Abstract
Purpose
Despite the well-established benefits of physical activity (PA), most Americans, especially those in rural, traditionally underserved areas, engage in considerably less PA than recommended. This study examines perceived barriers to and facilitators of PA and promising organized PA programs among rural Appalachians.
Design
Eight focus groups and seven group key informant interviews were conducted.
Setting
This study was conducted in eastern Kentucky, in Central Appalachia.
Subjects
114 rural Appalachian residents (74% female, 91% White) participated.
Measures
Open-ended, semi-structured, and structured questions regarding perceptions of, barriers to/facilitators of, and examples of successful/failed PA programs were asked.
Analysis
Qualitative data analysis was conducted, including codebook development and steps taken to ensure rigor and transferability. Interrater reliability was over 94%.
Results
In addition to barriers that are consistent with other populations, rural Appalachian residents indicated that travel time, family commitments, and inadequate community resources undermine PA. Suggested avenues to increase PA include partnership with churches and the U.S. Cooperative Extension Service; programs that include families, are well-advertised, focus on health rather than appearance; and, underlying all suggestions, culturally-relevant yet non-stereotyping activities.
Conclusions
When developing PA interventions in rural Appalachia, it is important to employ community-based participatory approaches that leverage unique assets of the population and show potential in overcoming challenges to PA.
Keywords: Physical activity, Appalachia, community-based research
Indexing Key Words: Manuscript format: research; Research purpose: descriptive; Study design: qualitative; Outcome measure: cognitive; Setting: local community; Health focus: fitness/physical activity; Strategy: education, skill building/behaviors change; Target population age: youth, adults, seniors; Target population characteristics: geographic location, underserved
Purpose
Despite the well-established benefits of physical activity (PA), most Americans, especially those in rural, traditionally underserved areas, engage in considerably less PA than recommended. In order to develop a community-based PA intervention, we conducted formative research with residents of rural Appalachian Kentucky to identify their perceptions of PA and to glean suggestions for programs to promote PA.
Benefits and Rates of Physical Activity
Optimal physical activity is a key component of health and well-being and is associated with decreased risk of morbidity and mortality1–3 and higher levels of perceived health.4 Higher levels of PA have been associated with lower rates of coronary heart disease, high blood pressure, stroke, type 2 diabetes, metabolic syndrome, colon and breast cancer, depression, and overall mortality.1
Although the benefits of PA are clear, Behavioral Risk Factor Surveillance System data indicate that fewer than half (49%) of all adults nationwide report obtaining the recommended amount of PA. The data are even more sobering for Kentucky, which ranks 45th among states for the percentage (45%) of adults receiving the recommended level of PA, and second in the nation for the percentage (24%) of adults who are inactive (defined as receiving fewer than 10 minutes of moderate to vigorous PA per week).5
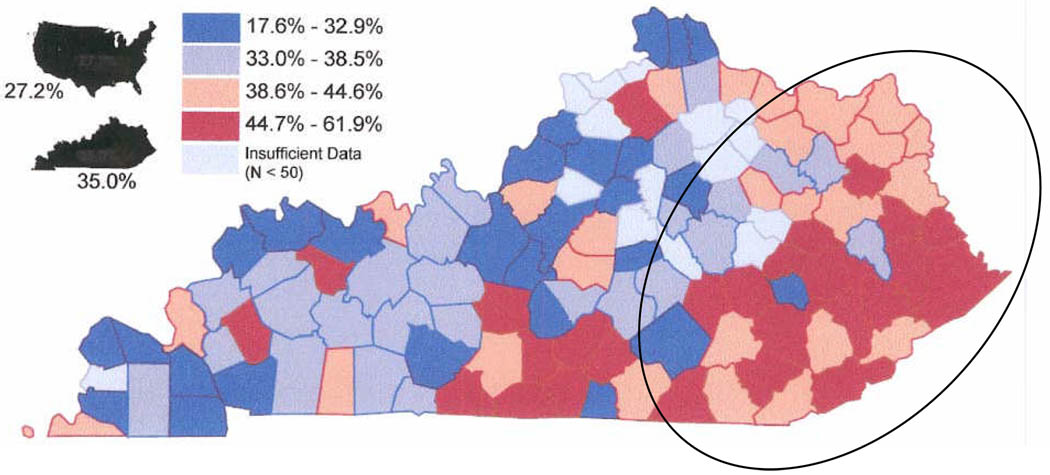
Kentucky’s 54 Appalachian counties have even more modest rates of PA: 35–44% of adults reported no participation in physical activities or exercise in the past month.6 As shown in Figure 1, Kentucky, particularly the Appalachian region, has low rates of leisure time activity. In the five counties in which the current study was conducted, between 39% and 62% of residents report no leisure time physical activities.7
Figure.
