Abstract
BACKGROUND:
We carried out this study to compare the efficacy of oral gabapentin and clonidine premedication for controlling the pressor responses to laryngoscopy and tracheal intubation.
METHODS:
In this double-blind clinical trial, ninety-six patients were randomly allocated to one of three groups according to the agents to be used before the induction of anaesthesia: Group P (n = 32) received oral placebo, Group G (n = 32) received 800 mg of gabapentin, and Group C (n = 32) received 0.3 mg of clonidine 90 minutes prior to surgery. Systolic arterial pressure (SAP), diastolic arterial pressure (DAP), mean arterial pressure (MAP), heart rate (HR) and rate pressure product (RPP) were measured at baseline (3 min before induction), just before laryngoscopy, and postintubation (at 1, 3, 5, 10 and 15 min after starting laryngoscopy). Statistical analysis of data was done with repeated measure ANOVA and chi-square test.
RESULTS:
HR and RPP significantly decreased in Group G and Group C at 5, 10, and 15 minutes after tracheal intubation compared with those just before laryngoscopy (p < 0.05). No significant difference was noted between Group G and Group C considering these variables. SAP, DAP, MAP and RPP at 1, 3, 5, 10, and 15 minutes after intubation were significantly lower in Group G compared with Group P (p < 0.05). There was no significant difference between Group C and Group P in this regard.
CONCLUSIONS:
The present study demonstrated that premedication with oral gabapentin 800 mg or clonidine 0.3 mg similarly blunted the hyperdynamic response after laryngoscopy and intubation.
KEYWORDS: Premedication, oral gabapentin, oral clonidine, pressor response, laryngoscopy, intubation
Induction of anesthesia and tracheal intubation may cause profound alteration of the hemodynamic state of the patient consequent to both the effects of anesthetic drug administered perioperatively and the adrenergic state of the patient.1
Tracheal intubation induces clinically significant neurovegetative responses.2 Plasma concentration of catecholamines is increased2 and there may be associated myocardial ischemia3 and cerebral hemorrhage.4
A large array of pharmacological agents was used to attenuate the hemodynamic responses to the laryngoscopy and tracheal intubation.5
Gabapentin, a structural analogue of γ-aminobutyric acid, is used as an anticonvulsant drug.6 Pretreatment with gabapentin can prevent the development of hyperalgesia.7 Also, gabapentin has a selective effect on the nociceptive process relating central sensitization.8
Memis and colleagues9 showed that oral administration of gabapentin 800 mg one hour before induction of anaesthesia can attenuate the pressor response to the laryngoscopy and tracheal intubation.
Also, Nishikawa et al10 showed that clonidine 4 μg/kg, a direct-acting α2 adrenergic agonist, could attenuate blunted catecholamine release and the pressor responses following laryngoscopy and tracheal intubation.
Remifentanyl, a short acting opioid, can attenuate the pressor response to the laryngoscopy but it causes bradycardia and hypotension. Also, it needs continuous infusion for providing it's effect. Remifentanyl is an expensive drug. These disadvantages are not accompanied when using clonidine or gabapentin.9,10
Few data are available comparing the efficacy of gabapentin or clonidine in controlling hemodynamic response throughout the periintubation period. We therefore, conducted this randomized double blind clinical trial study to compare any possible blunting cardiovascular effects of laryngoscopy and tracheal intubation by the use of 800 mg gabapentin or 0.3 mg clonidine in comparison with groups that didn’t receive any of two drugs.
Methods
After obtaining Institutional Ethics Committee approval and written informed consent from all the patients, ninety-six ASA I and II consequent patients, aged 18-65 years, scheduled for elective surgery under general anaesthesia requiring tracheal intubation, were included in this study. The other inclusion criteria covered patients without receiving any drugs that could influence hemodynamic and autonomic function, patients with no difficult airways or obesity (body weight > 100 kg), no allergy or contraindications to anaesthetics or any drug used, no hypovolemia, no electrocardiographic abnormalities, no congestive heart failure, no diabetes mellitus, no hypertension, no coronary artery, respiratory, renal, cerebral diseases, and no pregnancy. If there was profuse change in the technique of anesthesia, the patients were excluded from the study. The study was carried out in Alzahra Hospital of Isfahn University of Medical Sciences throughout 2008-2010.
According to earlier study,9 a sample-size approximation pointed out that 32 patients per group would provide a power of 80% at a level of 0.05 for identifying 30% attenuation in the post-intubation increase in heart rate.
