Abstract
Multi-resistant pathogens are a serious problem on a considerable scale for the health sector. Patients with infections induced by multi-resistant bacteria cause enormous additional treatment costs of around 20,500 € per insured. Due to the recently used billing and documentation system there is a significant shortage of information transparency. The guidelines for hospital hygiene and infection prevention published by the Robert Koch Institute (RKI) include a presumption provision, which means that subject to compliance with these guidelines the observance of the current state of medical science is suspected. In case of a derogation, a scientific justification is necessary, which is used e.g. in connection with liability questions. Within the framework of legal reforms in 2011, the legislator aspires a nationwide improvement of hygiene quality in medical institutions and information transparency. Many specific issues about the general reporting obligation of infections with multi-resistant pathogens or about the standardized exchange of infection documentations between medical institution and health authority remain unresolved.
Regional, cross-sectoral networks create the base to tackle targeted measures collectively and may develop sustainable and tailored solutions for their region. With these considerations in mind, the project HICARE was founded in Mecklenburg-Vorpommern. The project pursues the aim to develop an intervention strategy against the spread of multi-resistant pathogens. Health insurances make an important contribution to quality of medical treatment by participation.
Keywords: cost analysis, Staphylococcus aureus, health insurance, project HICARE, infection documentation, Law of Infection Protection
Abstract
Multiresistente Erreger (MRE) stellen ein ernstzunehmendes Problem erheblichen Ausmaßes für den Gesundheitssektor dar. Patienten mit MRE induzierten Infektionen verursachen immense zusätzliche Behandlungskosten von rund 20.500 € pro Versichertem. Aufgrund des derzeit genutzten pauschalen Abrechnungs- bzw. Dokumentationssystems besteht ein erheblicher Mangel an Informationstransparenz. Die vom Robert Koch-Institut (RKI) veröffentlichen Empfehlungen zur Krankenhaushygiene und Infektionsprävention beinhalten eine sog. Vermutungsregelung, d.h. bei ihrer Einhaltung wird vermutet, dass der Stand der medizinischen Wissenschaft beachtet worden ist. Im Fall der Abweichung muss dafür eine wissenschaftliche Begründung gegeben werden, was z.B. bei Haftungsfragen zugrunde gelegt wird. Im Rahmen gesetzlicher Neuerungen strebt der Gesetzgeber 2011 eine bundesweite Verbesserung der Hygienequalität in medizinischen Einrichtungen sowie der Informationstransparenz an. Viele konkrete Fragen über die allgemeine Meldepflicht für Infektionen mit MRE oder über den standardisierten Austausch von Infektionsdokumentationen zwischen medizinischer Einrichtung und Gesundheitsbehörde bleiben jedoch weiterhin offen.
Regionale, sektorübergreifende Netzwerke schaffen die Basis, Maßnahmen gezielt im Team anzugehen und können auf diese Weise nachhaltige, für ihre Region zugeschnittene Lösungen entwickeln. Unter diesen Gesichtspunkten bildete sich auch das Projekt HICARE in Mecklenburg-Vorpommern heraus. Das Projekt verfolgt das Ziel, Interventionsstrategien gegen die Ausbreitung von MRE zu entwickeln. Krankenkassen leisten durch ihre Mitwirkung einen wichtigen Beitrag zur Versorgungsqualität.
Introduction
Bacterial multi-resistance of staphylococcus aureus (MRSA), enterobacteria (ESBL) and other pathogens is a serious problem for the treatment of infections. Such multi-resistant bacteria result worldwide in severe wound as well as surgical site infections, infections of the respiratory and urinary tract, in life-threatening systemic infections (sepsis) or severe gastrointestinal impairment and other diseases.
In Germany, every year 400,000 to 600,000 patients fall ill with hospital acquired infections (nosocomial infections) [1]. Nationwide, up to 15,000 people die from the consequences of these infections [1]. Experts estimate that at least one third of nosocomial infections are preventable. In addition, there are infections with multi-resistant microorganisms which are acquired outside of the hospital, so-called “community acquired” MRSA (caMRSA).
The discussion about appropriate measures in the battle against “hospital germs”, especially multi-resistant bacteria, stirs the German health care system currently because, according to the WHO, the observing spread of multi-resistant bacteria in Germany signifies the entrance in the post-antibiotic era, a period in which many infections are hardly or incurable like hundred years ago.
