Abstract
Background
Biofilms contribute to the pathogenesis of many forms of Staphylococcus aureus infection. Treatment of these infections is complicated by intrinsic resistance to conventional antibiotics, thus creating an urgent need for strategies that can be used for the prevention and treatment of biofilm-associated infections.
Methodology/Principal Findings
This study demonstrates that a botanical natural product composition (220D-F2) rich in ellagic acid and its derivatives can limit S. aureus biofilm formation to a degree that can be correlated with increased antibiotic susceptibility. The source of this composition is Rubus ulmifolius Schott. (Rosaceae), a plant used in complementary and alternative medicine in southern Italy for the treatment of skin and soft tissue infections. All S. aureus clonal lineages tested exhibited a reduced capacity to form a biofilm at 220D-F2 concentrations ranging from 50–200 µg/mL, which were well below the concentrations required to limit bacterial growth (530–1040 µg/mL). This limitation was therapeutically relevant in that inclusion of 220D-F2 resulted in enhanced susceptibility to the functionally-distinct antibiotics daptomycin, clindamycin and oxacillin. Testing with kidney and liver cell lines also demonstrated a lack of host cell cytotoxicity at concentrations of 220D-F2 required to achieve these effects.
Conclusions/Significance
These results demonstrate that extract 220D-F2 from the root of Rubus ulmifolius can be used to inhibit S. aureus biofilm formation to a degree that can be correlated with increased antibiotic susceptibility without toxic effects on normal mammalian cells. Hence, 220D-F2 is a strong candidate for development as a botanical drug for use in the prevention and treatment of S. aureus biofilm-associated infections.
Introduction
Staphylococcus aureus is arguably the most problematic of all bacterial pathogens owing in large part to the persistent emergence of antibiotic resistant strains. This is evident in the recent appearance of methicillin-resistant strains even among isolates causing community-acquired infections [1], [2], [3]. While this has created an urgent need for new antimicrobial agents, many S. aureus infections are recalcitrant to antimicrobials even in the absence of issues related to acquired-antibiotic resistance. A primary contributing factor to this recalcitrance is the formation of a biofilm. Indeed, the National Institutes of Health estimates that 80% of all bacterial infections are biofilm related [4]. In addition to their impact on antimicrobial therapy, bacteria within biofilms reach a much higher density (1011 CFU/mL) than their planktonic counterparts (108 CFU/mL) [5], thus increasing the opportunity for gene transfer and the emergence of strains with new resistance and/or virulence profiles. The presence of a foreign body decreases the minimal infecting dose of S. aureus >100,000-fold [6], thus significantly increasing the chances of a biofilm-associated infection by comparison to individuals without such devices. In most cases, treatment of such biofilm-associated infections requires both aggressive antimicrobial treatment and surgical debridement to remove all infected tissues and/or indwelling medical devices [7], [8].
The paradigm of biofilm resistance presents a major hurdle for the treatment of many types of infectious disease, including dental caries, mastitis, otitis media, endocarditis, chronic wounds, and osteomyelitis [5]. The economic burden of these infections is tremendous with biofilm-associated infections lead to longer hospital stays, recurrent infection, and increased fatalities in the most recalcitrant cases. In total, up to 17 million new biofilm infections occur each year in the US, resulting in up to 550,000 fatalities annually [9], [10]. These statistics emphasize the fact that, while there is indeed a pressing need for new antibiotics, there is an equally urgent need to develop agents that could be used to limit biofilm formation to a therapeutically relevant degree. Such agents could be used to prevent colonization or as adjunct therapy to enhance the therapeutic efficacy of conventional antibiotics [10], [11].
Taking an ethnobotanical approach to drug discovery [12] offers considerable promise in many clinical contexts including infectious disease. Indeed, studies on botanical complementary and alternative (CAM) therapies have led to the discovery of novel ant-virulence agents. For instance, proanthocyanidins from Vaccinium macrocarpon (cranberry) disrupt adhesion of P-fimbriated E. coli to uroepithelial cells [13], [14], accounting for efficacy in preventing recurrent urinary tract infections [15]. Garlic extract (Allium sativum) attenuates virulence by inhibiting hyphae formation in Candida albicans [16] and by blocking quorum sensing in Pseudomonas aeruginosa [17], [18], [19]. In S. aureus, inhibitors of quorum sensing, biofilm formation, and the NorA efflux pump have all been isolated from botanical sources [20], [21], [22], [23], [24], [25], [26], [27], [28], [29]. Natural products offer a distinct advantage over their synthetic counterparts due to their rich structural diversity, chirality, and extensive functional group chemistry [24]. Thus, plants are a likely source of the next generation of anti-infectives [30].
Rubus ulmifolius Schott., Rosaceae (Elmleaf blackberry) is a wild shrub native to the Mediterranean. A limited number of published studies that have examined the antibacterial properties of R. ulmifolius. For example, Flamini et al. [31] identified an anthrone (Rubanthrone A) in the leaves, branches and flowering tops of R. ulmifolius that had an MIC of 4,500 µg/mL against S. aureus (ATCC 25923). Panizzi et al. [32] examined a crude extract of R. ulmifolius leaves, flowering tops and branches as well as subsequent extracts of increasing polarity for antibacterial activity using the same S. aureus strain and found that the greatest activity was present in the crude extract. The importance of R. ulmifolius as a traditional medicine was highlighted in an ethnobotanical field study conducted in rural communities of southern Italy [33]. In particular, the fresh leaves are topically applied with pork fat in the treatment of skin and soft tissue infections (SSTI) and a decoction of the roots is used as a wash to prevent hair loss. In a screening study that followed this fieldwork, ethanolic extracts from 104 Italian plants were assessed for their anti-biofilm potential and extracts from R. ulmifolius and nine other species were found to show some promise [28]. Here, we expanded on this work to determine whether bioassay-guided fractionation could be used to isolate a more potent extract of R. ulmifolius and whether this extract could limit biofilm formation in genotypically and phenotypically-diverse strains of S. aureus to a degree that can be correlated with increased antibiotic susceptibility.
Results
Bioassay-guided fractionation of the active constituents
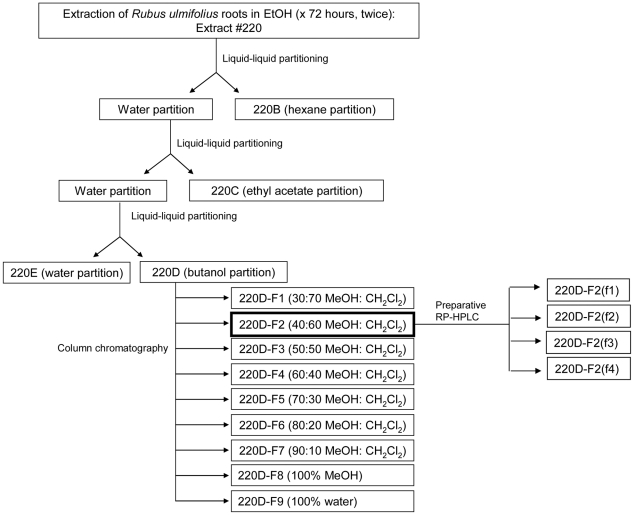
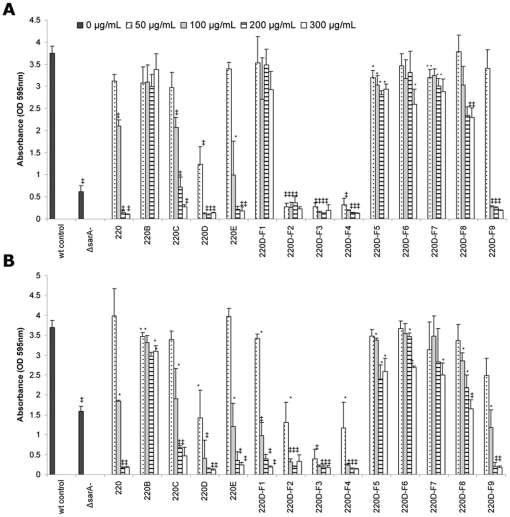
Fractionation of the crude ethanolic root extract was done as illustrated in Fig. 1. The activity of each fraction was assessed based on the ability to limit biofilm formation in a microtiter plate assay using the methicillin-sensitive (MSSA) strain UAMS-1 and the methicillin-resistant (MRSA) USA300 isolate FPR3757 (UAMS-1782). The greatest degree of inhibition was observed in the butanol partition of the aqueous phase obtained after successive extraction with hexane and ethyl acetate (Fig. 2). Further partitioning of the butanol extract with MeOH∶CH2Cl2 demonstrated that the greatest activity was observed with fractions ranging from 40∶60 to 60∶40 MeOH∶CH2Cl2 (220D-F2, 220D-F3 and 220D-F4). In fact, all three of these fractions limited biofilm formation in this assay in a dose dependent manner and to a degree that exceeded that observed with mutation of sarA (Fig. 2). Moreover, biofilm assays confirmed that the activity in these extracts was increased by comparison to the crude extract while activity in other MeOH∶CH2Cl2 extracts was decreased. This was true with both UAMS-1 and UAMS-1782 although at the lowest concentration tested (50 µg/mL) inhibition was slightly greater with the former by comparison to the latter (Fig. 2). While comparable inhibition was observed with the 220D-F2, 220D-F3 and 220D-F4 partitions, overall yield was greatest with 220D-F2 with a percent yield of 0.329% of dry root weight (3.29 g per kg of dry root weight). For this reason, 220D-F2 was selected for subsequent experiments.
Figure 1. Fractionation scheme for the separation of anti-biofilm constituents found in the roots of Rubus ulmifolius.
Figure 2. Biofilm inhibition of R. ulmifolius root extracts.
