Abstract
Purpose of the review
Decisions to withdraw or withhold potentially life-sustaining treatment are common in intensive care and precede the majority of deaths. Where families resist or oppose doctors’ suggestions that it is time to stop treatment it is often unclear what should be done. This review will summarize recent literature around futility judgements in intensive care emphasising ethical and practical questions.
Recent findings
There has been a shift in the language of futility. Patients’ families often do not believe medical assessments that further treatment would be unsuccessful. Attempts to determine through data collection which patients have a low or zero chance of survival have been largely unsuccessful, and are hampered by varying definitions of futility. A due-process model for adjudicating futility disputes has been developed in Texas, and may provide a better solution to futility disputes than previous futility statutes.
Summary
Specific criteria for unilateral withdrawal of treatment have proved hard to define or defend. However, it is ethical for doctors to decline to provide treatment that is medically inappropriate or futile. Understanding the justification for a futility judgement may be relevant to deciding the most appropriate way to resolve futility disputes.
Keywords: Medical futility, Intensive care, Withholding treatment, Treatment refusal, Terminal care
Introduction
It is relatively easy to know when to start intensive care. Patients with single or multiple organ failure who are not responding to interventions that are readily available in hospital wards will likely die if they do not receive advanced life support. Physiological and clinical criteria for admission to intensive care units (ICU) are commonplace. But it is much harder to reach agreement and develop formal criteria for who to exclude from admission and on when to stop intensive care.
At the same time, decisions to withhold or withdraw potentially life-sustaining treatment (LST) are common; they precede the majority of deaths in emergency departments[1] and adult [2*][3-9], paediatric [10,11] and neonatal [12,13] intensive care. Where families agree with doctors that further treatment should not be provided decisions are usually straightforward, particularly if it is clear that this is not something that the patient themselves would have wanted. But where families resist or oppose doctors’ suggestions that it is time to stop treatment it is much less clear what should be done. Should doctors unilaterally withdraw or withhold LST against family (or more rarely patient) requests? Is it acceptable to continue treatment that medical professionals strongly believe should not be provided?
The concept of ‘futility’ arose as an attempt to resolve or to avoid disputes like this. It reflects a perceived need by doctors to limit patient or family autonomy and a way to justify a decision not to provide life-sustaining treatment.[14**] In this paper we discuss three aspects of recent literature around futility in intensive care: 1) The evolving nature of ‘futility’ 2) Attempts to resolve the futility problem through data collection 3) Procedural solutions to futility conflicts. In the conclusion we will suggest that a simpler, but more nuanced understanding of futility may be part of the way forward.
The evolving nature of futility
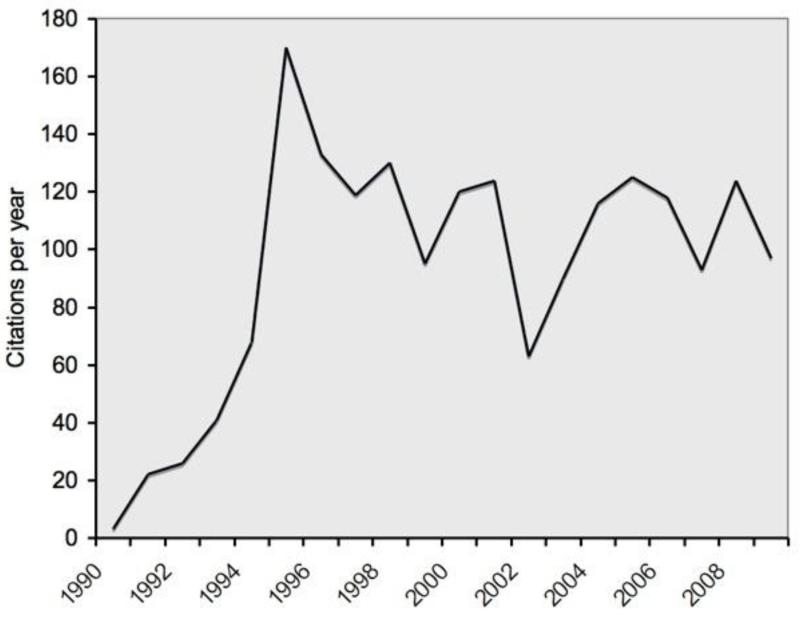
The idea of futility is not new. Famously, the Hippocratic oath included a promise not to treat patients who were “overmastered by their disease”.[15] But the futility debate in medical and ethical literature really began in the 1990s. In the previous decade there were a handful of papers discussing the term. However, after a paper in the Annals of Internal medicine in 1990[16] set out criteria for ‘medical futility’ there was a sharp increase in the number of medline citations (Figure 1). A decade later, an editorial in the New England Journal of Medicine noted the apparent waning of interest in futility.[17] The failure to reach agreement about the definition of futility or the criteria for judging treatment to be futile had led clinicians and ethicists to lose hope that the concept would help resolve conflicts about end-of-life-care.