The patients were randomly allocated to one of three groups according to the agents to be used before the induction of anaesthesia: Control group received oral placebo (n = 32, Group P), patients who received 800 mg of gabapentin (n = 32, Group G), and those patients who received 0.3 mg of clonidine (n = 32, Group C) 90 minutes prior to surgery.
The study drugs containing placebo, gabapentin, and clonidine were prepared in a double blind fashion, by a collaborator not involved in data recording and an appropriate code number was assigned. The same collaborator administered drugs while a blind observer collected data.
The randomization result concealed until after the patient had provided written consent. Also, the investigators obtaining consent were blind to the randomization.
No premedication was given. If there was any side effect (such as bradycardia, hypotension, nausea and vomiting, respiratory depression, dizziness, somnolence, peripheral oedema and headache) it was recorded.
In the operating room, an 18 G intravenous cannula was inserted in an appropriate antecubital vein and ringer's solution was started, at 10 ml/kg per h throughout the study period. Monitoring included an automated BP cuff, electrocardiography, and pulse oximetry. Systolic arterial pressure (SAP), diastolic arterial pressure (DAP), mean arterial pressure (MAP), heart rate (HR) and rate pressure product (RPP) at pre-induction time were measured as baseline values.
After preoxygenation, anaesthesia was induced with thiopental 5 mg/kg, fentanyl 3 μg/kg and atracurium 0.5 mg/kg. Patients’ lungs were manually ventilated with 100% oxygen before orotracheal intubation was performed. Direct laryngoscopy was performed 3 minutes after loss of verbal contact by using a Macintosh 3 laryngoscope blade and tracheal intubation was accomplished within 15 s. The patients’ lungs were then mechanically ventilated with a tidal volume of 10 ml/kg and a respiratory rate of 12/min to maintain endtidal PaCO2 at around 38 mmHg. Anesthesia was maintained with propofol 150 μg/kg with a fresh gas flow of 4 L/min (50% N2O in O2).
In each patient, the BP (SAP, DAP, MAP), and HR were measured at three time-points: baseline (3 min before induction), just before laryngoscopy, and postintubation (at 1, 3, 5, 10 and 15 min after starting laryngoscopy) by an independent investigator unaware of the group assignment. The rate pressure product was computed by multiplying the systolic blood pressure by the heart rate. The incidences of BP and HR percent changes more than 20% of baseline values during the observation were also recorded.
Hypertension was defined as a MAP more than 30% of a patient's baseline value, or 130 mm Hg, whichever was greater. Hypotension was defined as a MAP less than 70% of a patient's baseline value, or 65 mm Hg, whichever was less. Tachycardia and bradycardia were defined as a HR greater than 120 bpm and < 60 bpm, respectively. The incidence of hypertension, hypotension, tachycardia, and bradycardia was recorded during the study period and compared among the three groups. The incidence of dysrhythmia after intubation was also compared among the three groups.
A dysrhythmia was defined as any ventricular or supraventricular premature beat or any sustained rhythm other than sinus. Ephedrine (3 mg increments) was administered for hypotension and atropine, in 300 μg increments, for bradycardia.
Following termination of surgery, the remaining neuromuscular blockade was reversed with neostigmine 0.04 mg/kg and atropine 0.02 mg/kg.
Duration of anaesthesia (the time from induction of anaesthesia till extubation), and duration of post-anaesthesia care unit (PACU) stay based on PACU discharge criteria (awake, haemodynamically stable, able to maintain a patent airway without assistance, protective reflexes intact, comfortable and free of persistent bleeding) were also recorded.
Hemodynamic responses to induction and intubation in a given group were analyzed using a repeated-measurements ANOVA (one-way ANOVA) followed by a paired t-test with Bonferroni's correction. Chi-squared test or Fisher's exact test, when proper, was utilized for analysis of categorical data. Continuous variables are presented as mean ± SD. A value of P < 0.05 was considered the minimum level of statistical significance. Statistical analysis was performed using SPSS version 16.0.
Results
One-hundred forty patients completed the study criteria for randomization. Twelve patients dropped out of the study (see CONSORT Statement, Figure 1).
Figure 1.