A static microtiter plate biofilm assay which employed crystal violet as a biofilm matrix staining agent was used to assess the inhibitory activity of individual fractions from the R. ulmifolius root using UAMS-1 (A) or the USA300 isolate UAMS-1782 (B) as the wild-type (wt) test strains. Isogenic sarA mutants for each strains were included as controls. Other designations refer to the specific extract as defined by the fractionation scheme illustrated in Figure 1. The MBICs for the crude EtoH extract (220), butanol partition (220D), and 40∶60 (220D-F2), 50∶50 (220D-F3), and 60∶40 (220D-F4) MeOH∶CHCl2 fractions from the butanol partition were 200, 100, 50, 50 and 50 µg/mL, respectively in both UAMS-1 and UAMS-1782. Statistical significance (*, P<0.05; ‡, P<0.001) refers to differences observed in each parent strain with and without the indicated extract at the indicated concentration.
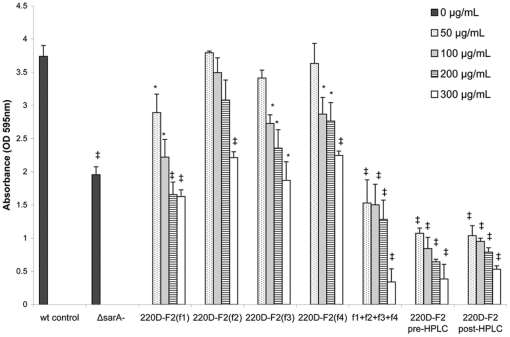
A preparative reversed-phase high-performance liquid chromatography (RP-HPLC) method was developed to further separate 220D-F2 into four fractions. Bioassays for biofilm inhibition with these fractions revealed that no single fraction was more effective than 220D-F2 itself, suggesting that more than one fraction was necessary for the anti-biofilm activity (Fig. 3). Thus, additional experiments were conducted in which fractions were combined in all possible permutations and tested for activity (data not shown). The only combination in which activity was restored was when all four fractions were recombined (Fig. 3). These results were also compared with 220D-F2 before and after running through the HPLC system to determine if the separation protocol itself had any effect on the activity. No significant difference between samples could be determined. These data suggest that the anti-biofilm effect of 220D-F2 is due to the synergistic activity of multiple compounds, and that the relative proportions of this mixture is important to the activity.
Figure 3. Biofilm inhibition by fractions of 220D-F2.
A static crystal violet microtiter plate biofilm assay was used to assess the inhibitory activity of fractions of 220D-F2 both alone and in combination using UAMS-1. No single fraction of 220D-F2 exhibited improved biofilm-inhibiting activity over 220D-F2 as a whole. Multiple combinations of the fractions were made and the only combination which resulted in restoration of activity on the same level as 220D-F2 was when all 4 fractions (f1+f2+f3+f4) were recombined. Likewise, a single collection, in which 220D-F2 was run through the HPLC system and collected as a whole (instead of splitting into fractions) also resulted in the same level of activity as the original 220D-F2. These findings suggest that multiple components found in extract 220D-F2 are necessary for the anti-biofilm activity. Statistical significance (*, P<0.05; ‡, P<0.001) refers to differences observed in comparison to the untreated control.
Identification of Active Constituents
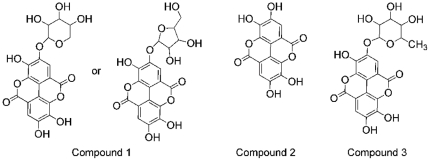
LC-UV/MS/MS (liquid chromatography-ultraviolet absorption-tandem mass spectrometry) studies on 220D-F2 revealed the presence of ellagic acid (EA) and several ellagic acid derivatives (EADs) or sapogenin-related compounds. Molecular formulas of C14H6O8, C20H16O12, C19H14O12, C30H46O7, C30H46O8 (Table 1) were identified and confirmed with accurate mass measurements (<5 ppm). Possible structures for three of these components (C14H6O8, C20H16O12, C19H14O12) are shown in Fig. 4. Neutral loss of a pentose group (m/z 132) was observed for peaks 1 (m/z 435) and 3 (m/z 449). A product ion of m/z 303 was observed for both of these peaks suggesting that both components contain an ellagic acid core. A similar product ion was not observed for peaks corresponding to molecular formulae C30H46O7, and C30H46O8 suggesting that these compounds do not contain an ellagic acid core. Likely structures of minor constituents in 220D-F2 could not be determined from these studies.
Table 1. Compounds detected in extract 220D-F2 by accurate mass LC/UV/MS/MS.
| # | Proposed Compound† | Molecular Formula | Retention Time (minutes) | [M+H]+ m/z | MS-MS Fragmentation (m/z) |
| 1 | Ellagic acid xylopyranoside or Ellagic acid xylofuranoside | C19H14O12 | 10.9 | 435.05594 | 303.01346 |
| 2 | Ellagic acid | C14H6O8 | 11.1 | 303.01354 | 285.00281, 275.01868, 259.02338, 241.01314 |
| 3 | Ellagic acid mannopyranoside | C20H16O12 | 11.1 | 449.07158 | 352.33952, 303.01366, 249.11220, 182.98514 |
| 4 | unknown | unknown | 11.5 | 437.97815 | 409.09189, 303.01351, 219.10153, 182.98507 |
| 5 | Sapogenin derivative | C30H46O8 | 13.5 | 535.32637 | 517.31604, 499.30499, 481.29480, 469.29486 |
| 6 | Sapogenin derivative | C30H46O7 | 13.7 | 519.33139 and 501.32097 | 501.32071, 483.31012, 473.32559, 455.31543, 437.30457, 409.30994 |
| 7 | unknown | unknown | 14.7 | 573.98540 and 396.98622 | 532.95864, 505.35274, 485.32649, 451.99400, 440.95009, 352.33958, 317.02929, 273.07586, 199.98796, 182.98517 |
| 8 | unknown | unknown | 16.9 | 1017.62898 and 999.61893 | 955.62813, 937.61896, 499.30520, 437.30489 |
Proposed structures corresponding to this data are reported in Figure 4. Of the major UV components identified, the most abundant was EA (#2, MW 302). The second most abundant UV component (#7) did not yield a clear MS signal suggestive of a single species or reasonable molecular formula, and thus no structure is proposed. The third most abundant UV component (#1, MW 434) appears to be EA plus a C5H8O4 moiety. A fourth UV component (#3, MW 448) was found to be consistent with a glyosylated derivative of EA. Investigation of the possible formulae consistent with the mass measurement of the fifth UV component (#4) did not yield sufficient data for proposal of a structure. Of the major MS components, the most abundant (#8) did not yield enough information to support the proposal of a structure, however the molecular weights and mass defects suggest that they may be dimers of MW∼500 species (similar to #6). The second most abundant MS component (#6) is consistent with a sapogenin. Successive loss of water (m/z 18) is consistent with a poly-hydroxylated compound. The third most abundant MS component (#5, MW 534) appears to be similar to #6 and has MS/MS losses consistent with a multiply hydroxylated compound like a sapogenin. Losses consisted with neutral loss of a sugar were not observed.
Figure 4. LC-MS/MS analysis revealed a mixture of ellagic acid and glycosylated ellagic acid derivatives in 220D-F2.
Corresponding ESI(+)-MS and MS/MS data is reported in Table S1. Compound 1. Ellagic Acid xylopyranoside or xylofuanoside Compound 2. Ellagic acid. Compound 3. Ellagic acid mannopyranoside. The configuration for each of the glycosylated ellagic acids could not be confirmed. Neutral loss of m/z 132 was used to confirm the presence of a pentose attached to ellagic acid.
Prophylactic efficacy of 220D-F2 in limiting S. aureus biofilm formation
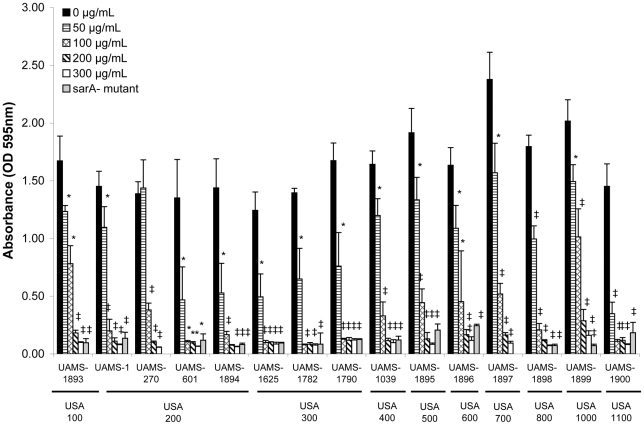
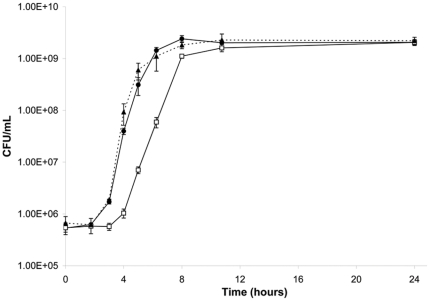
The ability of 220D-F2 to limit biofilm formation was assessed against 15 genotypically-diverse clinical isolates of S. aureus. The MBIC90 for these strains ranged from 50–200 µg/mL (Fig. 5). The MIC and MBC was also determined for all 15 strains, with the MIC90 ranging from 530–1040 µg/mL and the MBC90 from 530–2040 µg/mL (Table 2). The observation that the MBIC90 was at least 2-fold lower than the MIC90 and at least 4-fold lower than the MBC90 indicates that the inhibition of biofilm formation observed with 220D-F2 was due to something other than growth limitation. This was confirmed by demonstrating that, while the presence of the extract did delay entry into the exponential growth phase by ∼2 hours, cultures with and without 220D-F2 reached the same density within 12 hours and maintained the same cell counts throughout the stationary growth phase (Fig. 6).
