Abstract
Mangiferin-mediated down-regulation of NFκB showed potential for chemotherapeutic agent-mediated cell death, suggesting a role in combination therapy for cancer. In this study the combined mechanism of the anticancer action of oxaliplatin and mangiferin was investigated. MTT dose response curves, trypan blue staining, caspase 3 assays as well as DNA cell cycle analyses were performed on HeLa, HT29 and MCF7 cancer cell lines, with and without the addition of 10 µg/ml mangiferin. Mitochondrial membrane potential, DNA fragmentation, resistance induction studies and NFκB assays were performed on HT29 cells only. Addition of 10 µg/ml mangiferin reduced oxaliplatin IC50 values in HT29 (3.4 fold) and HeLa (1.7 fold) cells in the MTT assay while reducing trypan blue staining. This was accompanied by increased caspase 3 activation and DNA fragmentation and a delay in the S-phase of the cell cycle. Mitochondrial membrane permeabilization was not enhanced in the combination treatment. Mangiferin was shown to cause a reduction of NF-κB activation in HT29 cells rendered resistant to oxaliplatin. The present study indicates that mangiferin in combination with oxaliplatin favours apoptotic cell death and thereby improves the efficacy of oxaliplatin in vitro. In addition, combination therapy with mangiferin may also counteract the development of resistance in cancer cell lines.
Keywords: Oxaliplatin, Mangiferin, Combination treatment, Apoptosis, Drug resistance
Introduction
Cancer is an important public health concern around the world and the application of inorganic chemistry to medicine is a fast developing field (Parker et al., 1997; Walker and Walker, 1999). Novel therapeutic and diagnostic metal complexes are having a vast impact on medical practice. Advances in bio-coordination chemistry are crucial for improving the design of compounds to reduce toxic side effects and to aid in the understanding of their mechanisms of action (Sadler and Guo, 1998). At the same time traditional medicine is an integral part of South African cultural life, a position that is unlikely to change to any significant degree in years to come. It is estimated that between 12 and 15 million South Africans depend on traditional herbal medicines from as many as 700 indigenous plant species (Duncan et al., 1999).
The platinum drugs represent a unique and important class of anti-tumour agents. The discovery of cisplatin in the 1970s has revolutionized the chemotherapy of human cancer (Gonzalez et al., 2001). Unfortunately the full therapeutic potential of cisplatin has not been realized due to the serious side effects and the emergence of cisplatin-resistant tumour cells related to treatment with cisplatin (Walker and Walker, 1999). Many second-generation cisplatin-analogues have been synthesized and some of these, such as oxaliplatin, have been shown to produce the same therapeutic effects as cisplatin, but with lower required doses and reduced side-effects. Oxaliplatin is also clinically active in metastatic colorectal cancer, whereas cisplatin has a very low efficiency (Sergent et al., 2002).
The anticancer properties of tea are well known, and the tumour inhibition potential of certain polyphenolic compounds from green and black tea has been well documented (Marnewick et al., 2000; Marnewick et al., 2004; Marnewick et al., 2005). Honey-bush tea is a South African herbal beverage that is currently receiving prominent attention. Honey-bush tea is prepared from the leaves, stems and flowers of several Cyclopia spp. The major phenolic components of the unprocessed South African honey-bush tea are the xanthone, mangiferin and the flavanone, hesperidin (Marnewick et al., 2005).
Mangiferin is a natural polyphenol known to exhibit anti-inflammatory, antioxidant, and antiviral effects, though the molecular mechanism underlying these effects has not been well characterized. NF-κB plays an important role in these processes; hence it may be possible that mangiferin modulates NFκB activation.
NFκB is a transcription factor that exerts anti-apoptotic effects and is often activated in cancer cells in response to chemotherapeutic agents. This promotes cancer therapy resistance in tumours (Baldwin, 2001). The improper activation of NFκB in diseases such as tumourigenesis (Paul et al., 2006; Lee et al., 2008) has been linked to TNFα and other members of its superfamily. Through the activation of NFκB, TNFα induces the expression of various genes that can be involved in tissue invasion and metastasis. In addition, activation of NFκB can suppress apoptosis, which is likely to enhance tumourigenesis and may also play a role in chemotherapeutic agent resistance. Sarkar et al. (2004) showed that mangiferin blocks tumour necrosis factor (TNF)-induced NFκB activation and NFκB-dependent genes like ICAM1 and COX2. The effect was mediated through inhibition of IB (inhibitor proteins)-kinase complex (IKK) activation and subsequent blocking of phosphorylation and degradation of IκB-α (inhibitor protein α). Mangiferin inhibits TNF-induced p65 phosphorylation as well as translocation to the nucleus and also inhibits NFκB activation induced by other inflammatory agents. It has previously been shown that the development of anti-cancer drugs that can “switch” the function of NFκB from anti-apoptotic to pro-apoptotic may prove to be beneficial in the fight against cancer (Perkins, 2000; Perkins, 2004). Supranormal activation of NFκB is connected to cancer. Active NFκB promotes tumour growth by increasing the transcription of genes that are: anti-apoptotic; inducers of cell proliferation; pro-angiogenic; pro-metastatic and responsible for other cellular mechanisms related to tumour growth. Hence, tumour prevention may be achieved through inhibition of abnormally active NFκB (Perkins, 2000; Perkins, 2004).
