Abstract
Dermatitis of hands is a problem among nurses. The aim of this prospective questionnaire based survey was to analyze practice and knowledge of skin care of medical and surgical nurses.
250 questionnaires were distributed. 49% of respondent stated that they perform skin care at least 1–2 times/day. After hand-wash 15% of participants perform skin protection, after hand-disinfection only 2%. 40% give skin care products less than 3 minutes to be applied.
It was shown that this knowledge is lacking in many individuals, leading to wrong behavior at work and insufficient use of skin protection and skin care products.
Keywords: skin care, skin protection, intensive care nurses
Abstract
Die sog. Abnutzungsdermatose ist ein Problem bei Pflegekräften. Mit Hilfe einer prospektiven Fragebogenerhebung sollten das Wissen zum Hautschutz und zur Hautpflege und die praktische Umsetzung bei in der Intensivpflege tätigen internistischen und chirurgischen Pflegekräften analysiert werden.
Es wurden 250 Fragebögen verteilt. 49% der Antwortenden gaben an, Hautpflege mindestens 1–2 mal täglich durchzuführen. 40% der Befragten gingen davon aus, dass die Dauer zum Einziehen von Hautcreme weniger als 3 min beträgt.
Es wurden deutliche Wissensdefizite zur richtigen Anwendung von Hautschutz- und Hautpflegepräparaten offenkundig.
Background
Dermatitis of hands is a common and serious problem among nurses with reported prevalence ranging between 18 and 86% [1], [2], [3], [4], [5], [6]. The condition mostly is related to wet work, hand washing and wearing of gloves [3], [7]. During professional training prevalence of hand dermatitis increased from 7% in the first year to 23% in the fourth year among Korean nursing students [8]. Similar results were found in Australia among nursing students [9].
Development and prevention of dermatitis are dependent on the knowledge of healthcare workers on dangers of skin damage and possibilities of skin care [10]. Although the relevance and great effectiveness of target orientated teaching campaigns is of no doubt [11], also regular use of hand creams can reduce the risk for dermatitis by almost 50% [9], [12]. Despite this encouraging result, the advantage of barrier creams compared to bland emollients for skin protection is not clearly demonstrated and only scant literature exists on this issue [12], [13], [14], [15], [16], [17].
The aim of this prospective questionnaire based survey was to analyze the practice of skin protection and skin care of nurses in surgical and internal wards, their integration and differentiation of both measures within hand hygiene and the inquiry of motivation for skin care.
Material and methods
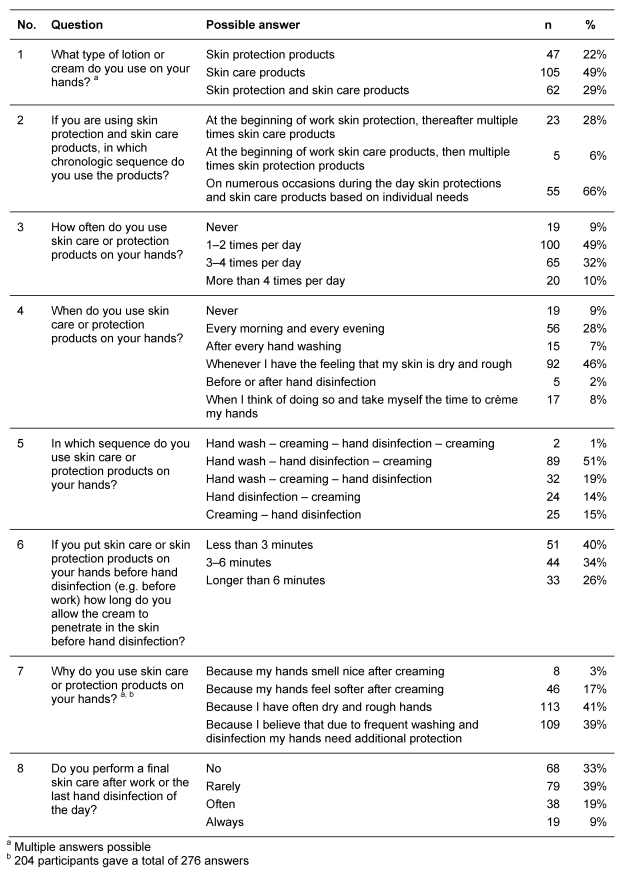
The study was conducted at the medical, surgical, medical intensive and surgical intensive care units of a 950-bedded tertiary care university teaching hospital in Germany. An 8-item multiple-choice questionnaire was developed. It included demographic questions (age, gender, type of medical setting) and structured questions on skin care and motivation for this procedure (Table 1 (Tab. 1)). A total of 250 questionnaires were distributed among nursing staff.
