Abstract
Background
Although lumbar spinal fusion has been performed for more than 70 years, few studies have examined rehabilitation strategies for spinal fusion patients, and there is only sparse information about the patient’s activity level after surgery. The Canadian Occupational Performance Measure (COPM) is a standardized semi-structured interview, developed to identify patients’ problems in relation to activities of daily living (ADL). The COPM has neither been examined in a randomised clinical study nor employed in relation to lumbar spinal fusion patients. We aimed to examine whether or not the use of the semi-structured interview COPM during in-hospital rehabilitation could: (1) identify more ADL-related problems of importance to the patients after discharge from the hospital, (2) enhance the patients’ ADL performance after discharge from hospital
Method
Eighty-seven patients undergoing a lumbar spinal fusion caused by degenerative diseases were randomly assigned to either use of the COPM or to standard treatment.
Results and conclusion
Use of the COPM during hospitalization helped in identifying more ADL problems encountered by patients during the first 3 months post-discharge period as COPM served to identify more treatment goals and plans of action. Use of the COPM had no impact on the patients’ ADL performance, and the difference is so small that COPM may be of little clinical consequence.
Keywords: Activities of daily living (ADL), Canadian Occupational Performance Measure (COPM), Occupational therapy, Rehabilitation, Lumbar spinal fusion
Introduction
Although lumbar spinal fusion procedures has been performed for more than 70 years, only a few studies have investigated rehabilitation following the lumbar spinal fusion [4, 6, 7, 15]. A study published in 2010 examined the effect of pre-habilitation and early rehabilitation after spinal surgery and found overall improved function and shortened the hospitalization [13]. A study from 1997 documented that within the first 10 weeks after discharge from the hospital, lumbar spinal fusion patients experienced a wide spectrum of problems related to activities of daily living (ADL) [4]. In order to prepare the patient for the post-surgery period, it is important to obtain insight into the patient’s activity level during the post-discharge period. A client-centred approach might help the occupational therapist in creating a productive dialogue to prepare the patient for the challenges they will meet following the discharge. In a client-centred approach, the patients are recognized as active participants in their own rehabilitation process. Ideally, they should also be active participants in both the definition and solutions to their problems [14].
The Canadian Occupational Performance Measure (COPM), a validated tool developed for the use in occupational therapy, is a standardized semi-structured interview that focuses on a client-centred approach [19]. The COPM is used by occupational therapists throughout the world; by means of an interview, the occupational therapist and the patients jointly identify the patient’s problems in performing ADL. Since its first publication in 1991, the COPM manual, has been translated into 24 languages and is used in more than 35 countries [5, 11].
The clinical efficacy of the COPM used with adults has been examined in several studies. A study from 2002 examined patients with different diagnoses and requiring post-discharge rehabilitation. This study concluded that the use of the COPM during rehabilitation helped the patients to participate more extensively in defining their own rehabilitation goals. Furthermore, using the COPM improved the patients’ ability to manage ADL after the rehabilitation period [20].
Although the COPM has been examined on other categories of patients with back problems and found to be a useful tool in identifying the patients’ problems in performing ADL, there are yet no published studies that evaluate the COPM in relation to spinal surgery [2, 8, 16]. Despite its worldwide use by occupational therapists, no studies have examined the tool either in a randomised clinical study or in terms of its applicability to lumbar spinal fusion patients. Based on this knowledge we found it relevant to examine the use of the COPM in rehabilitation after a lumbar spinal fusion.
Hypothesis
Using the COPM during in-hospital rehabilitation will help identify more ADL problems that patients encounter after discharge from the hospital
Using the COPM during in-hospital rehabilitation will enhance the patients’ performance of ADL within the first 3 months after discharge from the hospital.