Mangiferin's ability to inhibit NFκB and increase the intracellular GSH levels, suggest that it may be a potent agent for anti-inflammatory and antioxidant therapy. Mangiferin-mediated down-regulation of NFκB also shows potential for chemotherapeutic agent-mediated cell death, suggesting a role in combination therapy for cancer (Sarkar et al., 2004). In this study the combined mechanism of the anticancer action of oxaliplatin and mangiferin was investigated to determine whether such combination treatment results in enhanced apoptosis induction, as well as to determine whether mangiferin may counteract the development of resistance to oxaliplatin by reducing active NFκB levels.
Methods
Drugs
Oxaliplatin solutions were prepared fresh on the day of use by dissolving the required concentration in RPMI1640 (Sigma) containing 10% fetal calf serum (Delta Bioproducts, South Africa) by vortexing (1 min) followed by sonication (15 mins). Mangiferin was purchased from Sigma and the required concentrations prepared fresh in RPMI1640 containing 10% fetal calf serum on the day of use. The concentration of mangiferin used was 10 µg/ml (Sarkar et al., 2004).
Cell Lines
Three human cancer cell lines, HeLa (cervical cancer), HT29 (colon cancer) and MCF7 (breast cancer), were maintained in 10 cm culture dishes (Nunc) at 37°C in a humidified incubator containing 5% CO2 in growth medium (RPMI1640 supplemented with 10% fetal calf serum).
Dose response curves
Dose response curves were performed by using the MTT assay (Sigma) and the IC50 values were calculated using the GraphPad Prism4 software package. Cells (200µl per well) were seeded in flat-bottom 96 well culture plates (Nunc) at 30 000 cells per milliliter and incubated overnight at 37°C in a humidified incubator containing 5% CO2. Cells were allowed to attach and recover for 24 hrs before oxaliplatin was added to the wells at concentrations of 100, 50, 25, 10, 5 and 1µM, with and without the addition of 10µg/ ml mangiferin, and incubated for 48 hrs before the MTT assay was performed. A stock solution of MTT was prepared in PBSA (5 mg/ ml) and further diluted to 0.5 mg/ ml with growth medium. The medium from each well was replaced with 200µL MTT solution before the plates were incubated for another 3 hrs. MTT solution was replaced by 200µL DMSO and absorbance read at 540nm on a Labsystems Multiskan MS Plate Reader.
Caspase 3 activity
Caspase 3 activity was determined using the Cleaved Caspase 3 (Asp 175) Alexa Fluor® 488 Antibody (Beckman Coulter). Cells were seeded into 10cm cell culture dishes (Nunc) at 1.15×105 cells per ml and incubated in a 37°C incubator supplemented with 5% CO2 for 24 hours before 10µM of oxaliplatin was added, with and without the addition of 10µg/ ml mangiferin, and incubated for 15 hrs. The assay was performed, as per supplied instructions, and analyzed on a Beckman Coulter FC500 flow cytometer.
Trypan blue assay
The trypan blue assay was performed using a standard 0.4% trypan blue solution (Sigma) in phosphate buffered saline without calcium or magnesium. Cells (1ml per well) were seeded in flat-bottom 24 well culture plates (Nunc) at 500 000 cells per milliliter and incubated overnight at 37°C in a humidified incubator containing 5% CO2. Cells were allowed to attach and recover for 24 hours before they were exposed to 10µM of oxaliplatin, with and without the addition of 10µg/ ml mangiferin. The cells were trypsinised and counted with a heamocytometer in a 1:1 dilution of cells in a 0.4% trypan blue solution and the percentage of non-viable cells was calculated.
