Abstract
BACKGROUND:
Helicobacter pylori (H. pylori) infection has been associated with atherosclerosis of coronary arteries but there is lack of data regarding possible association between chronic H. Pylori infection and cerebral non-cardioembolic ischemia. We evaluated H. pylori serum antibody titers in patients with cerebral non-cardioembolic ischemic stroke.
METHODS:
This was a cross-sectional study carried out in Alzahra hospital, Isfahan, Iran. 96 patients with ischemic stroke were enrolled in this study. Control group were selected from healthy blood donors. IgG and IgA antibodies to H. pylori were detected using a rapid enzyme linked immunosorbent assay. Quantitative variables and categorical variables were compared using t student and chi-square tests.
RESULTS:
There were 21 cases of hypertension and 5 cases of diabetes mellitus among patients. Patients and controls were similar regarding serum IgA and IgG titers as well as positivity. There were 13 and 15 cases of positive IgA and 44 and 39 cases of positive IgG among patients and controls, respectively. Also, there were 7 and 9 cases of both positive IgA and IgG in patients and controls, respectively. No differences were found between the two groups in IgA or IgG titers or positivity (p > 0.05).
CONCLUSIONS:
Patients with stroke were not different regarding either H. Pylori IgA or IgG positivity or the antibody titers. Comparing genetic typing of H. pylori in patients with or without stroke and diagnosis of H. pylori with more specific and sensitive tests such as stool antigen test are recommended.
KEYWORDS: Helicobacter, Infection, Inflammation, Athreosclerosis, Stroke
There has been increasing evidence that in addition to established risk factors, markers of inflammation and chronic infectious diseases may be linked to stroke and other ischemic vascular diseases. Infection with helicobacter pylori is among the infectious diseases discussed in this respect. Helicobacter pylori is a gram-negative spiral bacterium that can cause gastritis, peptic ulcer, and gastric cancer but often remains asymptomatic.1
After infection, which occurs mostly in childhood via fecal-oral or oral-oral pathways, it persists in the gastric mucousal layer. The infection induces a serum antibody response, which persists during the entire lifetime. Socioeconomic factors influence the age and the rate of infection (IgG or IgA) with Helicobacter pylori,2,3 and low socioeconomic status in childhood appears to be associated with Helicobacter pylori seropositivity.4 Data on chronic infection in cerebrovascular disease are limited. In a pilot study, Hugh and coworkers found a significant relation between Helicobacter pylori infection and stroke.5
On the other hand Heushmann et al. found that chronic Helicobacter pylori infection was associated with higher risk of stroke caused by small artery occlusion and a lower risk of cardioembolic stroke, but totally elevated Helicobacter pylori antibodies were not associated with ischemic stroke.6 Because direct detection methods for Helicobacter pylori depend on cerebrovascular wall samples retrieved in vivo, which are not available obviously, so antibody levels must use to describe the association between stroke and previous infection in an indirect manner. Therefore, we conducted this case control study, to investigate serological evidence of Helicobacter pylori infection as an independent risk factor in cerebral non-cardioembolic ischemic stroke. In contrast to other studies, we excluded cases with other known risk factors in order to evaluate an independent role of this infection.
Methods
During a period of one year (2008-2009), all ischemic stroke patients with following criteria were enrolled in this prospective analysis study: (a) it was their first ischemic stroke, (b) treatment of their stroke was performed in Al-Zahra hospital, and (c) admission to hospital was within the first 72 h after stroke onset. Stroke was defined according to WHO criteria [computerized tomography scanning (CT scan) or magentic resonance imaging (MRI) finding].
Patients with a known cardiac source for cerebral embolism (arterial fibrillation, valvu-lar heart disease in echocardiography and prosthetic heart valves), those with major risk factors for atherosclerosis: [hypertension (blood pressure of 140/90 mmHg or greater in repetitive controls), diabetes mellitus (based on American Diabetes association criteria) and symptoms related to peptic ulcer disease (known peptic ulcer disorder using endoscopy, use of antipeptic ulcer treatment, suspected cases according to history and gastrointestinal symptoms] were excluded.
According to the above inclusion criteria, 96 patients were selected for study.
Control group were selected from healthy blood donors. Control group did not have any history of cerebrovascular and coronary accidents and suspected peptic ulcer disease. They were matched for age, sex, and area of residence so 93 controls were included in the study.
