Abstract
Background
In Germany, prostate cancer is the leading cause of cancer and the third leading cause of death from cancer in males. We investigate prostate cancer in Gernmany among migrants from the Former Soviet Union (FSU) and compare them to indigenous German population with regard to prostate cancer incidence, mortality and longitudinal effects.
Methods
Data were obtained from two migrant cohorts residing in the federal states of North Rhine Westphalia (n=34,393) and Saarland (n=18,619). Vital status was ascertained through local population registries. Causes of death were obtained from the federal statistical office or from local health authorities. Cancer incidence of the Saarland cohort was derived from the Saarland Cancer Registry using record linkage.
Results
From 1990 to 2005 we observed 3360 deaths of which 28 were due to prostate cancer. In the Saarland cohort 35 men were diagnosed with prostate cancer during the respective period. Migrants had lower prostate cancer incidence (SIR 0.74 (95% CI: 0.52–1.03)) and mortality (SMR 0.57 (95% CI: 0.38–0.83)) compared to the German population. Multivariate analysis showed a strong age effect on incidence meaning young migrants (below age 60) were diagnosed significantly more often with prostate cancer compared to Germans of the same age. However, mortality did not show any effects.
Discussion
Lower prostate cancer mortality and incidence among migrants may reflect an ongoing situation in the FSU. Additionally, longitudinal analysis did not reveal convergence of migrant prostate cancer to German rates as expected from lifestyle driven cancer sites. Therefore, our results support the hypothesis of a genetic effect on prostate cancer risk.
Keywords: prostate cancer, mortality, incidence, migrants, cohort study, Germany, Russia
Known risk factors for prostate cancer explain only a small proportion of all cases, and also factors affecting the progression of the disease are largely unknown. Male sex hormones and the aging process contribute to the development of prostate cancer, and a genetic predisposition has been discussed, because of a higher incidence observed for several ethnic groups, disease onset at a younger age, and family clustering of the disease (1). There are few findings on risk factors relating to lifestyle, diet or the environment. Possible risk factors are high intakes of α-linolenic acid and calcium (1–3). Additionally, there are studies showing an association between an early onset prostate cancer risk and a relatively high intake of total fat and fat derivatives, e.g. Lophatananon et al. (4). Known lifestyle risk factors for other cancer sites such as tobacco smoking, alcohol consumption and low physical activity do not seem to affect prostate cancer risk.
In Germany, prostate cancer is the most frequent cancer (26%) and the third leading cause of death from cancer in males (10%). Mean ages of diagnosis and death from prostate cancer are about 70.1 years and 77.5 years, respectively (5). Relative 5-year survival rates are about 90% (5).
Presently, there is a statutory screening programme for prostate cancer in Germany. Men aged 45 years and over are asked once a year by their physician if they have any symptoms. This screening also includes an examination of the sexual organs, the lymph nodes, as well as a palpation examination of the prostate via the rectum. The prostate-specific antigen (PSA) blood test is not part of the statutory screening, however, more and more PSA testing is offered to patients as an additional service. Therefore, incidence trends began to continuously increase. Since 1980, the age-standardised incidence rate increased by 110% (6). In 2008, it was 82.7 per 100,000 men (standardised to Segi) (7, 8). On the other hand, age-standardised mortality rates have been more or less stable during the last decades and began to fall slightly since 1995. In 2006, the age-standardised mortality rate was 12.3 per 100,000 men (9).
Mortality of prostate cancer in Germany is among the lowest in Europe, whereas incidence is around the European average (10). Some of the lowest prostate cancer rates with regard to mortality and incidence are seen in South-East Asia. In contrast, Scandinavian countries are among those with the highest prostate cancer mortality worldwide. Prostate cancer mortality rates are also estimated to be high in some African and South American countries (8). A country-specific comparison shows that high prostate cancer incidence rates do not necessarily mean high mortality rates and vice versa (10).