On the one hand infections with multi-resistant bacteria strain the patients. Otherwise they menace Germany as location of health and carry a financial risk for providers, in particular hospitals. In consequence of generalized billing with insurance companies and the currently insufficiently differentiated coding as well as the calculation of flat-rates, the financial deficit remains partially with the hospital.
A monitoring of nosocomial infections with multi-resistant bacteria by use of routine data of statutory health insurance bases on diagnostic documentation and documentation of realized operations or procedures. The systematic recording of infections with multi-resistant bacteria is hampered by incomplete documentation in the hospitals. This can't only be justified with the apprehension of stigmatization but is also the result of economic incentives in the DRG system. The recognition of ICD-diagnosis and OPS-numbers with a reference to multi-resistant bacteria could be abstained because of disincentive effects.
Method
In April 2011, the Scientific Institute of the Techniker Krankenkasse (WINEG) analyzed inpatient numbers of cases to quantify not documented infections with multi-resistant pathogens. On the basis of data supplied by the Charité, the expected (primary data) prevalence of infections with multi-resistant pathogens was projected onto all insured people of the Techniker Krankenkasse (TK) and was compared with the by OPS-Codes registered (secondary data) prevalence of 7.8 million TK-insured.
Results
Quantification of not documented infections
The preliminary result of the TK-routine-data review shows that, dependent from methodology, up to two thirds of expected inpatient cases of multi-resistant pathogens aren't documented. Hospital doctors confirm that the incompleteness of hospital documentation refers first of all to the appeal of optimizing profits in the existing DRG-system [2].
Routine data of health insurances from the residential sector are also billing data for relevant institutions. In general, it must be assumed that the documentations are always incomplete whereas diagnoses of hospital discharge are considered as comparatively reliable. The example of multi-resistant bacteria demonstrates that completeness of ICD- and OPS-codes in the residential sector must not be axiomatic implied. A quantification of incorrect documentations enables the calculation of an adequate correction factor.
If the exclusion of disincentive effects succeeds by virtue of advancement of the DRG-system, the suitability of routine data for incidence determination of nosocomial infections as quality indicator is still to verify – not least within the framework of selective contracts.
First cost analysis
In literature, some cost analysis are already to be found which were all compiled from the hospitals' point of view and reveal that a hospital has a deficit of around 6,000 € for the treatment of an infection by multi-resistant pathogens.
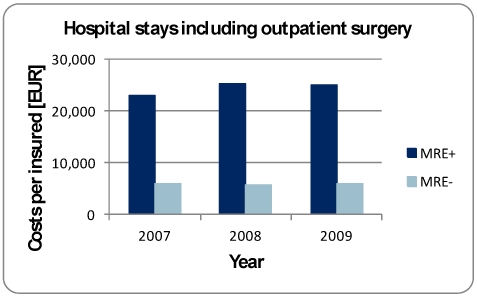
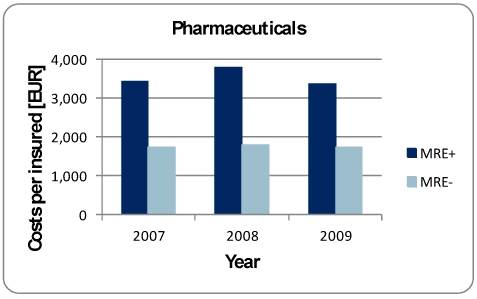
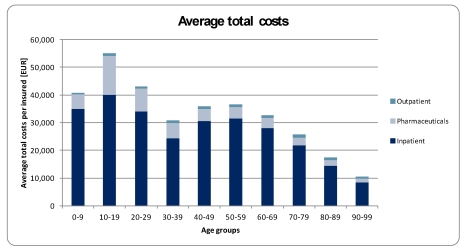
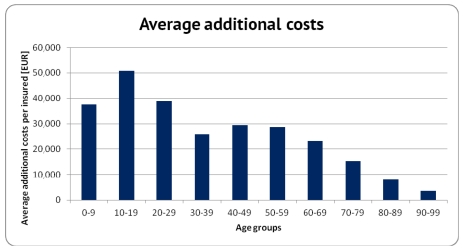
Health insurances are able to assess courses of treatment and costs cross-sectoral. In the direct cost comparison of inpatient stays of similar TK-insured regarding age, gender and basic-DRG with and without multi-resistant pathogens, it is recognizable that a total of 20,525 € additional charges accrue per insured person. These additional costs emerge primarily in the hospital (Figure 1 (Fig. 1)) but also the medication order occasions additional costs of 1,600 € per insured (Figure 2 (Fig. 2)). Further analysis is planned making the severity of comorbidities in both groups with and without multiresistant pathogens even more comparable to prevent possible overestimation of additional costs.