DNA cell cycle analysis
DNA cell cycle analysis was performed using the Coulter® DNA Prep™ Reagents Kit (Beckman Coulter). Cells were seeded and treated as described for the caspase 3 assay. The assay was performed as per kit instructions and the results analyzed on a Beckman Coulter FC500 flow cytometer.
DNA fragmentation assay
DNA fragmentation assays were performed using the Apo-BRDUtm kit (Phoenix Flow Systems). HT29 cells (5 mL aliquots) were seeded into 50ml non-adherent cell culture flasks (Nunc) at a density of 100 000 cells/ mL and were incubated for 48 hrs with 10µM of oxaliplatin, with and without the addition of 10µg/ ml mangiferin, before the assay was performed as per kit instructions and the results analyzed on a Beckman Coulter FC500 flow cytometer.
Mitochondrial transmembrane potential assay
Mitochondrial transmembrane potential studies were performed using the Guava® EasyCyte™ MitoPotential™ Kit (Guava Technologies). HT29 cells were seeded and treated as for DNA fragmentation, before the assay was performed as per kit instructions and the results analyzed on a Beckman Coulter FC500 flow cytometer.
Induction of resistance
HT29 colon cancer cells were exposed intermittently and incrementally to oxaliplatin, with and without the addition of 10µg/ ml mangiferin. Table 1 illustrates the conditions for inducing resistance in these cells. The degree of resistance was determined by performing dose response curves on these cells as above.
Table 1.
The conditions for inducing resistance to oxaliplatin in cancer cell lines.
| [Platinum drug] (µM) | Time exposed (hours) |
| 10 | 0.5 |
| 10 | 1.0 |
| 10 | 1.5 |
| 100 | 0.5 |
| 100 | 1.0 |
| 100 | 1.5 |
| 100 | 1.0 |
| 100 | 1.0 |
NF-κB Assay
The Phospho-NF-κB p65 (Ser536) (93H1) Rabbit mAb (Alexa Fluor®488 Conjugate) Kit (Cell Signalling Technology) was used to study the effect of resistance, with and without the addition of 10µg/ ml mangiferin, on the expression of NF-κB. HT29 cells (5 mL aliquots) were seeded into 50ml non-adherent cell culture flasks (Nunc) at a density of 100 000 cells/ mL and were incubated for 48 hrs with 10µM of oxaliplatin, with and without the addition of 10µg/ ml mangiferin, before the assay was performed as per kit instructions and the results analyzed on a Beckman Coulter FC500 flow cytometer with a minimum of 10 000 events being recorded.
Statistical analysis
Statistical analysis was performed via the Student's T-test. Certain experiments (trypan blue assay and caspase 3 assay) were performed in duplicate and therefore the average deviation of the values is depicted on the graphs. For flow cytometric analysis a minimum of 10 000 events were recorded.
Results and Discussion
The results obtained in Table 2 indicate that mangiferin enhances the effect of oxaliplatin on HeLa and HT29 cells, as lower IC50 values were obtained in combination with mangiferin in these two cell lines. This was, however, not the case in MCF7 cells.
Table 2.
IC50 values for oxaliplatin with and without the addition of 10µg/ ml mangiferin.
| IC50 (µM) | |||
| Treatment | HeLa | HT29 | MCF7 |
| Oxaliplatin | 11.92 | 12.30 | 6.21 |
|
Oxaliplatin + manigferin |
6.86 (1.7) | 3.63 (3.4) | 8.31 (0.75) |
Brackets: Fold decrease in IC50 value compared to corresponding IC50 in absence of mangiferin.
In contrast to the lower IC50 values in the presence of mangiferin, the trypan blue assay (Table 3) showed a decrease in the percentage of non-viable cells when treated with oxaliplatin plus mangiferin. A possible explanation for this discrepancy was that mangiferin favoured cell death as a result of apoptosis, rather than necrosis.
Table 3.
Percentage of non-viable cells (according to the trypan blue assay) with and without the addition of 10µg/ ml mangiferin.
| %Trypan positive cells | |||
| HeLa | HT29 | MCF7 | |
| 10 µM Oxaliplatin | 80.74±1.13 | 55.64±8.27 | 54.17±4.17 |
| 10 µM Oxaliplatin + manigferin | 45.69±2.59 | 42.58±3.38 | 33.54±5.73 |
Values represent mean ± average deviation, n=2
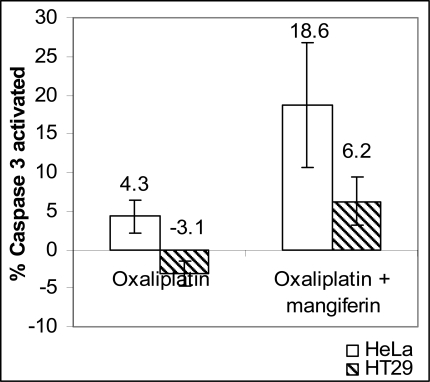
An increase in the percentage of activated caspase 3 (Figure 1), indicates that mangiferin indeed increased caspase 3 activation in combination with oxaliplatin. The MCF7 cell line does not express caspase 3 (Yang et al., 2001), therefore only HeLa and HT29 cell lines were tested for caspase 3 activities.