Figure 1.
Medline citations per year for the Medical Subject Heading “medical futility” from 1990-2009
Yet the debate about futility has not gone away.[18*] Two recent cases that have received considerable media attention illustrate this. In March 2009, the New Jersey superior court ordered Trinitas Hospital to continue to provide intensive care for Ruben Betancourt, a 72 year old man with multi-organ failure and a persistent vegetative state. Treatment continued for an extra 3 months before Mr Betancourt finally died. [14**] A year earlier in Canada, 84 year old Samuel Golubchuk remained in intensive care for 9 months while the court delayed judgement on whether doctors could withdraw treatment against the wishes of his family (he died before a decision was reached).[19**][20*][21*] There is some evidence that that perceived futility remains the most common justification for withdrawal of treatment in critically ill patients[22][23*]; it is also one of the most frequent reasons for seeking ethics consultation.[24] The relatively large number of recent publications (Figure 1) points to ongoing academic interest in these questions.
One way that the debate has changed is that there has been a shift in the language used. There are multiple different ways that futility has been interpreted (Table 1). All of these have been criticised.[17,26,27] The most frequent criticism is that despite its air of objectivity a determination that treatment is futile is subjective and based on the values of the doctor.[27] For example, treatment is sometimes judged futile because the chance of recovery is very small (eg 0.5%). Yet some patients would regard a chance of this magnitude as worth taking if there were a possibility of recovery or long term survival and the alternative were death. Many individuals place money in a lottery where the chance of success is considerably less than this.[28] In one study of family members of critically ill patients, 32% of surrogates would choose continued treatment for their family member despite being told of a <1% chance of the patient surviving.[29**]
Table 1.
Definitions/subtypes of futility
| Physiological futility | Treatment that cannot achieve its physiological aim [25] |
| Quantitative futility | Treatment that has <1% chance of succeeding [16] |
| Qualitative futility | Treatment that cannot achieve an acceptable quality of life [26]; treatment that merely preserves unconsciousness or fails to relieve total dependence on intensive medical care [16] |
| Imminent demise futility | An intervention that will not change the fact that the patient will die in the near future [26] |
| Lethal condition futility | The patient has an underlying condition that will not be affected by the intervention and which will lead to death within weeks to months [26] |
Recent guidelines eschew the term futility altogether, and use a variety of synonyms instead (Table 2). Because ‘futile’ has proven so difficult to define, and has negative overtones, some have advocated that the term not be used at all when talking with families.[37] Two thirds of surrogate decision-makers in the study described above, indicated that they would not believe doctors if informed by a doctor that treatment was futile.[29**] However, it is not clear that any of the suggested alternatives to ‘futility’ are any more objective, any easier to define, nor any easier to convey to family members.
Table 2.
Alternative terms for futility
Attempts to resolve the futility problem
One way in which some have sought to reduce problems with futility is through collection of more data about prognosis, and attempting to define those patients in whom treatment is futile because of a low or zero chance of survival. Recent studies, however, have not been encouraging. One study from a paediatric intensive care unit in the Netherlands looked at the outcome at one year for children with severe neurological impairment who required mechanical ventilation,[38*] a group in whom intensive care is sometimes considered futile. There was a high mortality in the group, but 50% of the 22 severely impaired children who were ventilated were alive one year after their ICU admission.[38*] The authors concluded that mechanical ventilation “cannot be regarded as futile”. A study from Austria, Switzerland and Germany looked at factors predicting survival to hospital discharge in 1166 patients with out-of-hospital cardiac arrest who were managed by an advanced life support team and enrolled in a randomised controlled trial.[39*] Factors including the initial arrest rhythm, duration of arrest before provision of basic life support, and number of defibrillation attempts were included in a logistic regression. However, no combination of pre-hospital factors was able to provide a useful algorithm for predicting non-survival and eliminating unnecessary transfer to hospital.[39*] More encouraging were the results from a study from California that didn’t attempt to derive a prediction rule, but looked at the ability of intensivists to predict outcome for 144 patients in a neurosurgical intensive care unit who were ventilated for longer than 72 hours.[2*] There was a high mortality in this cohort (49%), and intensivists had a high level of accuracy at predicting poor outcome (moderate or greater disability, or death). Ninety-four per-cent of those patients in whom a poor outcome was predicted either died or were significantly impaired at 6-month follow-up.