We aimed to examine whether or not the use of the semi-structured interview COPM during the in-hospital rehabilitation could:
identify more ADL problems that patients encounter after discharge from the hospital
enhance the patients’ performance of ADL after discharge from the hospital
Materials and methods
In the period from September 15, 2003 through June 15, 2004, patients who had undergone a lumbar spinal fusion due to degenerative disc diseases at a university centre were invited to participate in the randomized clinical study (RCT). Exclusion criteria were:
age younger than 18 years
requiring an interpreter during treatment
suffering from senile dementia
hospitalized directly from a psychiatric institution
nursing home resident
The patients meeting, the inclusion criteria were approached either on the first post-surgery day or as soon as they were able to receive information about the conditions associated with participation in the study. The patients were randomly assigned by the use of sealed envelopes to an experimental group (+COPM group) or a standard treatment group (−COPM group). The person who included the patients did not participate in the treatment. Based on the conditions of the study, it was not possible to blind neither the occupational therapists, nor the patients.
The experimental and the control group were treated by different occupational therapists. All four participating occupational therapists were experienced in treating lumbar spinal fusion patients. The patients in the −COPM group received the usual treatment, including the instruction in using aids and appliances for bath and dressing activities and, when necessary, guidance in connection with kitchen activities. For the patients in the +COPM group, the COPM was used as the starting point for the occupational therapy. The semi-structured interview was used to identify the patients ADL-related problems. The patients rated the importance of these problems on a 10-point scale from “not important at all” to “extremely important”. For the five most important problems the patients also rated their current performance on a 10-point scale from “not able to do it” to “able to do it very well”. Furthermore, the patients rated their satisfaction with their performance on a 10-point scale from “not satisfied at all” to “extremely satisfied”. Rehabilitation strategies were defined on the basis of the identified problems. After defining the goals, the occupational therapist met with the physiotherapist and nursing staff to determine a joint course of action and to include the patient’s goals in relation to occupational therapy, physiotherapy and nursing care. The occupational therapists treating both the +COPM and the −COPM groups were asked to document: ADL problems, rehabilitation goals and plans of action under pre-printed headings in the occupational therapy journal; for years, this procedure has been the standard occupational therapy procedure. Furthermore, they were asked to document their time consumption.
The primary outcome measure of this study was the concurrent identification of ADL problems during the in-hospital rehabilitation and 3 months after discharge from the hospital. There were four secondary outcome measures; a questionnaire composed for this study, Dallas Pain Questionnaire (DPQ) [9], length of hospitalization and duration of sick leave. The questionnaire composed for this study concerns a wide spectrum of ADL problems involving 19 specific activities (Table 1). For each of the 19 activities, the patients were asked to rank the importance of the activity and to evaluate their performance and their satisfaction with the performance of the activity. The questionnaire was pilot-tested on nine patients and adjusted. It was then sent to the patients 1 week, 1 month, 3 months and 3 years after discharge from the hospital, respectively. At the 3 year follow-up, the patients also received the DPQ [10].
Table 1.
Areas in questionnaire developed for the study
| 18 areas of activities of daily living |
|---|
| Dressing activities |
| Take a shower |
| Take a stand-up bath |
| Use the toilet |
| Tidy up the home |
| Carry out simple cleaning tasks |
| Carry plates from the table, water the flowers, or carry out other easy tasks in the home |
| Do simple cooking |
| Fold the laundry |
| Change light bulbs, repair small things and carry out other practical work in the home |
| Move around inside the home |
| Move around outside the home |
| Light grocery shopping |
| Use public transportation |
| Be a passenger in a car |
| Work outside your home |
| Have visitors |
| Go on visits |
For each of the 18 areas, the patients rate the importance of the activities, their present performance level and their satisfaction with their performance
Power
Because it was not possible to estimate the power according to the primary outcome measure, power calculation was based on the secondary outcome measure, the Dallas Pain Questionnaire. Based on earlier studies the standard deviation of the DPQ daily activity score was set at 25 points. A 15-point difference in this category was considered clinically significant. To fulfil these criteria, the study would need 43 patients in each group [1].
