Abstract
BACKGROUND:
This study aimed to determine red blood cell (RBC) and serum folate and vitamin B12 levels as well as their intake in schizophrenic patients.
METHODS:
The folate and cobalamin status of 60 schizophrenic patients (15-55 years) was compared to 60 matched healthy controls using Radio Isotope Dilution Assay (RIDA).
RESULTS:
Serum and RBC folate in schizophrenic patients was significantly lower than the control group. Mean serum cobalamin levels in the schizophrenic group were higher than controls.
CONCLUSIONS:
This study showed that folate deficiency is common in schizophrenic patients; therefore, it is important to pay attention to folate levels in these patients.
KEYWORDS: Folic Acid, Vitamin B12, Schizophrenia, Eating
The metabolism of cobalamin and folic acid is interrelated and both are necessary in several pathways in the human central nervous system. Cobalamin and folate facilitate the production of S-adenosylmethionine (SAM), the exceptional donor of a methylgroup for various reactions of methylation, by promoting the conversion of homocysteine into methionine.1
Cobalamin and folic acid deficiency may contribute to the pathogenesis of neuropsychiatric disorders such as mental confusion, memory changes, cognitive slowing, mood disorder, violent behavior, fatigue, delirium and paranoid psychosis.2
It was hypothesized that an aberrant folate metabolism could also contribute to the pathogenesis of schizophrenia. Schizophrenia is a complex psychiatric disease that is speculated to result from multiple genetic and environmental factors.3 A study by Silver (2000) on 644 bedridden psychotics reported that 78.3% of schizophrenic patients had vitamin B12 deficiency.4 Some studies have clearly indicated the contribution of folic acid, vitamin B12 and homocysteine to altered single-carbon metabolism and its role in the psychopathophysiology of schizophrenia.5
This study was aimed to determine cobalamin and folate status in schizophrenic patients and mentally healthy controls.
Methods
A total of 60 schizophrenic patients as well as 60 age- and sex- matched healthy controls (21 women and 39 men aged 15 to 55 years) were enrolled into the study from March 2009 to January 2010 in Taleqani hospital, Tehran, Iran. All the participants completed the written consent form. The healthy control group was recruited from volunteers in the staff of the Taleqani hospital. All enrolled cases fulfilled the DSM-IV (American Psychiatric Association, 2000) criteria for diagnosis of schizophrenia.6
Those who consumed vitamin B12 or folate supplements in previous year, the subjects with abnormal bleeding, digestive, infectious, parasitic or heart diseases, diabetes mellitus, hyperthyroidism, pregnancy and lactation during last year and vegetarians were excluded from the study.
Data were collected using general questionnaire, 24-hour food recall questionnaire and food frequency questionnaire (FFQ). Non fasting blood samples were taken from all subjects. Each blood sample (5 ml) divided in two parts. The first part (1.5 ml) containing 1 ml 1% ethylenediamine tetra-acetate (EDTA) was assayed for RBC folate concentrations. The samples with EDTA (100 μl) were mixed with 2 ml 0.2% ascorbic acid and stored at -20°C, until analysis.7 Hemoglobin (Hb), hematocrit (Hct), mean corpuscular volume (MCV) and mean corpuscular hemoglobin concentration (MCHC) were measured by H1 apparatus for hematological analyses of Taleqani hospital laboratory, Tehran, Iran. The second part of blood samples (3.5 ml) was transferred immediately into the tubes without any anticoagulant agents. The blood cells and plasma samples were separated by centrifugation (10 min, 3000 rpm). Plasma samples were stored at -20°C, until serum folate and cobalamin measurements.
Serum folate and cobalamin and RBC folate were determined by using radio isotope dilution assay (RIDA) kits in biochemistry department of the School of Public Health, Tehran University of Medical Sciences, Tehran, Iran, according to the manufacturer's instructions (Diagnostic Product Corporation, Los Angeles, CA, USA).
To compare averages in the case and control groups, Student's t-test and Mann-Whitney U test were used. To evaluate qualitative variables and hematological parameters, χ2 test and Fisher's exact test were utilized. To determine correlation between quantitative variables and hematological parameters, Pearson's Correlation Coefficient was used. Eventually, to omit the effects of confounding variables, Mantel-Haenszel was utilized. Results were presented as mean ± SD and p < 0.05 was regarded significant for all comparisons.
Results
Table 1 shows the non-fasting hematologic variables in the case and control groups.
Table 1.