Figure 1.
Percentage increase in activated caspase 3 with and without addition of 10µg/ml mangiferin, relative to untreated control cells (values represent mean ± average deviation, n=2).
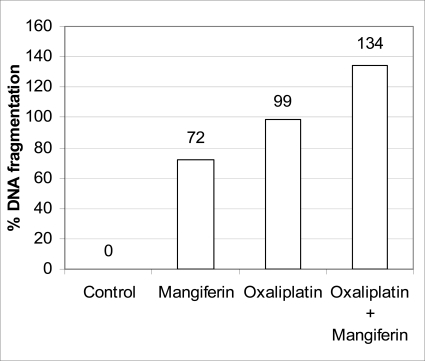
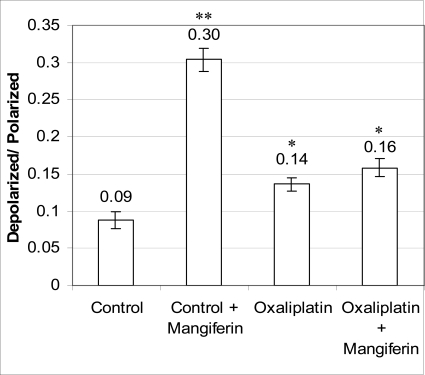
The results obtained from the DNA cell cycle analysis of HT29 cells (Table 4) indicates that mangiferin causes a delay in the S-phase in combination with oxaliplatin whereas it had no effect on its own apart from an increase in the subG1 population from 2.6 to 6.2%. The percentage apoptosis (cells in the sub-G1 peak) was further increased to 8.4% in the oxaliplatin/mangiferin combination treatment. This was also higher than the 6.4% observed in subG1 in the oxaliplatin only treatment. Similar results were obtained with MCF7 and HeLa cells (results not shown) and further experiments were performed on HT29 cells only. The DNA fragmentation assay (Figure 2) indicates that there was more DNA fragmentation in samples treated with oxaliplatin plus mangiferin than with oxaliplatin alone. From Figure 3 it is evident that both mangiferin and oxaliplatin decreased mitochondrial transmembrane potential with mangiferin having a greater effect. When added in combination, the ratio was not significantly different to that seen with oxaliplatin alone.
Table 4.
The percentage of cells in the different DNA cell cycle phases.
| Complex | %of Cells in different cell cycle phases | |||
| SubG1 | G0/G1 | S | G2/M | |
| Control | 2.6 | 43.7 | 27 | 23.4 |
| Control + mangiferin | 6.2 | 44.6 | 26.4 | 22.1 |
| Oxaliplatin | 6.4 | 40.2 | 24.8 | 26.4 |
| Oxaliplatin + mangiferin | 8.4 | 41 | 32.8 | 17.4 |
Figure 2.
Percentage increase in DNA fragmentation in HT29 cells with and without the addition of 10µg/ml mangiferin, relative to untreated control cells (bars indicate values from single experiment; a repeat of this experiment showed similar trends).
Figure 3.
Mitochondrial membrane potential, expressed as the ratio of depolarized to polarized membranes in HT29 cells with and without the addition of 10µg/ ml mangiferin (values represent mean ± standard deviation; n=3). (** p ≤ 0.001, * p ≤ 0.05 compared to control; no significant difference between Oxaliplatin and Oxaliplatin + mangiferin).
The IC50 concentrations depicted in Table 5 indicates that oxaliplatin resistant HT29 and HeLa cells had higher IC50 values than non-resistant cells and that the presence of 10µg/ ml mangiferin lowered the IC50 concentration in both nonresistant and resistant cells. MCF7 cells did not appear to develop resistance to oxaliplatin and mangiferin did not have the same sensitizing effect on this cell line as seen for HT29 and HeLa.
Table 5.