Physical and neurological examinations were performed for all cases and blood samples were taken within the first week after admission. Information was collected directly from the patient and in case of disability of participant to communicate, from a close relative. Control objects were interviewed and evaluated in the same manner as cases.
Blood samples of either cases or control group were labeled immediately after taking blood. Thus, laboratory investigators were blinded to case or control group status during the laboratory tests, sera was stored at 2-8°C for 1 week and at -20° C for more prolonged time. IgG and IgA antibodies to Helicobacter pylori were detected using a rapid enzyme linked immunosorbent assay (EIA WELL, REF K5HPG kit, Roma, Italia). Assay procedure according to the manufacturer's order and recommended measures were chosen to indicate IgG and IgA Helicobacter pylori seropositivity. Values higher than 20 U/ml were considered reactive. According to the manufactured statement, the sensitivity and the specificity of the methods were 95.8 and 96.2%, respectively.
Statistical analysis was performed using the SPSS 15.0 software package (IBM, USA).
Quantitative data were expressed through mean and standard deviation, and categorical variables were described by relative frequencies. For comparisons of the quantitative variables including serum IgA and IgG levels, we used t-test, and for comparisons between the categorical variables including the presence or absence of the diabetes, hypertension or sex, the chi-square test was used. The statistical significance criterion was set at p < 0.05.
Results
Baseline characteristics of the patients and controls are shown in Table 1. There was no significant difference regarding age and gender between the two groups (p > 0.05). There were 21 cases of hypertension (HTN) and 5 cases of diabetic mellitus (DM) among patients.
Table 1.
Baseline characteristics of the patients (stroke) and controls
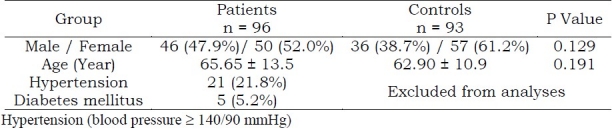
IgA and IgG titers and final results of the patients and controls are shown in Table 2 and Figure 1. As we can see, patients and controls were similar regarding serum IgA and IgG titers as well as positivity. There were 13 and 15 cases of positive IgA and 44 and 39 cases of positive IgG among patients and controls, respectively. Also, there were 7 and 9 cases of both positive IgA and IgG in patients and controls, respectively. No differences were found between the two groups in IgA or IgG titers or positivity (p > 0.05).
Table 2.
IgA and IgG titers (mg/dl) and final results of the patients (stroke) and controls
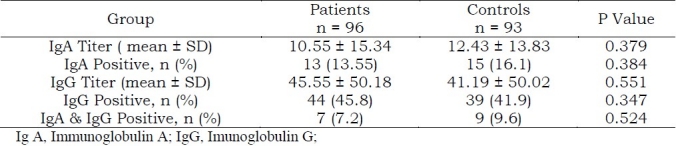
Figure 1.
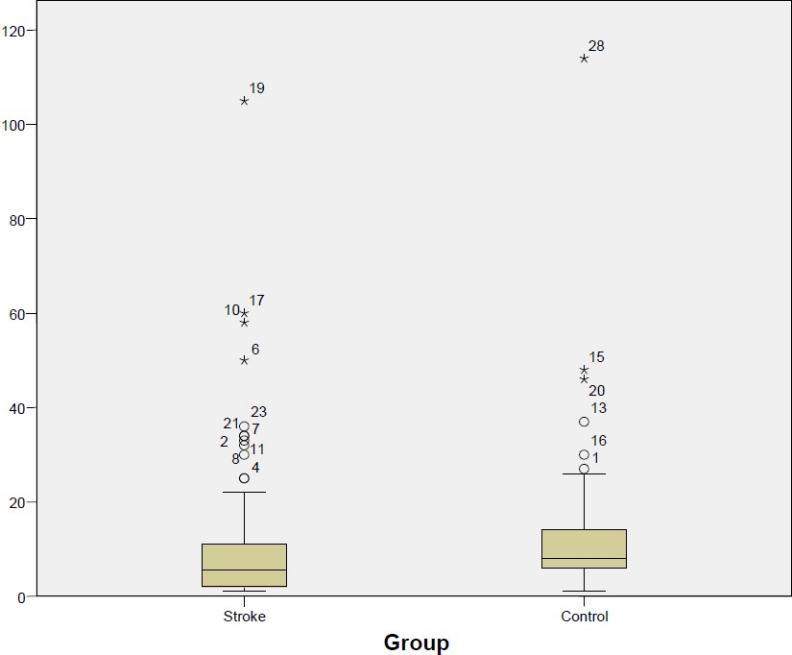
Comparison between IgA (immunoglobulin A) titer in the stroke and control groups
Discussion
There has been increasing evidence that in addition to established risk factors, markers of inflammation and chronic infectious diseases may be linked to stroke and other ischemic vascular diseases. Infection with helicobacter pylori is among the infectious diseases discussed in this respect.
