Abstract
Purpose
To investigate the association between SEPTIN12 gene variants and the risk of azoospermia caused by meiotic arrest.
Methods
Mutational analysis of the SEPTIN12 gene was performed using DNA from 30 Japanese patients with azoospermia by meiotic arrest and 140 fertile male controls.
Results
The frequencies of the c.204G>C (Gln38His) allele and the CC genotype were significantly higher in patients than in fertile controls (p < 0.05).
Conclusion
The c.204G>C (Gln38His) variant in the SEPTIN12 gene was associated with increased susceptibility to azoospermia caused by meiotic arrest.
Keywords: Male infertility, Meiosis, Septin, SNP
Introduction
Genetic causes of azoospermia in humans include chromosomal abnormalities, e.g., Y-chromosome microdeletions and mutations in specific genes; e.g., DAZ, SYCP3, PRM1, SPATA16, AURKC and KLHL10 [1–7]. As Y-chromosome deletions account for only 16% of men with infertility [8], azoospermia in many infertile men may be caused by mutations in autosomal genes. Genetic polymorphisms may also increase susceptibility to some forms of male infertility; e.g., mutations in the human BCL2 and eNOS genes are linked to male infertility [9, 10]. Defective meiosis during spermatogenesis causes azoospermia; however, the mechanisms leading to defective meiosis remain unknown. Meiosis is a fundamental process in sexually reproducing species that allows genetic exchange between maternal and paternal genomes [11]. Our understanding of the genetic regulation of meiosis in mammals is poor relative to that in lower eukaryotes, such as yeast.
Several critical genes expressed in mouse meiosis, such as Dmc1, Fkbp6, Scp3 (Sycp3), Spo11, Msh4 and Msh5, Meisetz, Cdk2, and Hop2, have been identified by disruption experiments in embryonic stem cells [12–22]. In 2006, Lin et al. identified 10 genes involved in human spermatogenesis by subtractive hybridization microarray analysis of mRNA expression in testicular tissue [23]. Their analysis of normal and Sertoli cell-only syndrome (SCOS) testicular tissues identified the human SEPTIN12 gene (NM_144605.3). This gene encodes SEPT12 (NP_653206.2), which belongs to the septin family of polymerizing GTP-binding proteins that are required for many cellular functions; e.g., membrane compartmentalization, vesicular trafficking, mitosis, and cytoskeletal remodeling [24]. SEPT12 can interact with SEPT6, independently of the coiled-coil domain of SEPT6 [25]. The testicular tissues of men with either hypospermatogenesis or maturation arrest have lower levels of the SEPTIN12 transcripts than those of fertile men [26]. Moreover, most chimeric mice derived from Septin12 knockout embryonic stem cells generated using gene targeting were infertile and had a decreased sperm count, decreased sperm motility, and spermatozoa with defects involving all subcellular compartments [26]. Oocytes fertilized with spermatozoa obtained from Septin12+/− chimeric mice failed to develop beyond the morula stage after in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) because of significant DNA defects in the spermatozoa [27]. Previously, we investigated whether SEPTIN12 gene variants are associated with azoospermia caused by SCOS [28]. The coding regions of SEPTIN12 from 100 infertile Japanese male patients and 140 fertile control males were directly sequenced, and the data were subjected to statistical analysis. No mutations were found in SEPTIN12; however, eight coding single nucleotide polymorphisms (SNP1-SNP8) could be detected in the patients with SCOS. The frequencies of particular SNP3, SNP4, and SNP6 variants and the frequencies of some genotypes were notably higher in the SCOS group than in the control group (P < 0.001). These results suggest that SEPTIN12 might play a critical role in human spermatogenesis [28].
In the present study, we analyzed possible associations between SEPTIN12 mutations and azoospermia caused by meiotic arrest (MA) in humans.