Figure 5. Anti-biofilm activity of 220D-F2 against genotypically- and phenotypically-diverse strains of S. aureus.
A crystal violet microtiter plate biofilm assay was used to assess the impact of 220D-F2 on biofilm formation. Strain designations are given based on both the corresponding author's culture collection (UAMS) and the clonal lineage of each isolate (USA). Statistical significance (*, P<0.05; ‡, P<0.001) refers to differences between the untreated cultures and cultures exposed to the indicated concentrations. When available, the isogenic sarA mutant for each isolate in the absence of 220D-F2 was included as a control; results obtained with all 15 sarA mutants were significantly different from those obtained with the isogenic parent strain (P<0.001).
Table 2. Activity of 220D-F2 (µg/mL) against wild-type strains of Staphylococcus aureus.
| Growth | Survival | Biofilm Formation | ||||||
| USA Type | Strain I.D. of wild type* | Strain I.D. of sarA mutant | MIC50 | MIC90 | MBC50 | MBC90 | MBIC50 | MBIC90 |
| 100 | UAMS-1893 | UAMS-1941 | 380 | 530 | 530 | 740 | 100 | 200 |
| 200 | UAMS-1 | UAMS-929 | 380 | 530 | 740 | 1040 | 50 | 50 |
| UAMS-270 | - | 380 | 530 | 1460 | 2040 | 100 | 200 | |
| UAMS-601 | UAMS-950 | 530 | 740 | 1460 | 2040 | 50 | 100 | |
| UAMS-1894 | UAMS-1945 | 380 | 530 | 740 | 1040 | 50 | 100 | |
| 300 | UAMS-1625 | UAMS-1653 | 380 | 530 | 530 | 740 | 50 | 100 |
| UAMS-1782 | UAMS-1804 | 380 | 530 | 380 | 530 | 50 | 100 | |
| UAMS-1790 | UAMS-1796 | 380 | 530 | 380 | 530 | 50 | 100 | |
| 400 | UAMS-1039 | UAMS-1938 | 530 | 740 | 530 | 740 | 100 | 200 |
| 500 | UAMS-1895 | UAMS-1942 | 740 | 1040 | 1040 | 1460 | 100 | 200 |
| 600 | UAMS-1896 | UAMS-1943 | 530 | 740 | 530 | 1040 | 100 | 200 |
| 700 | UAMS-1897 | - | 530 | 740 | 530 | 1040 | 100 | 200 |
| 800 | UAMS-1898 | UAMS-1944 | 530 | 740 | 1460 | 2040 | 100 | 200 |
| 1000 | UAMS-1899 | UAMS-1930 | 530 | 740 | 1040 | 1460 | 100 | 300 |
| 1100 | UAMS-1900 | UAMS-1931 | 380 | 530 | 740 | 1460 | 50 | 100 |
*A detailed description of the bacterial strains used in this study has been previously published [52].
Figure 6. Impact of 220D-F2 on S. aureus growth.
Results illustrate growth of UAMS-1 in biofilm medium (BM) supplemented with 200 µg/mL 220D-F2 in 0.2% DMSO (□) or 0.2% DMSO (•) as an excipient control. Growth of the isogenic UAMS-1 sarA mutant (UAMS-929, containing 0.2% DMSO in comparison with untreated wild type (UAMS-1) and sarA mutant (UAMS-929, ▴) is shown for comparison.
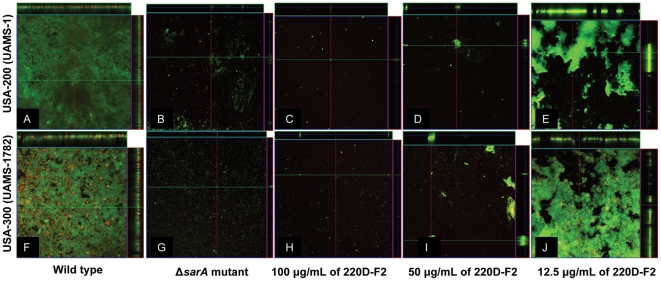
The ability of 220D-F2 to inhibit biofilm formation was also confirmed by confocal microscopy (Fig. 7). At concentrations as low as 50 µg/mL, the degree of inhibition observed with 220D-F2 was comparable to that associated with mutation of sarA in both UAMS-1 and the USA300 isolate UAMS-1782 at concentrations as low as 50 µg/mL. More specifically, the untreated wild-type strains formed uniform biofilms with a thickness ranging from 88–92 µm while the isogenic sarA mutants and parent strains exposed to 220D-F2 formed very patchy biofilms with a few isolated clumps of adherent cells.
Figure 7. Impact of 220D-F2 as assessed by confocal microscopy.
Microtiter plate biofilm assays were undertaken with UAMS-1 (top) or UAMS-1782 (bottom) after the addition of either 220D-F2 at the indicated concentrations or excipient (DMSO) to the growth medium. Confocal images were obtained after 20 hours of incubation. An orthogonal view is included to illustrate overall biofilm architecture at a magnification of 10×. Isogenic sarA mutants grown in BM with DMSO were included as negative controls.
Therapeutic efficacy of 220D-F2 in removal of established S. aureus biofilms
The microtiter plate assay used in the experiments discussed above does not lend itself easily to studies assessing relative antibiotic susceptibility. To address this, we employed an in vitro model of catheter-associated biofilm formation [34]. In order to assess the impact of 220D-F2 relative to an isogenic sarA mutant, we first examined the ability of 220D-F2 to inhibit colonization of the catheters. The total number of viable cells adherent to catheters following exposure to 220D-F2 during colonization was significantly reduced by comparison to the untreated control (P<0.05) and comparable to the number observed with the isogenic sarA mutant. Although the actual reduction in the number of adherent cells was relatively modest (1.23×106 CFU/catheter in the presence of 220D-F2 versus 1.34×107 CFU/catheter in the untreated control), previous work comparing UAMS-1 with its isogenic sarA mutant demonstrated that a similar level of inhibition was sufficient to improve the therapeutic response of a biofilm-associated infection to antimicrobial therapy under both in vitro and in vivo conditions [35].
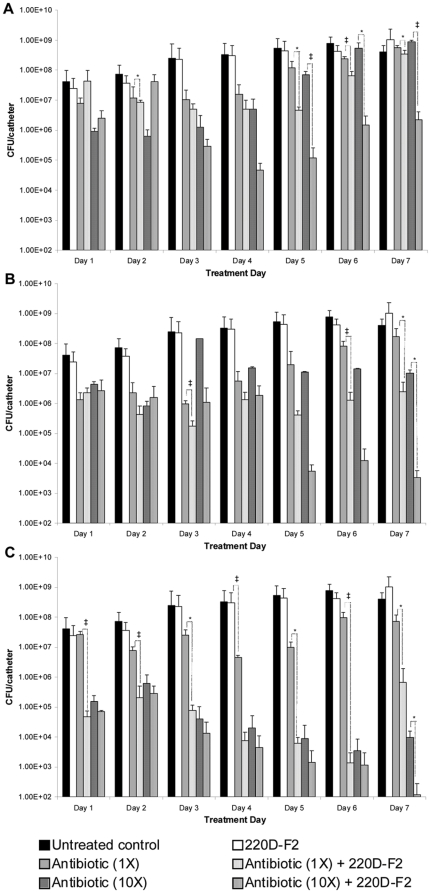
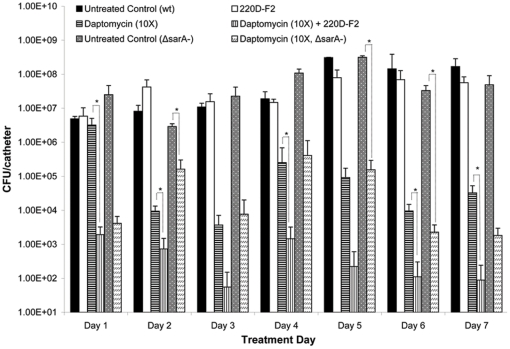
Based on these results, we used the in vitro catheter model to examine the therapeutic efficacy of 220D-F2 with and without concomitant antimicrobial therapy. In the absence of antibiotic, 220D-F2 had no impact on an established biofilm even after 7 consecutive days of exposure (Fig. 8). However, exposure of a UAMS-1 biofilm to 200 µg/mL 220D-F2 concomitantly with different antibiotics (daptomycin, clindamycin, and oxacillin) was shown to offer a significant therapeutic benefit by comparison to antibiotic alone. For example, catheters exposed to 220D-F2 and 10 µg/mL daptomycin (10× breakpoint MIC) exhibited average colony counts of 3.37×103 CFU/catheter while those exposed to daptomycin alone exhibited colony counts of 1.01×107 (Fig. 8). Enhanced efficacy was also observed with clindamycin and oxacillin. For example, exposure to 220D-F2 and clindamycin (10×) for 7 consecutive days resulted in a ∼2.5 log reduction by comparison to antibiotic alone (Fig. 8). Although we did not observe a significant difference between oxacillin and oxacillin+220D-F2 when oxacillin was used at a 10× concentration, when used at a concentration corresponding to the MIC of UAMS-1 (0.5 µg/mL), catheters exposed to 220D-F2 and oxacillin exhibited up to a 2–5 log reduction (depending on the number of days of exposure) by comparison to oxacillin alone (Fig. 8).
Figure 8. Use of 220D-F2 as adjunct therapy with conventional antibiotics.