Helicobacter pylori, one of the gramnegative spiral bacteria, acquired mostly during childhood, generally persists during lifetime period, and can cause chronic gastritis, peptic ulcer disease, and gastric cancer. Seroepidemiological studies on H pylori and CHD yielded widely varying results, but the larger studies and those that adjusted for potential confounders were mostly negative or reported moderate effects in multivariate analyses.1–3
Regarding stroke, a small, nested, case-control study found an increased risk in univariate but not in multivariate analysis. In 4 other case-control studies, seropositivity was associated with the risk of atherothrombotic and/or microangiopathic stroke.3,4,6 The studies used spouses as controls and adjusted for social class or school education;3,4 however, confounding mainly by childhood socioeconomic factors that are important regarding H pylori infection was not sufficiently excluded by these studies.
Furthermore, the studies were small and did not possess sufficient statistical power to exclude the play of chance in subgroup analyses. In a prospective study, seropositivity for H pylori–as for C pneumoniae, cytomegalovirus (CMV), and herpes simplex virus (HSV)–did not predict cardiovascular events in women.6 H pylori strains bearing the cytotoxin-associated gene-A (CagA) are particularly virulent and are associated with increased inflammation.
Seroprevalence against CagA strains but not H pylori in general increased in large-vessel stroke but not in cardioembolic stroke after adjustment for parental social class among other factors.7 An association between seropositivity against the CagA strain and increased intima-media thickness was rendered nonsignificant after controlling for cardiovascular risk factors.8 Antibodies against CagA cross-react with vascular wall antigens, and this may possibly represent a pathogenetic link between H pylori infection and atherosclerosis.9 Whereas H pylori had not been detected in atherosclerotic plaques in the past, recent studies showed its presence in carotid plaques and its association with upregulated adhesion receptors.9–11
There is conflicting evidence about the relevance of chronic infection by Helicobacter pylori (H. pylori) as a risk factor for stroke.12–14 In addition, it has been suggested that the aggregate burden of chronic or past infections rather than any one single infectious disease is related with the risk of stroke. Moreover, genetic predispositions relating to infection susceptibility and the strength of the inflammatory response had been suggested to co-determine this risk.15 However, the results of the present study showed that patients with stroke are not different from healthy age and sex matched controls in regards to either H. pylori IgA or IgG positivity or the antibody titers.
Cremonini et al performed a meta-analysis of case-control studies to assess association of H. pylori infection and more virulent H. pylori strains, bearing the cytotoxin-associated gene-A (CagA) antigen, with different types of stroke. Outcome measures were H. pylori and CagA seroprevalence in (1) patients with stroke versus controls, and (2) patients with stroke due to large vessel stroke versus patients with other types of stroke and controls. Seven cross-sectional, case-control studies were included. Odds ratio for individual case-control studies and pooled OR for the association between H. pylori seropositivity and stroke was 1.49 (95% CI 1.24-1.81), while for the association between stroke and anti-CagA positivity was 2.23 (95% CI 1.49-3.36). Patients with large vessel stroke had higher odds for H. pylori infection than patients with other types of stroke (odds ratio 1.65; 95% CI 1.12-2.45), and than controls (odds ratio 1.61; 95% CI 1.13-2.32). Authors concluded that association between H. pylori positivity, anti-CagA posi-tivity and stroke is modest and seems higher with stroke due to large vessel disease.
Conclusion
The results of the present study showed that patients with stroke are not different from healthy age and sex matched controls in regards to either H. pylori IgA or IgG positivity or the antibody titers.
Authors’ Contributions
SAM and IK have planned study and collected specimen and supervised the project with association of BA. BA has planned the study and prepared the first version and finalized the manuscript. KA has done statistical analysis and prepared the first version of manuscript. All authors have read and approved the content of the manuscript.
Acknowledgments
Authors are thankful to Dr. Ali Gholamrezaei who helped us in preparing this report.