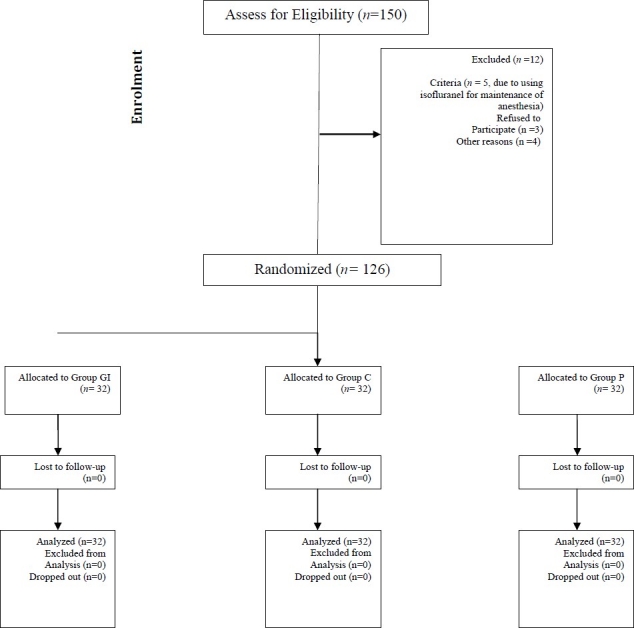
Flow diagram of the progress through the phases of the randomised trial. Group G = gabapentin, Group C = clonidine, Group P = placebo.
Demographic characteristics, duration of anesthesia, surgery and PACU stay were similar in the three groups (Table 1). The preoperative mean arterial pressure, heart rate and RPP values were similar in the three groups (Figure 2–4).
Table 1.
Demographic characteristics, duration of anesthesia, surgery and PACU stay in the three groups
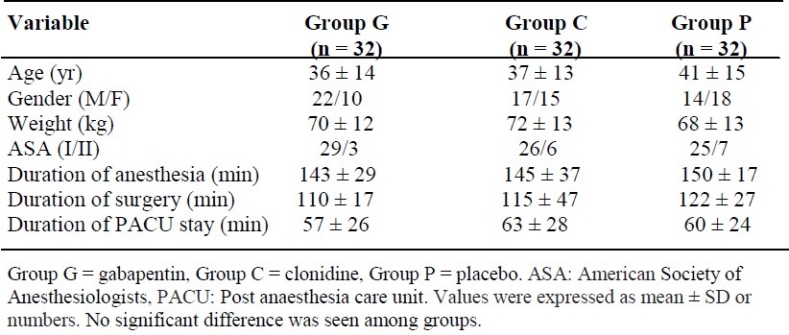
Figure 2.
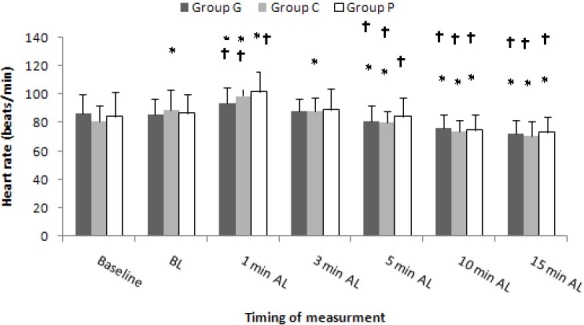
The heart rate changes during intubation period in the three groups. Data are mean ± SD. Group G = gabapentin, Group C = clonidine, Group P = placebo. BL = before laryngoscopy, AL = after laryngoscopy. * p < 0.05 vs. baseline; † p < 0.05 vs. BL
Figure 4.
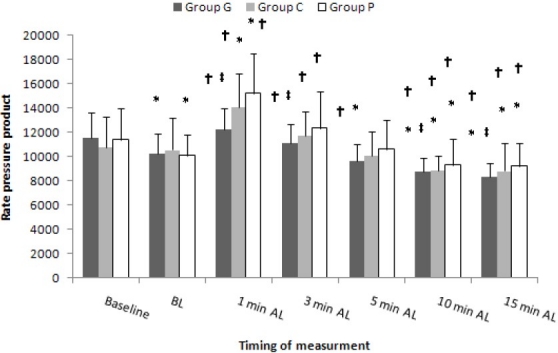
The rate pressure product changes during intubation period in the three groups. Data are mean ± SD. Group G = gabapentin, Group C = clonidine, Group P = placebo. BL = before laryngoscopy, AL = after laryngoscopy. ‡ p < 0.05 vs. Group P; * p < 0.05 = P vs. baseline; † p < 0.05 vs. BL.
After induction of anesthesia, HR increased in Group C and Group P but it was significant in Group C (Figure 2). The increase in HR was not significant in Group G.
Systolic, diastolic and mean arterial blood pressure (Figure 3) decreased significantly in all three groups compared with baseline values. RPP decreased significantly in Group G (Figure 4). BP, HR and RPP changes after induction of anaesthesia and before laryngoscopy were not significantly different among the three groups.
Figure 3.