The IC50 concentrations (µM) of the platinum drugs for non-resistant (normal) as well as oxaliplatin resistant cancer cell lines, with and without the addition of 10µg/ ml mangiferin.
| Compound | Normal HeLa |
Resistant HeLa |
Normal HT29 |
Resistant HT29 |
Normal MCF7 |
Resistant MCF7 |
| Oxaliplatin | 3 | 12 | 6 | 12 | 8 | 6 |
|
Oxaliplatin and Mangiferin |
4 | 7 | 3 | 4 | 5 | 8 |
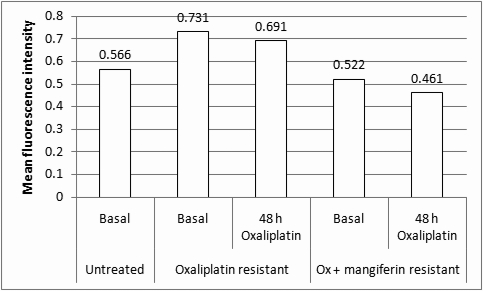
The NFκB assay (Figure 4) indicates that oxaliplatin resistant HT29 cells had a higher amount of activated NFκB than normal HT29 cells. This amount of activated NFκB was reduced to below that of normal control cells when resistance was induced in the presence of mangiferin. Therefore, mangiferin has been shown to reduce the amount of activated NFκB associated with resistant tumour cells and may prove beneficial in the prevention of resistance to platinum anticancer drugs in tumour cells.
Figure 4.
The amount of activated NF-κB (expressed as mean fluorescence intensity) in untreated and resistance-induced HT29 cells. Oxaliplatin resistance was induced as described under Materials and Methods, through intermittent, incremental exposure to Oxaliplatin (oxaliplatin resistant) or Oxaliplatin + 10 µg/ml mangiferin (ox + mangiferin resistant). These cells were finally seeded into culture flasks and levels of activated NF-κB measured in cells that received no further treatment (basal) or 10 µM Oxaliplatin for a further 48 hrs.
Normal cells treated with mangiferin alone showed an increased amount of NFκB activation, whereas treatment of normal cells with Oxaliplatin alone or in combination with mangiferin showed a similar, reduced, amount of activation. This suggests that mangiferin in combination with platinum containing complexes might have a synergistic effect and does not act as an NFκB inhibitor/ anticancer agent on its own. Although treatment of normal cells with mangiferin in combination with Oxaliplatin does not decrease the amount of activated NFκB more than when these cells are treated with Oxaliplatin alone, the 3.4 fold decrease in the IC50 concentration (Table 2) does indicate an enhanced anticancer action of this combination compared to Oxaliplatin alone. Figure 4 shows that after an additional treatment of the Oxaliplatin resistant control cells there is a slight decrease in the amount of NFκB activated, but this amount is decreased to a value even lower than that of normal control cells when Oxaliplatin and mangiferin resistant control cells are treated with Oxaliplatin. These results indicate that mangiferin in combination with Oxaliplatin acts as an NFκB inhibitor. It has been shown previously that the development of anti-cancer drugs that can “switch” the function of NFκB from anti-apoptotic to pro-apoptotic may prove to be beneficial in the fight against cancer and that tumour prevention may be achieved through inhibition of abnormally active NFκB (Perkins, 2000; Perkins, 2004).
Cisplatin showed great promise in the treatment of cancer, however, due to the numerous toxic side effects and the emergence of cisplatin resistant cell lines, drugs with less toxic side effects, improved cytotoxicity against cancer cells and activity against cisplatin resistant cell lines are urgently needed. Sarkar et al. (Sarkar et al., 2004) showed that mangiferin enhanced cell death caused by various apoptotic agents, including cisplatin. Mangiferin is a natural polyphenol found in Cyclopia spp., Canscora decussata (Bhattacharya et al., 1972) and Mangifera indica (Muruganandan et al., 2005). Although some controversy still exists, Honeybush tea (Cyclopia spp.), which is a rich source of antioxidants, is sometimes used in conjunction with chemotherapy to reduce the side-effects (Drisko et al., 2003a, b; Lawenda et al., 2008). This study was therefore done to determine whether mangiferin could enhance the in vitro anticancer activity of oxaliplatin.
The decreased IC50 values for oxaliplatin when combined with 10 µg/ml mangiferin (Table 2) were very promising. Furthermore, the fact that the highest fold decrease occurred in the HT29 cells treated with oxaliplatin in combination with mangiferin is very significant, since oxaliplatin is clinically used to treat colon cancer (Martin et al., 2000). A decrease in the percentage of non-viable cells was observed in the trypan blue assay (Table 3). Trypan blue stains dead/necrotic cells with “leaky” cell membranes, hence a decrease in the percentage of non-viable cells from this assay indicates less necrosis has taken place. These results therefore show strong evidence that mangiferin favours apoptotic cell death instead of necrosis.
