Abstract
Within the first two years after total hip arthroplasty implant-associated infection has become the second most common reason for a revision surgery. Two-stage implant exchange is frequently conducted using temporary spacers made of antibiotic-loaded cement in order to prevent a bacterial colonization on the spacer. Avoiding several disadvantages of cement spacers, a conventional hemi-endoprosthesis was equipped with a copper-containing implant coating for inhibition of bacterial biofilms. In the present paper details of this novel treatment concept are presented including a case report.
Keywords: total hip arthroplasty, infection, spacer, titanium-copper-nitride coating
Abstract
Innerhalb der ersten beiden Jahre nach endoprothetischem Hüftgelenkersatz stellt die implantat-assoziierte Infektion mittlerweile den zweithäufigsten Grund für eine Revisionsoperation dar. Beim zweizeitigen septischen Wechsel werden temporäre Platzhalter (Spacer) aus antibiotikahaltigem Zement zur Therapie und Vermeidung einer bakteriellen Besiedlung verwendet. Mit dem Ziel, bekannte Nachteile von Zementspacern zu umgehen, wurde eine Biofilm-inhibierende kupferhaltige Beschichtung auf eine konventionelle Hemi-Endoprothese aufgebracht. Im Folgenden soll das Design dieses neuartigen Therapieansatzes im Rahmen eines Fallberichts vorgestellt werden.
Introduction
Due to the increasing number of primary joint arthroplasties as well as revision surgeries, implant-associated infections gain in medical and economic importance [1], [2]. Multimorbidity and multiple previous revisions of the total joint replacement are major risk factors for infections. After insertion of an endoprosthetic implant the human cells and microorganisms compete for the colonization of the implant surface, which is called “race for the surface” [3]. That process is a crucial point particularly for temporary spacer implants within two-stage total hip revisions in terms of septic implant loosening. Spacers consisting of bone cement can be hand-made by the surgeon with or without using casting moulds and metallic endoskeletons. As an alternative, preformed cement spacers are commercially available. Depending on the specific chemical composition, antibiotic loading and the geometry respectively surface of the applied bone cement (e.g. monobloc spacer, beads) the release of the antibiotics is highly variable. Hence, some authors report on antimicrobial effective concentrations of antibiotics even six weeks after cement spacer implantation [4], the majority of the studies showed a significant decrease of the release of antibiotics already after a few days [5], [6]. As a consequence, the cement spacer itself may be colonized by residual bacteria. The portion of antibiotics in bone cement is limited, since it impairs the mechanical properties of spacers as well as of the cement mantle around endoprostheses [7], [8]. The development of a metallic spacer with titanium-copper-nitride (TiCuN) coating should combine the superior mechanical stability of a total hip stem with a biofilm-inhibiting implant surface.