However, all of these attempts to define futile treatment run into problems with self-fulfilling prophecies.[40*] This problem affects any condition where a high proportion of deaths follow decisions to limit LST. The danger is that where life-support is limited or withdrawn because of a predicted high risk of dying, the measured mortality rate will be artificially elevated. It has been argued that self-fulfilling prophecies contribute to mortality rates for adults with haemorrhagic stroke,[41] hypoxic brain injury,[42] critical illness,[43] and even brain death.[44]
One relevant example is whether it is futile to admit patients with malignancy to intensive care. A cohort study in one medical intensive care unit revealed that after adjusting for illness severity patients with a diagnosis of malignancy were three times more likely to have treatment withheld or withdrawn than those without that diagnosis.[45] On the other hand, there is evidence of improving survival in cancer patients when they are admitted to ICU, challenging previous assumptions that prognosis is inevitably poor, and treatment futile.[46]
Even where the problems of self-fulfilling prophecies are excluded by focussing on those patients who received maximal support, it is rarely possible to achieve a high level of certainty that survival is not possible. A recent review systematically looked at empirical evidence used to support or refute claims of medical futility.[47**] Many studies lacked explicit criteria for determining whether or not treatment was futile. Less than 1/3 of studies that claimed to demonstrate that treatment was futile actually met the most common standard for quantitative futility (Table 1). Although many of the studies gave point estimates of 100% mortality, few were large enough to exclude the possibility that a small proportion of patients would survive if treated.[47**] On the other hand, variable definitions of futility mean that treatment might still be regarded as futile even if it is not ‘quantitatively futile’.
Procedural solutions to futility
There have been two different legislative approaches to futility. One approach has been to set out criteria for unilateral withdrawal or withholding of treatment. There are statutes of this sort in the majority of states in the US (eg the Unilateral Health Care Decisions Act),[48] however, they appear to be ineffective. In a study in the in the late 1990s, the majority of US hospitals surveyed did not have futility policies.[49] Furthermore, it appears that even where such policies exist they are rarely invoked and treatment is usually continued if families request it.[48] The problem with such statutes may be at least in part that vague and imprecise definitions of futility do not provide a ‘safe harbour’ to protect against litigation.[48]
The second approach to futility focuses on the process for dealing with disputes rather than the criteria for withdrawing or withholding treatment. This approach is exemplified in the Texas Advance Directives Act,[33] which sets out an extrajudicial process of review involving hospital ethics committees.[32**] If doctors believe that providing treatment would be inappropriate for patients who are terminally or irreversibly ill, they may invoke the act and seek ethics committee review. If the committee agrees with doctors, families are given 10 days to find another healthcare provider willing to provide treatment, otherwise treatment will be withdrawn. In 2005, there were an estimated 974 futility cases reviewed by ethics committees in Texas.[32**] In the majority of cases, families and doctors were able to reach agreement about ongoing treatment. In 65 cases, ‘10-day letters’ were issued, and in 27 patients treatment was withdrawn.[32**] The Texas solution to futility disputes has been criticised for leaving decisions to ethics committees comprised largely of medical practitioners,[20,48][50**] and for giving families no recourse to the courts. Defenders of the due process approach have admitted that it is the worst method for resolving futility disputes, except for all the rest.[32**]
Futility moving forward
Is it possible to make progress in an area like futility that is plagued by dispute and disagreement? One positive step would be to agree on and be consistent in the terms that doctors use. What is a futile or medically inappropriate treatment? To put it simply, it is a treatment that is of sufficiently low efficacy that doctors believe it should not be provided even if the patient or his/her surrogates request it. We prefer the term “medically inappropriate” to “futile” for two reasons. Firstly, ‘medically inappropriate’ makes it clear that these are value judgements made by medical professionals. It avoids the pseudo-objectivity that is sometimes implied by the term ‘futile’. Secondly, referring to the inappropriateness of treatment highlights the importance of being clear about what treatment is appropriate for.[27][51**] Whether or not a treatment is judged appropriate depends crucially on what the goals of treatment are.[52] Where doctors and families disagree about the goals of treatment, they are unlikely to come to an agreement about futility.