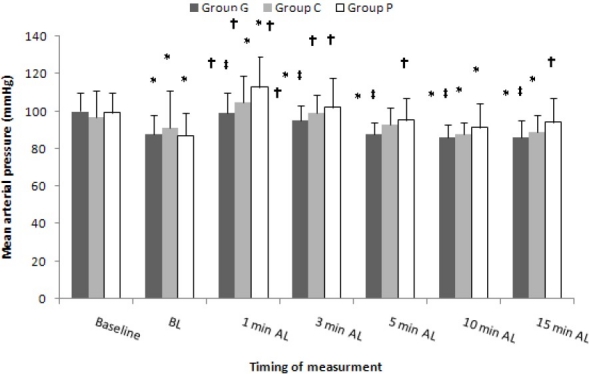
The mean arterial pressure changes during intubation period in the three groups. Data are mean ± SD. Group G = gabapentin, Group C = clonidine, Group P = placebo. BL = before laryngoscopy, AL = after laryngoscopy. ‡ p < 0.05 vs. Group P; * p < 0.05 = P vs. baseline; † p < 0.05 vs. BL.
Changes in arterial pressures, HR, and RPP were greatest 1 min after intubation. Increase in HR was less in Group G and Group C compared with Group P (Figure 2). HR, BP and RPP significantly decreased at 5, 10, and 15 minutes after intubation in Group G and Group C compared with the baseline values.
HR and RPP significantly decreased in Group G and Group C at 5, 10, and 15 minutes after tracheal intubation compared with those just before laryngoscopy (Figure 2, 4). SAP, DAP, MAP and RPP at 1, 3, 5, 10, and 15 minutes after intubation were significantly lower in Group G compared with Group P. There was no significant difference between Group C and Group P in this regard.
The incidence of HR, SAP, DAP, and MAP percent increases ≥ 20% of baseline values were significantly lower in Group G compared with Group P (p < 0.05). There was no case of bradycardia or hypotension among three groups. No ST segment depression or other electrocardiogram changes was noted in either group.
Discussion
The present study compared the efficacy of oral gabapentin 800 mg and clonidine 0.3 mg administered 90 minutes prior to surgery for controlling cardiovascular responses to laryngoscopy and tracheal intubation. The results of our study showed that comparable with clonidine, gabapentin significantly reduced DAP, SAP, MAP, and RPP changes for 15 min after endotracheal intubation. Compared with placebo, the incidence of HR, SAP, DAP, and MAP percent increase ≥ 20% of baseline values were significantly lower in Group G. This conclusion is not true about clonidine. There were no cases of bradycardia, tachycardia, arrhythmias, ST segment or other ECG changes noted throughout the study.
Direct laryngoscopy and endotracheal intubation lead to increasing blood pressure and heart rate.11 Mechanism of cardiovascular response to intubation is considered to be a reflex sympathetic response to the mechanical stimulation of larynx and trachea. Significant increase in serum levels of norepinephrine and epinephrine subsequent to laryngoscopy with and without tracheal intubation have been described.2,12,13
Various anesthetic methods and drugs are used for controlling the hemodynamic response to the laryngoscopy and intubation. The technique or drug of choice depends on the necessity and duration of operation, choice of anesthetic technique, rout of administration, and medical condition of the patient.14,15
Memiş and colleagues9 showed that oral administration of gabapentin 800 mg but not 400 mg given 1 h before operation blunted the arterial pressure and HR increase in the first 10 min after endotracheal intubation.
In animal models of nociception, gabapentin decreases hypersensitivity associated with nerve injury, inflammation, and pain after surgery.8,16–20
Gabapentin augmented the analgesic effect of morphine in healthy volunteers22 and its combination in patients experiencing neuropathic cancer pain showed better analgesia in comparison with morphine alone.23
Pretreatment with a single dose of gabapentin prevented dose-dependent development of hyperalgesia (which is NMDA-mediated) and tactile allodynia (which is AMPA- and metabotropic receptor-mediated).24
Gabapentin does not interact with other frequently prescribed drugs.25 The most common adverse effects of gabapentin are somnolence (20%), ataxia (13%), fatigue (11%), and dizziness (8%). The other complications are nystagmus, headache, diplopia, tremor, and nausea, each one fewer than 10%.26
There was no difference among our three groups in these side effects all through the study period. Fassoulaki et al.27 showed that pretreatment with gabapentin 1600 mg at 6 hourly intervals starting the day (noon) before surgery attenuates the pressor response to laryngoscopy and intubation of the trachea. They emphasized that gabapentin had no effect on the changes in HR. They induced anaesthesia with propofol, which produces bradycardia. Therefore, tachycardia resulting from intubation may have been attenuated by propofol in both groups concealing such a possible effect of gabapentin on the HR. In addition, propofol produces hypotension more than thiopental and bradycardia, which may compensate in part the cardiovascular changes attributable to laryngoscopy and tracheal intubation.