Adults with no Leisure Time Physical Activity by Kentucky County with Appalachian Kentucky Circled.7
Barriers to and Facilitators of PA
Explanations for the health inequities present in rural Appalachia tend to focus on the resources of the community (lack of public transportation and fewer community and health services—for example, nearly 80% of Appalachian Kentucky counties have health care provider shortages)8–9 and the characteristics of the population (rural residents tend to be older, poorer, less educated and lack health insurance).10 However, perceptual issues related to health shape both participation in PA and, ultimately, health outcomes.11
Barriers to engaging in adequate PA in Appalachia are not well-characterized, but research with other underserved populations has identified personal factors (e.g., caregiving responsibilities, lack of time and resources, and self-consciousness)12 and characteristics of the environment (e.g., lack of access to appropriate facilities, unsafe neighborhoods, poor weather, and inadequate programming and activities)13 as key barriers to PA. Facilitators of PA in underserved populations include enjoyment, self-efficacy, motivation, social support, family involvement, and access to facilities,14 as well as cultural norms and traditions that encourage PA.15
The magnitude of the problem of physical inactivity in Appalachia, coupled with the unique cultural, economic, and environmental characteristics of the region, warrants special attention to the barriers to and facilitators of successful PA interventions. Although there are investigations elucidating ecological factors that affect PA participation among older adults16 and children17 in other rural regions, we currently lack a comprehensive understanding of perceptions of PA and programs to promote PA among rural Appalachians. Research has indicated that it is crucial to understand perceptions of PA before appropriate and effective interventions can be developed and implemented.18 Therefore, the current study explored Appalachian residents’ perceptions of PA, providing vital information for the development of effective and acceptable PA interventions in this and other rural regions. The main question that guided our research was “how do rural Appalachian residents perceive PA and programs to promote PA?” Guided by the ecological model of health behavior,19 we sought to elicit responses that address a range of influences on PA, from personal (microsystem) to societal (macrosystem), ultimately to design a culturally-informed, tailored intervention to promote PA in the region.
Design
Since, to our knowledge, no empirically-based literature exists on perceptions of PA or PA promotion programs among Appalachians, we used qualitative methods (focus group [FG] and group key informant [GKI] interviews) to gain such insights and inform the development of a faith-based community intervention to increase PA. Although it is more typical to conduct individual key informant interviews,20 our past experience suggests that, like FG participants, key informants with shared expertise elaborate on or contradict, each others’ perspectives, resulting in a rich conversation. Furthermore, GKI interviews have been used to gather data from those with specialized knowledge in other areas.21 The protocols, measures, and analytic procedures were similar between the FG and GKI interviews, with slight variations in sampling approach, discussion guide, and honoraria. For example, although FG participants received both a meal and an honorarium ($25) GKIs received only the honorarium. All participants signed informed consent forms prior to participating in this study. All protocols were approved by the University of Kentucky’s Institutional Review Board.
Setting
Appalachia, a geographically and culturally diverse region of 410 counties in 13 states, contains nearly 22 million people, 8.3% of the total U.S. population.22–23 Along with many assets such as a beautiful terrain, a tradition of strong and supportive families, and longstanding involvement in community improvement, Central Appalachian residents face many challenges. In 2000, the poverty rate in Appalachian Kentucky was 28% higher than that of the nation,24 and in 2007, per capita personal income in Central Appalachia was only 71% of the U.S. average.25 The five Kentucky counties of Central Appalachia in which the current project was conducted have socioeconomic status and health indicators among the lowest in the U.S. Specifically, average per capita income in the participating counties ranged from 55% to 67% of the average U.S. income, and the average percent of adults age 25 and over who had graduated from high school was 58% in the participating counties compared to 80% in the nation.26 Health-wise, the five study counties demonstrate distinct disadvantage, with twice the national rate for diabetes and significantly higher rates of CVD and cancer.26
Sample Selection and Recruitment
FG participants were recruited through participating churches in the study counties for several reasons. First, because church attendance is so widespread in the region,27 recruiting through churches resulted in a wide cross-section of the population. Additionally, since the data form the basis for a subsequent faith-based intervention, this recruitment venue allowed us to develop appropriate and relevant programming. Finally, our previous partnerships with faith communities allowed us to gain access to diverse participants. Specifically, although a predominantly White region (on average, 97% White)23 our partnership with several African American churches helped us to obtain a more inclusive sample. We oversampled African Americans due to our commitment to inclusivity and to address the worse health profiles of Appalachian African Americans.28 Inclusion criteria included being 18 and older and being willing and able to participate in a FG. We did not specify that potential participants had to be church members, since many church attendees lack formal membership.
After a church agreed to host a FG, pastors or other church leaders assisted with recruitment by announcing the project from the pulpit or through church bulletins and requesting that any interested individual attend the discussion on a specified date. We did not select participants nor exclude anyone meeting our inclusion criteria. Theoretical saturation principles guided our sample size,29 and a total of eight FG were conducted before reaching saturation.
In addition to gauging perceptions of the general population via FG, we also conducted seven GKI interviews with 23 stakeholders from the churches, including the minister(s), or designee, and social services and healthcare providers. These individuals have specialized knowledge in a key area of importance for PA, such as providing PA education to school children or directing Senior Citizen’s Center programming. GKIs were selected through snowball sampling, with theoretical saturation again guiding our sample size. In snowball sampling, participants who have special areas of expertise or insight are asked to recommend others who have a particular skill set or knowledge base;30 in our case, a grounded understanding of PA determinants and perspectives on organized PA programming in rural Appalachia. Aside from age criteria (18 and older) and being willing to participate, the only GKI inclusion criteria was their specialized knowledge of PA, including community programming, historical perspectives on PA, and knowledge of the community. Once we had identified several individuals, including the director of a community center and a social service organization, we selected additional GKIs to ensure a broad representation of perspectives.