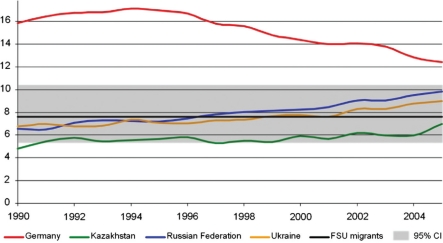
In countries of the Former Soviet Union (FSU) mortality from prostate cancer is lower compared to Germany, however, during the last years the difference shrinks continuously (see Fig. 1). In 2006, age-standardised mortality rates were 5.7 in Kazakhstan, 10.1 in the Russian Federation and 9.3 in Ukraine (9). Convergence of German and FSU prostate cancer mortality is probably due to differences in treatment, survival and an overall increasing life expectancy in the FSU.
Fig. 1.
Age-standardised prostate cancer mortality rates per 100,000 (Segi Standard).
The FSU incidence from prostate cancer is much lower compared to Germany. In 2008, age-standardised incidence rates are estimated to be 10.9 in Kazakhstan, 26.1 in the Russian Federation and 20.3 in Ukraine (8). Low incidence in countries of the FSU is likely to be the result of fewer prostate specific antigen testing and maybe also a general underestimation of cancer incidence. This results in an incidence:mortality ratio of about 7 in Germany and only about 2 in Kazakhstan, 2.5 in the Russian Federation and 2 in Ukraine.
Since the beginning of the 1990's more than two million ethnic German migrants from the FSU came to Germany. Previous studies revealed unanticipated mortality patterns of these migrants: They had a lower overall mortality, mainly determined by a low mortality from cardiovascular disease (11, 12). In contrast, males had a higher risk to die from external causes and deaths associated with these causes such as mental and behavioural disorders due to substance use (13). Overall cancer mortality of migrants was similar to the German population with great variations for specific cancer sites: lung cancer was elevated among males, but lower among females; stomach cancer was higher contrasting with lower ratios for prostate cancer, male colorectal cancer and female breast cancer. Based on an incomplete follow up procedure cancer incidence rates of the migrants were estimated to be similar to their mortality rates (14).
Several epidemiological studies on incidence and mortality of migrants have led to new findings on the etiology of diseases, but may also have important implications with regard to development of targeted cancer prevention and early detection strategies (16–18).
In this study, we compare prostate cancer mortality of two ethnic German migrant cohorts and prostate cancer incidence of one cohort to the autochthonous German population. Additionally, we investigated longitudinal effects of age, calendar year and years since migration to Germany which may help to understand (1) the health care utilisation of the migrants and (2) the influence of genetic versus lifestyle dependent effects. Converging prostate cancer rates of the migrants may be expected if lifestyle dependent factors influence the development of disease, which has already been shown for stomach cancer (19).
Methods
Study population
The study population consisted of two migrant cohorts from the FSU residing in two different federal states of Germany: North Rhine Westphalia (NRW) and Saarland.
To setup the NRW cohort routine data was provided from the migrant reception centre of NRW. The original dataset included all 281,356 ethnic German migrants from countries of the FSU who settled in NRW between 1990 and 2001 and contained information on name, date of birth, date of arrival in Germany, sex, country of origin and first city of residence. After sample size calculation the cohort was restricted to a representative sample of 34,393 migrants according to the spatial distribution and urban/rural proportion who were at least 15 years old when they migrated to Germany. Selection procedures and methodological details are described in detail elsewhere (20).
The migrant reception centre of the Saarland could not provide complete dataset with the above mentioned information on the migrants. As an alternative, all local refugee offices of the Saarland were contacted to get access to their available data. Eligibility criteria for the Saarland cohort were arrival between 1990 and 2005 from countries of the FSU. All together information on 26,384 migrants (more than 90% of all German migrants who settled in the Saarland during the respective period) were available. The dataset contained name, date of birth, issue date of a German passport as an approximation for date of migration, sex, country of birth for about 70% of the cohort and first city of residence. The final cohort consisted of a sample of 18,619 individuals with complete information.