Biofilms were formed on plasma-coated catheters for 24 hours by growth of the test strain (UAMS-1) in BM. Catheters were then placed in fresh BM containing 200 µg/mL 220D-F2 with or without the indicated amounts of antibiotic. In the case of all three antibiotics, the concentrations examined correspond to 1× or 10× the CLSI-defined breakpoint MIC for a sensitive strain of S. aureus. Statistical significance (*, P<0.05; ‡, P<0.001) refers to differences between the cultures treated with antibiotic alone and cultures exposed to both extract 220D-F2 and antibiotic. A. Clindamycin (1×: 0.5 µg/mL; 10×: 5 µg/mL); B. Daptomycin (1×: 1 µg/mL; 10×: 10 µg/mL); C. Oxacillin (1×: 0.5 µg/mL; 10×: 5 µg/mL).
An experiment in which 220D-F2 was added to the growth medium during biofilm formation and then included with and without daptomycin (10×) during the treatment phase of the experiment was also undertaken. Colony counts in the group exposed to daptomcyin alone were reduced to 3.37×106 CFU/catheter on day 1 while those in the group exposed to both 220D-F2 and daptomycin were reduced to 1.93×103 CFU/catheter (Fig. 9). This effect was even more apparent after 7 days of exposure, with colony counts on catheters exposed to daptomycin alone falling to 3.27×104 CFU/catheter and those exposed to daptomycin and 220D-F2 falling to 8.87×101. Moreover, ≥33% of all catheters exposed to both 220D-F2 and daptomycin were cleared of all adherent cells (lower detection limit of 10 cells/catheter) beginning on day 2 and continuing on all treatment days thereafter.
Figure 9. Prophylactic use of 220D-F2 prior to concomitant antibiotic therapy.
Biofilms were formed on plasma-coated catheters for 24 hours by growth of the test strain (UAMS-1) in BM containing 200 µg/mL 220D-F2. Catheters were then placed in fresh BM containing 200 µg/mL 220D-F2 with or without 10 µg/mL of daptomycin, which corresponds to 10× the CLSI-defined breakpoint MIC for a sensitive strain of S. aureus. Statistical significance (*, P<0.05; ‡, P<0.001) refers to differences between the untreated cultures and cultures exposed to the compounds. Results observed with the isogenic sarA mutant with and without the same concentration of daptomycin but without 220D-F2 are shown for comparison.
Anti-biofilm activity of select R. ulmifolius constituents
Ten commercially available phytochemical constituents reported in the literature [31], [32], [36] to have been isolated from R. ulmifolius (Table 3) were purchased and examined for their prophylactic efficacy in the prevention of biofilm formation using a static microtiter plate biofilm assay. The only compound exhibiting meaningful anti-biofilm activity at doses well below any growth inhibitory effects was EA (Table S1). This finding supports the hypothesis that EA and EADs present in 220D-F2 are responsible for the anti-biofilm properties of the extract.
Table 3. Phytochemicals previously isolated from Rubus ulmifolius [31], [32], [36].
| kaempferol-3-O-(6″-p-coumaroyl)-β-D-glucopyranoside | *quercetin |
| kaempferol-3-O-α-L-arabinopyranoside | rubanthrone A |
| kaempferol-3-O-(6″-feruloyl)-β-D-glucopyranoside | rubanthrone B |
| kaempferol-3-O-β-D-galactoside | rubanthrone C |
| quercetin-3-O-β-D-glucuronide | *caffeic acid |
| quercetin-3-O-β-D-glucoside | tormentic acid |
| quercetin-3-O-α-L-rhamnoside | *ursolic acid |
| *quercetin-3-O-glucuronide | euscaphic acid |
| luteolin-7-O-β-D-glucuronide | *oleanolic acid |
| kaempferol-3-O-glucuronide | 2α-hydroxyursolic acid |
| kaempferol-3-O-β-D-glucuronide | *ferulic acid |
| kaempferol-3-O-β-D-glucoside | *tiliroside |
| tormentic acid-28-glucoside | corosine |
| 23-hydroxy tormentic acid | *gallic acid |
| euscaphic acid-28-glucoside | nigaichigoside |
| ursolic acid-28-glucoside | 3-caffeoylquinic acid |
| 1,4-dicaffeoylquinic acid | 5-caffeoylquinic acid |
| 4-caffeoylquinic acid | *kaempferol |
| *ellagic acid |
*Individual compounds tested for anti-biofilm activity. Results are reported in Table 3.
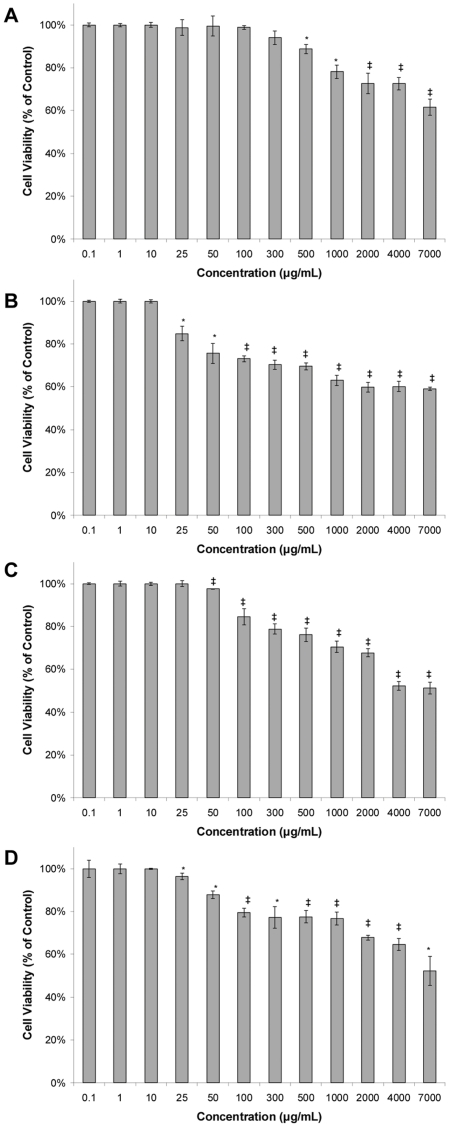
Cytotoxicity of 220D-F2 in normal mammalian cell lines
Normal human (HK-2) and mouse (TKPTS) proximal tubular kidney cells demonstrated very good tolerance for the extract, and no IC50 could be identified even at extremely high doses of 7,000 µg/mL (Fig. 10). Rat kidney (NRK-52E) cells and mouse hepatocytes (AML-12) were slightly more sensitive and had IC50 s of 4,000 and 7,000 µg/mL, respectively. Human kidney cells were the least impacted and a significant effect in decreasing cell viability was notable only at concentrations ≥500 µg/mL. These results are relevant as the active doses for biofilm inhibition range from 50–200 µg/mL (depending on the S. aureus strain) and no or very limited impact (<20%) on cell viability was notable at these concentrations in the cell lines examined.
Figure 10. Cytotoxicity of 220D-F2 against normal mammalian cell lines.
Cytotoxicity was assessed using a lactate dehydrogenase (LDH) test following 24 hours of exposure to the extract. Results are reported as the percent of cell viability after exposure to the indicated dosage of 220D-F2 in the culture growth medium. Statistical significance (*, P<0.05; ‡, P<0.001) refers to differences observed in comparison to the untreated (excipient) control. A. Normal human kidney proximal tubular (HK-2) cells; B. Normal mouse kidney proximal tubular (TKPTS) cells; C. Normal rat kidney (NRK-52E) cells; D. Normal mouse hepatocytes (AML12).
Discussion
In a previous study we demonstrated that an ethanolic extract from the root of R. ulmifolius can be used to limit S. aureus biofilm formation [28]. However, this work was limited to the crude extract and examined only one strain of S. aureus. In this report, we expanded on this work by fractionating the extract and assessing the anti-biofilm properties of the resulting fractions against genotypically and phenotypically-diverse strains of S. aureus. The results confirmed that an EA and EAD-rich fraction (220D-F2) obtained from the roots of R. ulmifolius was effective at preventing S. aureus biofilm formation irrespective of strain identity. While addition of the same fraction had no impact on dispersal of an established biofilm, this limitation was therapeutically relevant in that inclusion of 220D-F2 was associated with enhanced susceptibility to functionally-diverse antibiotics including daptomycin, oxacillin, and clindamycin in the specific context of an established biofilm. Moreover, when the extract was employed both prophylactically during the colonization process and therapeutically in combination with daptomycin, it was possible to completely clear infected catheters of all viable cells.
A few studies [31], [32], [36] have addressed the phytochemical makeup of R. ulmifolius and identified some compounds (Table 3), but it is unlikely that this list is comprehensive. Indeed, the EADs isolated in this study have not been previously reported for R. ulmifolius. Importantly, we demonstrated that EA alone has potent anti-biofilm properties at concentrations (MBIC50<50 µM) well below those that impact bacterial growth (MIC90>2000 µM). This is consistent with the hypothesis that the activity of 220D-F2 is likely to be related to the high content of EA and glycosylated EAs. The decline in activity when 220D-F2 is divided into four separate fractions may be related to the EAD content of the various fractions and possibly the unequal distribution of the most active forms. More work involving the isolation of substantive amounts of individual EADs for further testing and structural elucidation by NMR (nuclear magnetic resonance) is necessary to determine which compound(s) are most efficacious in preventing S. aureus biofilm formation and if they act in a distinctly synergistic fashion when combined.