Table 1. Structured questions of the 8-item multiple choice questionnaire together with responses.
Skin protection products were defined as products used before the contact to irritating substances, skin care products were defined as products used to support skin recovery.
For statistical analysis, categorical (discrete) variables were expressed as numbers (percentages) and compared using chi-square test or by Fisher’s exact test, respectively. All tests of significance were 2-tailed; P values of ≤.05 were considered significant.
Results
A total of 204/205 (81.2%) questionnaires were correctly filled out and returned. 179 (87.7%) of the respondents were female, and 25 (12.3%) male. 69 participants (33.8%) were between 20–29 years, 64 (31.3%) between 30–39 years, 47 (23.0%) between 40–49 years, 20 (9.8%) between 50–59 years, and 3 older than 60 years. Significantly more respondents from surgical wards (n=137; 67.1%) submitted the questionnaire than participants from medical wards (n=67; 32.9%), P<0.001. 68 questionnaires (33.3%) were obtained from surgical wards, 69 (33.8%) from surgical intensive units, 37 (18.2%) from medical wards, and 30 (14.7%) from medical intensive units. There was, however, no difference between participants from normal wards (n=105; 51.5%) and intensive care units (n=99; 48.5%), P=0.552.
100/204 (49%) respondent stated that they perform skin care at least 1–2 times per day. 9% (n=19) never apply skin care to their hands (Table 1 (Tab. 1)). Almost 1/3 of healthcare workers use a combination of these products.
204 respondents gave a total of 276 answers to the question why they crème their hands. Almost 20% of respondents’ consider protective effects of skin care as the main objective for their action. 39% state that hands of healthcare workers are at risk of damage and therefore need additional care. 41% justify skin care because of dry and rough hands.
At the beginning of daily work, 28% of respondents perform skin care and protection. After hand washing 15% perform skin protection, while after hand disinfection only 2%. The main reason for using skin care or skin protection products was the feeling of dry and rough skin. Less than half of participants gave any answer to performance of skin care and skin protection at beginning of the working day and during the day. Of those, only 28% applied skin protection products. At the end of work, 1/3 did not use any product. Less than 10% always applied a skin care product before they work ends.
172 answered the question on the sequence of hand hygiene and hand protection measures. 65% practiced the sequence “hand washing – hand disinfection – using skin care products”. All others use skin care products before hand disinfection (35%). 40% of 128 respondents gave skin care products less than 3 minutes to be applied; almost 1/3 gave 3–6 minutes, and 1/4 more than 6 minutes time.
Discussion
Because the survey was anonymous, biased answers were minimized. This was confirmed by the fact that responses to different but similar questions were correct. When asked “How often do you cream your hands” (question no. 3) 9% stated that they never do. Consequently, also 9% responded they never cream their hands when asked about the timing (question no. 4). Our results indicate shortcomings to both, motivation for skin protection and skin care as well as on practical implementation. The finding of almost 10% of healthcare workers never using products for hand protection and care is alarming. Also, the frequency of 49% for hand care 1–2 times/day can not be considered sufficient.
Different reasons were stated for the application of skin care or skin protection products. The main reason was subjective feeling of dry and rough hands, which is plausible. This however, is not sufficient to achieve relevant skin protection, as almost 20% of respondents did not state that protection of their skin is the main objective. Only 51% of the participants used a skin protection product, and only 28% did so at the beginning of work. The others used only skin care emollients.
One main reason for the high prevalence of occupational hand dermatitis is primarily the lack of knowledge. This includes knowledge on risk factors but also being able to identify early signs of dermatitis. Many light to moderate initial changes of the skin condition like dryness or discrete interdigitale eczema are often not taken seriously or are overlooked due to lack of knowledge [18]. If the nursing staff recognized that eczematous skin condition of the hands are linked to their clinical work, then often it is not unusual to blame alcohol based hand disinfectants as the triggering factor. Several studies, however, show clearly that alcohol based hand disinfectants are changing the physiological condition of the skin only in a minute fraction, yet by hand washing using detergents the skin condition is changed significantly [19], [20], [21], [22]. Since in most hands disinfectants also include emollients, they additionally prevent drying and skin irritation simultaneously.
In addition to the importance of knowledge of the etiology of dermatitis [23], [24], implementing measures to allow staff a correct skin protection and care during their clinical routine work is of great importance and must not be neglected [23]. Aside of including skin care and skin protection into hand hygiene standard operating procedures (SOPs), provision of an informative leaflet might be supporting this task. The main contents of such a leaflet could be information on the risk factors and the resulting consequences of dermatitis in healthcare settings.