Non-fasting hematologic variables concentrations in the case group versus the control group
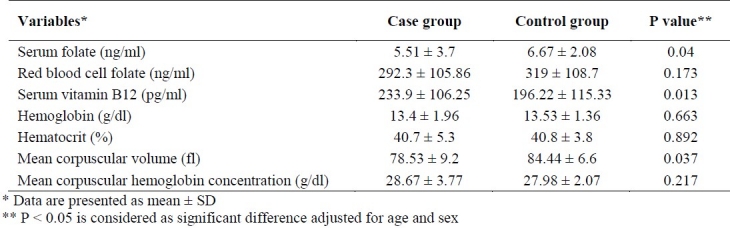
Serum folate levels of controls were significantly higher than schizophrenic patients (p < 0.05). In the case group, 5 out of 60 patients (8.3%) had serum folate deficiency (less than 3 ng/ml), while folate deficiency was not seen in the control group (p < 0.05). RBC folate levels of schizophrenic patients and the control group were not different. Twelve out of 60 schizophrenic patients (20%) had confined and marginal RBC folate deficiencies (less than 200 ng/ml), which was significantly higher (p < 0.05) than its proportion in the healthy controls (4 out of 60, 6.7%). Serum cobalamin in schizophrenic patients was higher than healthy controls (p < 0.05). In schizophrenic patients, serum cobalamin deficiency (less than 120 pg/ml) was observed in 13.3% (8 out of 60), which was less (p < 0.05) than its proportion in the healthy controls (14 out of 60, 23.3%).
There was no significant difference in hemoglobin and hematocrit concentrations between schizophrenic patients and healthy controls. MCV in schizophrenic patients was significantly lower than the healthy controls (p < 0.05). MCV was high in 8 out of 60 schizophrenic patients (13.3%), but only in 2 out of 60 (3.3%) controls was higher than normal range (p < 0.05). There was no significant difference between MCHC of schizophrenic patients and healthy controls. MCHC was higher than normal range in 12 out of 60 cases (20%), but only in 1 out of 60 (1.7%) healthy controls was higher (p < 0.05).
Table 2 shows the relationship of hematologic variables in schizophrenic patients and healthy controls.
Table 2.
Relationship between blood parameters in schizophrenic patients and controls*
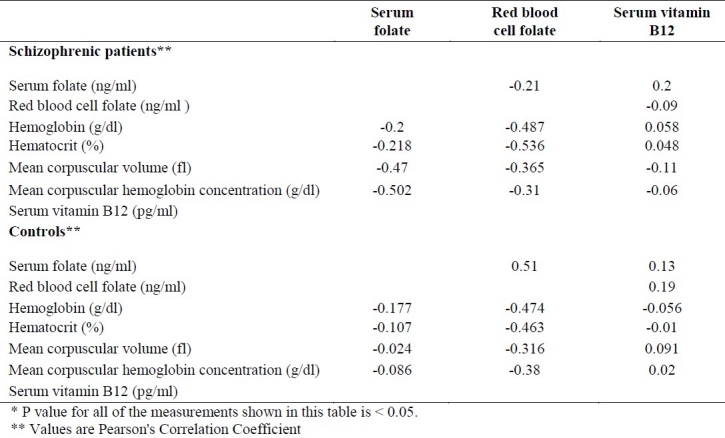
Serum folate levels showed a positive and significant correlation with the RBC folate in healthy controls (p < 0.001). In the case and control groups, serum folate and cobalamin levels had no correlation. RBC folate levels did not show any correlation with serum cobalamin in schizophrenic patients and healthy controls. RBC folate levels had a strong negative and significant correlation (p < 0.001) versus hemoglobin and hematocrit levels in both schizophrenic patients and healthy controls. Significant negative correlation was observed between MCHC and MCV levels versus RBC folate in both groups (p < 0.01). In schizophrenic patients, serum folate levels had a significant negative correlation (p < 0.01) versus MCHC and MCV concentrations.
In schizophrenic patients, folate intake was (167.3 ± 90.5) and in the control group it was (195.9 ± 70), which is not significantly different. However, in schizophrenic patients, cobalamin intake average (2.38 ± 3.8) was significantly (p < 0.01) less than healthy controls (2.49 ± 1.2).
Discussion
We found a higher frequency of low levels of serum folate deficiency in schizophrenic patients compared to controls (8.3% versus 0%). Mean serum folate levels in healthy controls were significantly higher than the case group. Although mean RBC folate levels was equal between schizophrenic patients and controls, there was a significant difference in RBC folate deficiency between cases and controls (20% versus 6.7%). In one study, a lower plasma folate level is found in schizophrenic patients compared to the healthy controls,8 which is confirmed in the present study. On the other hand, researchers did not find any difference in folic acid status among different psychiatric disorders versus healthy controls.9 Reduced levels of serum folate but not the red blood cell folate are reported in both schizophrenic and depressive disorder patients.10 In our study, the average of folate intake in schizophrenic patients was non-significantly lower (167.3 ± 90.5) than the healthy controls (195.9 ± 70). Nevertheless, there was no indication of any nutritional shortage or a defect in folate uptake to explain the lowered plasma folate levels in the group of schizophrenic patients in the present study.