Method
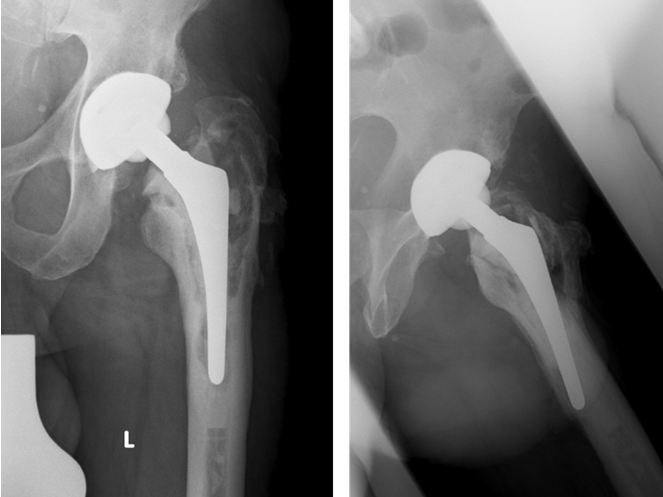
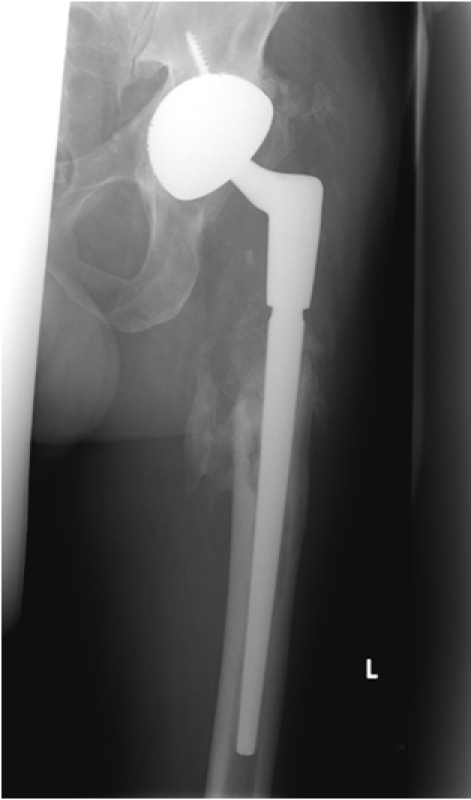
Metallic spacers coated with TiCuN are used in patients with proven late periprosthetic infection according to international criteria [9], [10] as temporary implants within a two-stage revision concept. The total spacer interval is eight weeks. Tissue samples for a microbiological and histological examination are obtained before explantation of the infected total hip endoprosthesis, during implant removal, two weeks before reimplantation and within the reimplantation. The spacers are commercially available metallic hip stems and jumbo heads of different sizes and lengths (Figure 1 (Fig. 1)) with a polished surface which is coated by physical vapor deposition (PVD, DOT Coating, Rostock, Germany). The TiCuN coating is firmly connected to the implant surface [11]. Titanium and copper are released from a target by electricity, ionized and deposited on the implant surface. That process leads to the formation of a face-centered cubic grid of titanium atoms with nitrogen ions embedded in the gaps. The TiCuN coating solely modifies the implant surface but leaves the mechanical properties of the implant unchanged [11]. From the biological point of view, copper combines high antimicrobial respectively biofilm-inhibiting effectiveness with relatively little toxicity for human tissue when compared to other metal ions [12], [13]. The TiCuN spacers are inserted after removal of the infected soft tissue and bone as well as the total hip endoprosthesis. In most cases the spacer can be implanted without additional cement fixation. If additional rotational or axial stabilization is required, a cement augmentation of the proximal implant part is performed (Figure 2 (Fig. 2)). Within the routine laboratory examination of the first and 14th postoperative day as well as after six weeks, the serum copper level is monitored. Six weeks after spacer implantation tissue samples from the affected hip joint are taken for a microbiological and histological examination by a mini-incision biopsy. In case of missing clinical, microbiological and histological signs of persistent infection, the reimplantation is performed after another two weeks. So far, the application was limited to selected patients. The clinical course of one patient is reported below.
Figure 1. TiCuN coated (DOT GmbH, Rostock, Germany) hip stem and jumbo head for a hemiarthroplasty.

Figure 2. TiCuN-coated spacer implant. Additional cement augmentation (at the femoral diaphysis) for improved rotational and axial stability after resection of the proximal femur.

Admission situation (3/2010)
67-year-old male patient with clinical signs of a loosening of his left total hip replacement (THR).
Medical history
Primary THR 4/2004 (alio loco) because of hip dysplasia (Implants: thrust plate prosthesis (TPP), press-fit acetabular cup),
since 6/2004: groin pain during walking and stair-climbing,
9/2004: Loosening of the TPP. One-stage revision with removal of the TPP, implantation of a cemented hip stem, exchange of the polyethylene liner, leaving of the well-fixed acetabular shell. Histology: capsule with massive metallosis, no signs of an infection. Microbiology: no growth of bacteria after 14 days incubation.