In our study, gabapentin also had no effect on the changes in HR. We used thiopental for induction of anaesthesia. Tsuchiya and colleagues[28] showed that induction of anaesthesia with thiopental increased heart rate due to reducing cardiac parasympathetic tone. It is possible that tachycardia induced by thiopental inhibited the beneficial effect of gabapentin on HR. This is also in agreement with Kaya et al.[29] study that reported gabapentin blocked the increase in the MAP but not the HR associated with tracheal intubation.
In our study none of the patients had hypotension before induction of anaesthesia. Also, none of the patients in the Group G or Group C exhibited severe hypotension compared with the control group. Consistent with our study protocol during the induction period, we should administer ephedrine if SAP remained less than 80 mm Hg 1 min after intubation. Nonetheless, none of our patients needed active treatment for hypotension during the study period. These data documented the safety of gabapentin administration.
The mechanism by which gabapentin attenuates the pressor response to laryngoscopy and intubation is unidentified. The drug inhibits membrane voltage-gated calcium channels, therefore acting in a manner like calcium channel blockers.30
The effect of clonidine on attenuation of pressor response to the laryngoscopy and tracheal intubation has been reported previously by many studies.31 Previous investigations showed that a dose of 300-μg clonidine orally or larger decreases sympathetic activity.32 The Matot et al.31 study shows that, in patients undergoing laryngoscopic or bronchoscopic procedures under general anesthesia, premedication with oral clonidine (4–4.5 μg/kg) attenuates hemodynamic responses. In our study, premedication with clonidine 0.3 mg administered 90 minutes prior to surgery significantly reduced HR, DAP, SAP, MAP, and RPP changes for 15 min after endotracheal intubation.
Our data confirmed the results of above studies who demonstrated clonidine to be beneficial in blunting reflex tachycardia and hypertensive responses associated with intubation. The risk of undesirable side effects is very important in evaluating the overall safety of preanesthetic medication. The potentially beneficial effect of α2 agonists may be counteracted by bradycardia33 and hypotension.34
Our data showed that hypotension may be expected. This hypotensive effect has been described in other investigations in which clonidine was used either in its IV form34 or as an oral dose of 4 or 5 mg/kg.34 In our study, nevertheless, hypotension occurred only during the induction of anaesthesia and might be related to thiopental used.
This finding is in agreement with a previous study35 in elderly patients undertaking ophthalmic surgery under local anaesthesia, in which 30% of the patients pre-medicated with 300 μg clonidine, but no patient in the other groups (150 μg clonidine or placebo), were treated at least once for hypotension. Other author36 has also described severe hypotensive episodes in at least 10% of patients pre-medicated with 300 μg of clonidine. The above mentioned studies together with the results of our study advocate caution in the use of clonidine 300 mg as a general premedicant.
We prefered a dose of 4 μg/kg clonidine in the present study because previous studies showed that administration of 4 μg/kg clonidine blunted catecholamine release during intubation and surgery and that larger clonidine doses were not more effective.37 Smaller doses, nevertheless, were not adequate to blunt the reaction to laryngoscopy. Additionally, the maximum dose of clonidine is limited by its action on peripheral α-adrenoceptors. Larger doses might cause peripheral α stimulation, which could result in an increase in blood pressure. In most human researches, 4 μg/kg clonidine was applied without signs of peripheral α stimulation.
Some mechanisms by which clonidine blunt the heart rate and blood pressure response to instrumentation of the airway have been proposed. Activation of central α2-adrenoceptors, which causes both a decrease in peripheral sympathetic tone and an increase in vagally induced reflex bradycardia,37 and stimulation of peripheral presynaptic α-adrenoceptors, which leads to diminished release of norepinephrine from the nerve endings toward the vasculature and to a reduction in peripheral sympathetic tone, are amongst probable explanations.
We did not quantify stress mediators such as endogenous plasma catecholamines or cortisone, and we did not score sedation. These can be regarded as limitations of our study. Although measurements of endogenous catecholamines would give valuable information, scoring sedation prior to induction of anaesthesia would impede with the double blinding of the study. We studied patients up to 65 yr as elderly patients take more often drugs such as antidepressants, hypnotics and antihypertensives. Older patients also demonstrate increased sensitivity to drugs38 and the cardiovascular effects of gabapentin were not investigated extensively. Aged patients should in-clude a different group with doses of gabapentin probably adjusted to age. Accordingly, its optimal dosing and side effects for the older population require more study before planning a similar study.