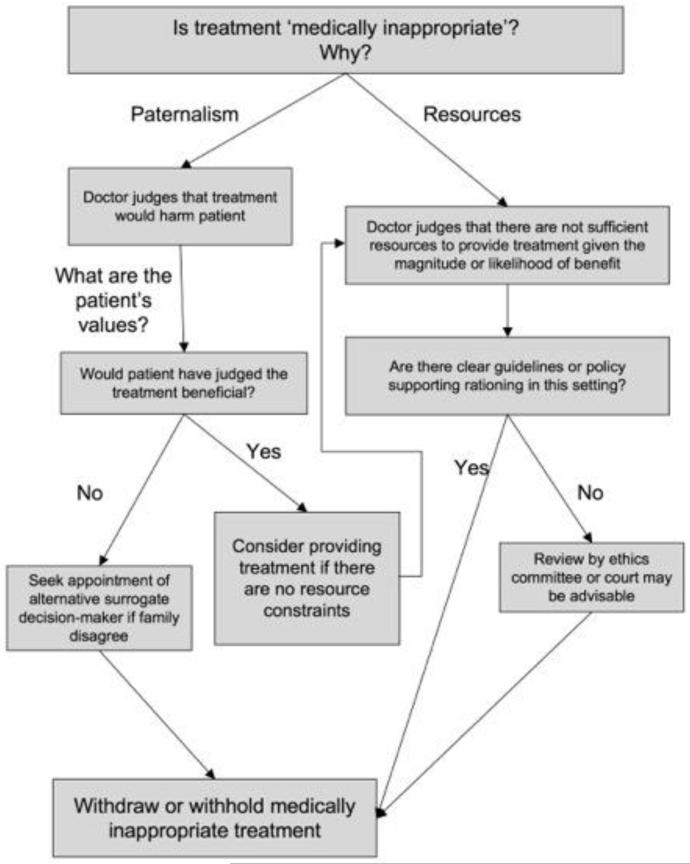
A second important step is to be clear and open with families about the reasons why treatment is judged to be medically inappropriate. There are ultimately only two ethical justifications for refusing to provide treatment that a patient or their surrogate wants provided.[25] The first is that the doctor believes that further treatment is contrary to the patient’s interests and would harm them. It is a type of paternalistic judgment about the value of treatment and life. Either the quantity of life (duration of survival) is so short or improbable, or the quality of their life so reduced, that the pain, suffering, distress and indignities of treatment outweigh the benefits. The second, and more controversial, justification is that providing treatment would be harmful to other patients.[53] In a setting of limited resources (for example intensive care beds), providing treatment to this patient would mean denying treatment to other patients with a significantly greater chance of benefit.[54,55] Sometimes both of these reasons may be present.
Understanding the justification of a futility judgement may be relevant to deciding whether treatment is futile and to the most appropriate way to resolve futility disputes (Table 3). For example, where the judgement is on the basis of the patient’s best interests it is reasonable to give considerable weight to the individual’s own values. Some people judge life worth living even it is accompanied by severe pain or disability, or where prolonged survival is unlikely. The doctor may not share these values, but it is hard to see why medical values should take precedence over the patient’s own. If families or surrogates do not appear to be genuinely representing the wishes of the patient the appropriate response may be to have an alternative surrogate decision-maker appointed.[50**] On the other hand, where the judgement of futility is on the basis of limited resources, patients’ wishes are arguably less relevant, and what is important is whether this is a fair and reasonable basis for limiting treatment. Decisions should ideally be based on consensus guidelines or hospital policy,[54] or alternatively follow a due process model such as that used in Texas. Ethics consultation may be beneficial. A multicenter randomized trial has demonstrated that ethics consultation for intensive care patients with conflicts related to treatment led to reduced duration of mechanical ventilation, intensive care and hospital stay, without an effect on mortality rates.[56] Figure 2 represents a summary of one approach to resolving futility disputes.
Table 3.
Options for resolving futility disputes
| 1. Capitulation – provide treatment that patient or surrogate requests even if judged futile by doctors |
| 2. Unilateral withdrawal/withholding – decline to provide treatment that patient/surrogate requests if doctors judge it futile |
| 3. Mediation/adjudication by ethics committee |
| 4. Seek appointment of different surrogate |
| 5. Adjudication by court |
Figure 2.
An approach to determining whether treatment is futile or medically inappropriate, and to resolving futility disputes.
Finally, where the costs of treatment are small and the risk of harm to the patient negligible, it is arguably appropriate to treat even if the provider thinks that it would be futile to do so. For example, Robert Truog has argued recently that in some circumstances it is ethical to provide futile CPR.[57*][58*]
Conclusions
Decisions to withdraw or withhold intensive care treatment are complex and value laden; it has not proved possible to generate specific criteria for them. However, it is ethical for doctors to decline to provide treatment that is judged to be medically inappropriate or futile either where such treatment is contrary to the interests of the patient, or where there are insufficient resources to provide treatment of this level of benefit. Although resources are rarely discussed in futility disputes, these may provide the strongest rationale for judging treatment to be medically inappropriate, in the absence of clear information about patient values.