Data analysis
All data were entered twice in EpiData and possible divergence was corrected according to the original material. STATA 9.0 was used for the statistical evaluation. The risk of a type 1 error was set to 5% (significance level, 0.05). The answers from the questionnaires were ordinal data for which the Wilcoxon rank sum test was used. For comparison of proportions, the Chi-square or Fisher’s exact test was used.
Results
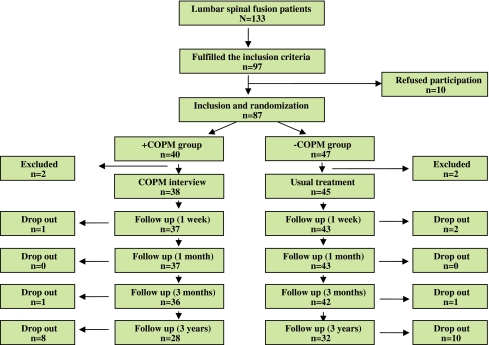
At our university clinic a total of 133 went through lumbar spinal fusion during the inclusion period. Thirteen were excluded due to cancer and 23 patients due to spinal fracture diagnosis. A total of 97 patients fulfilled the inclusion criteria, and 87 patients (mean age 55, range 19–81, 35% males) agreed to participate in the study (Fig. 1, Table 2).
Fig. 1.
Flow diagram
Table 2.
Basic data for the experimental and control groups
| Subject | N (+COPM/−COPM) | +COPM group | −COPM group |
|---|---|---|---|
| Gender (male) | 40/47 | 35% | 34% |
| Transfer before primary training | 40/47 | 5% | 4% |
| Age (mean) | 40/47 | 54.5 years | 54.6 years |
| Living alone | 40/47 | 29.7% | 14.3% |
| Living with a partner | 40/47 | 59.5% | 81% |
| Alternative living arrangements | 40/47 | 10.1% | 4.8% |
| Children living at home | 40/47 | 22.2% | 35.7% |
| Working/sick leave | 40/47 | 44.4% | 45.2% |
| Unemployed | 40/47 | 8.3% | 9.5% |
| Retired from work | 40/47 | 47.2% | 45.2% |
| Previous lumbar spinal fusion | 40/47 | 23.6% | 27.6% |
| Follow-up after 1 week | 40/47 | 92.5% | 91.5% |
| Follow-up after 1 month | 40/47 | 92.5% | 89.4% |
| Follow-up after 3 months | 40/47 | 90% | 89.4% |
| Follow-up after 3 years | 40/47 | 70% | 68% |
| Diagnosis | |||
| Disc. degeneration/spondylosis | 40/47 | 29 (72%) | 28 (60%) |
| Instability/spondylitis | 40/47 | 11 (28%) | 19 (40%) |
| Spondylodesis procedure | |||
| ALIF | 40/47 | 2 (5%) | 2 (4%) |
| PLF without instrumentation | 40/47 | 9 (23%) | 7 (15%) |
| PLF with instrumentation | 40/47 | 19 (47%) | 27 (58%) |
| TLIF | 40/47 | 10 (25%) | 11 (23%) |
| Fusion and decompression | 40/47 | 17 (43%) | 22 (47%) |
ALIF anterior lumbar interbody fusion, PLF posterior lumbar fusion, TLIF transforaminal lumbar interbody fusion
The follow-up rate was 91% after 3 months 69% after 3 years (Table 2). The patients in the +COPM and in the −COPM groups were comparable according to age, gender, transfer to another hospital before primary training, working status and levels of spinal fusion. However, random selection resulted in more patients in the −COPM group who were living with a partner (81%) compared to the +COPM group (59.5%). Additionally, more patients in the −COPM group (35.7%) had children living at home in comparison to the +COPM group (22.2%) (Table 1).
The ten patients who chose not to participate in the study were considerably older than the patients who opted to participate, with a mean age of 71 (range 44–81) compared to a mean age of 55 (range 18–81) for the participating patients. As shown in Fig. 2, two patients in each group were subsequently excluded because they were transferred to another hospital before primary training. Two patients in the +COPM group were lost to follow-up after 3 months and another eight at 3 years follow-up. In the −COPM group, three patients were lost to follow-up after 3 months and another ten after 3 years (Fig. 1).