Materials and methods
Patients and controls
Azoospermia was confirmed in patients by two consecutive semen analyses obtained after 5–7 days of sexual abstinence and by examination of a centrifuged semen pellet. Patients with defective spermatogenesis following infection or due to obstruction of the seminal tract, to pituitary failure, or to other causes of possible testicular damage revealed upon clinical examination were excluded from the study. Final diagnosis was carried out by histological examination; more than 20 testicular specimens from each of the 30 patients included in the study were examined by a pathologist and urologists at Osaka University. Briefly, it was determined based on the most advanced pattern of spermatogenesis. MA is defined as spermatocyte stage arrest without spermatozoa throughout the seminiferous tubules in the specimen, so-called “uniform MA” [29]. We carefully distinguished MA from hypospermatogenesis, which is characterized with reduction in the degree of normal spermatogenesis and focal spermatogenesis with spermatid stage arrest [30]. Each of the 30 patients had a normal 46, XY karyotype based on analysis of chromosomes in peripheral lymphocytes. No patients had Y chromosome microdeletions. Ultimately, 30 Japanese patients with azoospermia secondary to MA were included in the study; 140 healthy, pregnancy-proven, fertile men were also examined as controls [28]. All normal controls were Japanese men and had normal sperm inspections, in addition to all having a child by spontaneous pregnancy. All subjects were Japanese and provided written informed consent for molecular blood analysis. This study was approved by the local ethics committee.
Mutation screening
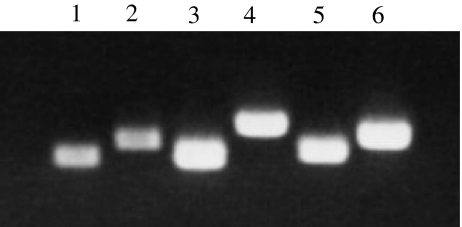
We screened 30 Japanese patients diagnosed with azoospermia secondary to MA for mutations in the SEPTIN12 gene. Full-length cDNA sequences were compared to human genomic sequences (NT_037887.4) from the NCBI reference database by BLAST, and all exon-intron borders were determined. The following SEPTIN12 primers were used for mutational analysis. Exon 2: E2F1, E2F2, E2R1 and E2R2; Exons 3, 4: E3F1, E3F2, E3R1 and E3R2; Exon 5: E5F1, E5F2, E5R1 and E5R2; Exons 6, 7: E6F1, E6F2, E6R1 and E6R2; Exon 8: E8F1, E8F2, E8R1 and E8R2; and Exon 9: E9F1, E9F2, E9R1 and E9R2 [28]. Nested PCR was performed using primers for each intronic region and 10-fold diluted first PCR products as templates. The initial PCR was performed in a final volume of 25 μl, consisting of genomic DNA (10 ng), dNTP (0.32 mM each), each primer (0.2 μM), 0.2 μM Taq polymerase (0.625 IU) and reaction buffer containing MgCl2. First PCR was performed as follows: initial denaturation at 95°C for 150 s, followed by 32 cycles of denaturation at 95°C for 30 s, annealing at (primers Tm −5°C) for 90 s, and extension at 72°C for 90 s. Nested PCR was carried out for 20 cycles under the same conditions as above, except that 2 μl of 10-fold diluted first PCR products were used as templates. Nested PCR products were purified using a QIAquick PCR Purification kit (Qiagen; Tokyo, Japan), and direct sequencing of each product was conducted (Fig. 1). To confirm the role of the detected polymorphisms in azoospermia, the coding region of the SEPTIN12 gene of 140 healthy, fertile control men was also analyzed by direct sequencing analysis previously [28].
Fig. 1.