10/2004–2/2010: good clinical function of the THR,
3/2010: Outpatient presentation reporting groin and thigh pain during walking for three weeks. Clinical findings: Scar and skin without irritation, no systemic signs of an infection. Thigh pain during compression. Radiological findings: extended osteolyses around the hip stem, breakage of the cement mantle (Figure 3 (Fig. 3)). Tissue samples were obtained (same-day surgery). Histology: scar tissue and neocapsule, no sign of an infection. Microbiology: Staphylococcus capitis (only fosfomycine resistance). Laboratory: chronic infection-associated anaemia, elevated infection parameters (Hb 5.6 mmol/l; WBC 13.1/nl; CRP 50.2 mg/l; BSR 17 mm/1 h).
Figure 3. Chronically septic loosening of a cemented hip stem with extended osteolyses, breakage of the cement mantle and migration of the total hip stem.
Diagnosis
Based on the findings, the diagnosis of late implant-associated infection caused by S. capitis after aseptic total hip revision was made.
Additional diagnoses
Arterial hypertension, smoking (40 py), chronic peptic esophagitis, sigmoid diverticulitis (conservative treatment in 2006), cataract operation on both eyes in 2005. Risk classification (anaesthesia): ASA 2.
Results
Course of treatment
4/2010: Explantation of the THR including a complete removal of cement, infected tissue and the proximal femoral bone. Implantation of a TiCuN coated hip stem as a temporary spacer (stem length 200 mm). A TiCuN coated jumbo head was used to complete the hemiarthroplasty (Figure 2 (Fig. 2)). Microbiology: Staphylococcus capitis (identical with preoperative biopsy)
Antibiotic treatment for four weeks (cefuroxim/moxifloxacin, two weeks i.v. and two weeks p.o.)
Postoperative serum copper levels: day 1: 18.4 µmol/l, day 14: 21.4 µmol/l and week 6: 19.1 µmol/l. Copper levels were within physiological range [11.0–23.5 µmol/l].
Outpatient mini-incision biopsy six weeks after explantation: Histology/microbiology: no signs of a persisting infection. Laboratory: no signs of an infection (Hb 8.3 mmol/l; WBC 7.4/nl; CRP <1.00 mg/l; BSR 6 mm/1 h)
6/2010: Cementless revision THR (Acetabular component: Metallsockel 2000, Orthodynamics, Luebeck, Germany; Femoral component: Restoration Modular Stryker, Mahwah, NJ, USA). Microbiology: Five tissue samples and PCR/culture of the spacer sonication fluid without detection of microorganisms
7/2011: Clinical and radiological follow-up one year after reimplantation: no clinical or laboratory signs of a relapse of the periprosthetic infection. The X-rays (Figure 4 (Fig. 4)) show moderate ossifications of the soft tissue around the femoral diaphysis without clinical relevance. No signs of implant-loosening or migration.
Figure 4. Cementless total hip revision implant: radiological follow-up 1 year after implantation.