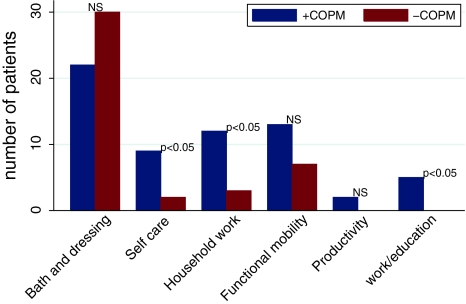
Fig. 2.
ADL problems important to the patient after discharge
Occupational therapists in both groups were asked to document ADL problems, rehabilitation goals and plans of action. As illustrated in Fig. 2, adhering to normal practice revealed significantly less information about ADL problems related to work/education when compared to the use of the COPM (p = 0.046). Use of the COPM identified significantly more problems in the areas of self-care (p < 0.05) and household work (p < 0.01) compared to the −COPM group (p < 0.05). In the +COPM group, the median number of treatment goals was 1.5 (range 0–5) compared to the −COPM group with 0.0 treatment goals (range 0–2) (p < 0.0001). Likewise, more plans of action were defined in the +COPM group with a median of 1.6 (1.2; 2.1) compared to 1.1 (0.8; 1.3) in the −COPM group (p = 0.01).
As expected, the use of COPM helped in identifying more ADL problems encountered by the patients during the first 3 months post-discharge period. The median number of ADL problems was 2.1 (1.5; 2.7) in the +COPM group compared to 0.9 (0.7; 1.2) in the −COPM group (p < 0.0001). Also, significantly more rehabilitation goals were identified for the +COPM group with a median = 5 (range 0–5) compared to the median = 0.0 (range 0–2) for the −COPM group (P < 0.0001). Similarly, more plans of action were established for the +COPM group compared to the −COPM group (P = 0.1).
No statistically significant difference in the occupational therapists’ reported time-consumption was found in the two groups (p < 0.05). However, in the +COPM group, the occupational therapist used 30 min more on work that did not entail direct involvement with the patients compared to the −COPM group (p < 0.0001).
As seen in Table 3, the use of the COPM did not result in any significant difference regarding the patients’ evaluation of ADL performance or satisfaction with this performance during the post-discharge period. These results were similar when measured with the DPQ at 3 year follow-up (Table 4).
Table 3.
ADL performance and satisfaction
| Post-surgery | n +COPM/−COPM | +COPM Median (25p.;75.p) | −COPM Median (25p.;75.p) | p value |
|---|---|---|---|---|
| Performance | ||||
| 1 week | 37/43 | 3.1 (2.3:3.6) | 2.9 (2.2:3.6) | 0.40 |
| 1 month | 37/43 | 2.8 (2.4:3.4) | 2.4 (2.1:3.4) | 0.75 |
| 3 months | 36/42 | 2.2 (1.8:2.9) | 2.4 (1.9:2.9) | 0.64 |
| 3 years | 28/32 | 1.5 (1.1:2.5) | 2.0 (1.3:3.0) | 0.26 |
| Satisfaction | ||||
| 1 week | 37/43 | 3.0 (2.3:3.6) | 2.9 (2.1:3.5) | 0.81 |
| 1 month | 36/42 | 2.8 (2.2:3.5) | 2.8 (2.1:3.6) | 0.81 |
| 3 months | 36/42 | 2.3 (1.8:3.1) | 2.5 (2.0:3.0) | 0.61 |
| 3 years | 28/32 | 1.7 (1.1:2.4) | 2.2 (1.3:3.0) | 0.11 |
Performance: 1 very good, 2 good, 3 fairly good, 4 rather poor, 5 poor, 6 unacceptable
Satisfaction: 1 very satisfied, 2 satisfied, 3 fairly satisfied, 4 rather discontented, 5 discontented, 6 unacceptable
Table 4.