Six PCR products include the exons and adjacent introns. Lane1: the region including exon2 (E2), 336 bp; Lane2: E3&E4, 473 bp; Lane3: E5, 342 bp; Lane4: E6&E7, 637 bp; Lane5: E8, 395 bp; Lane6: E9, 533 bp
Genotyping and statistical analyses
Single-locus analysis
To investigate the role of SEPTIN12 polymorphisms in azoospermia, Fisher’s exact test was used to determine a meaningful difference in allele and genotype frequencies between the patient and control groups. A P < 0.05 was considered to be statistically critical. Hardy-Weinberg equilibrium (HWE) was tested using SNPAlyze software (Dynacom; Chiba, Japan). Linkage disequilibrium (LD) of all possible two-way combinations of single nucleotide polymorphisms (SNPs) with the absolute value of the correlation coefficient (D’) was tested; P values were determined by a χ2 approximation, and again a P < 0.05 was consider significant. Haplotype frequencies were estimated by the method of maximum likelihood based on the expectation-maximization (E-M) algorithm under the assumption of HWE. LD and haplotype frequency were tested using SNPAlyze software. P values were determined by χ2 approximation, and a P = 0.05 level was considered significant.
Results
Sequence analysis of the SEPTIN12 gene revealed three nucleotide changes in the 30 patients: 204G>C (Gln38His) in exon 2, 422C>A (Thr111Lys) in exon 4, and 564G>A in exon 5. All three SNPs were identified in the previous study (Table 1) [28]. SNP1 and SNP2 were non-synonymous, and SNP3 was synonymous. Genotyping for the SEPTIN12 SNP alleles among the 30 patients and 140 controls revealed significantly different genotype distributions and allele frequencies of SNP1 between the two groups (Table 1). However, there were no meaningful differences on SNP2 and SNP3 between the two groups (p > 0.05) (Table 1).
Table 1.
Genotype and allele frequencies of three coding single-nucleotide polymorphisms (cSNPs) in the human SEPTIN12 gene of 30 azoospermic patients with MA and 140 fertile male controls
| SNP | Alteration | Genotype frequency | Allele frequency | |||
|---|---|---|---|---|---|---|
| Nucleotide | Amino acid | Genotype/Total no. of samples (%) | Minor allele/Total no. of chromosomes (%) | |||
| (G) MA | Controls p value | (A) MA | Controls p value | |||
| SNP1 | 204G>C | Gln38His | CC 2/30 (6.67) | 0/140 (0.00) | C 9/60 (15.0) | 0/280 (0.00) |
| 0.030* | <0.001* | |||||
| SNP2 | 422C>A | Thr111[Thr, Lys] | AC 1/30 (3.33) | 1/140 (0.714) | A 1/60 (1.67) | 1/280 (0.357) |
| 0.323 | 0.322 | |||||
| SNP3 | 564G>A | Synonymous | AA 1/30 (3.33) | 15/140 (10.7) | A 12/60 (20.0) | 92/280 (32.9) |
| 0.310 | 0.063 | |||||
(G) and (A) indicate genotype and allele, respectively.
At the c.204G>C (Gln38His) site, the proportion of CC homozygote/GG homozygote was 0.067/0.933 in the patient group and 0.00/1.00 in the control group (P < 0.05). The allele frequency of c.204G>C (Gln38His) was 0.15/0.85 in the patient group and 0.00/1.00 in the control group; again, the difference was significant (P < 0.001). Haplotype analysis revealed no significant difference in the haplotype frequency estimates for the three polymorphisms in the patient and control groups (P > 0.05). Haplotype estimation and LD analysis also revealed no significant differences between the patient and control groups (P > 0.05) (Tables 2 and 3).
Table 2.
Pairwise linkage disequilibrium (D’-value above right triangle) and statistical significance (P-value below left triangle) for the three SNPs. Significant at P = 0.05 level by χ2 tests
| SNP1 | SNP2 | SNP3 | |
|---|---|---|---|
| Case group | |||
| SNP1 | 1 | 1 | |
| SNP2 | 0.5808 | −0.1158 | |
| SNP3 | 0.5808 | 0.2595 | |
| Control group | |||
| SNP1 | 0.1002 | 1 | |
| SNP2 | 0.1049 | 1 | |
| SNP3 | 0.1049 | 0.1406 | |
Table 3.