Discussion Guide
Our FG discussion guide (Table 1) was developed by project staff, which included both academic researchers and community members. The guide focused on four domains: semantic/cognitive constructs (including terminology of ‘exercise’ versus ‘physical activity’ and conceptualization of PA); perceptions of engaging in PA; determinants of PA; and perceptions of programs designed to increase PA. A similar, but slightly more detailed, guide was used for the GKI interviews.
Table 1.
Discussion Guide
|
Procedures
Our community staff, who have extensive experience organizing and moderating FG, conducted the eight sessions over five months. The community staff consisted of two primary moderators (SW, KD) who conducted all of the sessions, with two additional experienced staff members assisting them in collecting paperwork, taking fieldnotes, and writing memos. The following steps were taken to ensure consistency among the eight FG: the same moderators were present at all sessions; one discussion guide was used; transcripts were reviewed immediately to detect deviation from or incompleteness of the discussion guide; and, periodically, outside investigators (MS, RD, NS) attended the sessions.31 Most sessions lasted 90–120 minutes.
The moderator opened with a description of the purpose of the FG and then posed the open-ended questions from the discussion guide to the group. Upon completion of the discussion, participants completed a sociodemographic form. The process was repeated for the GKI interviews, with the exception that, since there were only 1–3 individuals participating in each GKI interview, transcripts included statements attributable to specific people, while specific FG participants were unidentifiable.
Analysis
The tape-recorded sessions were transcribed by local, trained transcriptionists and reviewed for accuracy by the community staff. The transcripts were then imported into NVivo (QSR, Melbourne, Australia) for coding, organization, and analysis. Coding began with one researcher (TK) engaging in line-by-line coding of the transcripts, affixing codes to each text segment. She then worked with another researcher (RD) to refine and define the codes, eventually developing a preliminary codebook, which allowed standardization of the content analysis and served as a record for definitions and operationalization of codes. The codebook was refined eight times.32–33
In addition to the standardization of the codebook, several steps enhanced the rigor and transferability of the data collection and analysis. First, we employed member checks through summarizing what was said at the completion of each FG and asking participants if the team was asking relevant questions and comprehending the group’s messages.34 Second, consistent with standard interrater reliability techniques, transcripts were coded by two researchers to refine the codebook, resulting in a final rate of 94%, generally considered strong evidence of reliability.35
Results
Table 2 displays the demographic characteristics of the 114 participants. Although the vast majority of participants were female and we oversampled African Americans, our sample was fairly representative of Central Appalachia otherwise, with a modest level of education, lower income, and moderate health.
Table 2.
Group Key Informant (n=23) and Focus Group Participant (n=91) Characteristics
| Variable | GKI n(%) |
FG n(%) |
|
|---|---|---|---|
| Sex | |||
| Male | 2(9) | 28(31) | |
| Female | 21(91) | 63(69) | |
| Age | |||
| 18–30 | 9(39) | 12(13) | |
| 31–50 | 6(26) | 24(26) | |
| 51+ | 8(35) | 55(60) | |
| Race | |||
| White | 22(96) | 82(90) | |
| African-American | 1(4) | 7(8) | |
| Other | - | 2(2) | |
| Education | |||
| High school or less | 5(22) | 54(59) | |
| Some college/college graduate | 11(48) | 37(41) | |
| Graduate school | 7(30) | - | |
| Marital Status | |||
| Married | 14(61) | 56(62) | |
| Separated/Divorced/Never married | 8(35) | 22(24) | |
| Widowed | 1(4) | 13(14) | |
| Perceived Income Adequacy | |||
| Struggle to get by | 4(17) | 19(21) | |
| Enough to get by | 11(48) | 44(48) | |
| More than I need | 8(35) | 24(26) | |
| Unable/unwilling to say | - | 4(4) | |
| Actual income | |||
| Under $20,000 | 7(30) | 24(26) | |
| $20,001–40,000 | 8(35) | 30(33) | |
| $40,001 or more | 8(35) | 26(29) | |
| Unwilling to say | - | 11(12) | |
| Perceived Health Status | |||
| Excellent | 3(13) | 5(6) | |
| Very good | 7(30) | 23(25) | |
| Good | 9(39) | 40(44) | |
| Fair | 3(13) | 19(21) | |
| Poor | 1(4) | 4(4) | |
Analysis of the transcripts revealed several important themes concerning perceptions of PA, facilitators of and barriers to PA, and important considerations for the design of culturally-appropriate PA programs in the region.
‘Physical Activity’ vs. ‘Exercise’
Among the participants the word ‘exercise’ had multiple meanings, which were both positive (“[Exercise is] something that will strengthen your body, make you healthier, and give you a better lifestyle.”) and negative (e.g., exercise is associated with pain). When describing exercise, participants focused on experiences during and outcomes of exercising. The general opinion of ‘physical activity’ was that “[PA] is something you do and don’t think about.” Frequently, participants discussed the two terms in regard to one another: “You can do physical activity and make exercise of it.”