We decided to use a deviation of 30% for MAP or 20%for HR based on the results of Memis et al. study9 which showed gabapentin administration caused attenuation of at least 20% in HR and 25-30% in MAP increase one minute after laryngoscopy. So, it seems that sample size determination was relatively accurate in our study.
The advantages of using gabapentin or clonidine premedication for attenuation of cardiovascular responses to the laryngoscopy are easy administration, no significant side effects, and availability with low price. Also, both drugs have antinociceptive effects that may be beneficial for controlling post-operating pain. Remifentanil is expensive and has adverse effects such as bradycardia and hypotension that inhibits its use in hemodynamic compromised patients. Esmolol needs infusion pump for administration and it is not available always everywhere. Labetolol is an appropriate drug for this purpose but it is not available everywhere.
In conclusion, our study showed that oral gabapentin 800 mg or clonidine 0.3 mg, given 1 h before operation, comparably blunted the pressor response to laryngoscopy and endotracheal intubation. More studies focusing on their cardiovascular effects and their effect on stress mediators especially in elderly are needed. Also, it is recommended that the attenuating cardiovascular effects of gabapentin after intubation be compared with the newer α2- adrenoreceptor, dexmedetomidine.
Authors’ Contributions
KM has planned the study and finalized it; PK has planned the study and finalized it too; AH and MRS did the statistical analysis and prepared the first version of manuscript and revised final version for publish; AH has planned the study and finalized study. All authors read and approved the final manuscript.
Acknowledgments
The authors wish to sincerely thank the support of all the staff of Isfahan Nursing and all the colleagues in Alzahra Hospital Medical Center affiliate to Isfahan University of Medical Sciences in Isfahan, Iran. Furthermore, our special thanks go to the patients, who wholeheartedly and actively assisted us to carry out this research. No conflict of interest existed. Research project number is 386155. This randomized prospective double blind clinical trial was approved by the Ethics Committee of Isfahan University of Medical Sciences and all patients gave written informed consent.
Footnotes
Conflict of Interests Authors has no conflict of interests.
References
- 1.Iannuzzi E, Iannuzzi M, Cirillo V, Viola G, Parisi R, Cerulli A, et al. Peri-intubation cardiovascular response during low dose remifentanil or sufentanil administration in association with propofol TCI.A double blind comparison. Minerva Anestesiol. 2004;70(3):109–15. [PubMed] [Google Scholar]
- 2.Russell WJ, Morris RG, Frewin DB, Drew SE. Changes in plasma catecholamine concentrations during endotracheal intubation. Br J Anaesth. 1981;53(8):837–9. doi: 10.1093/bja/53.8.837. [DOI] [PubMed] [Google Scholar]
- 3.Edwards ND, Alford AM, Dobson PM, Peacock JE, Reilly CS. Myocardial ischaemia during tracheal intubation and extubation. Br J Anaesth. 1994;73(4):537–9. doi: 10.1093/bja/73.4.537. [DOI] [PubMed] [Google Scholar]
- 4.Fox EJ, Sklar GS, Hill CH, Villanueva R, King BD. Complications related to the pressor response to endotracheal intubation. Anesthesiology. 1977;47(6):524–5. doi: 10.1097/00000542-197712000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Lunn JK, Stanley TH, Eisele J, Webster L, Woodward A. High dose fentanyl anesthesia for coronary artery surgery: plasma fentanyl concentrations and influence of nitrous oxide on cardiovascular responses. Anesth Analg. 1979;58(5):390–5. [PubMed] [Google Scholar]
- 6.Backonja M, Beydoun A, Edwards KR, Schwartz SL, Fonseca V, Hes M, et al. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA. 1998;280(21):1831–6. doi: 10.1001/jama.280.21.1831. [DOI] [PubMed] [Google Scholar]