Caspases (cysteine aspartic acid-specific proteases) play key roles in apoptosis of mammalian cells. The fact that an increase in the caspase 3 activity (Figure 1) was observed during combination treatment with oxaliplatin and mangiferin in both HeLa and HT29 cells indicates that the decreased IC50 values may be due to increased apoptosis.
The results obtained from the DNA cell cycle analysis (Table 4) shows a slight increase in G2/M-phase in oxaliplatin treated cells. Fujie et al. (Fujie et al., 2005) also showed that oxaliplatin causes an S or G2M phase delay in the cell cycle of HT29 cells. Although mangiferin alone did not induce cell cycle arrest, the presence of mangiferin in combination with oxaliplatin shows a delay in the S-phase. The percentage of apoptotic cells were also increased in the cells subjected to a combination treatment. The Sub-G1 phase refers evidence for apoptosis. Apoptotic cells can be seen to the left of the G0/G1 peak due to DNA fragmentation occurring during apoptosis, DNA is lost from the permeabilized cells thus rendering these cells with less DNA (Kwon et al., 2005). This increased apoptosis was verified by a DNA fragmentation assay (Figure 2) that showed an increase in the amount of DNA fragmentation in HT29 cells subjected to a combination treatment in contrast to cells treated with oxaliplatin alone.
The health and bioenergetic function of the mitochondria depend on its membrane potential (ΔΨm). The preservation of ΔΨm is essential during normal conditions and, especially, during conditions of stress and disease. Depolarization of the membrane results in a reduction of ATP production and is also thought to precipitate the release of pro-apoptotic factors in some cell systems; hence there are good reasons to search for therapeutic agents to decrease ΔΨm as possible pro-apoptotic drugs, for example, in the case of cancer (Wong and Cortopassi, 2002). Both mangiferin and oxaliplatin treatment caused a significant reduction in mitochondrial membrane potential (Figure 3). Therefore the apoptosis observed in the subG1 peak of the cell cycle analysis (Table 4) and the increase in DNA fragmentation was induced through a mitochondrial pathway. In combination, there was no significant increase in mitochondrial depolarization above that of oxaliplatin alone.
NFκB is a transcription factor that exerts anti-apoptotic effects and is often activated in cancer cells in response to chemotherapeutic agents. This promotes cancer therapy resistance in tumours (Baldwin, 2001). The improper activation of NFκB in diseases such as tumorigenesis (Paul et al., 2006; Lee et al., 2008) has been linked to TNFα and other members of its superfamily. Through the activation of NFκB, TNFα induces the expression of various genes that can be involved in tissue invasion and metastasis. In addition, activation of NFκB can suppress apoptosis, which is likely to enhance tumorigenesis. Many natural compounds, including the phenolics, have been found to inhibit upstream signaling molecules that are involved in TNFα expression (Paul et al., 2006). Leiro et al. 2004 (Leiro et al., 2004) illustrated that mangiferin modulates the expression of a large number of genes that are critical for the regulation of apoptosis and tumorigenesis, and raised the possibility that it may be of value in the treatment of cancer.
Mabuchi et al. (Mabuchi et al., 2004) showed that combination therapy of cisplatin with an NFκB inhibitor would increase the therapeutic efficacy of cisplatin. Our results indicate that mangiferin is an NFκB inhibitor and that it increases the therapeutic efficacy of oxaliplatin (Table 2). Furthermore, we have shown evidence that mangiferin may counteract the development of resistance to oxaliplatin in HT29 colon cancer cells by reducing active NFκB levels (Figures 4).
Conclusion
The results obtained in this study indicate that mangiferin might be used as a combination therapy with platinum anticancer drugs in order to increase the efficacy of these drugs as well as counteract the development of drug-resistant cells. Unfortunately no published literature could be found to indicate how much mangiferin is present in a cup of tea such as Honeybush, nor how much mangiferin is absorbed through the gastro-intestinal tract. Such information would assist in extrapolating our in vitro results to the in vivo situation. Recent findings also point to a link between Stat 3 and NFκB activation and signaling pathways (Nadiminty et al., 2006; Lee et al., 2008) and it has been illustrated that a more effective strategy might be the simultaneous inhibition of both Stat3 and NFκB, rather than individually. Therefore we suggest that the effect of mangiferin on Stat3 activation should also be investigated in future.