Facilitators of and Barriers to PA
When asked what they think about PA, participants identified a range of physical and mental benefits of PA that encourage participation in PA as well as barriers to PA such as negative experiences while engaging in PA, fatigue from time spent at work, and time taken by other commitments reducing their desire and ability to engage in PA (see Table 3). Such facilitators and barriers are common regardless of whether a person lives in a rural or urban area. Participants also identified barriers unique to this sample such as long distances to destinations, the challenging physical environment, competing priorities (especially family commitments), and the lack of PA opportunities in the community, noting that these barriers were exacerbated by the economic stresses faced in a region of persistent poverty.
Table 3.
Facilitators of and Barriers to PA
| Facilitators of PA | |
|
|
|
|
|
|
| Barriers to PA | |
|
|
|
|
|
|
Travel Time and Family Commitments in Appalachia
Participants reported that the extensive distances required to reach common destinations in their rural communities (schools, grocery stores, the closest town) consume a significant portion of their time. A community center director noted, “I think it has become custom in this area that you are going to have to travel a little bit to get something. That is not necessarily the right way, but, in fact, that is the way it is.”
Similarly, lengthy distances required to get to workout facilities often discouraged rural Appalachians from engaging in PA. Several participants who lived far away from one of the few local PA facilities noted, “The Sportsplex would definitely work better if it was closer,” and “nobody wants to drive 45 minutes to the Sportsplex.” Conversely, nearby residents touted the success of the Sportsplex noting, “It’s so close I can’t help but go every free minute I get.” Furthermore, although many participants reported that they used and enjoyed formally organized PA programs such as Curves and Silver Sneakers, they also reported that few of those programs exist or last in their communities. A FG participant mentioned that, “Curves closed down even though it seemed successful; I think the distance made it fail.”
Family commitments comprise an additional source of time constraints that result in PA barriers. Many participants expressed remorse when they took time to do PA rather than engaging with their family. One FG participant revealed, “Even though I know I need to exercise, and I know it’s going to help me, and it will make me feel better, I feel guilty for doing it because I feel like I should be doing something else in the house or for the kids or for someone other than myself.”
Inadequate community resources
Participants reported that without a large population, PA programs often are poorly or sporadically attended and cannot be self-supporting. This situation causes program directors to forego organized activities, thus decreasing individuals’ opportunities to engage in PA. A manager at a district health department indicated that she had to cancel the aerobics class there due to poor attendance. She described how costly it was to identify, train, and retain a regular instructor; to advertise for the classes; and to run the program (secure a location, find music, purchase equipment, etc.) With very few people attending, the health educator felt that she could not justify the expense of the aerobics program and will not offer another program in the foreseeable future.
Other inadequate community resources negatively influence individuals’ opportunities to engage in PA. Participants mentioned environmental challenges such as poor road conditions that prevent people from traveling to PA facilities and that resources in the region for repairing roads and clearing mountain roads of snow are limited. Participants discussed the lack of public transportation or carpooling options in the region, suggesting the establishment of carpools as a means of increasing access to the few existing PA programs.
Suggestions for PA Programming
Participants offered numerous suggestions to increase PA programming that included tailoring PA programs to the needs and culture of rural Appalachian Kentucky. Specifically, participants suggested partnering with the well-established institutions of churches and the U.S. Department of Agriculture’s Cooperative Extension Service (Extension), designing programs with the needs of extended families in mind, incorporating culturally-relevant activities into PA programs, and making sure programs are well-advertised and focus on health rather than appearance.
Partnership with Churches
Participants provided many reasons why partnerships with churches would be successful, including easy access for nearby residents, ability of the church to disseminate information about PA programs, and the close fit between spirituality and health. A long-term resident and VISTA volunteer expressed, “I think that churches are a wonderful means for overall wellness. In our communities, faith is a very important part of our lives… Most people are affiliated with a church, even if it is a family member’s church, and that makes it a good way to get the word out.” A FG participant noted, “Having the spiritual component is important,” while another felt that “you can reach some people just on the spiritual level.”
Other participants felt that certain activities that might be included in PA programs would be inappropriate in a church. A FG participant said, “Some of our churches don’t approve of a dancing group.” Furthermore, participants cautioned that if one did partner with a church to develop a PA program, and music was to be included, program developers would have to carefully select music that was deemed appropriate by the church.
Partnership with the USDA Cooperative Extension Service
Participants discussed the success of existing Extension programs. Several wellness programs currently sponsored by Extension were viewed favorably, including the national program, ‘Second Sunday,’ and the local ‘Get Healthy, Kentucky.’ One GKI stated that, “The Extension office, their focus on physical activity has a program that is called ‘Get Healthy, Kentucky,’ and it has a combination of nutrition and exercise…the motto to that class was ‘Eat better. Move More’…I like the simplicity of that motto.”
Programs for the Entire Family
Many participants noted that “having family time is a big aspect to not leave out” of PA programs in these communities. Some participants advocated for having people of all ages workout together, while others felt that hosting family events, but separating people by age, would be more beneficial. One FG participant felt PA programs need to “keep everyone interested and give them all something to do.” Another stated, “I also think that child supervision is necessary. I am not going to leave my grandson with just anyone and tell him that I will get back in two hours and get you.” Participants also felt that, if childcare was provided at a PA facility, the children should be active, rather than waiting passively for their parents or guardians to finish working out.