Figure 1. Costs of hospital stays including outpatient surgery per insured with (MRE+) and without (MRE-) infections induced by multi-resistant bacteria 2007–2009.
Figure 2. Costs of pharmaceuticals per insured with (MRE+) and without (MRE-) infections induced by multi-resistant bacteria 2007–2009.
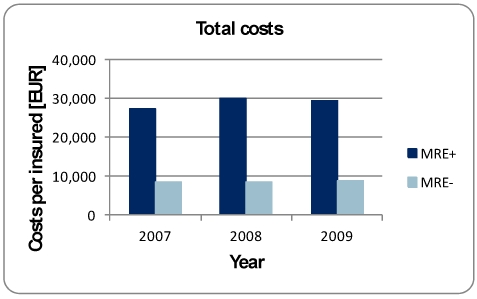
It becomes apparent that there is no obvious increase of additional costs over time (Figure 3 (Fig. 3)). Allowing for prevalence rise and TK-insured growth, a huge increase of annual additional costs can be ascertained all in all. There is a need of reflection about which categories of insured persons are generally affected by multi-resistant pathogens and how far these patients correspond to the clientele of the TK. By far, the highest costs induced by multi-resistant pathogens are caused by insured of lower age groups (0 to 30 years) (Figure 4 (Fig. 4) and Figure 5 (Fig. 5)). This ascertainment contrasts with comparable insured where a higher age also correlates with higher costs. The percentage of TK-insured persons under 30 years of more than 35 percent is above the German average of 31.8 percent [3]. Furthermore, multi-resistant bacteria as a high cost factor will be of great significance for the TK.
Figure 3. Total costs per insured with (MRE+) and without (MRE-) infections induced by multi-resistant bacteria 2007–2009.
Figure 4. Average total costs per insured with infections induced by multi-resistant bacteria 2007–2009.
Figure 5. Average additional costs per insured with infections induced by multi-resistant bacteria 2007–2009.
Discussion
New documentation possibilities are necessary
To ensure transparency about multi-resistant pathogens in the medical processes, distinguishing features regarding source of infection, gates and infection routes are required. These characteristics are the basis for a quality-assured medical care. Adaptations in the ICD and OPS catalog by the German Institute of Medical Documentation and Information (DIMDI) are necessary. Suggestions for a differentiated coding have already been received, especially referring to the problem about the impossibility of a sufficient differentiated coding of multi-resistant pathogens in the valid ICD-10 catalog. An encoding about the acquisition of multi-resistant pathogens before hospital stay or during inpatient service doesn't exist yet.
The Initiative of Quality Medicine (IQM) already proposed the admission of a separate code for MRSA in February 2011 to make the pathogen codeable as well as to arrange a clear separation of the acquisition before or during the current hospital stay. Documentations on this basis enable the Institute for Hospital Reimbursement System (InEK) which is responsible for advancement of the DRG-system to project multi-resistant bacteria more differentially in the DRG-system. This is ultimately the only way to create conditions for higher reimbursement for better care quality.
Legal reforms
According to the Federal Ministry of Health, the problem of the high infection and resistance rates is not the lack of recommendations but rather the insufficient implementation of applicable and published guidelines. The law amending the Law of Infection Protection (IfSG) passed in July 2011 should lay the foundations to improve the quality of hospital hygiene. The reduction of infections with multi-resistant pathogens is strongly emphasized. This applies both to guidelines on an appropriate antibiotics therapy and prevention by the commission antiinfectives, resistance and therapy (ART) and on infection control in general by the commission of hospital hygiene and infection prevention, both resident at the RKI.