Haplotype frequency estimation in the patient group and control group
| SNP1-SNP2-SNP3 | Case | Control | P-value |
|---|---|---|---|
| G - C - G | 0.6944 | 0.7857 | 0.2719 |
| G - C - A | 0.2500 | 0.1735 | 0.3209 |
Discussion
In this study, we hypothesized that mutations or polymorphisms of the SEPTIN12 may be associated with azoospermia caused by MA. We could not state that we could find SEPTIN12 mutations that directly cause azoospermia by these results. The number of analyzed patients is not enough to achieve a final decision. However, we identified three cSNPs in the gene at least. The present association study revealed that the genotype distribution for SNP1, 204G>C (Gln38His), is significantly different between Japanese azoospermic patients and fertile controls (P < 0.05). This finding indicated that the G allele at SNP 204 in exon 2 and the resulting Gln amino acid, or their flanking regions, may play a role in the disruption of spermatogenesis in Japanese patients. However, the number of patients analyzed was not large enough to allow a definitive conclusion to be drawn. Moreover, the function of the SNP at position 204 is unknown. Nevertheless, azoospermia by MA is very rare, and our histological diagnostic criteria were very strict—i.e., we have DNA samples from more than 5,000 patients with azoospermia, and only 30 of these patients had azoospermia secondary to MA.
In conclusion, we suggest that the C variant of the SNP at position 204 might be associated with azoospermia secondary to MA in humans, but the relationship between the C allele and the mechanistic cause of azoospermia was not investigated. Our results may provide insight into the molecular basis of meiotic arrest as a cause of non-obstructive azoospermia. It remains to be determined whether an association between this variant and azoospermia secondary to MA exists in similar patients from other ethnic groups.
Acknowledgments
This study was supported by Grants-in-Aid for Scientific Research (22591811, 22591812, and 23592388) from the Ministry of Education, Culture, Sports, Science and Technology of Japan, and the Ministry of Health, Labour and Welfare of Japan.
Footnotes
Grants
Grants-in-Aid for Scientific Research (22591811, 22591812, and 23592388) from the Ministry of Education, Culture, Sports, Science and Technology of Japan, the Ministry of Health, Labour and Welfare of Japan.
Capsule c.204G>C (Gln38His) variant in the SEPTIN12 gene was associated with increased susceptibility to azoospermia by meiotic arrest in Japanese men.
References
- 1.Reijo R, Lee TY, Salo P, Alagappan R, Brown LG, Rosenberg M, et al. Diverse spermatogenic defects in humans caused by Y chromosome deletions encompassing a novel RNA-binding protein gene. Nat Genet. 1995;10:383–393. doi: 10.1038/ng0895-383. [DOI] [PubMed] [Google Scholar]
- 2.Matzuk MM, Lamb DJ. Genetic dissection of mammalian fertility pathway. Nat Med. 2002;8(suppl 1):S41–S49. doi: 10.1038/ncb-nm-fertilityS41. [DOI] [PubMed] [Google Scholar]
- 3.Miyamoto T, Hasuike S, Yogev L, Maduro MR, Ishikawa M, Westphal H, Lamb DJ. Azoospermia in patients heterozygous for a mutation in SYCP3. Lancet. 2003;362:1714–1719. doi: 10.1016/S0140-6736(03)14845-3. [DOI] [PubMed] [Google Scholar]