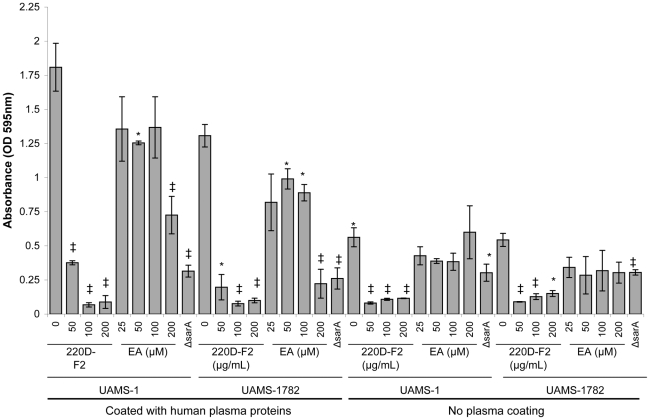
EA is a polyphenol found at high concentrations in a number of edible fruits, such as grapes, strawberries, raspberries, blackberries, and black currants. Berries of the Rosaceae family, in particular, contain high levels of EA equivalents [37]. EA is derived from gallic acid, in which two gallic acid molecules are linked by ester bonds. EA has been the focus of many studies in recent years, primarily related to its antioxidant [38], [39], anti-proliferative [40], anti-estrogenic [41] anti-inflammatory [42], anti-bacterial [37], [43] and protein kinase CK-2 inhibiting [44] effects. Reports concerning the biofilm inhibiting properties of EA against Escherichia coli [45], [46] Streptococcus dysgalactiae [47], Pseudomonas putida [46], and Burkholderia cepacia [46] have also recently emerged. EADs, on the other hand, have been found to have anti-plasmodial [48], anti-babesial [49], antibacterial [50] and antioxidant [50], [51] effects. However, to our knowledge, this is the first report of the anti-biofilm properties of EA and EADs against S. aureus. This is in contrast to Dürig et al. [47], who examined the impact of EA on S. aureus biofilm formation but did not observe any inhibitory activity. This contrast may be attributable to differences in the methodologies employed in the respective studies. Specifically, we employ in vitro assays in which the substrate, whether microtiter plate or catheter, is first coated with plasma proteins [34], [52]. We do this both because indwelling medical devices are invariably coated with plasma proteins and because the results we have obtained with our in vitro assays have been consistent with those obtained using in vivo assays [35]. This was not done in the study by Dürig et al. [47]. This is potentially important in that we have also demonstrated that the results obtained when examining the contribution of specific S. aureus factors to biofilm formation differ depending on whether the assay is done with or without plasma coating [34], [52], [53]. To determine whether this may account for this discrepancy, we tested both 220D-F2 and EA in a biofilm assay with and without plasma coating. Our results confirmed that, when the substrate is coated with plasma proteins, EA elicits a significant decrease in the biofilm phenotype that is not apparent in the absence of coating with plasma proteins (Fig. 11). Thus, it is likely that this difference is related to EA interactions with proteins. At the same time, the inhibitory activity of 220D-F2 was apparent under both conditions, which suggests that 220D-F2 contains components unrelated to EA that also have anti-biofilm properties or that alternative derivatives of EA exist in the extract that are not present in the commercially-available EA preparation.
Figure 11. Biofilm inhibition in the presence and absence of human plasma proteins.
Previous studies have indicated that ellagic acid is not an effective biofilm inhibitor for S. aureus [47]. Our data suggest otherwise. UAMS-1 (USA200) and UAMS-1782 (USA300) were used to assess the efficacy of 220D-F2 and EA in experiments that included or omitted the use of plasma coating for the test wells. Treatment with 220D-F2 elicited a dose-dependent response in limiting biofilm formation under both growth conditions, whereas ellagic acid inhibited biofilm formation only in plasma coated wells, suggesting that the mechanistic basis of EA's biofilm-inhibiting effects involves surface protein recognition or attachment.
The focus in this study was on further characterization of the crude R. ulmifolius extract and confirmation of its anti-biofilm properties in diverse strains of S. aureus. Nevertheless, the results discussed above potentially provide important clues about the mechanistic basis for this activity. Most notably, the fact that the inhibitory effects of 220D-F2 were apparent with and without plasma coating suggests that components within the extract are likely to impact multiple biofilm-associated processes. This also appears to be the case with sarA in that the negative impact of mutating sarA on biofilm formation is apparent, albeit to greatly varying degrees, irrespective of whether the assay is done with plasma coating [52], [54]. Mutation of sarA results in decreased production of the polysaccharide intercellular adhesion (PIA), increased production of extracellular nucleases, and increased production of extracellular proteases [52], [53], [54]. The impact of sarA on the production of PIA appears to play a minor role by comparison to these other factors [53], and this suggests that the inhibitory effects we observed with 220D-F2 are not mediated by changes in PIA production. This is consistent with the observation that 220D-F2 did not inhibit biofilm formation in S. epidermidis (data not shown). We have demonstrated that the increased production of both nucleases and proteases contribute to the biofilm-deficient phenotype of sarA mutants [52], [53], [54]. However, the impact of eliminating nuclease production in a sarA mutant is apparent only when the assay is done without plasma coating. To the extent that 220D-F2 inhibited biofilm formation both with and without plasma coating, it is plausible to suggest that the inhibitory effects may impact both protein-dependent and protein-independent mechanisms of biofilm formation in much the same way as sarA itself. We included sarA mutants as controls based on previous work demonstrating that mutation of sarA limits biofilm formation to a therapeutically-relevant degree [34], [35], but based on this we also examined whether the presence of 220D-F2 had any impact on expression of sarA, and somewhat surprisingly our results to date suggest that this is not the case (data not shown). Nevertheless, the results reported in this study provide strong support for the hypothesis that 220D-F2 or its associated components may well have therapeutic utility in the specific context of an S. aureus biofilm-associated infection.
Materials and Methods
Acquisition of botanical materials
Bulk samples of Rubus ulmifolius Schott. (Rosaceae) roots were collected from wild populations in August 2009 in the village of Ginestra, Italy. Procedures from the 2003 WHO Guidelines on Good Agricultural and Collection Practices for Medicinal Plants [55] were followed for the collection and identification of bulk and voucher specimens. Voucher specimens (CQ-164) were deposited at the Herbarium Lucanum (HLUC) at the Università della Basilicata in Potenza, Italy. Additional vouchers are in the possession of the first author. The specimens were identified using the standard Italian Flora [56] and identification was confirmed at HLUC. All soil and other contaminants (i.e. insects, other plant species etc.) were removed from each sample. Roots were cut into small pieces and air dried. Upon drying, materials were packed into plastic bags with silica packets and vacuum sealed, and then exported to the USA under USDA Permit PDEP-09-00228 for phytochemical evaluation and bioassays.
Extraction and bioassay guided fractionation of plant materials
Air-dried roots (1 kg) were ground into a fine powder and extracted with 95% EtOH (2×10 L) at room temperature for 72 hours with constant agitation. Filtered extracts were combined, concentrated at reduced pressure and a temperature <45°C, and lyophilized before being re-suspended in water and partitioned in succession with hexane, ethyl-acetate and butanol (all solvents acquired from Fisher Chemical, Certified ACS). The partitions were dried over anhydrous sodium sulfate, concentrated at reduced pressure, and lyophilized before testing for activity. The most active partition (butanol) was subjected to column chromatography using Silica gel (0.015–0.040 µm particle size, EMD Chemicals) and fractions were collected after eluting successively with mixtures of MeOH∶CH2Cl2 (30∶70, 40∶60, 50∶50, 60∶40, 70∶30, 80∶20, 90∶10) followed by 100% MeOH and 100% H2O (18Ω). Fractions were dried, weighed and tested for anti-biofilm activity using an established microtiter plate assay (see below).
A preparative HPLC method was developed to split 220D-F2 into 4 additional fractions in an effort to identify the active constituent(s). Briefly, 220D-F2 was dissolved in 2-propanol∶water (2∶8) at a concentration of 50 mg/mL. A C-18 column (μBondapak™, 19 mm×300 mm, 125 ′Å, 10 µm) was used to separate 1 mL injections (total 5 mg) with a Waters 600E system controller and pump and an isocratic mobile phase of H2O∶acetonitrile∶2-propanol∶formic acid (74∶17∶8∶1) at a flow rate of 7 mL/min (all solvents HPLC-grade, Fisher Chemical) and detection at a wavelength of 360 nm using a Waters 486 Tunable Absorbance Detector and Shimadzu C-R5A Chromatopac. Fractions were collected at 17.5 (220D-F2-f1), 20.5 (-f2), 27 (-f3) and 45 (-f4) minutes. The largest single peaks were located in fractions 2 and 3, whereas fractions 1 and 4 contained multiple minor peaks. Fractions were collected for chemical analysis and bioassays described below.
Characterization of major extract components
Further characterization of 220D-F2 (suspended in 5% isopropanol in H2O, 1 mg/mL) was performed using accurate mass LC/UV/MS/MS to identify the major components. A Mac-Mod HALO C18 column (3.0×100 mm) was used with a mobile phase (A: 0.1% formic acid in water; B: 0.1% formic acid in acentonitrile) with a gradient (hold 2% B for 2 min., 2–50% B over 18 min, 100% B for 5 min.), flow of 0.4 mL/min and PDA (photodiode array detector) detection range of 200–790 nm. MS detection was with a Thermo LTQ Orbitrap Discovery, +ESI mode, and scan range of 140–2000 Da. Searches of multiple databases (Human Metabolome Database (version 2.5), ChemSpider, SciFinder, and Kyoto Encyclopedia of Genes and Genomes (KEGG) LIGAND Database) were performed using chemical formula queries. All mass measurements were within 0.5 mmu of the proposed formulae, well within the expected measurement tolerances of the mass spectrometer.