- 7.Mellick GA, Mellick LB. Reflex sympathetic dystrophy treated with gabapentin. Arch Phys Med Rehabil. 1997;78(1):98–105. doi: 10.1016/s0003-9993(97)90020-4. [DOI] [PubMed] [Google Scholar]
- 8.Dirks J, Moiniche S, Hilsted KL, Dahl JB. Mechanisms of postoperative pain: clinical indications for a contribution of central neuronal sensitization. Anesthesiology. 2002;97(6):1591–6. doi: 10.1097/00000542-200212000-00035. [DOI] [PubMed] [Google Scholar]
- 9.Memis D, Turan A, Karamanlioglu B, Seker S, Ture M. Gabapentin reduces cardiovascular responses to laryngoscopy and tracheal intubation. Eur J Anaesthesiol. 2006;23(8):686–90. doi: 10.1017/S0265021506000500. [DOI] [PubMed] [Google Scholar]
- 10.Nishikawa T, Taguchi M, Kimura T, Taguchi N, Sato Y, Dai M. Effects of clonidine premedication upon hemodynamic changes associated with laryngoscopy and tracheal intubation. Masui. 1991;40(7):1083–8. [PubMed] [Google Scholar]
- 11.Stoelting RK. Circulatory changes during direct laryngoscopy and tracheal intubation: influence of duration of laryngoscopy with or without prior lidocaine. Anesthesiology. 1977;47(4):381–4. doi: 10.1097/00000542-197710000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Bruder N, Ortega D, Granthil C. Consequences and prevention methods of hemodynamic changes during laryngoscopy and intratracheal intubation. Ann Fr Anesth Reanim. 1992;11(1):57–71. doi: 10.1016/s0750-7658(05)80321-1. [DOI] [PubMed] [Google Scholar]
- 13.Slogoff S, Keats AS. Does perioperative myocardial ischemia lead to postoperative myocardial infarction? Anesthesiology. 1985;62(2):107–14. doi: 10.1097/00000542-198502000-00002. [DOI] [PubMed] [Google Scholar]
- 14.Fassoulaki A, Kaniaris P. Intranasal administration of nitroglycerine attenuates the pressor response to laryngoscopy and intubation of the trachea. Br J Anaesth. 1983;55(1):49–52. doi: 10.1093/bja/55.1.49. [DOI] [PubMed] [Google Scholar]
- 15.Stoelting RK. Attenuation of blood pressure response to laryngoscopy and tracheal intubation with sodium nitroprusside. Anesth Analg. 1979;58(2):116–9. [PubMed] [Google Scholar]
- 16.Cheng JK, Pan HL, Eisenach JC. Antiallodynic effect of intrathecal gabapentin and its interaction with clonidine in a rat model of postoperative pain. Anesthesiology. 2000;92(4):1126–31. doi: 10.1097/00000542-200004000-00031. [DOI] [PubMed] [Google Scholar]
- 17.Field MJ, Holloman EF, McCleary S, Hughes J, Singh L. Evaluation of gabapentin and S-(+)-3-isobutylgaba in a rat model of postoperative pain. J Pharmacol Exp Ther. 1997;282(3):1242–6. [PubMed] [Google Scholar]
- 18.Gee NS, Brown JP, Dissanayake VU, Offord J, Thurlow R, Woodruff GN. The novel anticonvulsant drug, gabapentin (Neurontin), binds to the alpha2delta subunit of a calcium channel. J Biol Chem. 1996;271(10):5768–76. doi: 10.1074/jbc.271.10.5768. [DOI] [PubMed] [Google Scholar]
- 19.Luo ZD, Chaplan SR, Higuera ES, Sorkin LS, Stauderman KA, Williams ME, et al. Upregulation of dorsal root ganglion (alpha)2(delta) calcium channel subunit and its correlation with allodynia in spinal nerve-injured rats. J Neurosci. 2001;21(6):1868–75. doi: 10.1523/JNEUROSCI.21-06-01868.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maneuf YP, McKnight AT. Block by gabapentin of the facilitation of glutamate release from rat trigeminal nucleus following activation of protein kinase C or adenylyl cyclase. Br J Pharmacol. 2001;134(2):237–40. doi: 10.1038/sj.bjp.0704227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hurley RW, Chatterjea D, Rose FM, Taylor CP, Hammond DL. Gabapentin and pregabalin can interact synergistically with naproxen to produce antihyperalgesia. Anesthesiology. 2002;97(5):1263–73. doi: 10.1097/00000542-200211000-00033. [DOI] [PubMed] [Google Scholar]
- 22.Eckhardt K, Ammon S, Hofmann U, Riebe A, Gugeler N, Mikus G. Gabapentin enhances the analgesic effect of morphine in healthy volunteers. Anesth Analg. 2000;91(1):185–91. doi: 10.1097/00000539-200007000-00035. [DOI] [PubMed] [Google Scholar]