Moreover, record keeping requirements for nosocomial infections and resistant pathogens exist from now. A standardized exchange of recording information between medical institutions and the RKI isn't provided. The compliance of hygiene standards in medical and dental practices is considered in § 23(5) IfSG, however not obligatory at federal level. State governments can define specific measures of infection hygiene in practices.
Until 31 March 2012, the state governments commit to enact executive order laws for the compliance of infection hygiene in institutions of health care. The legislator puts provisions to be taken in concrete terms in the framework of a ten-point catalog. Established physicians are more involved in the flow of information by means of point ten of § 23(8), thereby taking the principle “search and follow” more into account. According to that, the care should be effective and cross-sectoral along the whole “MRSA supply chain” [4].
The law also provides to include the measured hygiene quality of hospitals in their quality reports prospectively to increase transparency and competition. The reimbursement system has to set incentives for providers to behave responsibly towards the identification of multi-resistant pathogens, measures for treatment and for the protection of infected patients.
New health care approaches of the TK: the project HICARE
“Visions need fantasy”, is the title of Heinz Lohmann's publication about innovative projects in the health care sector [5]. The vision of the project HICARE (Health, Innovative Care and Regional Economy) is the effective encounter of medical pathogens. The action alliance against multi-resistant pathogens unifies in addition to the TK also a variety further partner like BioCon Valley. In this regional, on the German Baltic coast focused project effective, standardized and transferable intervention strategies should be developed, attempted and prepared for the standard care. The project idea was chosen as one of five winners in the contest “Health Regions in the Future” from the Federal Ministry of Education and Research (BMBF).
The aspiration is to organize the health region Baltic coast in such a way that it can serve as model region for the whole of Germany related to the successful containment of the spread of multi-resistant pathogens. The project should foster the development in health industry of Mecklenburg-Pomerania successively. In general, the positive development of the health industry is dependent from the mobilization of private and public resources. Important circumstances were created by project funding recently. Start-up funding in the context of integrated medical care was a catalyst for such project foundations.
Conclusion
In the fight against “hospital germs” health insurances are potential partners. From a competitive point of view, considering mostly simplified health insurance contributions, insurances should seize the opportunity to cope with competition by the supply of high-quality services. Infection prevention and protection in the medical care can entail a competitive advantage. Necessary condition for comparability of service offerings of individual health insurances is transparency of quality.
What concerns primarily in the future are common solutions for patients between health service providers and industry, in other words to consider fighting the pathogens as a collective concept. The integrated medical care offers a platform for committed partners in the health care system.
Notes
Competing interests
The authors declare that they have no competing interests.
References
- 1.Gastmeier P, Geffers C. Nosokomiale Infektionen in Deutschland: Wie viele gibt es wirklich? Eine Schätzung für das Jahr 2006. Dtsch med Wochenschr. 2008;133(21):1111–1115. doi: 10.1055/s-2008-1077224. Available from: http://dx.doi.org/10.1055/s-2008-1077224. [DOI] [PubMed] [Google Scholar]
- 2.Linder R, Horenkamp-Sonntag D, Pfenning I, Verheyen F. Quantifizierung stationärer Patientenfallzahlen mit nicht-dokumentierter Infektion multiresistenter Erreger. AGENS Methoden Workshop; Köln, 14.-15.04.2011; Hamburg: Wissenschaftliches Institut der TK für Nutzen und Effizienz im Gesundheitswesen; 2011. Available from: http://www.tk.de/centaurus/servlet/contentblob/339556/Datei/6664/Nicht-Dokumentation-MRE-Infektionen.pdf. [Google Scholar]
- 3.Bundeszentrale für politische Bildung. Bevölkerungsgruppen nach Altersgruppen und Geschlecht. Altersgruppen in absoluten Zahlen, Anteile der Geschlechter in Prozent. 2009. [Google Scholar]
- 4.Friedrich AW. EUREGIO MRSA-net Twente/Münsterland: „search & follow“ by Euregional network building. Gesundheitswesen. 2009;71(11):766–770. doi: 10.1055/s-0029-1241892. Available from: http://dx.doi.org/10.1055/s-0029-1241892. [DOI] [PubMed] [Google Scholar]
- 5.Lohmann H. Visionen brauchen Fantasie. Stuttgart: Thieme; 2009. [Google Scholar]