Participants suggested that those who participate in PA programs could take the lessons they learned home to other family members, thereby extending limited community resources. A registered nurse who works at a school felt that, “You have to start with the parents and then have them take it home for their family. Parents have to be the ones that want to make a change for the better because without them pushing their children, they will not want to do anything other than sit on the couch and play video games.” A church director felt that the exchange of information between parents and children was not always so unidirectional. She noted, “I have seen this through church, when the children start coming and then the parents just follow along because it is something that they are interested in. I don’t think that we should underestimate the influence that children have over their parents.”
Culturally-Relevant Activities
Participants emphasized the importance of offering culturally-relevant PA programming. A health department administrator warned, “You also have to think again about the people. What would they like to do? Yoga for [coal] miners would not go very well.” Dancing, both traditional square dances and more contemporary line and couples dances, was perceived as promising and consistent with culturally-acceptable activity. One FG participant noted, “Line dancing is just like aerobics, and you don’t have to have a partner, and it’s fun, and people would go for a program like that.” However, a GKI cautioned not to assume uniformity across rural Appalachia, noting, “Just having a county by county plan [is important], because what works in one place might not work for another.”
Participants recommended striking a careful balance between appealing to cultural norms and avoiding stereotyping and generalizations. While one participant said, “I think that comes back to the educational piece. We need to teach people how to change for the better,” another warned against “…just telling people that their lifestyle is bad. Most of them already know that it is bad; you have to make them want to do something about it.”
Well-Advertised
Participants pointed out that programs needed to be advertised, noting that some programs in the area were not well-advertised, which led to low attendance and closures. A worker at a local community center reported, “There have been a few [programs] that just have failed to get the word out that have not been as successful as if they would have advertised more. I think that there are some people that just don’t know.”
Health Rather than Appearance Focus
Although many participants indicated that improvement in appearance was a benefit of PA, others expressed concern about emphasizing appearance. A school aide with children of her own cautioned that the focus on appearance should not be paramount in promoting PA, particularly when youth are involved. She warned that, “We also need to work with the schools on self-image and what is healthy in terms of being too skinny. Children have in their mind the image of a supermodel and that they think they are healthy because they are beautiful. That is not the case, and we need to do a better job at letting them know that.”
Conclusions
Local perceptions and recommendations must be the starting point for enhancing PA and health promotion in general, including consideration of preferred terminology, perceived barriers, and desired program attributes. These formative data collection efforts have equipped us with insights to implement a culturally-appropriate intervention. Because our participants perceive the term ‘physical activity’ more positively than ‘exercise,’ we recommend that those attempting to increase energy expenditure in Appalachia orient programs around the PA term.
Although our study intention was not exclusively oriented toward organized PA programs, most participants discussed group-based rather than individual lifestyle suggestions as ways to increase PA in their community. Since discussion questions focused on programs designed to increase PA, participants may have assumed our interest was in organized PA programming. Additionally, participants may view lifestyle PA, including walking or household chores using physical labor, as a “given” (i.e., they are already doing this, so they may feel that encouraging more walking, etc. will not boost PA levels). Finally, participants are well aware that certain lifestyle activities are not always feasible in the mountain terrain. Narrow mountain roads, for example, lack shoulders and coal and logging trucks make it dangerous to walk, jog, or ride a bicycle. Some participants did suggest efforts to increase lifestyle PA, such as working with community members to build walking trails, but participants themselves tended to emphasize more programmatic approaches.
As with previous work on barriers to PA in other underserved populations, the results of this study indicate that careful attention must be paid to Appalachian residents’ perceptions of time constraints due to distances to resources13 and their family and household responsibilities.12 While rural life often is perceived as idyllic, pastoral, and relaxed, where the vagaries of urban life and industrialization have not encroached,36 this research, along with previous research on rural women’s barrier to PA,12 dispels some of those images. Geographic isolation and long distances to resources require greater travel time to destinations, thus compressing activities into shorter time spans. Providing a variety of opportunities for PA in diverse locations throughout rural Appalachia may allow residents to more easily access PA programs than is possible when programs are located in the region’s population centers. Since one’s perceived time available has been correlated with participation in both supervised and spontaneous exercise programs,37 interesting, innovative programs that can be compressed into small pockets of available time may be in order.