Discussion
The temporary insertion of cement spacers is a widely accepted procedure in two-stage septic arthroplasty revision to avoid soft-tissue contractures, to apply antibiotics locally and to facilitate the reimplantation [14]. The addition of antibiotics to bone cement is also practiced in conjunction with one-stage septic revisions when a cemented implant is used and the bacterial antibiogram is known [15]. Additional mixing of antibiotics into bone cement intraoperatively reduces the mechanical resilience of the cement [7], [8] which may lead to breakage of the spacer [16] or cement mantle around endoprostheses. Moreover, manual addition of antibiotics leads to a more varying agent release and the mixing as well as the polymerization may partially deactivate the antibiotics [17], [18]. Cement spacers made with casting moulds and metallic endoskeletons provide a better mechanical stability [19]. But any type of cement spacer may become colonized by bacteria [20] when the antibiotic elution comes below the antimicrobial effective concentration [5], [6]. The release of zirconium oxide particles from bone cement is a further disadvantage that received only little attention so far. Zirconium oxide particles are suspected to increase the wear rate of the following revision endoprosthesis [21] caused by ceramic third body particles and hence to result in osteolyses and implant loosening [22]. In order to avoid these disadvantages of bone cement spacers, several concepts of antiseptic or biofilm-inhibiting coatings were developed for metallic implants. Gollwitzer et al. and Vester et al. tested a biodegradable poly(D,L-lactide) coating for binding antibiotics on metallic surfaces [23], [24]. The clinical application of these PDLLA coatings is still limited due to a rapidly declining release of antibiotics and a poor mechanical stability of the coating [23], [25]. As an alternative to antibiotics, metal ions are also known to show an antimicrobial and biofilm-inhibiting effect. Silver containing coatings on titanium surfaces have been proven to be effective against Staphylococcus aureus and Staphylococcus epidermidis [26], [27]. Gosheger et al. reported significantly less infections in an animal experiment with silver-coated implants compared to titanium-coated implants after inoculation of S. aureus [28]. In the animals silver ion levels were elevated in the blood serum as well as in their organs [28]. Since silver ions are known to be toxic to bacteria and human cells by induction of oxidative stress [29], [30], F. Heidenau and W. Mittelmeier tested various other metal ions concerning their biocompatibility and antimicrobial activity [12]. At the first step, mouse-fibroblasts and S. epidermidis were cultivated on culture media containing metal salts with differing concentrations of Ag+, Zn2+, Co2+, Al3+, Cu2+ and Hg2+. Within a second setup, Ti6Al4V test specimens were sol-gel coated with these metal ions. Finally the colonization of the specimens by MC3T3-E1 cells and S. aureus was analyzed. In summary, compared to the other metal coatings, especially silver, copper showed a high antibacterial effectiveness in relation to its cytotoxicity [12]. Haenle et al. confirmed antibacterial effects of Cu-TiO2 coatings against MRSA [31]. During bending and scratch tests with a single (1x Cu-TiO2) as well as fourfold (4x Cu-TiO2) coating thickness the layer showed a high mechanical stability without cracking or chipping-off [31] which was confirmed in a test series using artificial bones. Moreover, different kinds of copper coatings manufactured with different procedures [11], [32], [33] are currently tested aiming towards future clinical use.
Conclusion
Based on the first experiences, TiCuN-coated implants can be appropriate as temporary spacers for two-stage septic hip revision for selected patients. Concerning further application of those coatings for permanent endoprostheses (e.g. tumour implants) or articulating surfaces (e.g. knee endoprostheses) sufficient data are not available yet.
Notes
Acknowledgement
The authors would like to thank DOT GmbH, Rostock, Germany for technical support as well as the Institut für Medizinische Mikrobiologie, Virologie und Hygiene (Direktor: Prof. Dr. med. Dr. rer. nat. A. Podbielski) and the Institut für Pathologie (Direktor: Prof. Dr. med. A. Erbersdobler) for the microbiological and histological analyses.
Competing interests
The authors declare that they have no competing interests.