Dallas Pain Questionnaire
| Subject | n (+COPM/−COPM) | +COPM group median (25å; 75p) | −COPM group median (25p; 75p) | p value |
|---|---|---|---|---|
| Daily activities | 28/32 | 38.0 (25.7:50.3) | 45.1 (34.6:55.5) | 0.37 |
| Work/leisure | 28/32 | 37.2 (22.5:51.8) | 47.4 (33.7:61.1) | 0.30 |
| Anxiety/depression | 28/32 | 25.9 (15.2:36.6) | 31.0 (21.4:40.6) | 0.47 |
| Social concerns | 28/32 | 24.9 (13.1:36.7) | 26.2 (17.9:34.4) | 0.86 |
| Total | 28/32 | 33.0 (21.5:44.7) | 39.4 (30.4:48.5) | 0.38 |
Follow-up after 3 years. The patients score their problems on a VAS-scale, where 0% corresponds to “no problems” and 100% corresponds to “maximum problems”
Discussion
Our results indicate that the use of the COPM improved identification of the ADL problems encountered during the first 3 months after discharge. The documentation of ADL problems was a part of the normal rehabilitation strategy. In order to ensure homogeneous documentation in the two groups, the occupational therapists were asked to document under pre-printed headings. Our results are similar to McColl, et. al., who found a good correlation between the ADL problems identified by the COPM and the problems the patients meet in their everyday life after completing rehabilitation [12]. In a study from 2004, Wals, et. al. found that the COPM is a good tool for identifying ADL problems in patients with chronic low back pain. This patient group is relatively similar to the group of patients included in our study [3].
We also found the COPM to provide an efficient means of identifying rehabilitation goals and plans of action in the patients’ designated areas of importance. This tallies well with the findings of a 2002 qualitative study, which concluded that the use of the COPM made it easier to define relevant rehabilitation goals and plans of action [22]. A study on the multimodal use of COPM for rheumatic patients showed similar results [21].
The −COPM group displayed a tendency to identify a larger number of important ADL problems in the “bath” and “dressing” categories than the +COPM group. This result was not unexpected, because bathing and dressing activities are always an issue in the conventional occupational therapeutic treatment regardless of the patients’ priorities.
The results of this study indicate that the COPM can identify work-related problems. If work-related problems are identified at an early stage, it provides an opportunity to prepare a better and safer return to work. The two groups in our study showed, however, no significant difference regarding sick leave.
Use of the COPM did not result in any significant difference regarding the patients’ evaluation of ADL performance. Our power calculation estimated the need of 86 patients to be included in the study. Eighty-seven patients were enrolled, but due to the lost-to-follow-up-rate we cannot rule out that the results are not powerful enough to show a difference.
In order to prevent reduced patient compliance, only the questionnaire composed for this study was used in the first three follow-ups. However, recent findings from a study with a similar patient category published in 2006 indicated that multiple questionnaires do not necessarily reduce patient compliance [17]. Therefore, at the 3 year follow-up we chose to send both the questionnaire composed for this study and the DPQ to the patients for final follow-up. As expected, the COPM had no long-term impact on the patients’ ADL performance.
The COPM focuses on the patients’ ADL performance in the immediate post-surgery period, where spinal fusion patients encounter a wide range of ADL-related problems [4]. In a follow-up study from 2002, Wressle, et. al. concluded that using the COPM in rehabilitation improved the patients’ ADL performance 4 weeks after the rehabilitation period [18]. These results, combined with clinical experience, led us to expect that a possible clinically significant difference would occur within the first 3 months of the post-discharge period. However, we found no difference in the patients’ ADL performance, neither in the post-surgery period nor in the long run (3 years).