Throughout this study participants emphasized the importance of local facilities to meet their PA needs, but commercially-based PA programs such as fitness centers may be beyond the ability of local communities to support. Since the FG were conducted in churches, it is not surprising that many participants suggested that partnering with local churches would provide useful venues for organized PA programs. Smaller churches tend to be dispersed throughout the region, meaning that virtually every resident lives relatively near at least one church. Many of the larger churches already use buses to transport people to religious services on Sundays and Wednesday evenings, providing a model of how to decrease transportation problems and improve attendance rates. Given the wide diversity of churches in the region, tailoring a PA program to faith communities offers both a challenge and an opportunity. In addition, use of institutional resources such as Extension or school systems could play a key role in initiating and maintaining PA programs. Since Extension serves every county of the state, its familiarity and visibility, particularly among middle-aged and older adults, make it an ideal institution to launch and sustain PA programming. Evidence suggests that many rural residents favor policies such as allocation of government funds (e.g., to Extension) to increase PA,38 and policy initiatives have led to considerable improvement in PA level.39
With family involvement serving as a facilitator of PA,14 domestic and other responsibilities must be addressed through innovative programming in order to minimize perceptions of competing demands. If families are involved together, people can engage in PA as a group, use economies of scale, and reinforce positive health practices. Partnerships between churches, Extension, school systems, local health departments, and other community institutions might develop creative ways of accomplishing those goals, perhaps through family nights with PA and healthy potlucks. In rural Appalachia, a sparsely populated region with people who generally place high value on family ties40–41 and remain in the community for multiple generations,42 programs that appeal to the entire family may have a greater chance of success than programs designed for the more atomistic orientation of many urban locales.43–44
Rural residents are generally seen as being more physically active than non-rural residents because of the farming, mining, and other physically demanding jobs assumed to be commonplace. However, just as the image of rural life being bucolic and unhurried is increasingly contested, so too is the assumption that rural dwellers engage exclusively in physically taxing work. In the present study, as with previous research,45 it is unclear whether those participants reporting being too tired after a day at work to engage in PA have physically demanding jobs or just are mentally fatigued after a day at work. Future research is needed to delineate actual patterns of PA that takes place at work, particularly in rural environments, to determine whether or not some residents are engaging in adequate levels of PA without participating in additional, organized activity. Programs that encourage individuals to rise above personal limitations such as fatigue after a day of work may more successfully engage participants as they “foster internally directed exercise and wellness behaviors,” which have been associated with increased PA.46
PA program developers and researchers in Appalachia and elsewhere walk a fine line between trying to create culturally-appropriate programs (a facilitator of PA in other underserved populations)15 and stereotyping the residents. Although generalizations can be useful for generating questions regarding what may appeal to Appalachian residents, one cannot stop there. PA program developers should ask what programs appeal to the specific local population and focus on developing culturally-relevant programs that appeal to a variety of potential participants.47 For example including square or line dancing or an educational component in a PA program may conform to stereotypes of the region, but developing programs that involve such a focus may also be warranted. On the other hand, uptake of technology is very rapid among many rural residents,48–50 so integration of Wiis or web-based PA support may resonate with many Appalachian residents. Clearly, these divergent perspectives require a careful handling of messages, as does establishing culturally-relevant, but not stereotypical or over-generalizing programming.
This study is limited by having utilized churches as recruitment venues and the predominance of married, female participants. Although many Appalachian residents attend church,27 and given that the current research serves as a foundation for a faith-based intervention, our procedures were appropriate for our aims, but caution is warranted in seeking to generalize these findings to non-church-goers and other Appalachian and rural residents. In addition, because the vast majority of our participants were married and female, our results will be less applicable to men or unmarried women. Future research in this region regarding perspectives on PA should, therefore, seek to recruit non-church-goers, men, and unmarried women. Finally, although we employed rigorous qualitative methods, our data analysis may have been strengthened by having all transcripts co-coded by two researchers rather than just a subset of transcripts.
So What?
What is already known on this topic?
Americans in general, and particularly rural Appalachians, engage in less PA than recommended and often suffer poor health as a consequence. Understanding perceptions of PA and PA programs can offer insights into why people participate in organized programs and how to increase their PA.
What does this article add?
This article explores Appalachian residents’ perceptions of barriers to and potential facilitators of PA and begins to rectify the dearth of information on these topics. Community-relevant and -supported PA programs may help stem the significant health inequities suffered by Appalachian residents.
What are the implications for health promotion practice or research?
This information should help researchers and other PA program planners in rural Appalachia and similar regions create opportunities for individuals and families to engage in good health behavior, which is likely to promote the health and well-being of typically underserved populations.
Acknowledgments
Support for this research was provided by the National Institutes of Health through a grant (R01 DK081324-01) made to Nancy E. Schoenberg, Ph.D.
Contributor Information
Tina M. Kruger, University of Kentucky, Graduate Center for Gerontology, 900 S. Limestone, 304 Wethington, Lexington, KY 40536-0200, Tel. (859) 257-1450 x80195, Fax. (859) 323-5747, tina.kruger@uky.edu.
Mark Swanson, University of Kentucky, Department of Health Behavior, College of Public Health, 121 Washington Avenue, Ste. 111B, Lexington, KY 40536-0003, Tel: (859) 218-2060, Fax: (859) 323-2933, mark.swanson@uky.edu.
Rian E. Davis, University of Kentucky, Department of Anthropology, 211 Lafferty Hall, Lexington, KY 40536-0024, Tel.859-257-2710, Fax.859-323-1959, rian.e.davis@gmail.com.
Sherry Wright, 298A Main Street, Whitesburg, KY 41858, Tel: (606) 622-2229, Fax: (606) 633-3311, wright.sherry@gmail.com.
Katie Dollarhide, 298A Main Street, Whitesburg, KY 41858, Tel. (606) 633-3339, Fax: (606) 633-3311, katie.dollarhide@gmail.com.
Nancy E. Schoenberg, University of Kentucky, Behavioral Science, 125 College of Medicine Office Bldg., Lexington, KY 40536-0086, Tel: (859) 323-8175, Fax: (859) 323-5350, nesch@uky.edu.