To ascertain vital status of each cohort member until the 31st December 2005 a follow up procedure was performed: letters were sent to local registry offices in the cities of residence assessing the status of individuals. If migrants moved, the new residence and date of moving was provided. Then the local registry office of the destination was contacted and so on until the individual could be located. Changes of residence were recorded in a database with the exact date of moving. In the case of death, date and place of death were provided by the local registry office.
Cause of death was either ascertained through a record linkage system of the regional statistical office or through local health authorities (21). In case of contacting local health offices an anonymised copy of the relevant death certificate was provided. Causes of death were coded according to the International Classification of Diseases.
For the Saarland cohort a cancer incidence follow up was directly done by the Saarland Cancer Registry. Record linkage was performed using name, sex, date of birth and place of residence. The possibility to change surname and first name is often used by these migrants during the first years of stay in Germany and did therefore not allow a simple identification by name. To minimise this problem matching procedure additionally included the phonetic of the names. Forty-three cases were not considered in the analysis because individuals were already diagnosed with cancer in their country of origin. All analyses were restricted to the first cancer, multiple tumours were not considered.
Statistical methods
For evaluation of the migrants’ incidence and mortality in comparison to the host population reference rates are needed. Analysis of mortality was done in comparison to the German population as standardized mortality ratio (SMR). German mortality rates were calculated using the WHO mortality database (9). For calculation of the standardized incidence ratio (SIR) we used data from the Saarland Cancer Registry which has population figures and incidence data for the full observation period 1990–2005. Person-time was computed as person-years (PY) to calculate the expected number of cases for indirect standardization. Exact 95% confidence intervals for SMR and SIR were calculated.
In a multivariable model we analysed simultaneously the effects of age group, calendar year, and years since migration to Germany. The effect of these covariables on (1) incidence rates, (2) mortality rates, (3) SIR and (4) SMR was modelled with Poisson regression (22). The covariable effects for each variable separately and for the model overall was given by likelihood-ratio tests. Age standardised rates were adjusted to the Segi population. For mortality analysis additionally the variable ‘cohort’ (NRW or Saarland) was considered. Analysis was performed using SAS version 9.2.
Results
Descriptive characteristics of both cohorts and results of the follow up procedure are presented in Table 1. The Saarland cohort was about half the size of the cohort in NRW. The arrival period for entering the cohort was four years longer for the Saarland cohort. The NRW study population was restricted by age at migration of 15 years or older; the Saarland cohort had no age restriction. Thus, the Saarland cohort was on average younger. Country of origin distribution was similar for both cohorts: around 55% of the migrants came from Kazakhstan, 37% from the Russian Federation. Other countries of the FSU contributed each less than 5%.
Table 1.
Descriptive results of both migrant cohorts, from North-Rhine Westphalia and Saarland
| Migrant cohort in the Federal State of NRW | Migrant cohort in the Federal State of Saarland | |
|---|---|---|
| Number of cohort members | 34,393 | 18,619 |
| Males (%) | 16,734 (48.7%) | 8,977 (48.2%) |
| Females (%) | 17,659 (51.3%) | 9,642 (51.8%) |
| Immigration period | 1990–2001 | 1990–2005 |
| 1990–1993 | 14,728 | 6,933 |
| 1994–1997 | 11,441 | 6,536 |
| 1998–2001/5 | 8,224 | 5,150 |
| Age restriction | 15+ | – |
| Mean age at migration | ||
| (standard deviation; range) | 40.0 (17.0; 15–97) | 32.4 (19.8; 0–103) |
| Males | 38.4 (16.0; 15–93) | 30.9 (19.0; 0–95) |
| Females | 41.5 (17.7; 15–97) | 33.8 (20.4; 0–103) |
| End of follow up date | 31-12-2005 | 31-12-2005 |
| Mean duration of follow up | 10.1 years | 8.0 years |
| Person-years | 346,671.5 | 148,313.1 |
| Males | 167,882.0 | 71703.4 |
| Females | 178,789.4 | 76,609.6 |
| Alive | 89.2% | 73.2% |
| Dead | 7.5% | 4.2% |
| Lost to follow up | 3.3% | 22.6% |
| Prostate cancer Incident cases | – | 35 |
| Deaths | 24 | 4 |
Overall, the NRW cohort accumulated 346,671.5 PY and the Saarland cohort 148,313.1 PY. Follow up of the NRW cohort was complete for 96.7% of the cohort members with a mean follow up time of 10.1 years. Overall 2,580 (7.5%) cohort members died. Causes of death were known for 94.8% of deceased persons. Also 1,138 (3.3%) persons were lost to follow up within the observation period, which means their last date of contact was censored. Individuals became lost follow up due to different reasons: moving abroad or moving to an unknown destination or insufficient data of the population registries.