Key Points.
A judgement that further treatment would be futile or medically inappropriate is one of the most common justifications for limiting potentially life-sustaining treatment in intensive care
There has been a shift in the language of futility, with recent guidelines using a variety of synonyms or euphemisms.
Studies of outcome from treatment are influenced by self-fulfilling prophecies and are rarely able to substantiate a claim that further treatment would be quantitatively futile
It is ethical for doctors to decline to provide treatment that is judged to be medically inappropriate or futile either where such treatment is contrary to the interests of the patient, or where there are insufficient resources to provide treatment.
Acknowledgements
Funding: This work was supported in part by a grant from the Wellcome Trust [086041/Z/08/Z].
REFERENCES
- 1.Le Conte P, Riochet D, Batard E, et al. Death in emergency departments: a multicenter cross-sectional survey with analysis of withholding and withdrawing life support. Intensive Care Med. 2010;36:765–772. doi: 10.1007/s00134-010-1800-1. [DOI] [PubMed] [Google Scholar]
- 2.Finley Caulfield A, Gabler L, Lansberg MG, et al. Outcome prediction in mechanically ventilated neurologic patients by junior neurointensivists. Neurology. 2010;74:1096–1101. doi: 10.1212/WNL.0b013e3181d8197f. [DOI] [PMC free article] [PubMed] [Google Scholar]; * Study of the relationship between predicted and actual outcome for patients (ventilated for at least three days) in a single neurosurgical-intensive care unit.
- 3.Brieva JL, Cooray P, Rowley M. Withholding and withdrawal of life-sustaining therapies in intensive care: an Australian experience. Crit Care Resusc. 2009;11:266–268. [PubMed] [Google Scholar]
- 4.Spronk PE, Kuiper AV, Rommes JH, et al. The practice of and documentation on withholding and withdrawing life support: a retrospective study in two Dutch intensive care units. Anesthesia and analgesia. 2009;109:841–846. doi: 10.1213/ane.0b013e3181acc64a. [DOI] [PubMed] [Google Scholar]
- 5.Cooper Z, Rivara FP, Wang J, et al. Withdrawal of life-sustaining therapy in injured patients: variations between trauma centers and nontrauma centers. J Trauma. 2009;66:1327–1335. doi: 10.1097/TA.0b013e31819ea047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Varelas PN, Hacein-Bey L, Schultz L, et al. Withdrawal of life support in critically ill neurosurgical patients and in-hospital death after discharge from the neurosurgical intensive care unit. Clinical article. Journal of neurosurgery. 2009;111:396–404. doi: 10.3171/2009.3.JNS08493. [DOI] [PubMed] [Google Scholar]
- 7.Bertolini G, Boffelli S, Malacarne P, et al. End-of-life decision-making and quality of ICU performance: an observational study in 84 Italian units. Intensive Care Med. 2010;36:1495–1504. doi: 10.1007/s00134-010-1910-9. [DOI] [PubMed] [Google Scholar]
- 8.Sprung CL, Cohen SL, Sjokvist P, et al. End-of-life practices in European intensive care units: the Ethicus Study. JAMA. 2003;290:790–797. doi: 10.1001/jama.290.6.790. [DOI] [PubMed] [Google Scholar]
- 9.Piva J, Lago P, Othero J, et al. Evaluating end of life practices in ten Brazilian paediatric and adult intensive care units. J Med Ethics. 2010;36:344–348. doi: 10.1136/jme.2009.035113. [DOI] [PubMed] [Google Scholar]
- 10.Naghib S, van der Starre C, Gischler SJ, et al. Mortality in very long-stay pediatric intensive care unit patients and incidence of withdrawal of treatment. Intensive Care Med. 2010;36:131–136. doi: 10.1007/s00134-009-1693-z. [DOI] [PubMed] [Google Scholar]
- 11.Sands R, Manning JC, Vyas H, et al. Characteristics of deaths in paediatric intensive care: a 10-year study. Nursing in critical care. 2009;14:235–240. doi: 10.1111/j.1478-5153.2009.00348.x. [DOI] [PubMed] [Google Scholar]
- 12.Verhagen A, Dorscheidt J, Engels B, et al. End-of-life decisions in Dutch neonatal intensive care units. Arch Pediatr Adolesc Med. 2009;163:895–901. doi: 10.1001/archpediatrics.2009.166. [DOI] [PubMed] [Google Scholar]
- 13.Verhagen AA, Janvier A, Leuthner SR, et al. Categorizing neonatal deaths: a cross-cultural study in the United States, Canada, and The Netherlands. J Pediatr. 2010;156:33–37. doi: 10.1016/j.jpeds.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 14.Pope TM. Legal briefing: medical futility and assisted suicide. J Clin Ethics. 2009;20:274–286. [PubMed] [Google Scholar]; ** US legal scholar Thaddeus Pope provides a summary of recent changes to the law and key legal cases involving medical futility in the US, Canada, UK and Australia. He summarises statutes, ex-ante cases that have gone to the courts, cases replacing surrogates, and ex-post cases of court review after treatment withdrawal.