- 23.Caraceni A, Zecca E, Martini C, De Conno F. Gabapentin as an adjuvant to opioid analgesia for neuropathic cancer pain. J Pain Symptom Manage. 1999;17(6):441–5. doi: 10.1016/s0885-3924(99)00033-0. [DOI] [PubMed] [Google Scholar]
- 24.Field MJ, Oles RJ, Lewis AS, McCleary S, Hughes J, Singh L. Gabapentin (neurontin) and S-(+)-3-isobutylgaba represent a novel class of selective antihyperalgesic agents. Br J Pharmacol. 1997;121(8):1513–22. doi: 10.1038/sj.bjp.0701320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Beydoun A, Uthman BM, Sackellares JC. Gabapentin: pharmacokinetics, efficacy, and safety. Clin Neuropharmacol. 1995;18(6):469–81. [PubMed] [Google Scholar]
- 26.Mellegers MA, Furlan AD, Mailis A. Gabapentin for neuropathic pain: systematic review of controlled and uncontrolled literature. Clin J Pain. 2001;17(4):284–95. doi: 10.1097/00002508-200112000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Fassoulaki A, Melemeni A, Paraskeva A, Petropoulos G. Gabapentin attenuates the pressor response to direct laryngoscopy and tracheal intubation. Br J Anaesth. 2006;96(6):769–73. doi: 10.1093/bja/ael076. [DOI] [PubMed] [Google Scholar]
- 28.Tsuchiya S, Kanaya N, Hirata N, Kurosawa S, Kamada N, Edanaga M, et al. Effects of thiopental on bispectral index and heart rate variability. Eur J Anaesthesiol. 2006;23(6):454–9. doi: 10.1017/S0265021506000159. [DOI] [PubMed] [Google Scholar]
- 29.Kaya FN, Yavascaoglu B, Baykara M, Altun GT, Gulhan N, Ata F. Effect of oral gabapentin on the intraocular pressure and haemodynamic responses induced by tracheal intubation. Acta Anaesthesiol Scand. 2008;52(8):1076–80. doi: 10.1111/j.1399-6576.2008.01627.x. [DOI] [PubMed] [Google Scholar]
- 30.Sarantopoulos C, McCallum B, Kwok WM, Hogan Q. Gabapentin decreases membrane calcium currents in injured as well as in control mammalian primary afferent neurons. Reg Anesth Pain Med. 2002;27(1):47–57. doi: 10.1053/rapm.2002.29124. [DOI] [PubMed] [Google Scholar]
- 31.Matot I, Sichel JY, Yofe V, Gozal Y. The effect of clonidine premedication on hemodynamic responses to microlaryngoscopy and rigid bronchoscopy. Anesth Analg. 2000;91(4):828–33. doi: 10.1097/00000539-200010000-00011. [DOI] [PubMed] [Google Scholar]
- 32.Zalunardo MP, Zollinger A, Spahn DR, Seifert B, Radjaipour M, Gautschi K, et al. Effects of intravenous and oral clonidine on hemodynamic and plasma-catecholamine response due to endotracheal intubation. J Clin Anesth. 1997;9(2):143–7. doi: 10.1016/S0952-8180(97)00239-0. [DOI] [PubMed] [Google Scholar]
- 33.Mikawa K, Maekawa N, Nishina K, Takao Y, Yaku H, Obara H. Efficacy of oral clonidine premedication in children. Anesthesiology. 1993;79(5):926–31. doi: 10.1097/00000542-199311000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Ghignone M, Calvillo O, Quintin L. Anesthesia and hypertension: the effect of clonidine on perioperative hemodynamics and isoflurane requirements. Anesthesiology. 1987;67(1):3–10. [PubMed] [Google Scholar]
- 35.Filos KS, Patroni O, Goudas LC, Bosas O, Kassaras A, Gartaganis S. A dose-response study of orally administered clonidine as premedication in the elderly: evaluating hemodynamic safety. Anesth Analg. 1993;77(6):1185–92. doi: 10.1213/00000539-199312000-00018. [DOI] [PubMed] [Google Scholar]
- 36.Carabine UA, Wright PM, Moore J. Preanaesthetic medication with clonidine: a dose-response study. Br J Anaesth. 1991;67(1):79–83. doi: 10.1093/bja/67.1.79. [DOI] [PubMed] [Google Scholar]
- 37.Kobinger W, Pichler L. Localization in the CNA of adrenoceptors which facilitate a cardioinhibitory reflex. Naunyn Schmiedebergs Arch Pharmacol. 1975;286(4):371–7. doi: 10.1007/BF00506651. [DOI] [PubMed] [Google Scholar]
- 38.Habib AS, Parker JL, Maguire AM, Rowbotham DJ, Thompson JP. Effects of remifentanil and alfentanil on the cardiovascular responses to induction of anaesthesia and tracheal intubation in the elderly. Br J Anaesth. 2002;88(3):430–3. doi: 10.1093/bja/88.3.430. [DOI] [PubMed] [Google Scholar]