In the Saarland cohort vital status was known for 77.4% of individuals. Mean follow up time was 8 years, while 87% of the lost individuals were censored at the day of leaving the study area because of moving to another federal state. Since the Saarland is a rather small state people are much more likely to move to another state compared to larger ones such as NRW. During the observation period 780 (4.2%) persons died. Cause of deaths was known through the Saarland Cancer Registry for all individuals diagnosed with cancer and those who died from cancer without prior diagnosis (death certificate only (DCO) cases). Between 1990 and 2005 448 cohort members of the Saarland cohort were diagnosed with a malignant neoplasm.
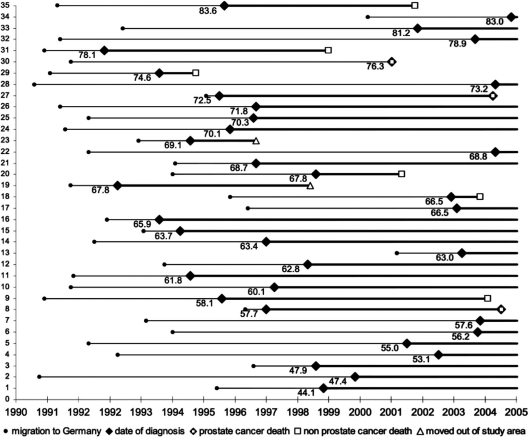
During the observation period 28 men died from prostate cancer in both cohorts. Their mean age of death was 76.9 years (Range: 60.8–92.1). In the Saarland cohort 35 men were diagnosed with prostate cancer. Mean age of diagnosis was 67.6 years (Range: 45.3–85.8). Fig. 2 displays follow up of all 35 incident prostate cancer cases starting with their migration to Germany, their age at diagnosis and their vital status at end of follow up. Most cases were alive at the end of the observation period. Two patients left Saarland and nine died during the observation period. Three of the deceased men died from prostate cancer; one of these was not registered during lifetime (DCO case).
Fig. 2.
Overview of all 35 incident prostate cancer cases from the Saarland cohort sorted by age at diagnosis.
Multivariate Poisson regression showed that mortality rates did not change appreciably over time. Age standardised mortality was 44.1 (95% CI: 32.0–62.1) per 100,000 individuals, respectively (see Fig. 1).
In comparison with the German resp. state of Saarland population we found that mortality from prostate cancer was strongly reduced among the migrants with an SMR of 0.57 (95% CI: 0.38–0.83, p<0.001, both cohorts combined). Prostate cancer incidence was also reduced among the migrants with a SIR of 0.74, however, the result was not significant (95% CI: 0.52–1.03, p=0.076) (see Table 2).
Table 2.
Standardised incidence and mortality ratios of the migrant cohorts in comparison to the German resp. state of Saarland population
| Observed | Expected | SIR/SMR (95% CI) | |
|---|---|---|---|
| Incidence (Saarland cohort) | 35 | 47.3 | 0.74 (0.52–1.03) |
| Mortality (both cohorts) | 28 | 48.7 | 0.57 (0.38–0.83) |
In further analysing the SMR, Poisson regression analysis showed little and insignificant effects of the considered covariables calendar year, years since migration, age and ‘cohort’ on the SMR (data not shown).