Individual phytochemicals tested
In addition to testing the chemically complex R. ulmifolius extracts for anti-biofilm activity, all known constituents of R. ulmifolius (Table 2) that were commercially available were purchased for anti-biofilm analysis using the static microtiter plate method described below. Ferulic acid, kaempferol, ursolic acid, quercetin dehydrate, caffeic acid, ellagic acid, and oleanolic acid were purchased from MP BioMedicals (Solon, OH, USA); quercetin-3-O-glucuronide and tiliroside from Chromadex (Irvine, CA, USA); and gallic acid from Acros Organics (NJ, USA). Compounds were tested for growth and biofilm inhibitory activity at doses ranging from 25–2000 µM.
Quality control
Extracts and drugs were suspended in either DMSO or PBS (depending on solubility), then sterile filtered (0.2 µm), and stored in sterile vials prior to use in all bioassays. Sterility controls were included in all assays (extract+media). Tests for sterility followed standard quality control methods [57] to ensure that no microbial growth was detectable prior to bioassay testing. Prior to performing bioassays, batches of extract 220D-F2 were checked for the relative ratios of constituents by RP-HPLC, and were found to be reproducible. All chemicals (including extract) were stored at −20°C.
Bacterial strains and growth conditions
The Staphylococcus aureus strains used in these experiments are listed in Table 1. When available, isogenic strains carrying a mutation in the staphylococcal accessory regulator (sarA) were included as negative controls based on the observation that mutation of sarA results in a reduced capacity to form a biofilm that can be correlated with increased antibiotic susceptibility [35], [53]. For biofilm assays, strains were grown in tryptic soy broth (TSB) supplemented with 3.0% NaCl (wt/vol) and 0.5% dextrose (biofilm medium, BM). In experiments that included daptomycin, BM was supplemented (wt/vol) with 2.5 mM CaCl2. For all assays, overnight cultures of the test strains were used to inoculate fresh medium at an initial cell density of 5×105 colony-forming units (CFU) per ml (confirmed with plate counts). This cell density was achieved by taking the optical density of overnight cultures and diluting to an OD560 nm of 0.05. Studies examining growth rate were done at 37°C in BM with constant shaking (200 rpm) and a volume-to-flask ratio of 0.4.
Determination of MIC and MBC
To determine the minimum inhibitory concentration (MIC) and minimum bactericidal concentration (MBC) for each fraction, strains were grown at 37°C in cation-adjusted Mueller-Hinton broth (CAMHB). MIC and MBC were determined following Clinical and Laboratory Standards Institute (CSLI) broth microdilution guidelines [58], [59]. Briefly, test strains were inoculated into 0.1 ml CAMHB containing varying concentrations of extract. For MIC, optical density (OD600) was assessed immediately after inoculation and again after 18 hours using a Biotek Synergy II microplate reader. Corrections for extract color were done as previously described [28]. The MIC was defined as the lowest concentration that inhibited growth to a level ≥90% (for MIC90) or ≥50% (for MIC50) by comparison to untreated control cultures. MBC was assessed by determining the number of colony-forming units (CFU) after 24 hours of exposure and was defined as the lowest concentration at which the initial density of viable cells was reduced to a level by ≥90% (for MBC90) or ≥50% (for MBC50) by comparison to the untreated control cultures.
Assessment of biofilm formation
The primary biofilm assays, used as a guide during fractionation, were undertaken using a human plasma protein-coated microtiter plate assay as previously described [53]. Wells were pre-coated for 24 h at 4°C with 20% human plasma diluted in carbonate buffer (pH 9.6). After inoculation and addition of the appropriate media (containing drug or excipient alone), the plates were incubated without shaking at 37°C for 24 h, the wells were gently washed twice with 200 µl of phosphate-buffered saline to remove nonadherent cells. Adherent biofilms were fixed with 200 µl of 100% ethanol prior to staining for 2 min with 200 µl of 0.41% (wt/vol) crystal violet in 12% ethanol (Protocol Crystal Violet; Biochemical Sciences, Swedesboro, N.J.). The stain was then aspirated, and the wells were washed several times with phosphate-buffered saline. A quantitative assessment of biofilm formation was obtained by adding 100 µl of 100% ethanol and incubating at room temperature for 10 min. A total of 50 µl of the eluate was then transferred to a sterile polystyrene microtiter plate and the absorbance (OD595 nm) was determined using a plate reader. The minimum biofilm-inhibiting concentration (MBIC) was defined as the lowest concentration of extract in which biofilm formation was limited to a level ≥90% (for MBIC90) or ≥50% (for MBIC50) by comparison to the untreated parent control strain. Additional tests with 220D-F2 and EA were conducted to examine the influence of plasma proteins on the relative activity of the drugs. In this case, both coated and uncoated wells were employed in the static microtiter plate assay.
Assays examining the impact of different extracts on antibiotic susceptibility were done using an in vitro model of catheter-associated biofilm formation [34]. Briefly, 1-cm segments of fluorinated ethylene propylene catheters (14-gauge Introcan Safety catheter; B. Braun, Bethlehem, PA) were coated with human plasma proteins (Sigma-Aldrich, St. Louis, MO, USA), placed in the wells of a 12-well microtiter plate containing BM, and inoculated with the test strain at an initial optical density (OD560 nm) of 0.05. After 24 hours, the BM was replaced with fresh BM containing 220D-F2 (or excipient alone) with or without antibiotic. Antibiotics tested were daptomycin, clindamycin, and oxacillin, all of which were examined at concentrations corresponding to 1 and 10 times (1× and 10×) the CLSI-defined breakpoint MIC defined for an antibiotic-resistant strain of S. aureus. The medium was replaced in its entirety at 24 hour intervals for 7 days. Following each 24 hour interval, catheters were removed and processed to assess viability as previously described [34], [35]. More specifically, catheters were dunked into sterile PBS several times using a sterile forceps in order to remove all of the loosely adherent cells from both the interior lumen of the catheter and external surface. In a second set of experiments, extracts were added to BM during colonization of plasma-coated catheters. After 24 hours, catheters were either processed for plate counts as described above or transferred to fresh BM with and without antibiotics.
Confocal laser scanning microscopy (CLSM) of static biofilms
Two S. aureus strains (UAMS-1 and the USA300 isolate UAMS-1782) and their isogenic sarA mutants (UAMS-929 and UAMS-1804) were grown in 96 well microtiter plates (Costar 3603, Corning Life Sciences) as described above. After 20 hours, the well contents were aspirated and the wells gently washed three times with 0.85% (wt/vol) NaCl. The adherent biofilm was then stained with LIVE/DEAD stain (Invitrogen) at room temperature in the dark for 18 minutes. After removal of the stain, the wells were gently washed with 0.85% NaCl before collecting CLSM images using a Zeiss LSM 510 Meta confocal scanning system and inverted microscope. SYTO 9 fluorescence was detected by excitation at 488 nm and emission collected with a 500–530 bandpass filter. All z-sections were collected at 4-µm intervals using a 10× objective lens. A 0.9×0.9 mm section of biofilm was selected from the center of the well for each image. Image acquisition and processing was performed using LSM Image Browser (Carl Zeiss). Identical acquisition settings were employed for all samples.
Cell culture and cytotoxicity assays
Normal human kidney proximal tubular (HK-2) cells, normal rat kidney (NRK-52E) cells, and normal mouse hepatocytes (AML12) were purchased from the American Type Culture Collection (ATCC). Normal mouse kidney proximal tubular cells (TKPTS) were developed and gifted by Dr. Elsa Bello-Reuss [60]. The four cell lines were cultured with different media, keratinocyte serum free media (K-SFM) supplemented with bovine pituitary extract (BPE) and human recombinant epidermal growth factor (EGF) for HK-2 cells, Dubelcco's Modified Eagle's Medium (DMEM) for NRK-52E cells, and ATCC complete growth medium (1∶1 mix of DMEM and Ham's F12 medium supplemented with insulin, transferring, dexamethasone, and fetal bovine serum) for AML12 and TKPTS cells. Cells were maintained in humidified air with 5% CO2 at 37°C. Cells were transferred to 96-well cell culture plates (10,000 cells seeded per well) and incubated for 24 hours prior to aspirating the media, adding extract 220D-F2 in serum-free media and undertaking cytotoxicity tests. To examine the cytotoxic effects of 220D-F2 on normal mammalian liver and kidney cells, a lactate dehydrogenase (LDH) assay was employed. LDH is a stable cytosolic enzyme that is released upon membrane damage in necrotic cells. LDH activity can serve as a useful measure for determining drug toxicity to cell lines.
LDH was measured using a commercial cytotoxicity assay kit (Promega CytoTox 96® Non-Radioactive Cytotoxicity Assay, WI, USA), in which LDH released in culture supernatants is measured with a coupled enzymatic assay, resulting in conversion of a tetrazolium salt into a red formazan product. The cells were treated with concentrations of extract 220D-F2 ranging from 0.1–7,000 µg/mL and incubated in humidified air with 5% CO2 at 37°C for 24 hours. Controls for the extract excipient (20% DMSO in phosphate buffered saline, PBS), positive LDH control, and positive LDH control with media and extract were also included. The sample solution (supernatant) was removed, and the LDH released from the cells into culture medium treated according to kit instructions, then measured at an OD490 nm. The maximal release was obtained after treating cells with a lysis solution for 45 minutes, then treating the supernatant according to kit instructions. All tests were performed in quadruplicate. The necrotic percentage (% cytotoxicity) was expressed using the formula: (sample value/maximal release)×100%.
Statistical analysis
Pair-wise testing was performed based on t tests as formatted in Sigma Stat® Statistical Software Version 2 (SPSS, Inc) with P values<0.05 considered significant.