The occupational therapists did not spend significantly more time with the patients in the +COPM group than in the −COPM group, indicating that the use of the COPM is not more time-consuming per se. However, it is worth noting that the intervention group did not spend more time on training, even though this group was reported to have significantly more ADL problems in the areas of self-care and household work, areas traditionally addressed by occupational therapy. This could be due to the fact that no additional training was required, or that the time set aside for extra training was used in other areas of the occupational therapist’s work. The latter could be the reason, why the use of the COPM did not result in any significant improvement in the patients’ evaluation of ADL performance.
Because the COPM was not implemented as a standard treatment in the rehabilitation program, and because the +COPM and the −COPM groups did not show any significant difference regarding the length of hospitalization, it has not been possible to conclude whether or not the COPM is cost-effective. However, we find that the extra cost affiliated with performing the +COPM procedure is minimal.
Since the patients were consecutively included and only a few patients chose not to participate in the study, the results seem to have a good external validity for spinal fusion patients with degenerative diseases. The results could also be relevant for patients who have undergone a lumbar spinal fusion necessitated by other ailments such as lumbar spinal fracture or cancer. These patients are most likely confronted with similar ADL problems in the post-discharge period.
Conclusion
Use of the COPM during hospitalization helped in identifying more ADL problems encountered by patients during the first 3 months post-discharge period as COPM served to identify more treatment goals and plans of action. Use of the COPM had no impact on the patients’ ADL performance, and the difference is so small that COPM may be of little clinical consequence. The main clinical conclusion is that it might not be worth the time of an OT to use the COPM on this group of patients.
Acknowledgments
This study received financial support by The Danish Research Foundation of Occupational Therapy.
Conflict of interest None.
References
- 1.Andersen T, Christensen FB, Egund N, et al. The effect of electrical stimulation on lumbar spinal fusion in older patients: a randomized, controlled, multi-center trial: part 2: fusion rates. Spine (Phila Pa 1976) 2009;34(21):2248–2253. doi: 10.1097/BRS.0b013e3181b02c59. [DOI] [PubMed] [Google Scholar]
- 2.Andrew WD, Jane KS, Sebastian JP, Rajkumar S, Bennetts K. Performance problems of patients with chronic low-back pain and the measurement of patient-centered outcome. Spine. 2004;29(1):87–93. doi: 10.1097/01.BRS.0000105533.09601.4F. [DOI] [PubMed] [Google Scholar]
- 3.Andrew WD, Jane KS, Sebastian JP, Rajkumar S, Bennetts K. Performance problems of patients with chronic low-back pain and the measurement of patient-centered outcome. Spine. 2004;29(1):87–93. doi: 10.1097/01.BRS.0000105533.09601.4F. [DOI] [PubMed] [Google Scholar]
- 4.Budge G. An evaluation of the occupational therapy for spine fusion hip spica patients. Br J Occup Ther. 1997;60(8):365–369. [Google Scholar]
- 5.Carswell A, McColl MA, Baptiste S, et al. The Canadian Occupational Performance Measure: a research and clinical literature review. Can J Occup Ther. 2004;71(4):210–222. doi: 10.1177/000841740407100406. [DOI] [PubMed] [Google Scholar]
- 6.Christensen FB. Lumbar spinal fusion. Outcome in relation to surgical methods, choice of implant and post-operative rehabilitation. Acta Orthop Scand Suppl. 2004;75(313):2–43. [PubMed] [Google Scholar]
- 7.Christensen FB, Laurberg I, Bunger CE. Importance of the back-cafe concept to rehabilitation after lumbar spinal fusion: a randomized clinical study with a 2-year follow-up. Spine. 2003;28(23):2561–2569. doi: 10.1097/01.BRS.0000097890.96524.A1. [DOI] [PubMed] [Google Scholar]