Acknowledgements
The authors would like to thank Shimoda Biotech Pty (Ltd) for their continual support provided during this study.
References
- 1.Baldwin AS. Control of oncogenesis and cancer therapy resistance by the transcription factor NF-kappaB. Journal of Clinical Investigation. 2001;107:241–246. doi: 10.1172/JCI11991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bhattacharya SK, Sanyal AK, Ghosal S. Monoamine oxidase-inhibiting activity of mangiferin isolated from Canscora decussate. Naturwissenschaften. 1972;59:651. doi: 10.1007/BF00609562. [DOI] [PubMed] [Google Scholar]
- 3.Drisko JA, Chapman J, Hunter VJ. The use of antioxidants with first-line chemotherapy in two cases of ovarian cancer. Journal of the American College of Nutrition. 2003a;22:118–123. doi: 10.1080/07315724.2003.10719284. [DOI] [PubMed] [Google Scholar]
- 4.Drisko JA, Chapman J, Hunter VJ. The use of antioxidant therapies during chemotherapy. Gynecol Oncol. 2003b;88:434–439. doi: 10.1016/s0090-8258(02)00067-7. [DOI] [PubMed] [Google Scholar]
- 5.Duncan AC, Jager AK, van Staden J. Screening of Zulu medicinal plants for angiotensin converting enzyme (ACE) inhibitors. Journal of Ethnopharmacology. 1999;68:63–70. doi: 10.1016/s0378-8741(99)00097-5. [DOI] [PubMed] [Google Scholar]
- 6.Fujie Y, Yamamoto H, Ngan CY, Takagi A, Hayashi T, Suzuki R, Ezumi K, Takemasa I, Ikeda M, Sekimoto M, Matsuura N, Monden M. Oxaliplatin, a Potent Inhibitor of Survivin, Enhances Paclitaxel-induced Apoptosis and Mitotic Catastrophe in Colon Cancer Cells. Japanese Journal of Clinical Oncology. 2005;35:453–463. doi: 10.1093/jjco/hyi130. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez VM, Fuertes MA, Alonso C, Perez JM. Is Cisplatin-Induced Cell Death Always Produced by Apoptosis. Molecular Pharmacology. 2001;59:657–663. doi: 10.1124/mol.59.4.657. [DOI] [PubMed] [Google Scholar]
- 8.Kwon HJ, Hong YK, Kim KH, Han CH, Cho SH, Choi JS, Byung-Woo K. Methanolic extracts of Pterocarpus santalinus induces apoptisis in HeLa cells. Journal of Ethnopharmacology. 2005;105:229–234. doi: 10.1016/j.jep.2005.10.025. [DOI] [PubMed] [Google Scholar]
- 9.Lawenda BD, Kelly KM, Ladas EJ, Sagar SM, Vickers A, Blumberg JB. Should supplemental antioxidant administration be avoided during chemotherapy and radiation therapy? Journal of the national cancer institute. 2008;100:773–783. doi: 10.1093/jnci/djn148. [DOI] [PubMed] [Google Scholar]
- 10.Lee TL, Yeh J, Friedman J, Yan B, Yang X, Yeh NT, van Waes C, Chen Z. A signal network involving coactivated NF-kappaB and STAT3 and altered p53 modulates BAX/BCL-XL expression and promotes cell survival of head and neck squamous cell carcinomas. International Journal of Cancer. 2008;122:1987–1998. doi: 10.1002/ijc.23324. [DOI] [PubMed] [Google Scholar]
- 11.Leiro J, Arranza JA, Yanez M, Ubeira FM, Sanmartn ML, Orallo F. Expression profiles of genes involved in the mouse nuclear factor-kappa B signal transduction pathway are modulated by mangiferin. International Immunopharmacology. 2004;4:763–778. doi: 10.1016/j.intimp.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Mabuchi S, Ohmichi M, Nishio Y, Hayasaka T, Kimura A, Ohta T, Saito M, Kawagoe J, Takahashi K, Yada-Hashimoto N, Sakata M, Motoyama T, Kurachi H, Tasaka K, Murata Y. Inhibition of NFkB increases the efficacy of Cisplatin in in vitro and in vivo ovarian cancer models. The Journal of Biological Chemistry. 2004;10:1–39. doi: 10.1074/jbc.M313709200. [DOI] [PubMed] [Google Scholar]
- 13.Marnewick J, Gelderblom WCA, Joubert E. An investigation on the antimutagenic properties of South African herbal teas. Mutation Research. 2000;471:157–166. doi: 10.1016/s1383-5718(00)00128-5. [DOI] [PubMed] [Google Scholar]