- 15.Whitmer M, Hurst S, Prins M, et al. Medical futility: a paradigm as old as Hippocrates. Dimens Crit Care Nurs. 2009;28:67–71. doi: 10.1097/DCC.0b013e318195d43f. [DOI] [PubMed] [Google Scholar]
- 16.Schneiderman LJ, Jecker NS, Jonsen AR. Medical futility: its meaning and ethical implications. Ann Intern Med. 1990;112:949–954. doi: 10.7326/0003-4819-112-12-949. [DOI] [PubMed] [Google Scholar]
- 17.Helft PR, Siegler M, Lantos J. The rise and fall of the futility movement. N Engl J Med. 2000;343:293–296. doi: 10.1056/NEJM200007273430411. [DOI] [PubMed] [Google Scholar]
- 18.Luce JM. A history of resolving conflicts over end-of-life care in intensive care units in the United States. Crit Care Med. 2010;38:1623–1629. doi: 10.1097/CCM.0b013e3181e71530. [DOI] [PubMed] [Google Scholar]; * Review of the history of conflicts over end-of-life care in intensive care, including key legal decisions, futility policies, and criticisms of ‘futility’.
- 19.Jotkowitz A, Glick S, Zivotofsky AZ. The case of Samuel Golubchuk and the right to live. Am J Bioeth. 2010;10:50–53. doi: 10.1080/15265160903581700. [DOI] [PubMed] [Google Scholar]; ** Interesting article in the American Journal of Bioethics (with a set of accompanying commentaries). The authors review a Canadian futility dispute and a policy developed by the College of Physicians and surgeons in Manitoba. They argue that the doctors’ attempt to withdraw treatment, and the new guidelines were contrary to the principle of autonomy, culturally insensitive, and flawed because of prognostic uncertainty
- 20.Pope TM. The case of Samuel Golubchuk: the dangers of judicial deference and medical self-regulation. Am J Bioeth. 2010;10:59–61. doi: 10.1080/15265160903581908. [DOI] [PubMed] [Google Scholar]; * Thaddeus Pope disagrees with Jotkowitz et al on the legal principle of patient autonomy, and argues that there is a need for an independent dispute resolution process when (as is often the case) futility disputes are religiously motivated
- 21.Paris JJ. Autonomy does not confer sovereignty on the patient: a commentary on the Golubchuk case. Am J Bioeth. 2010;10:54–56. doi: 10.1080/15265160903581916. [DOI] [PubMed] [Google Scholar]; * Ethicist John Paris replies to Jotkowitz et al, arguing that the principle of autonomy is the paramount principle in medical practice, and does not confer a right to demand treatment.
- 22.Bloomer MJ, Tiruvoipati R, Tsiripillis M, et al. End of life management of adult patients in an Australian metropolitan intensive care unit: A retrospective observational study. Aust Crit Care. 2010;23:13–19. doi: 10.1016/j.aucc.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Seale C. Hastening death in end-of-life care: a survey of doctors. Soc Sci Med. 2009;69:1659–1666. doi: 10.1016/j.socscimed.2009.09.025. [DOI] [PubMed] [Google Scholar]; * A survey reporting the practice of 2923 UK doctors who had cared for patients who had died in the previous 12 months. 28.9% of doctors reported having taken actions that they expected or intended to hasten death
- 24.Romano ME, Wahlander SB, Lang BH, et al. Mandatory ethics consultation policy. Mayo Clin Proc. 2009;84:581–585. doi: 10.1016/S0025-6196(11)60746-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Youngner SJ. Who defines futility? JAMA. 1988;260:2094–2095. [PubMed] [Google Scholar]
- 26.Brody BA, Halevy A. Is futility a futile concept? J Med Philos. 1995;20:123–144. doi: 10.1093/jmp/20.2.123. [DOI] [PubMed] [Google Scholar]
- 27.Truog RD, Brett AS, Frader J. The problem with futility. N Engl J Med. 1992;326:1560–1564. doi: 10.1056/NEJM199206043262310. [DOI] [PubMed] [Google Scholar]
- 28.Truog RD. The conversation around CPR/DNR should not be revived--at least for now. Am J Bioeth. 2010;10:84–85. doi: 10.1080/15265160903460988. [DOI] [PubMed] [Google Scholar]
- 29.Zier LS, Burack JH, Micco G, et al. Surrogate decision makers’ responses to physicians’ predictions of medical futility. Chest. 2009;136:110–117. doi: 10.1378/chest.08-2753. [DOI] [PMC free article] [PubMed] [Google Scholar]; **A mixed qualitative and quantitative study of surrogate decision-makers of 50 critically ill patients in Californian intensive care units. Surrogates were asked about their views of the accuracy of physician’s futility predictions. A modified time-trade-off technique was used to assess the probability of death (predicted by doctors) at which they would be willing to withdraw life support.