In summary, this study has shown that knowledge on healthcare related dermatitis is lacking at many individuals, possibly leading to wrong behavior at work and insufficient use of skin protection and skin care products. Regular teaching and better information might decrease the prevalence of dermatitis in nurses.
Notes
Conflicts of interest
The authors declare that they have no competing interests.
References
- 1.Larson E, Friedman C, Cohran J, Treston-Aurand J, Green S. Prevalence and correlates of skin damage on the hands of nurses. Heart Lung. 1997;26(5):404–412. doi: 10.1016/S0147-9563(97)90027-3. Available from: http://dx.doi.org/10.1016/S0147-9563(97)90027-3. [DOI] [PubMed] [Google Scholar]
- 2.Smit HA, Coenraads PJ, Lavrijsen AP, Nater JP. Evaluation of a self-administered questionnaire on hand dermatitis. Contact Dermatitis. 1992;26(1):11–16. doi: 10.1111/j.1600-0536.1992.tb00861.x. Available from: http://dx.doi.org/10.1111/j.1600-0536.1992.tb00861.x. [DOI] [PubMed] [Google Scholar]
- 3.Szepietowski JC, Salomon J. Hand dermatitis among nurses: the reasons and consequencies. Contact Dermatitis. 2006;54(2):129–130. doi: 10.1111/j.0105-1873.2006.00568.x. Available from: http://dx.doi.org/10.1111/j.0105-1873.2006.00568.x. [DOI] [PubMed] [Google Scholar]
- 4.Lampel HP, Patel N, Boyse K, O'Brien SH, Zirwas MJ. Prevalence of hand dermatitis in inpatient nurses at a United States hospital. Dermatitis. 2007;18(3):140–142. doi: 10.2310/6620.2007.06024. Available from: http://dx.doi.org/10.2310/6620.2007.06024. [DOI] [PubMed] [Google Scholar]
- 5.Schürer NY, Klippel U, Schwanitz HJ. Secondary individual prevention of hand dermatitis in geriatric nurses. Int Arch Occup Environ Health. 2005;78(2):149–157. doi: 10.1007/s00420-004-0588-0. Available from: http://dx.doi.org/10.1007/s00420-004-0588-0. [DOI] [PubMed] [Google Scholar]
- 6.Stingeni L, Lapomarda V, Lisi P. Occupational hand dermatitis in hospital environments. Contact Dermatitis. 1995;33(3):172–176. doi: 10.1111/j.1600-0536.1995.tb00540.x. Available from: http://dx.doi.org/10.1111/j.1600-0536.1995.tb00540.x. [DOI] [PubMed] [Google Scholar]
- 7.Löffler H, Effendy I, Happle R. Die irritative Kontaktdermatitis. [Irritant contact dermatitis]. Hautarzt. 2000;51(3):203–215. doi: 10.1007/s001050051023. (Ger). Available from: http://dx.doi.org/10.1007/s001050051023. [DOI] [PubMed] [Google Scholar]
- 8.Smith DR, Choe MA, Jeong JS, An GJ, Chae YR, Jeon MY. Hand dermatitis among Korean nursing students. Int J Nurs Pract. 2006;12(3):160–165. doi: 10.1111/j.1440-172X.2006.00564.x. Available from: http://dx.doi.org/10.1111/j.1440-172X.2006.00564.x. [DOI] [PubMed] [Google Scholar]
- 9.Smith DR, Leggat PA. Hand dermatitis among female nursing students in tropical Australia. Nurs Health Sci. 2004;6(2):109–113. doi: 10.1111/j.1442-2018.2004.00181.x. Available from: http://dx.doi.org/10.1111/j.1442-2018.2004.00181.x. [DOI] [PubMed] [Google Scholar]
- 10.Löffler H, Effendy I. Prevention of irritant contact dermatitis. Eur J Dermatol. 2002;12(1):4–9. [PubMed] [Google Scholar]
- 11.Löffler H, Bruckner T, Diepgen T, Effendy I. Primary prevention in health care employees: a prospective intervention study with a 3-year training period. Contact Dermatitis. 2006;54(4):202–209. doi: 10.1111/j.0105-1873.2006.00825.x. Available from: http://dx.doi.org/10.1111/j.0105-1873.2006.00825.x. [DOI] [PubMed] [Google Scholar]
- 12.Berndt U, Wigger-Alberti W, Gabard B, Elsner P. Efficacy of a barrier cream and its vehicle as protective measures against occupational irritant contact dermatitis. Contact Dermatitis. 2000;42(2):77–80. doi: 10.1034/j.1600-0536.2000.042002077.x. Available from: http://dx.doi.org/10.1034/j.1600-0536.2000.042002077.x. [DOI] [PubMed] [Google Scholar]