References
- 1.BQS-Bundesauswertung 2008 Hüft-Endoprothesen-Erstimplantation. BQS Bundesgeschäftsstelle Qualitätssicherung gGmbH; 2009. pp. 1–65. Available from: http://www.bqs-online.de. [Google Scholar]
- 2.Ong KL, Mowat FS, Chan N, Lau E, Halpern MT, Kurtz SM. Economic burden of revision hip and knee arthroplasty in Medicare enrollees. Clin Orthop Relat Res. 2008;446:22–28. doi: 10.1097/01.blo.0000214439.95268.59. Available from: http://dx.doi.org/10.1097/01.blo.0000214439.95268.59. [DOI] [PubMed] [Google Scholar]
- 3.Gristina AG. Biomaterial-centered infection: microbial adhesion versus tissue integration. Science. 1987;237(4822):1588–1595. doi: 10.1126/science.3629258. Available from: http://dx.doi.org/10.1126/science.3629258. [DOI] [PubMed] [Google Scholar]
- 4.Masri BA, Duncan CP, Beauchamp CP. Long-term elution of antibiotics from bone-cement: an in vivo study using the Prosthesis of Antibiotic-Loaded Acrylic Cement (PROSTALAC) system. J Arthroplasty. 1998;13(3):331–338. doi: 10.1016/S0883-5403(98)90179-6. Available from: http://dx.doi.org/10.1016/S0883-5403(98)90179-6. [DOI] [PubMed] [Google Scholar]
- 5.Anagnostakos K, Wilmes P, Schmitt E, Kelm J. Elution of gentamicin and vancomycin from polymethylmethacrylate beads and hip spacers in vivo. Acta Orthopaedica. 2009;80(2):193–197. doi: 10.3109/17453670902884700. Available from: http://dx.doi.org/10.3109/17453670902884700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moojen DJF, Hentenaar B, Vogely HC, Verbout AJ, Castelein RM, Dhert WJA. In Vitro Release of Antibiotics from Commercial PMMA Beads and Articulating Hip Spacers. J Arthroplasty. 2008;23(8):1152–1156. doi: 10.1016/j.arth.2007.08.020. Available from: http://dx.doi.org/10.1016/j.arth.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 7.Vorndran E, Spohn N, Nies B, Rößler S, Storch S, Gbureck U. Mechanical properties and drug release behaviour of bioactivated PMMA cements. J Biomater Appl. 2010 doi: 10.1177/0885328210376996. Available from: http://dx.doi.org/10.1177/0885328210376996. [DOI] [PubMed] [Google Scholar]
- 8.Lee AJ, Ling RS, Vangala SS. Some clinically relevant variables affecting the mechanical behavior of bone cement. Arch Orthop Surg. 1978;92(1):1–18. doi: 10.1007/BF00381635. Available from: http://dx.doi.org/10.1007/BF00381635. [DOI] [PubMed] [Google Scholar]
- 9.Maurer TB, Ochsner PE. Infekt nach Knietotalprothesenimplantation Zweizeitiger Wechsel als Element des Liestaler Behandlungsalgorithmus. Orthopäde. 2006;35(9):917–928. doi: 10.1007/s00132-006-0978-y. Available from: http://dx.doi.org/10.1007/s00132-006-0978-y. [DOI] [PubMed] [Google Scholar]
- 10.Laffer RR, Graber P, Ochsner PE, Zimmerli W. Outcome of prosthetic knee-associated infection: Evaluation of 40 consecutive episodes of a single centre. Clin Microbiol Infect. 2006;12(5):433–439. doi: 10.1111/j.1469-0691.2006.01378.x. Available from: http://dx.doi.org/10.1111/j.1469-0691.2006.01378.x. [DOI] [PubMed] [Google Scholar]
- 11.Prinz C. Antibakterielle Optimierung von Implantatoberflächen. Rostock: Universität Rostock, Agrar- und Umweltwissenschaftliche Fakultät; 2010. Available from: http://rosdok.uni-rostock.de/file/rosdok_derivate_000000004369/Dissertation_Prinz_2010.pdf. [Google Scholar]
- 12.Heidenau F, Mittelmeier W, Detsch R, Haenle M, Stenzel F, Ziegler G, Gollwitzer H. A novel antibacterial titania coating: metal ion toxicity and in vitro surface colonization. J Mater Sci Mater Med. 2005;16(10):883–888. doi: 10.1007/s10856-005-4422-3. Available from: http://dx.doi.org/10.1007/s10856-005-4422-3. [DOI] [PubMed] [Google Scholar]