References
- 1.Physical Activity Guidelines Advisory Committee. Physical Activity Guidelines Advisory Committee Report, 2008. Washington, DC: Department of Health and Human Services; 2008
- 2.Blair SN, Morris JN. Healthy hearts--and the universal benefits of being physically active: Physical activity and health. Ann Epidemiol. 2009;19:253–256. doi: 10.1016/j.annepidem.2009.01.019. [DOI] [PubMed] [Google Scholar]
- 3.Lollgen H, Bockenhoff A, Knapp G. Physical activity and all-cause mortality: An updated meta-analysis with different intensity categories. Int J Sports Med. 2009;30:213–224. doi: 10.1055/s-0028-1128150. [DOI] [PubMed] [Google Scholar]
- 4.Unger JB. Sedentary lifestyle as a risk factor for self-reported poor physical and mental health. Am J Health Promot. 1995;10:15–17. doi: 10.4278/0890-1171-10.1.15. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. US Physical Activity Statistics. [Accessed on November 30];2009 Available at: http://apps.nccd.cdc.gov/PASurveillance/StateSumResultV.asp.
- 6.Foundation for a Healthy Kentucky. Lack of Physical Activity (percent adults) [Accessed November 30];2009 Available at: http://www.kentuckyhealthfacts.org/data/topic/map.aspx?ind=4.
- 7.Kentucky Department for Public Health Division of Adult and Child Health Improvement. Frankfort, KY: Nutrition Services Branch; The Kentucky Nutrition & Physical Activity State Action Plan 2005. 2005
- 8.Friedell GH, Rubio A, Maretzki A, et al. Community cancer control in a rural, underserved population: The Appalachia Leadership Initiative on Cancer Project. J Health Care Poor Underserved. 2001;12:5–19. doi: 10.1353/hpu.2010.0523. [DOI] [PubMed] [Google Scholar]
- 9.An Analysis of the Financial Conditions of Health Care Institutions in the Appalachian Region and their Economic Impacts. 2002. [Accessed June 1];2007 Available at: http://www.arc.gov/index.do?nodeId=1647.
- 10.United States Congress. Washington, DC: Government Printing Office; Health Care in Rural America. 1990
- 11.Fletcher GM, Behrens TK, Domina L. Barriers and enabling factors for work-site physical activity programs: A qualitative examination. J Phys Act Health. 2008;5:418–429. doi: 10.1123/jpah.5.3.418. [DOI] [PubMed] [Google Scholar]
- 12.Wilcox S, Castro C, King AC, Housemann R, Brownson RC. Determinants of leisure time physical activity in rural compared with urban older and ethnically diverse women in the United States. J Epidemiol Community Health. 2000;54:667–672. doi: 10.1136/jech.54.9.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sloane D, Nascimento L, Flynn G, et al. Assessing resource environments to target prevention interventions in community chronic disease control. J Health Care Poor Underserved. 2006;17:146–158. doi: 10.1353/hpu.2006.0094. [DOI] [PubMed] [Google Scholar]
- 14.Belza B, Walwick J, Shiu-Thornton S, Schwartz S, Taylor M, LoGerfo J. Older adult perspectives on physical activity and exercise: Voices from multiple cultures. Prev Chronic Dis. 2004;1:A09. [PMC free article] [PubMed] [Google Scholar]
- 15.Yancey AK, Ory MG, Davis SM. Dissemination of physical activity promotion interventions in underserved populations. Am J Prev Med. 2006;31:S82–S91. doi: 10.1016/j.amepre.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 16.Shores KA, West ST, Theriault DS, Davison EA. Extra-individual correlates of physical activity attainment in rural older adults. J Rural Health. 2009;25:211–218. doi: 10.1111/j.1748-0361.2009.00220.x. [DOI] [PubMed] [Google Scholar]
- 17.O'Hara Tompkins N, Zizzi S, Zedosky L, Wright J, Vitullo E. School-based opportunities for physical activity in West Virginia public schools. Prev Med. 2004;39:834–840. doi: 10.1016/j.ypmed.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 18.Airhihenbuwa CO, Kumanyika S, Agurs TD, Lowe A. Perceptions and beliefs about exercise, rest, and health among African-Americans. Am J Health Promot. 1995;9:426–429. doi: 10.4278/0890-1171-9.6.426. [DOI] [PubMed] [Google Scholar]
- 19.Satariano W. Epidemiology of aging: An ecological approach. Sudbury, MA: Jones and Bartlett Publishers, Inc; 2005. Aging, health and the environment: An ecological model; pp. 39–77. [Google Scholar]
- 20.Bernard H. Research Methods in Anthropology. Walnut Creek, CA: Altamira; 2002. [Google Scholar]
- 21.Lewis MJ, West B, Bautista L, Greenberg AM, Done-Perez I. Perceptions of service providers and community members on intimate partner violence within a Latino community. Health Educ Behav. 2005;32:69–83. doi: 10.1177/1090198104269510. [DOI] [PubMed] [Google Scholar]
- 22.Friedell G, Linville L, Hullet S. Cancer control in rural Appalachia. Cancer. 1998;83 suppl:1868–1871. [Google Scholar]
- 23.Appalachian Regional Commission. Demographic and health information. [Accessed December 21];2009 Available at: http://www.arc.gov/index.do?nodeId=56.
- 24.Appalachian Regional Commission. Poverty Rates, 2000. [Accessed May 3];2010 Available at: http://www.arc.gov/reports/custom_report.asp?REPORT_ID=11.
- 25.Appalachian Regional Commission. Appalachian Region Income Report, 2009. [Accessed May 3];2010 Available at: http://www.arc.gov/images/appregion/AppalachianIncomeReport2009%282007Data%29.pdf.