Results of modelling the SIR are shown in Table 3. Calendar year and age had a significant effect, while time since immigration showed no effect. The SIR decreased with increasing age and with increasing calendar year (models 2.1 and 2.2). This means that the incidence relative to the corresponding German population was most different for the old ages and for the early years of immigration. An interaction effect between age and year could not be seen, which, however, was unlikely given the low sample size (models 3.1 and 3.2).
Table 3.
Poisson regression analysis on prostate cancer incidence in comparison to the German population, state of Saarland
| Model | Variable(s). | Deviance | Difference of deviance* | df | pmodel | β | pβ |
|---|---|---|---|---|---|---|---|
| 0 | (Null model) | 269.5 | – | – | – | ||
| 1.1 | Calendar year | 265.3 | 4.2 | 1 | 0.04 | –0.09 | 0.04 |
| 1.2 | Years since immigration | 268.5 | 1.0 | 1 | 0.31 | –0.05 | 0.31 |
| 1.3 | Age | 266.6 | 2.9 | 1 | 0.09 | –0.17 | 0.08 |
| 1.4 | Age dichotomized (<60 vs. 60+) | 265.9 | 4.6 | 1 | 0.03 | –0.83 | 0.04 |
| 2.1 | Calendar year+Age | 262.2 | 7.3 | 2 | 0.03 | –0.09 | 0.03 |
| –0.18 | 0.07 | ||||||
| 2.2 | –0.09 | 0.03 | |||||
| Calendar year+Age (<60 vs. 60+) | 261.6 | 7.9 | 2 | 0.02 | |||
| –0.84 | 0.04 | ||||||
| 3.1 | –0.06 | 0.67 | |||||
| Calendar year+age+(calendar year)×(age) | 262.1 | 7.4 | 3 | 0.06 | –0.16 | ||
| –0.01 | 0.75 | ||||||
| –0.11 | 0.01 | ||||||
| Calendar year+age(<60 vs. 60+)+ | –0.55 | 0.30 | |||||
| 3.2 | (calendar year)×(age (<60 vs. 60+)) | 260.5 | 9.0 | 3 | 0.03 | –0.11 | 0.31 |
Relative to null model
Discussion
The aim of the study was to analyse prostate cancer mortality and incidence among ethnic German migrants who came to Germany from the FSU since the year 1990. Therefore, we analysed two cohorts of migrants in terms of prostate cancer mortality and incidence including longitudinal and age effects. As one main result we found that these migrants had significantly lower prostate cancer incidence and mortality compared to the German population.
Methodological aspects of the cohorts and the statistical analysis have been discussed in detail elsewhere (11, 14, 20). In brief, both cohort studies have the pros and cons of historical cohort studies. It was possible to give valid estimates of the migrant's mortality and incidence in terms of SMR and SIR. Indirect standardisation has proven to be more precise for rare outcomes compared to the direct standardisation method meaning the calculation of rates (23). However, we had only access to routine data and no information on access of health care or other lifestyle-related risk factors.
The analysis of prostate cancer mortality and incidence showed several different aspects. First, the descriptive comparison of the migrants’ mean age of death from prostate cancer to the Saarland population showed no difference with 76.9 and 77.5 years of age, respectively. However, mean age of diagnosis was 2.5 years earlier among the migrants.
Overall evaluation of prostate cancer showed lowered mortality in comparison to the German population. Based on regression analysis the estimated age-standardised mortality rates of the migrants were close to rates observed in the FSU (Fig. 1). Multivariate analysis did not show any longitudinal trends or difference to the age-specific prostate cancer mortality of the German population. However, we cannot rule out that this was due to the relatively small number of observed deaths.
Prostate cancer diagnosis was also reduced among the migrants, but not significantly. Incidence rates among the migrants were constant in contrast to German incidence which rises contiguously since the 1980s. Multivariate Poisson regression confirmed reduced diagnosis with calendar time in comparison to the German population especially among old migrants. A possible explanation might be differences in health seeking such as lower use of prostate cancer screening in younger migrants, however, there is no data available to check this hypothesis. In general, one has to be aware that measured incidence often represents rather a detection rate than the true incidence rate.