In the present study, mean serum cobalamin levels of schizophrenic patients were significantly higher than healthy controls. Cobalamin deficiency in schizophrenic patients (13.3%) was significantly lower than the controls (23.3%). In one study, in disagreement with our findings, mean serum cobalamin concentrations were similar in schizophrenic patients and controls.9 On the other hand, one study has demonstrated reduced folate and cobalamin levels, among schizophrenic patients.11 In a survey in Mexico, the mean serum cobalamin levels in schizophrenic patients (409.75 ± 243.79) were higher than healthy controls (407.71 ± 210.18),8 which is confirmed in the present study. In the present study, RBC folate levels had no correlation with serum cobalamin in schizophrenic patients, which confirms another study.12 Some schizophrenic patients did not collaborate in filling out the FFQ. The FFQ was merely qualitative and eventually the blood samples were collected from only one hospital, which may act as possible shortages of the present study. Meanwhile, some researchers have recommended an examination of serum methyl malonic acid (MMA) and/or homocysteine (Hcy) as a proof of cobalamin or folate deficiency.1
Conclusions
In conclusion, the findings suggest that decreased plasma folate may act as a risk factor for schizophrenia. Therefore, it is suggested to evaluate the serum cobalamin and folate levels for all newly admitted schizophrenic patients.
Authors’ Contributions
MD supervised the biochemistry experiments and assisted in preparation of the manuscript. AS supervised nutrition science experiments and assisted in preparation of the manuscript. AMM, OR and LN selected patients for the samples, performed laboratory tests, analyzed the data and also assisted in preparation of the manuscript. All authors have read and approved the content of the manuscript.
Footnotes
Conflict of Interests Authors has no conflict of interests.
References
- 1.Stabler SP, Marcell PD, Podell ER, Allen RH, Savage DG, Lindenbaum J. Elevation of total homocysteine in the serum of patients with cobalamin or folate deficiency detected by capillary gas chromatography-mass spectrometry. J Clin Invest. 1988;81(2):466–74. doi: 10.1172/JCI113343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bottiglieri T. Folate, vitamin B12, and neuropsychiatric disorders. Nutr Rev. 1996;54(12):382–90. doi: 10.1111/j.1753-4887.1996.tb03851.x. [DOI] [PubMed] [Google Scholar]
- 3.Levi RN, Waxman S. Schizophrenia, epilepsy, cancer, methionine, and folate metabolism.Pathogenesis of schizophrenia. Lancet. 1975;2(7923):11–3. doi: 10.1016/s0140-6736(75)92952-9. [DOI] [PubMed] [Google Scholar]
- 4.Silver H. Vitamin B12 levels are low in hospitalized psychiatric patients. Isr J Psychiatry Relat Sci. 2000;37(1):41–5. [PubMed] [Google Scholar]
- 5.Monji A, Yanagimoto K, Maekawa T, Sumida Y, Yamazaki K, Kojima K. Plasma folate and homocysteine levels may be related to interictal “schizophrenia-like” psychosis in patients with epilepsy. J Clin Psychopharmacol. 2005;25(1):3–5. doi: 10.1097/01.jcp.0000150225.76748.73. [DOI] [PubMed] [Google Scholar]
- 6.4th ed. Washington: American Psychiatric Association Inc; 2000. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR. [Google Scholar]
- 7.Zemlin AE, Essack Y, Rensburg M, Jephtha E, Abrahams N, Brinkmann T. Red blood cell folate stability study: stability of whole blood prior to haemolysate preparation and stability of the haemolysate at various temperatures. Med Technol SA. 2009;23(1):14–6. [Google Scholar]
- 8.García-Miss Mdel R, Pérez-Mutul J, López-Canul B, Solís-Rodríguez F, Puga-Machado L, Oxté-Cabrera A, et al. Folate, homocysteine, interleukin-6, and tumor necrosis factor alfa levels, but not the methylenetetrahydrofolate reductase C677T polymorphism, are risk factors for schizophrenia. J Psychiatr Res. 2010;44(7):441–6. doi: 10.1016/j.jpsychires.2009.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Reif A, Pfuhlmann B, Lesch KP. Homocysteinemia as well as methylenetetrahydrofolate reductase polymorphism are associated with affective psychoses. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29(7):1162–8. doi: 10.1016/j.pnpbp.2005.06.027. [DOI] [PubMed] [Google Scholar]
- 10.Herrán A, García-Unzueta MT, Amado JA, López-Cordovilla JJ, Díez-Manrique JF, Vázquez-Barquero JL. Folate levels in psychiatric outpatients. Psychiatry Clin Neurosci. 1999;53(4):531–3. doi: 10.1046/j.1440-1819.1999.00572.x. [DOI] [PubMed] [Google Scholar]
- 11.Silver H, Goodman C, Bilker W, Gur RC, Isakov V, Knoll G, et al. Impaired error monitoring contributes to face recognition deficit in schizophrenia patients. Schizophr Res. 2006;85(1-3):151–61. doi: 10.1016/j.schres.2006.02.027. [DOI] [PubMed] [Google Scholar]
- 12.Muntjewerff JW, van der Put N, Eskes T, Ellenbroek B, Steegers E, Blom H, et al. Homocysteine metabolism and B-vitamins in schizophrenic patients: low plasma folate as a possible independent risk factor for schizophrenia. Psychiatry Res. 2003;121(1):1–9. doi: 10.1016/s0165-1781(03)00200-2. [DOI] [PubMed] [Google Scholar]