- 26.The Health of Kentucky: A County Assessment. Lexington, KY: Kentucky Institute of Medicine; 2007. Kentucky Institute of Medicine. [Google Scholar]
- 27.American religious identification survey. [Accessed July 15];2007 Available at: http://www.gc.cuny.edu/faculty/research.briefs/aris/aris_index.htm.
- 28.Behringer B, Friedell GH, Dorgan KA, et al. Understanding the challenges of reducing cancer in Appalachia: Addressing a place-based health disparity population. Californian J Health Promot. 2007;5:10. [Google Scholar]
- 29.Luborsky M, Rubenstein R. Sampling in qualitative research. Res Aging. 1995;17:89–113. doi: 10.1177/0164027595171005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patton MQ. Qualitative Research and Evaluation Methods. 3rd ed. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 31.Morgan D. Focus Groups as Qualitative Research. Thousand Oaks, CA: Sage; 1997. [Google Scholar]
- 32.MacQueen KM, McLellan E, Milstein KK, Milstein B. Codebook development for team-based qualitative analysis. Cultural Anthropology Methods. 1998;10:6. [Google Scholar]
- 33.Weston C, Gandell T, Beauchamp J, McAlpine L, Wiseman C, Beauchamp C. Analyzing interview data: The development and evolution of a coding system. Qual Sociol. 2001;24:15. [Google Scholar]
- 34.Morse JM, Swanson JM, Kuzel AJ, editors. The Nature of Qualitative Evidence. Thousand Oaks, CA: Sage Publications, Inc; 2001. [Google Scholar]
- 35.Boyatzis RE. Transforming Qualitative Information: Thematic Analysis and Code Development. Thousand Oaks, CA: SAGE Publications, Inc.; 1998. [Google Scholar]
- 36.Masuda JR, Garvin T. Place, culture, and the social amplification of risk. Risk Anal. 2006;26:18. doi: 10.1111/j.1539-6924.2006.00749.x. [DOI] [PubMed] [Google Scholar]
- 37.Dishman RK. Exercise adherence research: Future directions. Am J Health Promot. 1988;3:5. doi: 10.4278/0890-1171-3.1.52. [DOI] [PubMed] [Google Scholar]
- 38.Brownson RC, Schmid TL, King AC, et al. Support for policy interventions to increase physical activity in rural Missouri. Am J Health Promot. 1998;12:263–266. doi: 10.4278/0890-1171-12.4.263. [DOI] [PubMed] [Google Scholar]
- 39.Sharpe PA, Granner ML, Hutto B, Ainsworth BE. Association of environmental factors to meeting physical activity recommendations in two South Carolina counties. Am J Health Promot. 2004;18:251–257. doi: 10.4278/0890-1171-18.3.251. [DOI] [PubMed] [Google Scholar]
- 40.Small C. Appalachians. In: Giger JN, Davidhizar RE, editors. Transcultural Nursing: Assessment & Intervention. St. Louis, MO: Mosby, Inc; 2004. [Google Scholar]
- 41.Sortet JP, Banks SR. Health beliefs of rural Appalachian women and the practice of breast self-examination. Cancer Nurs. 1997;20:231–235. doi: 10.1097/00002820-199708000-00001. [DOI] [PubMed] [Google Scholar]
- 42.Appalachian Regional Commission. Demographic Characteristics. [Accessed May 5];2009 Available at: http://www.arc.gov/index.do?nodeId=1842.
- 43.Denham SA. Family routines: A structural perspective for viewing family health. ANS Adv Nurs Sci. 2002;24:60–74. doi: 10.1097/00012272-200206000-00010. [DOI] [PubMed] [Google Scholar]
- 44.Lohri-Posey B. Middle-aged Appalachians living with diabetes mellitus. Fam Community Health. 2006;29:7. doi: 10.1097/00003727-200607000-00008. [DOI] [PubMed] [Google Scholar]
- 45.Burton NW, Turrell G. Occupation, hours worked, and leisure-time physical activity. Prev Med. 2000;31:673–681. doi: 10.1006/pmed.2000.0763. [DOI] [PubMed] [Google Scholar]
- 46.Field LK, Steinhardt MA. The relationship of internally directed behavior to self-reinforcement, self-esteem, and expectancy values for exercise. Am J Health Promot. 1992;7:21–27. doi: 10.4278/0890-1171-7.1.21. [DOI] [PubMed] [Google Scholar]
- 47.Galanti GA. An introduction to cultural differences. West J Med. 2000;172:335–336. doi: 10.1136/ewjm.172.5.335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Setting the pace: Accelerating Broadband Expansion. [Accessed August 3];2010 Available at: http://www.connectkentucky.org/_documents/ConnectKentuckyProgressReport2008.pdf.
- 49.Rural broadband internet use. Pew Internet and American Life Project. [Accessed August 3];2010 Available at: http://www.pewinternet.org/Reports/2006/Home-Broadband-Adoption-in-Rural-America.aspx.
- 50.Stoops WW, Dallery J, Fields NM, et al. An internet-based abstinence reinforcement smoking cessation intervention in rural smokers. Drug Alcohol Depend. 2009;105:56–62. doi: 10.1016/j.drugalcdep.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]