- 13.Cormick RD, Buchman TL, Maki DG. Double-blind, randomized trial of scheduled use of a novel barrier cream and an oil-containing lotion for protecting the hands of health care workers. Am J Infect Control. 2000;28(4):302–310. doi: 10.1067/mic.2000.107425. Available from: http://dx.doi.org/10.1067/mic.2000.107425. [DOI] [PubMed] [Google Scholar]
- 14.Lewis-Byers K, Thayer D. An evaluation of two incontinence skin care protocols in a long-term care setting. Ostomy Wound Manage. 2002;48(12):44–51. [PubMed] [Google Scholar]
- 15.zur Mühlen A, Klotz A, Allef P, Weimans S, Veeger M, Thörner B, Eichler JO. Using skin models to assess the effects of a pre-work cream. Methodological aspects and perspective of the industry. Curr Probl Dermatol. 2007;34:19–32. doi: 10.1159/000099601. Available from: http://dx.doi.org/10.1159/000099601. [DOI] [PubMed] [Google Scholar]
- 16.Teichmann A, Jacobi U, Waibler E, Sterry W, Lademann J. An in vivo model to evaluate the efficacy of barrier creams on the level of skin penetration of chemicals. Contact Dermatitis. 2006;54(1):5–13. doi: 10.1111/j.0105-1873.2006.00749.x. Available from: http://dx.doi.org/10.1111/j.0105-1873.2006.00749.x. [DOI] [PubMed] [Google Scholar]
- 17.Zhai H, Maibach HI. Barrier creams – skin protectants: can you protect skin? J Cosmet Dermatol. 2002;1(1):20–23. [PubMed] [Google Scholar]
- 18.Schwanitz HJ, Uter W. Interdigital dermatitis: sentinel skin damage in hairdressers. Br J Dermatol. 2000;142(5):1011–1012. doi: 10.1046/j.1365-2133.2000.03487.x. Available from: http://dx.doi.org/10.1046/j.1365-2133.2000.03487.x. [DOI] [PubMed] [Google Scholar]
- 19.Löffler H, Kampf G, Schmermund D, Maibach HI. How irritant is alcohol? Br J Dermatol. 2007;157(1):74–81. doi: 10.1111/j.1365-2133.2007.07944.x. Available from: http://dx.doi.org/10.1111/j.1365-2133.2007.07944.x. [DOI] [PubMed] [Google Scholar]
- 20.Slotosch CM, Kampf G, Löffler H. Effects of disinfectants and detergents on skin irritation. Contact Dermatitis. 2007;57(4):235–241. doi: 10.1111/j.1600-0536.2007.01200.x. Available from: http://dx.doi.org/10.1111/j.1600-0536.2007.01200.x. [DOI] [PubMed] [Google Scholar]
- 21.Pedersen LK, Held E, Johansen JD, Agner T. Short-term effects of alcohol-based disinfectant and detergent on skin irritation. Contact Dermatitis. 2005;52(2):82–87. doi: 10.1111/j.0105-1873.2005.00504.x. Available from: http://dx.doi.org/10.1111/j.0105-1873.2005.00504.x. [DOI] [PubMed] [Google Scholar]
- 22.Pedersen LK, Held E, Johansen JD, Agner T. Less skin irritation from alcohol-based disinfectant than from detergent used for hand disinfection. Br J Dermatol. 2005;153(6):1142–1146. doi: 10.1111/j.1365-2133.2005.06875.x. Available from: http://dx.doi.org/10.1111/j.1365-2133.2005.06875.x. [DOI] [PubMed] [Google Scholar]
- 23.Löffler H, Dickel H, Bruckner T, Effendy I, Happle R. Skin changes in geriatric nurses prior to training heralding a particular risk of hand dermatitis. Eur J Dermatol. 2002;12(5):452–454. [PubMed] [Google Scholar]
- 24.Weisshaar E, Radulescu M, Bock M, Albrecht U, Zimmermann E, Diepgen TL. Hautschutzseminare zur sekundaren Individual- prävention bei Beschäftigten in Gesundheitsberufen: erste Ergebnisse nach über 2-jahriger Durchführung. [Skin protection and skin disease prevention courses for secondary prevention in health care workers: first results after two years of implementation]. J Dtsch Dermatol Ges. 2005;3(1):33–38. doi: 10.1046/j.1439-0353.2005.04798.x. (Ger). Available from: http://dx.doi.org/10.1046/j.1439-0353.2005.04798.x. [DOI] [PubMed] [Google Scholar]
- 25.Hübner NO, Große-Schütte K, Assadian O, Löffler H, Kramer A. The effects of skin protection cream on the effectiveness of hygienic hand disinfection and the implications for practicing hand disinfection. BMC Inf Dis. (submitted) [Google Scholar]