- 14.Marnewick JL, Batenburg W, Swart P, Joubert E, Swanevelder S, Swart P, Gelderblom WCA. Ex vivo modulation of chemical-induced mutagenesis by subcellular liver fractions of rats treated with rooibos (Aspalathus linearis) tea, honeybush (Cyclopia intermedia) tea, as well as green and black (Camellia sinensis) teas. Mutation Research. 2004;558:145–154. doi: 10.1016/j.mrgentox.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Marnewick J, Joubert E, Josepha S, Swanevelder S, Swart P, Gelderblom W. Inhibition of tumour promotion in mouse skin by extracts of rooibos (Aspalathus linearis) and honeybush (Cyclopia intermedia), unique South African herbal teas. Cancer Letters. 2005;224:193–202. doi: 10.1016/j.canlet.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 16.Martin AG, Lockwood GF, Greenslade D, Brienza S, Bayssas M, Gamelin E. Clinical Pharmacokinetics of Oxaliplatin: A Critical Review. Clinical Cancer Research. 2000;6:1205–1218. [PubMed] [Google Scholar]
- 17.Muruganandan S, Srinivasan K, Gupta S, Gupta PK, Lal J. Effect of mangiferin on hyperglycemia and atherogenicity in streptozotocin diabetic rats. Journal of Ethnopharmacology. 2005;97:497–501. doi: 10.1016/j.jep.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 18.Nadiminty N, Lou W, Lee SO, Lin X, Trump DL, Gao AC. Stat3 activation of NF-κB p100 processing involves CBP/ p300-mediated acetylation. PNAS. 2006;103:7264–7269. doi: 10.1073/pnas.0509808103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parker SH, Tong T, Bolden S, Wingo PA. Cancer Statistics, 1997. CA Cancer J Clin. 1997;47:5–27. doi: 10.3322/canjclin.47.1.5. [DOI] [PubMed] [Google Scholar]
- 20.Paul AT, Gohil VM, Bhutani KK. Modulating TNF-α signaling with natural products. Drug Discovery Today. 2006;11:725–732. doi: 10.1016/j.drudis.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Perkins N D. The Rel/NF-kB family: friend and foe. TIBS. 2000;25:434–440. doi: 10.1016/s0968-0004(00)01617-0. [DOI] [PubMed] [Google Scholar]
- 22.Perkins N D. NF-kB: tumor promoter or suppressor? TRENDS in Cell Biology. 2004;14:64–69. doi: 10.1016/j.tcb.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Sadler PJ, Guo Z. Metal complexes in medicine: Design and mechanism of action. Pure and Applied Chemistry. 1998;70:863–971. [Google Scholar]
- 24.Sarkar A, Sreenivasan Y, Ramesh GT, Manna SK. β-D-Glucoside Suppresses Tumor Necrosis Factor-induced Activation of Nuclear Transcription Factor κB but Potentiates Apoptosis. Journal of Biological Chemistry. 2004;279:33768–33781. doi: 10.1074/jbc.M403424200. [DOI] [PubMed] [Google Scholar]
- 25.Sergent C, Franco N, Chapusot C, Lizard-Nacol S, Isambert N, Correia M, Chauffert B. Human colon cancer cells surviving high doses of cisplatin or oxaliplatin in vitro are not defective in DNA mismatch repair proteins. Cancer Chemotherapy Pharmacology. 2002;49:445–452. doi: 10.1007/s00280-002-0450-6. [DOI] [PubMed] [Google Scholar]
- 26.Walker EM, Walker SM. Evolution of chemotherapy with platinum compounds. Annals of Clinical and Laboratory Science. 1999;29:263–274. [PubMed] [Google Scholar]
- 27.Wong A, Cortopassi JA. High-throughput measurement of mitochondrial membrane potential in a neural cell line using a fluorescence plate reader. Biochemical and Biophysical Research Communications. 2002;298:750–754. doi: 10.1016/s0006-291x(02)02546-9. [DOI] [PubMed] [Google Scholar]
- 28.Yang X, Sladek TL, Liu X, Butler BR, Froelich CJ, Thor AD. Reconstitution of Caspase 3 Sensitizes MCF-7 Breast Cancer Cells to Doxorubicin- and Etoposide-induced Apoptosis. Cancer Research. 2001;61:348–354. [PubMed] [Google Scholar]