- 4.Oliva R. Protamines and male infertility. Hum Reprod Update. 2006;12:417–435. doi: 10.1093/humupd/dml009. [DOI] [PubMed] [Google Scholar]
- 5.Dam AHDM, Koscinski I, Kremer JAM, Moutou C, Jaeger AS, Oudakker AR, Tournaye H, et al. Homozygous mutation in SPATA16 is associated with male infertility in human globozoospermia. Am J Hum Genet. 2007;81:813–820. doi: 10.1086/521314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dieterich K, Rifo RS, Faure AK, Hennebicq S, Amar BB, Zahi M, et al. Homozygous mutation of AURKC yields large-headed polyploidy spermatozoa and causes male infertility. Nat Genet. 2007;39:661–665. doi: 10.1038/ng2027. [DOI] [PubMed] [Google Scholar]
- 7.Yatsenko AN, Roy A, Chen R, Ma L, Murthy LJ, Yan W, et al. Non-invasive genetic diagnosis of male infertility using spermatozoa RNA: KLHL10 mutations in oligozoospermic patients impair homodimerization. Hum Mol Genet. 2006;15:3411–3419. doi: 10.1093/hmg/ddl417. [DOI] [PubMed] [Google Scholar]
- 8.Yao G, Chen G, Pan T. Study of microdeletions in the Y chromosome of infertile men with idiopathic oligo- or azoospermia. J Assist Reprod Genet. 2001;18:612–616. doi: 10.1023/A:1013117123244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ma J, Lu HY, Xia YK, Dong HB, Gu AH, Li ZY, et al. BCL2 Ala43Thr is a functional variant associated with protection against azoospermia in a Han-Chinese population. Biol Reprod. 2010;83:656–662. doi: 10.1095/biolreprod.109.082339. [DOI] [PubMed] [Google Scholar]
- 10.Safarinejad MR, Shafiei N, Safarinejad S. The role of endothelial nitric oxide synthase (eNOS) T-786C, G894T, and 4a/b gene polymorphisms in the risk of idiopathic male infertility. Mol Reprod Dev. 2010;77:720–727. doi: 10.1002/mrd.21210. [DOI] [PubMed] [Google Scholar]
- 11.Nasmyth K. Segregating sister genomes: the molecular biology of chromosome separation. Science. 2002;297:559–565. doi: 10.1126/science.1074757. [DOI] [PubMed] [Google Scholar]
- 12.Yoshida K, Kondoh G, Matsuda Y, Habu T, Nishimune Y, Morita T. The mouse RecA-like gene Dmc1 is required for homologous chromosome synapsis during meiosis. Mol Cell. 1998;1:707–718. doi: 10.1016/S1097-2765(00)80070-2. [DOI] [PubMed] [Google Scholar]
- 13.Pittman DL, Cobb J, Schimenti KJ, Wilson LA, Cooper DM, Brignull E, et al. Meiotic prophase arrest with failure of chromosome synapsis in mice deficient for Dmc1, a germline-specific RecA homolog. Mol Cell. 1998;1:697–705. doi: 10.1016/S1097-2765(00)80069-6. [DOI] [PubMed] [Google Scholar]
- 14.Edelmann W, Cohen PE, Kneitz B, Winand N, Lia M, Heyer J, et al. Mammalian MutS homologue 5 is required for chromosome pairing in meiosis. Nat Genet. 1999;21:123–127. doi: 10.1038/5075. [DOI] [PubMed] [Google Scholar]
- 15.Baudat F, Manova K, Yuen JP, Jasin M, Keeney S. Chromosome synapsis defects and sexually dimorphic meiotic progression in mice lacking Spo11. Mol Cell. 2000;6:989–998. doi: 10.1016/S1097-2765(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 16.Kneitz B, Cohen PE, Avdievich E, Zhu L, Kane MF, Hou H, Jr, et al. MutS homolog 4 localization to meiotic chromosomes is required for chromosome pairing during meiosis in male and female mice. Genes Dev. 2000;14:1085–1097. [PMC free article] [PubMed] [Google Scholar]