Ethnic German migrants from the FSU are a unique group of diaspora migrants. There are hardly any other examples in the world where such a big ethnic group has migrated in this short time period from one country to another. Prostate cancer mortality and incidence was lower among the migrants and somehow reflect the situation in the FSU. Additional analysis did not yet reveal any convergence of their prostate cancer mortality compared to German rates as it would be expected from lifestyle driven cancer sites. Therefore, our results may support the hypothesis of a genetic component on the development of prostate cancer. However, we cannot rule out that this is due to the limited number of observations.
There are few studies on Asian migrants living in the United States reporting increased prostate cancer incidence among those migrants compared to their countries of origin presumably due to changes in lifestyle and diet (24). On the other hand, prostate cancer rates of Asian migrants remain very low. Therefore increased rates might also be due to better detection.
The results also hint to the hypothesis that ethnic German migrants from the FSU are genetically different to the German population, which might be the result of positive or negative selection usually occurring during a migration process (25). However, previous analysis revealed hardly any selection of the migrants when the came to Germany after the fall of the Iron Curtain in 1989. So we believe selection might have occurred when the migrants went to Russia about 200 years ago (26). Yet, there are no studies about genetic differences on FSU migrants.
Acknowledgements
The study was funded by the German Research Foundation (DFG), Grant No. GK793.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Patel AR, Klein EA. Risk factors for prostate cancer. Nat Clin Pract Urol. 2009;6:87–95. doi: 10.1038/ncpuro1290. [DOI] [PubMed] [Google Scholar]
- 2.Grönberg H. Prostate cancer epidemiology. Lancet. 2003;361:859–64. doi: 10.1016/S0140-6736(03)12713-4. [DOI] [PubMed] [Google Scholar]
- 3.Hsing AW, Sakoda LC, Chua S., Jr Obesity, metabolic syndrome, and prostate cancer. Am J Clin Nutr. 2007 Sep;86:S843–S857. doi: 10.1093/ajcn/86.3.843S. [DOI] [PubMed] [Google Scholar]
- 4.Lophatananon A, Archer J, Easton D, Pocock R, Dearnaley D, et al. Dietary fat and early-onset prostate cancer risk. Br J Nutr. 2010;103:1375–80. doi: 10.1017/S0007114509993291. [DOI] [PubMed] [Google Scholar]
- 5.Ziegler H, Stabenow R, Holleczek B, Stegmaier C. Krebs im Saarland, Ministerium für Justiz. Available from: http://www.krebsregister.saarland.de/krebsatlas/EKRS_Krebsatlas_21082009.pdf [cited 3 May 2010]
- 6.Robert Koch Institute. Prostata (C61). Available from: http://www.rki.de/cln_169/nn_203956/DE/Content/GBE/DachdokKrebs/KID/Lokalisationen__Tabellen/C61,templateId=raw,property=publicationFile.xls/C61.xls [cited 5 April 2010]
- 7.Segi M. Cancer mortality for selected sites in 24 countries (1950–57) Sendai, Japan: Department of Public Health, Tohoku University of Medicine; 1960. [Google Scholar]
- 8.Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 Cancer incidence and mortality worldwide. Available from: http://globocan.iarc.fr [cited 12 January 2011]
- 9.WHO Mortality Database. Available from: http://www.who.int/healthinfo/morttables/en/index.html [cited 2 February 2011]
- 10.Cancer in Germany 2005/2006. Berlin: Robert Koch Institute and Association of Population-based Cancer Registries in Germany; 2010. Incidence and trends. 7th ed. [Google Scholar]