Footnotes
Conflict of Interests Authors has no conflict of interests.
References
- 1.Lindsberg PJ, Grau AJ. Inflammation and infections as risk factors for ischemic stroke. Stroke. 2003;34(10):2518–32. doi: 10.1161/01.STR.0000089015.51603.CC. [DOI] [PubMed] [Google Scholar]
- 2.Graham DY, Malaty HM, Evans DG, Evans DJ, Jr, Klein PD, Adam E. Epidemiology of Helicobacter pylori in an asymptomatic population in the United States. Effect of age, race, and socioeconomic status. Gastroenterology. 1991;100(6):1495–501. doi: 10.1016/0016-5085(91)90644-z. [DOI] [PubMed] [Google Scholar]
- 3.Mendall MA, Goggin PM, Molineaux N, Levy J, Toosy T, Strachan D, et al. Childhood living conditions and Helicobacter pylori seropositivity in adult life. Lancet. 1992;339(8798):896–7. doi: 10.1016/0140-6736(92)90931-r. [DOI] [PubMed] [Google Scholar]
- 4.Fiedorek SC, Malaty HM, Evans DL, Pumphrey CL, Casteel HB, Evans DJ, Jr, et al. Factors influencing the epidemiology of Helicobacter pylori infection in children. Pediatrics. 1991;88(3):578–82. [PubMed] [Google Scholar]
- 5.Markus HS, Mendall MA. Helicobacter pylori infection: a risk factor for ischaemic cerebrovascular disease and carotid atheroma. J Neurol Neurosurg Psychiatry. 1998;64(1):104–7. doi: 10.1136/jnnp.64.1.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heuschmann PU, Neureiter D, Gesslein M, Craiovan B, Maass M, Faller G, et al. Association between infection with Helicobacter pylori and Chlamydia pneumoniae and risk of ischemic stroke subtypes: Results from a population-based case-control study. Stroke. 2001;32(10):2253–8. doi: 10.1161/hs1001.097096. [DOI] [PubMed] [Google Scholar]
- 7.Ameriso SF, Fridman EA, Leiguarda RC, Sevlever GE. Detection of Helicobacter pylori in human carotid atherosclerotic plaques. Stroke. 2001;32(2):385–91. doi: 10.1161/01.str.32.2.385. [DOI] [PubMed] [Google Scholar]
- 8.phull PS, Gower JD, Price AB, Green CJ, Jacyna MR. Alpha-tocopherol antioxidant levels in chronic gastritis: correlation with mucosal neutrophil infiltration. Gut. 1993;34(Supplement 1):133. [Google Scholar]
- 9.Stringer MD, Gorog PG, Freeman A, Kakkar VV. Lipid peroxides and atherosclerosis. BMJ. 1989;298(6669):281–4. doi: 10.1136/bmj.298.6669.281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sung JJ, Sanderson JE. Hyperhomocysteinaemia, Helicobacter pylori, and coronary heart disease. Heart. 1996;76(4):305–7. doi: 10.1136/hrt.76.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Muhlestein JB. Bacterial infections and atherosclerosis. J Investig Med. 1998;46(8):396–402. [PubMed] [Google Scholar]
- 12.Preusch MR, Grau AJ, Buggle F, Lichy C, Bartel J, Black C, et al. Association between cerebral ischemia and cytotoxin-associated gene-A-bearing strains of Helicobacter pylori. Stroke. 2004;35(8):1800–4. doi: 10.1161/01.STR.0000131751.35926.48. [DOI] [PubMed] [Google Scholar]
- 13.Diomedi M, Pietroiusti A, Silvestrini M, Rizzato B, Cupini LM, Ferrante F, et al. CagA-positive Helicobacter pylori strains may influence the natural history of atherosclerotic stroke. Neurology. 2004;63(5):800–4. doi: 10.1212/01.wnl.0000138025.82419.80. [DOI] [PubMed] [Google Scholar]
- 14.Elkind MS, Ramakrishnan P, Moon YP, Boden-Albala B, Liu KM, Spitalnik SL, et al. Infectious burden and risk of stroke: the northern Manhattan study. Arch Neurol. 2010;67(1):33–8. doi: 10.1001/archneurol.2009.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grau AJ, Urbanek C, Palm F. Common infections and the risk of stroke. Nat Rev Neurol. 2010;6(12):681–94. doi: 10.1038/nrneurol.2010.163. [DOI] [PubMed] [Google Scholar]