- 30.Doukas DJ, McCullough LB. A preventive ethics approach to counseling patients about clinical futility in the primary care setting. Archives of family medicine. 1996;5:589–592. doi: 10.1001/archfami.5.10.589. [DOI] [PubMed] [Google Scholar]
- 31.American College of Emergency Physicians Non-beneficial (‘Futile’) Emergency Medical Interventions. Available at: http://www.acep.org/practres.aspx?id=29590 accessed 07/10/2010.
- 32.Fine RL. Point: The Texas advance directives act effectively and ethically resolves disputes about medical futility. Chest. 2009;136:963–967. doi: 10.1378/chest.09-1267. [DOI] [PubMed] [Google Scholar]; ** Ethicist Robert Fine (involved in the development of the Texas act), argues that it is a fair, effective and appropriate process for dealing with medical futility
- 33.Texas Health and Safety Code . Advance Directives. 2002. Chapter 166. 166.046. [Google Scholar]
- 34.General Medical Council . Treatment and care towards the end of life: good practice in decision making. GMC; London: 2010. [Google Scholar]; * Revised UK guidelines on end-of-life care. Treatment need not be provided if doctors believe that it would not be “clinically appropriate”, though patients or families should be explained the reasons for this judgement, and their options (including seeking a second opinion and statutory review).
- 35.McCabe MS, Storm C. When doctors and patients disagree about medical futility. Journal of oncology practice / American Society of Clinical Oncology. 2008;4:207–209. doi: 10.1200/JOP.0848503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.College of Physicians and Surgeons of Manitoba Withholding and withdrawing life-sustaining treatment. Statement no. 1602 Available at: http://www.cpsm.mb.ca/statements/st1602.pdf accessed.
- 37.Grossman E, Angelos P. Futility: what Cool Hand Luke can teach the surgical community. World J Surg. 2009;33:1338–1340. doi: 10.1007/s00268-009-9997-2. [DOI] [PubMed] [Google Scholar]
- 38.van Gestel JP, Robroch AH, Bollen CW, et al. Mechanical ventilation for respiratory failure in children with severe neurological impairment: is it futile medical treatment? Dev Med Child Neurol. 2010;52:483–488. doi: 10.1111/j.1469-8749.2009.03582.x. [DOI] [PubMed] [Google Scholar]; * A study of one-year outcomes for 22 severely neurologically impaired children admitted to a single paediatric intensive care unit.
- 39.Pircher IR, Stadlbauer KH, Severing AC, et al. A prediction model for out-of-hospital cardiopulmonary resuscitation. Anesthesia and analgesia. 2009;109:1196–1201. doi: 10.1213/ane.0b013e3181b15a70. [DOI] [PubMed] [Google Scholar]; * Nested study of factors predicting survival to hospital discharge and neurological outcome in 1166 patients with out-of-hospital cardiac arrest treated with advanced cardiac life support.
