes D, Hollenbeck A, Leitzmann MF, Schatzkin A (2008) Intakes of fruit, vegetables, and specific botanical groups in relation to lung cancer risk in the NIH-AARP Diet and Health Study. Am J Epidemiol 168: 1024–1034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaji T, Inoue M, Sasazuki S, Iwasaki M, Kurahashi N, Shimazu T, Tsugane S (2008) Fruit and vegetable consumption and squamous cell carcinoma of the esophagus in Japan: the JPHC study. Int J Cancer 123: 1935–1940 [DOI] [PubMed] [Google Scholar]