- 17.Romanienko PJ, Camerini-Otero RD. The mouse Spo11 gene is required for meiotic chromosome synapsis. Mol Cell. 2000;6:975–987. doi: 10.1016/S1097-2765(00)00097-6. [DOI] [PubMed] [Google Scholar]
- 18.Yuan L, Liu JG, Zhao J, Brundell E, Daneholt B, Hoog C. The murine SCP3 gene is required for synaptonemal complex assembly, chromosome synapsis, and male fertility. Mol Cell. 2000;5:73–83. doi: 10.1016/S1097-2765(00)80404-9. [DOI] [PubMed] [Google Scholar]
- 19.Crackower MA, Kolas NK, Noguchi J, Sarao R, Kikuchi K, Kaneko H, et al. Essential role of Fkbp6 in male fertility and homologous chromosome pairing in meiosis. Science. 2003;300:1291–1295. doi: 10.1126/science.1083022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hayashi K, Yoshida K, Matsui Y. A histone H3 methyltransferase controls epigenetic events required for meiotic prophase. Nature. 2005;438:374–378. doi: 10.1038/nature04112. [DOI] [PubMed] [Google Scholar]
- 21.Ortega S, Prieto I, Odajima J, Martin A, Dubus P, Sotillo R, et al. Cyclin-dependent kinase 2 is essential for meiosis but not for mitotic cell division in mice. Nat Genet. 2003;35:25–31. doi: 10.1038/ng1232. [DOI] [PubMed] [Google Scholar]
- 22.Petukhova GV, Romanienko PJ, Camerini-Otero RD. The Hop2 protein has a direct role in promoting interhomolog interactions during mouse meiosis. Dev Cell. 2003;5:927–936. doi: 10.1016/S1534-5807(03)00369-1. [DOI] [PubMed] [Google Scholar]
- 23.Lin YH, Lin YM, Teng YN, Hsieh TY, Lin YS, Kuo PL. Identification of ten novel genes involved in human spermatogenesis by microarray analysis testicular tissue. Fertil Steril. 2006;86:1650–1658. doi: 10.1016/j.fertnstert.2006.04.039. [DOI] [PubMed] [Google Scholar]
- 24.Hall PA, Russell SEH. The pathobiology of the septin gene family. J Pathol. 2004;204:489–505. doi: 10.1002/path.1654. [DOI] [PubMed] [Google Scholar]
- 25.Ding X, Yu W, Liu M, Shen S, Chen F, Wan B, Yu L. SEPT12 interacts with SEPT6 and this interaction alters the filament structure of SEPT6 in Hela cells. J Biochem Mol Biol. 2007;40:973–978. doi: 10.5483/BMBRep.2007.40.6.973. [DOI] [PubMed] [Google Scholar]
- 26.Lin YH, Lin YM, Wang YY, Yu IS, Lin YW, Wang YH, et al. The expression level of Septin12 is critical for spermatogenesis. Am J Pathol. 2009;174:1857–1868. doi: 10.2353/ajpath.2009.080955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lin YH, Chou CK, Hung YC, Yu IS, Pan HA, Lin SW, et al. SEPT12 deficiency causes sperm nucleus damage and developmental arrest of preimplantation embryos. Fertil Steril. 2011;95:363–365. doi: 10.1016/j.fertnstert.2010.07.1064. [DOI] [PubMed] [Google Scholar]
- 28.Miyakawa H, Miyamoto T, Koh E, Tsujimura A, Miyagawa Y, Saijo Y et al (2011) Single-nucleotide polymorphisms in the SEPTIN12 gene may be a genetic risk factor for Japanese patients with Sertoli cell-only syndrome. J Androl. doi:10.2164/jandrol.110.012146 [DOI] [PubMed]
- 29.Hung AJ, King P, Schlegel PN. Uniform testicular maturation arrest: a unique subset of men with nonobstructive azoospermia. J Urol. 2007;178:608–612. doi: 10.1016/j.juro.2007.03.125. [DOI] [PubMed] [Google Scholar]
- 30.Tsujimura A, Matsumiya K, Miyagawa Y, Tohda A, Miura H, Nishimura K, et al. Conventional multiple or microdissection testicular sperm extraction: a comparative study. Hum Reprod. 2002;17:2924–2929. doi: 10.1093/humrep/17.11.2924. [DOI] [PubMed] [Google Scholar]