Supporting Information
Inhibitory effects of individual phytochemicals reported in the literature for R. ulmifolius against biofilm formation and growth of UAMS-1.
(DOCX)
Acknowledgments
The authors thankfully acknowledge Dr. Alexei G. Basnakian, Dr. Yevgeniy Apostolov and Ms. Anna Stewart for technical support at the DNA Damage and Toxicology Core Center. We thank Dr. Elsa Bello-Reuss for the gift of the TKPTS cell line used in this study. We thank Dr. Kenneth Ray at Novatia, LLC (Monmouth Junction, NJ, USA) for the LC/UV/MS/MS analysis of 220D-F2. We thank the community of Ginestra, Italy and the D. Caputo and C. Allamprese families for permission to collect plant materials from wild populations growing on their land.
Footnotes
Competing Interests: Cassandra Quave, Howard Hendrickson, Cesar Compadre, Mark Smeltzer and the University of Arkansas for Medical Sciences have a pending USA patent application on anti-biofilm compositions, (#052592-417257, date of filing October 6, 2010). This has no influence on the content of this article and does not alter the authors' adherence to all the PLoS ONE policies on sharing data and materials.
Funding: This work was supported by an F32 Fellowship to CQ (AT005040) from the National Center for Complementary and Alternative Medicine (NCCAM) and by a grant from the Department of the Army USAMRAA to MSS (OR090571). Support was also obtained from resources provided through the Clinical and Translational Sciences Award (RR0298884) to the University of Arkansas for Medical Sciences. The content is solely the responsibility of the authors and does not necessarily reflect the official views of NCCAM, USAMRAA, or NIH. The funding agencies had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Yamamoto T, Nishiyama A, Takano T, Yabe S, Higuchi W, et al. Community-acquired methicillin-resistant Staphylococcus aureus: community transmission, pathogenesis, and drug resistance. Journal of Infection and Chemotherapy. 2010;16:225–254. doi: 10.1007/s10156-010-0045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hildron AI, Low CE, Honig EG, Blumberg HM. Emergence of community-acquired methicillin-resistant Staphylococcus aureus strain USA300 as a cause of necrotising community-onset pneumonia. The Lancet Infectious Diseases. 2009;9:384–392. doi: 10.1016/S1473-3099(09)70133-1. [DOI] [PubMed] [Google Scholar]
- 3.Klevens RM, Morrison M, Nadle J, Petit S, Gershman K, et al. Invasive Methicillin-Resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–1771. doi: 10.1001/jama.298.15.1763. [DOI] [PubMed] [Google Scholar]
- 4.Harro JM, Peters BM, O'May GA, Archer N, Kerns P, et al. Vaccine development in Staphylococcus aureus: taking the biofilm phenotype into consideration. FEMS Immunology and Medical Microbiology. 2010;59:306–323. doi: 10.1111/j.1574-695X.2010.00708.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomas JG, Litton I, Rinde H. Economic impact of biofilms on treatment costs. In: Pace JL, Rupp ME, Finch RG, editors. Biofilms, Infection and Antimicrobial Therapy. Boca Raton, FL: CRC Press. Taylor and Francis; 2006. pp. 21–37. [Google Scholar]
- 6.Zimmerli W, Waldvogel FA, Vaudaux P, Nydegger UE. Pathogenesis of foreign body infection: description and characteristics of an animal model. Journal of Infectious Diseases. 1982;146:487–497. doi: 10.1093/infdis/146.4.487. [DOI] [PubMed] [Google Scholar]
- 7.Toms AD, Davidson D, Masri BA, Duncan CP. The management of peri-prosthetic infection in total joint arthroplasty. The Journal of Bone and Joint Surgery. 2006;88-B:149–155. doi: 10.1302/0301-620X.88B2.17058. [DOI] [PubMed] [Google Scholar]
- 8.Brause BD. Infections with prostheses in bones and joints. In: Mandell GL, Bennett JE, Dolin R, editors. Principles and Practices of Infectious Diseases. Washington, DC: WB Saunders; 2005. pp. 1332–1337. [Google Scholar]
- 9.Wolcott RD, Rhoads DD, Bennett ME, Gogokhia L, Costerton JW, et al. Chronic wounds and the medical biofilm paradigm. Journal of Wound Care. 2010;19:45–53. doi: 10.12968/jowc.2010.19.2.46966. [DOI] [PubMed] [Google Scholar]
- 10.Wolcott RD, Dowd SE. The role of biofilms: are we hitting the right target? Plastic and Reconstructive Surgery. 2010;127:28S–35S. doi: 10.1097/PRS.0b013e3181fca244. [DOI] [PubMed] [Google Scholar]
- 11.Kalan L, Wright GD. Antibiotic adjuvants: multicomponent anti-infective strategies. Expert Reviews in Molecular Medicine. 2011;13:null–null. doi: 10.1017/S1462399410001766. [DOI] [PubMed] [Google Scholar]
- 12.Cox PA, Balick MJ. The ethnobotanical approach to drug discovery. Scientific American. 1994;270:82–87. [PubMed] [Google Scholar]
- 13.Howell A, Botto H, Combescure C, Blanc-Potard A-B, Gausa L, et al. Dosage effect on uropathogenic Escherichia coli anti-adhesion activity in urine following consumption of cranberry powder standardized for proanthocyanidin content: a multicentric randomized double blind study. BMC Infectious Diseases. 2010;10:94. doi: 10.1186/1471-2334-10-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Howell AB. Bioactive compounds in cranberries and their role in prevention of urinary tract infections. Molecular Nutrition & Food Research. 2007;51:732–737. doi: 10.1002/mnfr.200700038. [DOI] [PubMed] [Google Scholar]
- 15.Pérez-López FR, Haya J, Chedraui P. Vaccinium macrocarpon: An interesting option for women with recurrent urinary tract infections and other health benefits. Journal of Obstetrics and Gynaecology Research. 2009;35:630–639. doi: 10.1111/j.1447-0756.2009.01026.x. [DOI] [PubMed] [Google Scholar]
- 16.Low CF, Chong PP, Yong PVC, Lim CSY, Ahmad Z, et al. Inhibition of hyphae formation and SIR2 expression in Candida albicans treated with fresh Allium sativum (garlic) extract. Journal of Applied Microbiology. 2008;105:2169–2177. doi: 10.1111/j.1365-2672.2008.03912.x. [DOI] [PubMed] [Google Scholar]
- 17.Bodini SF, Manfredini S, Epp M, Valentini S, Santori F. Quorum sensing inhibition activity of garlic extract and p-coumaric acid. Letters in Applied Microbiology. 2009;49:551–555. doi: 10.1111/j.1472-765X.2009.02704.x. [DOI] [PubMed] [Google Scholar]
- 18.Harjai K, Kumar R, Singh S. Garlic blocks quorum sensing and attenuates the virulence of Pseudomonas aeruginosa. FEMS Immunology & Medical Microbiology. 2010;58:161–168. doi: 10.1111/j.1574-695X.2009.00614.x. [DOI] [PubMed] [Google Scholar]
- 19.Fulghesu L, Giallorenzo C, Savoia D. Evaluation of Different Compounds as Quorum Sensing Inhibitors in Pseudomonas aeruginosa. Journal of Chemotherapy. 2007;19:388–391. doi: 10.1179/joc.2007.19.4.388. [DOI] [PubMed] [Google Scholar]
- 20.Smith ECJ, Kaatz GW, Seo SM, Wareham N, Williamson EM, et al. The phenolic diterpene Totarol Inhibits multidrug efflux pump activity in Staphylococcus aureus. Antimicrob Agents Chemother. 2007;51:4480–4483. doi: 10.1128/AAC.00216-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chérigo L, Pereda-Miranda R, Fragoso-Serrano M, Jacobo-Herrera N, Kaatz GW, et al. Inhibitors of bacterial multidrug efflux pumps from the resin glycosides of Ipomoea murucoides. Journal of Natural Products. 2008;71:1037–1045. doi: 10.1021/np800148w. [DOI] [PubMed] [Google Scholar]
- 22.Wang W, Zeng YH, Osman K, Shinde K, Rahman M, et al. Norlignans, acylphloroglucinols, and a dimeric xanthone from Hypericum chinense. Journal of Natural Products. 2010;73:1815–1820. doi: 10.1021/np1004483. [DOI] [PubMed] [Google Scholar]
- 23.Gibbons S. Anti-staphylococcal plant natural products. Natural Product Reports. 2004;21:263–277. doi: 10.1039/b212695h. [DOI] [PubMed] [Google Scholar]
- 24.Gibbons S. Phytochemicals for bacterial resistance–strengths, weaknesses and opportunities. Planta Medica. 2008;74:594–602. doi: 10.1055/s-2008-1074518. [DOI] [PubMed] [Google Scholar]
- 25.Gibbons S, Ohlendorf B, Johnsen I. The genus Hypericum–a valuable resource of anti-Staphylococcal leads. Fitoterapia. 2002;73:300–304. doi: 10.1016/s0367-326x(02)00082-5. [DOI] [PubMed] [Google Scholar]
- 26.Giusti EM, Pieroni A, Quave CL. Medical anthropology at the borders: ritual healing in Arbëreshë Albanian ethnic communities in Lucania (southern Italy). In: Paládi-Kovács A, Csukás G, Kiss R, Kristóf I, Nagy I, editors. Times, Places, Passages Ethnological Approaches in the New Millennium 7th SIEF Selected Papers. Budapest, Hungary: Akadémiai Kiadó; 2004. pp. 237–245. [Google Scholar]