- 8.Dagfinrud H, Kjeken I, Mowinckel P, Hagen KB, Kvien TK. Impact of functional impairment in ankylosing spondylitis: impairment, activity limitation, and participation restrictions. J Rheumatol. 2005;32(3):516–523. [PubMed] [Google Scholar]
- 9.Lawlis GF, Cuencas R, Selby D, McCoy CE. The development of the Dallas Pain Questionnaire. An assessment of the impact of spinal pain on behavior. Spine. 1989;14(5):511–516. doi: 10.1097/00007632-198905000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Lawlis GF, Cuencas R, Selby D, McCoy CE. The development of the Dallas Pain Questionnaire. An assessment of the impact of spinal pain on behavior. Spine. 1989;14(5):511–516. doi: 10.1097/00007632-198905000-00007. [DOI] [PubMed] [Google Scholar]
- 11.McColl MA, Law M, Baptiste S, et al. Targeted applications of the Canadian Occupational Performance Measure. Can J Occup Ther. 2005;72(5):298–300. doi: 10.1177/000841740507200506. [DOI] [PubMed] [Google Scholar]
- 12.McColl MA, Paterson M, Davies D, Doubt L, Law M. Validity and community utility of the Canadian Occupational Performance Measure. Can J Occup Ther. 2000;67(1):22–30. doi: 10.1177/000841740006700105. [DOI] [PubMed] [Google Scholar]
- 13.Nielsen PR, Jorgensen LD, Dahl B, Pedersen T, Tonnesen H. Pre-habilitation and early rehabilitation after spinal surgery: randomized clinical trial. Clin Rehabil. 2010;24(2):137–148. doi: 10.1177/0269215509347432. [DOI] [PubMed] [Google Scholar]
- 14.Pollock N. Client-centered assessment. Am J Occup Ther. 1993;47(4):298–301. doi: 10.5014/ajot.47.4.298. [DOI] [PubMed] [Google Scholar]
- 15.Sogaard R, Bunger CE, Laurberg I, Christensen FB. Cost-effectiveness evaluation of an RCT in rehabilitation after lumbar spinal fusion: a low-cost, behavioural approach is cost-effective over individual exercise therapy. Eur Spine J. 2008;17(2):262–271. doi: 10.1007/s00586-007-0479-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Toomey M, Nicholson D, Carswell A. The clinical utility of the Canadian Occupational Performance Measure. Can J Occup Ther. 2002;62(5):242–249. doi: 10.1177/000841749506200503. [DOI] [PubMed] [Google Scholar]
- 17.Videbaek TS, Christensen FB, Soegaard R, et al. Circumferential fusion improves outcome in comparison with instrumented posterolateral fusion: long-term results of a randomized clinical trial. Spine. 2006;31(25):2875–2880. doi: 10.1097/01.brs.0000247793.99827.b7. [DOI] [PubMed] [Google Scholar]
- 18.Wressle E, Eeg-Olofsson AM, Marcusson J, Henriksson C. Improved client participation in the rehabilitation process using a client-centred goal formulation structure. J Rehabil Med. 2002;34(1):5–11. doi: 10.1080/165019702317242640. [DOI] [PubMed] [Google Scholar]
- 19.Wressle E, Eeg-Olofsson AM, Marcusson J, Henriksson C. Improved client participation in the rehabilitation process using a client-centred goal formulation structure. J Rehabil Med. 2002;34(1):5–11. doi: 10.1080/165019702317242640. [DOI] [PubMed] [Google Scholar]
- 20.Wressle E, Eeg-Olofsson AM, Marcusson J, Henriksson C. Improved client participation in the rehabilitation process using a client-centred goal formulation structure. J Rehabil Med. 2002;34(1):5–11. doi: 10.1080/165019702317242640. [DOI] [PubMed] [Google Scholar]
- 21.Wressle E, Lindstrand J, Neher M, Marcusson J, Henriksson C. The Canadian Occupational Performance Measure as an outcome measure and team tool in a day treatment programme. Disabil Rehabil. 2003;25(10):497–506. doi: 10.1080/0963828031000090560. [DOI] [PubMed] [Google Scholar]
- 22.Wressle E, Marcusson J, Henriksson C. Clinical utility of the Canadian Occupational Performance Measure—Swedish version. Can J Occup Ther. 2002;69(1):40–48. doi: 10.1177/000841740206900104. [DOI] [PubMed] [Google Scholar]