- 11.Becher H, Kyobutungi C, Laki J, et al. Mortalität von Aussiedlern aus der ehemaligen Sowjetunion: Ergebnisse einer Kohortenstudie. Deutsches Ärzteblatt. 2007;23:A-1655–62. (English version available from: http://www.aerzteblatt.de/int/article.asp?id=58120) [Google Scholar]
- 12.Ronellenfitsch U, Kyobutungi C, Becher H, Razum O. All-cause and cardiovascular mortality among ethnic German immigrants from the Former Soviet Union: a cohort study. BMC Public Health. 2006;6:16. doi: 10.1186/1471-2458-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ott JJ, Winkler V, Kyobutungi C, Laki J, Becher H. Effects of residential changes and time patterns on external cause mortality in migrants: results of a German cohort study. Scand J Public Health. 2008;36:524–31. doi: 10.1177/1403494807087293. [DOI] [PubMed] [Google Scholar]
- 14.Winkler V, Ott JJ, Holleczek B, Stegmaier C, Becher H. Cancer profile of migrants from the Former Soviet Union in Germany: incidence and mortality. Cancer Causes Control. 2009;20:1873–9. doi: 10.1007/s10552-009-9381-4. [DOI] [PubMed] [Google Scholar]
- 15.Marmot MG, Adelstein AM, Bulusu L. Lessons from the study of immigrant mortality. Lancet. 1984;1:1455–7. doi: 10.1016/s0140-6736(84)91943-3. [DOI] [PubMed] [Google Scholar]
- 16.McKeigue PM, Miller GJ, Marmot MG. Coronary heart disease in South Asians overseas – a review. J Clin Epidemiol. 1989;42:597–609. doi: 10.1016/0895-4356(89)90002-4. [DOI] [PubMed] [Google Scholar]
- 17.McKeigue PM, Shah B, Marmot MG. Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet. 1991;337:382–6. doi: 10.1016/0140-6736(91)91164-p. [DOI] [PubMed] [Google Scholar]
- 18.Grulich AE, Swerdlow AJ, Head J, Marmot MG. Cancer mortality in African and Caribbean migrants to England and Wales. Br J Cancer. 1992;66:905–11. doi: 10.1038/bjc.1992.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ronellenfitsch U, Kyobutungi C, Ott JJ, et al. Stomach cancer mortality in two large cohorts of migrants from the Former Soviet Union to Israel and Germany: are there implications for prevention? Eur J Gastroenterol Hepatol. 2009;21:409–16. doi: 10.1097/MEG.0b013e3283155220. [DOI] [PubMed] [Google Scholar]
- 20.Ronellenfitsch U, Kyobutungi C, Becher H, Razum O. Large-scale, population-based epidemiological studies with record linkage can be done in Germany. Eur J Epidemiol. 2004;19:1073–4. doi: 10.1007/s10654-004-1752-2. [DOI] [PubMed] [Google Scholar]
- 21.Klug SJ, Zeeb H, Blettner M. New research avenues in exploring causes of death in Germany via regional statistical offices as exemplified by a retrospective cohort study. Gesundheitswesen. 2003;65:243–9. doi: 10.1055/s-2003-39273. [DOI] [PubMed] [Google Scholar]
- 22.Breslow NE, Day NE., editors. Statistical methods in cancer research: Volume II-The design and analysis of cohort studies. Lyon: IARC Scientific Publications; 1987. Rates and Rate standardization; pp. 48–79. [PubMed] [Google Scholar]
- 23.23. McMichael AJ, Giles GG. Cancer in migrants to Australia: extending the descriptive epidemiological data. Cancer Res. 1988;48:751–6. [PubMed] [Google Scholar]
- 24.Lee J, Demission K, Lu SE, Rhoads GG. Cancer incidence among Korean-American immigrants in the United States and native Koreans in South Korea. Cancer Control. 2007;14:78–85. doi: 10.1177/107327480701400111. [DOI] [PubMed] [Google Scholar]
- 25.Jason G, Massey DS, Rosenzweig MR, Smith JP. Immigrant health: selectivity and acculturation. Available from: http://129.3.20.41/eps/lab/papers/0412/0412002.pdf [cited 5 March 2011]
- 26.Bade KJ, Oltmer J. Aussiedler: deutsche Einwanderer aus Osteuropa. Vol. 8. IMIS, ISBN 978-3-89971-120-2, Osnabrück; 1999. [Google Scholar]