- 27.Quave CL, Plano LWR, Bennett BC. Quorum sensing inhibitors for MRSA from Italian medicinal plants. Planta Medica. 2010;76:1–8. doi: 10.1055/s-0030-1250145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Quave CL, Plano LWR, Pantuso T, Bennett BC. Effects of extracts from Italian medicinal plants on planktonic growth, biofilm formation and adherence of methicillin-resistant Staphylococcus aureus. Journal of Ethnopharmacology. 2008;118:418–428. doi: 10.1016/j.jep.2008.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin M-H, Chang F-R, Hua M-Y, Wu Y-C, Liu S-T. Inhibitory effects of 1,2,3,4,6-Penta-O-Galloyl-β-D-Glucopyranose on biofilm formation by Staphylococcus aureus. Antimicrobial Agents and Chemotherapy. 2011;55:1021–1027. doi: 10.1128/AAC.00843-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alviano DS, Alviano CS. Plant Extracts: Search for New Alternatives to Treat Microbial Diseases Current Pharmaceutical Biotechnology. 2009;10:106–121. doi: 10.2174/138920109787048607. [DOI] [PubMed] [Google Scholar]
- 31.Flamini G, Catalano S, Caponi C, Panizzi L, Morelli I. Three anthrones from Rubus ulmifolius. Phytochemistry. 2002;59:873–876. doi: 10.1016/s0031-9422(02)00012-2. [DOI] [PubMed] [Google Scholar]
- 32.Panizzi L, Caponi C, Catalano S, Cioni PL, Morelli I. In vitro antimicrobial activity of extracts and isolated constituents of Rubus ulmifolius. Journal of Ethnopharmacology. 2002;79:165–168. doi: 10.1016/s0378-8741(01)00363-4. [DOI] [PubMed] [Google Scholar]
- 33.Quave CL, Pieroni A, Bennett BC. Dermatological remedies in the traditional pharmacopoeia of Vulture-Alto Bradano, inland southern Italy. Journal of Ethnobiology and Ethnomedicine. 2008;4:5. doi: 10.1186/1746-4269-4-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weiss EC, Spencer HJ, Daily SJ, Weiss BD, Smeltzer MS. Impact of sarA on antibiotic susceptibility of Staphylococcus aureus in a catheter-associated in vitro model of biofilm formation. Antimicrobial Agents and Chemotherapy. 2009;53:2475–2482. doi: 10.1128/AAC.01432-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Weiss EC, Zielinska A, Beenken KE, Spencer HJ, Daily SJ, et al. Impact of sarA on daptomycin susceptibility of Staphylococcus aureus biofilms in vivo. Antimicrobial Agents and Chemotherapy. 2009;53:4096–4102. doi: 10.1128/AAC.00484-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dall'Acqua S, Cervellati R, Loi MC, Innocenti G. Evaluation of in vitro antioxidant properties of some traditional Sardinian medicinal plants: Investigation of the high antioxidant capacity of Rubus ulmifolius. Food Chemistry. 2008;106:745–749. [Google Scholar]
- 37.Landete JM. Ellagitannins, ellagic acid and their derived metabolites: A review about source, metabolism, functions and health. Food Research International. 2011;44:1150–1160. [Google Scholar]
- 38.Zafrilla P, Ferreres F, Tomas-Barberan FA. Effect of processing and storage on the antioxidant ellagic acid derivatives and flavonoids of red raspberry (Rubus idaeus) jams. Journal of Agricultural and Food Chemistry. 2001;49:3651–3655. doi: 10.1021/jf010192x. [DOI] [PubMed] [Google Scholar]
- 39.Lee J-H, Talcott ST. Fruit maturity and juice extraction influences ellagic acid derivatives and other antioxidant polyphenolics in muscadine grapes. Journal of Agricultural and Food Chemistry. 2003;52:361–366. doi: 10.1021/jf034971k. [DOI] [PubMed] [Google Scholar]
- 40.Losso JN, Bansode RR, Trappey A, Bawadi HA, Truax R. In vitro anti-proliferative activities of ellagic acid. The Journal of Nutritional Biochemistry. 2004;15:672–678. doi: 10.1016/j.jnutbio.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 41.Papoutsi Z, Kassi E, Tsiapara A, Fokialakis N, Chrousos GP, et al. Evaluation of estrogenic/antiestrogenic activity of ellagic acid via the estrogen receptor subtypes ERα and ERβ. Journal of Agricultural and Food Chemistry. 2005;53:7715–7720. doi: 10.1021/jf0510539. [DOI] [PubMed] [Google Scholar]
- 42.Umesalma S, Sudhandiran G. Differential inhibitory effects of the polyphenol ellagic acid on inflammatory mediators NF-κB, iNOS, COX-2, TNF-α, and IL-6 in 1,2-dimethylhydrazine-induced rat colon carcinogenesis. Basic & Clinical Pharmacology & Toxicology. 2010;107:650–655. doi: 10.1111/j.1742-7843.2010.00565.x. [DOI] [PubMed] [Google Scholar]
- 43.Weidner-Wells MA, Altom J, Fernandez J, Fraga-Spano SA, Hilliard J, et al. DNA gyrase inhibitory activity of ellagic acid derivatives. Bioorganic & Medicinal Chemistry Letters. 1998;8:97–100. doi: 10.1016/s0960-894x(97)10197-4. [DOI] [PubMed] [Google Scholar]
- 44.Cozza G, Bonvini P, Zorzi E, Poletto G, Pagano MA, et al. Identification of ellagic acid as potent inhibitor of protein kinase CK2: a successful example of a virtual screening application. Journal of Medicinal Chemistry. 2006;49:2363–2366. doi: 10.1021/jm060112m. [DOI] [PubMed] [Google Scholar]
- 45.Hancock V, Dahl M, Vejborg RM, Klemm P. Dietary plant components ellagic acid and tannic acid inhibit Escherichia coli biofilm formation. Journal of Medical Microbiology. 2010;59:496–498. doi: 10.1099/jmm.0.013680-0. [DOI] [PubMed] [Google Scholar]
- 46.Huber B, Eberl L, Feucht W, Polster J. Influence of polyphenols on bacterial biofilm formation and quorum-sensing. Zeitschrift für Naturforschung. 2003;58c:879–884. doi: 10.1515/znc-2003-11-1224. [DOI] [PubMed] [Google Scholar]
- 47.Dürig A, Kouskoumvekaki I, Vejborg R, Klemm P. Chemoinformatics-assisted development of new anti-biofilm compounds. Applied Microbiology and Biotechnology. 2010;87:309–317. doi: 10.1007/s00253-010-2471-0. [DOI] [PubMed] [Google Scholar]
- 48.Simões-Pires CA, Vargas S, Marston A, Ioset JR, Paulo MQ, et al. Ellagic acid derivatives from Syzygium cumini stem bark: investigation of their antiplasmodial activity. Natural Product Communications. 2009;4:1371–1376. [PubMed] [Google Scholar]
- 49.Elkhateeb A, Subeki TK, Matsuura H, Yamasaki M, Yamato O, et al. Anti-babesial ellagic acid rhamnosides from the bark of Elaeocarpus parvifolius. Phytochemistry. 2005;66:2577–2580. doi: 10.1016/j.phytochem.2005.08.020. [DOI] [PubMed] [Google Scholar]
- 50.Atta-Ur-Rahman NFN, Choudhary MI, Malik S, Makhmoor T, Nur-E-Alam M, et al. New antioxidant and antimicrobial ellagic acid derivatives from Pteleopsis hylodendron. Planta Medica. 2001;67:335–339. doi: 10.1055/s-2001-14306. [DOI] [PubMed] [Google Scholar]
- 51.Matthew S, Kao KC, Chang YS, Abreu P. Ellagic acid glycosides from Turpinia ternata. Natural Product Research. 2007;21:83–88. doi: 10.1080/14786410500441516. [DOI] [PubMed] [Google Scholar]
- 52.Beenken KE, Mrak LN, Griffin LM, Zielinska A, Shaw LN, et al. Epistatic relationships between sarA and agr in Staphylococcus aureus biofilm formation. PLoS ONE. 2010;5 doi: 10.1371/journal.pone.0010790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Beenken KE, Blevins JS, Smeltzer MS. Mutation of sarA in Staphylococcus aureus limits biofilm formation. Infection and Immunity. 2003;71:4206–4211. doi: 10.1128/IAI.71.7.4206-4211.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tsang LH, Cassat JE, Shaw LN, Beenken KE, Smeltzer MS. Factors contributing to the biofilm-deficient phenotype of Staphylococcus aureus sarA mutants. PLoS One. 2008;3:e3361. doi: 10.1371/journal.pone.0003361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.WHO. WHO guidelines on good agricultural and collection practices (GACP) for medicinal plants. Geneva 2003 [Google Scholar]
- 56.Pignatti S. Flora d'Italia. Bologna, Italy: Edizioni Edagricole; 2002. [Google Scholar]
- 57.Isenberg HD. Clinical Microbiology Procedures Handbook; In: Isenberg HD, editor. Washington, D.C.: ASM Press; 2004. [Google Scholar]
- 58.NCCLSNCCLS, editor. Wayne, PA: National Committee for Clinical Laboratory Standards; 1999. Methods for Determining Bactericidal Activity of Antimicrobial Agents; Approved Guideline; [Google Scholar]
- 59.NCCLS. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria that Grow Aerobically; Approved Standard. Wayne, PA: National Center for Clinical Laboratory Standards; 2001. [Google Scholar]
- 60.Ernest S, Bello-Reuss E. Expression and function of P-glycoprotein in a mouse kidney cell line. American Journal of Physiology - Cell Physiology. 1995;269:C323–C333. doi: 10.1152/ajpcell.1995.269.2.C323. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Inhibitory effects of individual phytochemicals reported in the literature for R. ulmifolius against biofilm formation and growth of UAMS-1.
(DOCX)