- 40.Wilkinson D. The self-fulfilling prophecy in intensive care. Theor Med Bioeth. 2009;30:401–410. doi: 10.1007/s11017-009-9120-6. [DOI] [PubMed] [Google Scholar]; * An analysis of the practical and ethical problems arising from self-fulfilling prophecies in intensive care
- 41.Becker KJ, Baxter AB, Cohen WA, et al. Withdrawal of support in intracerebral hemorrhage may lead to self-fulfilling prophecies. Neurology. 2001;56:766–772. doi: 10.1212/wnl.56.6.766. [DOI] [PubMed] [Google Scholar]
- 42.Zandbergen E, De Haan R, Stoutenbeek C, et al. Systematic review of early prediction of poor outcome in anoxic ischaemic coma. Lancet. 1998;352:1808–1812. doi: 10.1016/S0140-6736(98)04076-8. [DOI] [PubMed] [Google Scholar]
- 43.Cook D, Rocker G, Marshall J, et al. Withdrawal of mechanical ventilation in anticipation of death in the intensive care unit. N Engl J Med. 2003;349:1123–1132. doi: 10.1056/NEJMoa030083. [DOI] [PubMed] [Google Scholar]
- 44.Truog R, Robinson W. Role of brain death and the dead-donor rule in the ethics of organ transplantation. Crit Care Med. 2003;31:2391–2396. doi: 10.1097/01.CCM.0000090869.19410.3C. [DOI] [PubMed] [Google Scholar]
- 45.Cavallazzi R, Hirani A, Vasu TS, et al. Influence of malignancy on the decision to withhold or withdraw life-sustaining therapy in critically ill patients. The American journal of hospice & palliative care. 2009;26:464–469. doi: 10.1177/1049909109341872. [DOI] [PubMed] [Google Scholar]
- 46.Darmon M, Azoulay E. Critical care management of cancer patients: cause for optimism and need for objectivity. Current opinion in oncology. 2009;21:318–326. doi: 10.1097/CCO.0b013e32832b68b6. [DOI] [PubMed] [Google Scholar]
- 47.Gabbay E, Calvo-Broce J, Meyer KB, et al. The empirical basis for determinations of medical futility. J Gen Intern Med. 2010;25:1083–1089. doi: 10.1007/s11606-010-1445-3. [DOI] [PMC free article] [PubMed] [Google Scholar]; ** A systematic review including 92 papers which presented outcome data in critically ill or cardiac arrest patients and which claimed that this data supported or refuted a judgement of ‘futility’. The authors looked at the criteria used for judging futility, and the point estimates for mortality (with confidence intervals) based on the presented data. There was statistical overlap between data used to support, and data used to refute claims of futility.
- 48.Pope TM. Medical futility statutes: no safe harbor to unilaterally refuse life-sustaining treatment. Tennessee Law Review. 2007;75:1–81. [Google Scholar]
- 49.Johnson SH, Gibbons VP, Goldner JA, et al. Legal and institutional policy responses to medical futility. J Health Hosp Law. 1997;30:21–36. [PubMed] [Google Scholar]
- 50.Truog RD. Counterpoint: The Texas advance directives act is ethically flawed: medical futility disputes must be resolved by a fair process. Chest. 2009;136:968–971. doi: 10.1378/chest.09-1269. discussion 971-963. [DOI] [PubMed] [Google Scholar]; ** Ethicist (and intensivist) Robert Truog responds to Fine. He accepts that the Texas act is an effective compromise, however, argues that it is constitutionally and ethically problematic.
- 51.Chwang E. Futility clarified. J Law Med Ethics. 2009;37:487–495. 396. doi: 10.1111/j.1748-720X.2009.00409.x. [DOI] [PubMed] [Google Scholar]; ** Philosopher Eric Chwang argues that futility is easy to define (it is the same as ‘uselessness’). However, it is not possible concisely to set out the criteria for futility, since the goals of medicine are not able to be reduced to a simple algorithm.
- 52.Mohindra RK. Medical futility: a conceptual model. J Med Ethics. 2007;33:71–75. doi: 10.1136/jme.2006.016121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Niederman M, Berger J. The delivery of futile care is harmful to other patients. Crit Care Med. 2010;38:S518–S522. doi: 10.1097/CCM.0b013e3181f1cba5. [DOI] [PubMed] [Google Scholar]
- 54.Orentlicher D. Rationing health care: its a matter of the health care system’s structure. Annals of health law. 2010;19:449. [PubMed] [Google Scholar]
- 55.McDermid RC, Bagshaw SM. Prolonging life and delaying death: the role of physicians in the context of limited intensive care resources. Philos Ethics Humanit Med. 2009;4:3. doi: 10.1186/1747-5341-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Schneiderman LJ, Gilmer T, Teetzel HD, et al. Effect of ethics consultations on nonbeneficial life-sustaining treatments in the intensive care setting: a randomized controlled trial. JAMA. 2003;290:1166–1172. doi: 10.1001/jama.290.9.1166. [DOI] [PubMed] [Google Scholar]
- 57.Truog RD. Is it always wrong to perform futile CPR? N Engl J Med. 2010;362:477–479. doi: 10.1056/NEJMp0908464. [DOI] [PubMed] [Google Scholar]; * Truog discusses a case of futile CPR, and argues that in some circumstances it can be an act of caring and compassion
- 58.Paris JJ, Angelos P, Schreiber MD. Does compassion for a family justify providing futile CPR? J Perinatol. 2010 doi: 10.1038/jp.2010.105. [DOI] [PubMed] [Google Scholar]; * Paris provides a commentary on the above case, and argues that it violates the Kantian imperative against using individuals as a mere means, and that there is no way of clearly defining cases where futile treatment may be justifiably provided.