- 13.Nie Y, Kalapos C, Nie X, Murphy M, Hussein R, Zhang J. Superhydrophilicity and antibacterial property of a Cu-dotted oxide coating surface. Ann Clin Microbiol Antimicrob. 2010;16(9):25. doi: 10.1186/1476-0711-9-25. Available from: http://dx.doi.org/10.1186/1476-0711-9-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anagnostakos K, Fürst O, Kelm J. Antibiotic-impregnated PMMA hip spacers: Current status. Acta Orthopaedica. 2006;77(4):628–637. doi: 10.1080/17453670610012719. Available from: http://dx.doi.org/10.1080/17453670610012719. [DOI] [PubMed] [Google Scholar]
- 15.Friesecke C, Wodtke J. Management des Protheseninfektes. Chirurg. 2008;79(8):777–792. doi: 10.1007/s00104-008-1570-2. Available from: http://dx.doi.org/10.1007/s00104-008-1570-2. [DOI] [PubMed] [Google Scholar]
- 16.Jung J, Schmid NV, Kelm J, Schmitt E, Anagnostakos K. Complications after spacer implantation in the treatment of hip joint infections. Int J Med Sci. 2009;6(5):265–273. doi: 10.7150/ijms.6.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buchholz HW, Engelbrecht E. Über die Depotwirkung einiger Antibiotika bei Vermischung mit dem Kunstharz Palacos. Chirurg. 1970;41:511–515. [PubMed] [Google Scholar]
- 18.Pattyn C, De Geest T, Ackerman P, Audenaert E. Preformed gentamycin spacers in two-stage revision hip arthroplasty: functional results and complications. Int Orthop. 2011;35(10):1471–1476. doi: 10.1007/s00264-010-1172-8. Available from: http://dx.doi.org/10.1007/s00264-010-1172-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ger E, Dall D, Miles T, Forder A. Bone cement and antibiotics. S Afr Med J. 1977;51(9):276–279. [PubMed] [Google Scholar]
- 20.Bertazzoni Minelli E, Della Bora T, Benini A. Different microbial biofilm formation on polymethylmethacrylate (PMMA) bone cement loaded with gentamicin and vancomycin. Anaerobe. 2011 Apr 16; doi: 10.1016/j.anaerobe.2011.03.013. Available from: http://dx.doi.org/10.1016/j.anaerobe.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Fink B. Revision of late periprosthetic infections of total hip endoprostheses: pros and cons of different concepts. Int J Med Sci. 2009;6(5):287–295. doi: 10.7150/ijms.6.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lochner K, Fritsche A, Jonitz A, Hansmann D, Mueller P, Mueller-Hilke B, Bader R. The potential role of human osteoblasts for periprosthetic osteolysis following exposure to wear particles. Int J Mol Med. 2011;28(6):1055–1063. doi: 10.3892/ijmm.2011.778. Available from: http://dx.doi.org/10.3892/ijmm.2011.778. [DOI] [PubMed] [Google Scholar]
- 23.Gollwitzer H, Ibrahim K, Meyer H, Mittelmeier W, Busch R, Stemberger A. Antibacterial poly(D,L-lactid acid) coating of medical implants using a biodegradable drug delivery technology. J Antimicrob Chemother. 2003;51(3):585–591. doi: 10.1093/jac/dkg105. Available from: http://dx.doi.org/10.1093/jac/dkg105. [DOI] [PubMed] [Google Scholar]
- 24.Vester H, Wildemann B, Schmidmaier G, Stöckle U, Lucke M. Gentamycin delivered from a PDLLA coating of metallic implants: In vivo and in vitro characterisation for local prophylaxis of implant-related osteomyelitis. Injury. 2010;41(10):1053–1059. doi: 10.1016/j.injury.2010.05.010. Available from: http://dx.doi.org/10.1016/j.injury.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 25.Gollwitzer H, Thomas P, Diehl P, Steinhauser E, Summer B, Barnstorf S, Gerdesmeyer L, Mittelmeier W, Stemberger A. Biomechanical and allergological characteristics of a biodegradable poly(D,L-lactid acid) coating for orthopaedic implants. J Orthop Res. 2005;23(4):802–809. doi: 10.1016/j.orthres.2005.02.003. Available from: http://dx.doi.org/10.1016/j.orthres.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 26.Ewald A, Glückermann SK, Thull R, Gburek U. Antimicrobial titanium/silver PVD coatings on titanium. Biomed Eng Online. 2006;24(5):22. doi: 10.1186/1475-925X-5-22. Available from: http://dx.doi.org/10.1186/1475-925X-5-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shimazaki T, Miyamoto H, Ando Y, Noda I, Yonekura Y, Kawano S, Miyazaki M, Mawatari M, Hotokebuchi T. In vivo antibacterial and silver-releasing properties of novel thermal sprayed silver-containing hydroxyapatite coating. J Biomed Mater Res B Appl Biomater. 2010;92(2):386–389. doi: 10.1002/jbm.b.31526. [DOI] [PubMed] [Google Scholar]
- 28.Gosheger G, Hardes J, Ahrens H, Streitburger A, Buerger H, Erren M, Gunsel A, Kemper FH, Winkelmann W, Von Eiff C. Silver-coated megaendoprostheses in a rabbit model – an analysis of the infection rate and toxicological side effects. Biomaterials. 2004;25(24):5547–5556. doi: 10.1016/j.biomaterials.2004.01.008. Available from: http://dx.doi.org/10.1016/j.biomaterials.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 29.Cortese-Krott MM, Münchow M, Pirev E, Hessner F, Bozkurt A, Uciechowski P, Pallua N, Kröncke KD, Suschek CV. Silver ions induce oxidative stress and intracellular zinc release in human skin fibroblasts. Free Radic Biol Med. 2009;47(11):1570–1577. doi: 10.1016/j.freeradbiomed.2009.08.023. Available from: http://dx.doi.org/10.1016/j.freeradbiomed.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 30.Paasche G, Ceschi P, Löbler M, Rösl C, Gomes P, Hahn A, Rohm HW, Sternberg K, Lenarz T, Schmitz KP, Barcikowski S, Stöver T. Effects of metal ions on fibroblasts and spiral ganglion cells. J Neurosci Res. 2011;89(4):611–617. doi: 10.1002/jnr.22569. Available from: http://dx.doi.org/10.1002/jnr.22569. [DOI] [PubMed] [Google Scholar]
- 31.Haenle M, Fritsche A, Zietz C, Bader R, Heidenau F, Mittelmeier W, Gollwitzer H. An extended spectrum bactericidal titanium dioxide (TiO2) coating for metallic implants: in vitro effectiveness against MRSA and mechanical properties. J Mater Sci Mater Med. 2011;22(2):381–387. doi: 10.1007/s10856-010-4204-4. Available from: http://dx.doi.org/10.1007/s10856-010-4204-4. [DOI] [PubMed] [Google Scholar]
- 32.Schröder K, Finke B, Polak M, Lüthen F, Nebe JB, Rychly J, Bader R, Lukowski G, Walschus U, Schlosser M, Ohl A, Weltmann KD. Gas-Discharge Plasma-Assisted Functionalization of Titanium Implant Surfaces. Materials Science Forum Vols. 2010;638-642:700–705. doi: 10.4028/www.scientific.net/MSF.638-642.700. Available from: http://dx.doi.org/10.4028/www.scientific.net/MSF.638-642.700. [DOI] [Google Scholar]
- 33.Stranak V, Wulff H, Rebl H, Zietz C, Arndt K, Bogdanowicz R, Nebe B, Bader R, Podbielski A, Hubicka Z, Hippler R. Deposition of thin titanium-copper films with antimicrobial effect by advanced magnetron sputtering methods. Materials Science and Engineering C. 2011;31(7):1512–1519. doi: 10.1016/j.msec.2011.06.009. Available from: http://dx.doi.org/10.1016/j.msec.2011.06.009. [DOI] [Google Scholar]