Abstract
Objectives
Extreme vasculobiliary injuries usually involve major hepatic arteries and portal veins. They are rare, but have severe consequences, including rapid infarction of the liver. The pathogenesis of these injuries is not well understood. The purpose of this study was to elucidate the mechanism of injury through an analysis of clinical records, particularly the operative notes of the index procedure.
Methods
Biliary injury databases in two institutions were searched for data on extreme vasculobiliary injuries. Operative notes for the index procedure (cholecystectomy) were requested from the primary institutions. These notes and the treatment records of the tertiary centres to which the patients had been referred were examined. Radiographs from the primary institutions, when available, as well as those from the tertiary centres, were studied.
Results
Eight patients with extreme vasculobiliary injuries were found. Most had the following features in common. The operation had been started laparoscopically and converted to an open procedure because of severe chronic or acute inflammation. Fundus-down cholecystectomy had been attempted. Severe bleeding had been encountered as a result of injury to a major portal vein and hepatic artery. Four patients have required right hepatectomy and one had required an orthotopic liver transplant. Four of the eight patients have died and one remains under treatment.
Conclusions
Extreme vasculobiliary injuries tend to occur when fundus-down cholecystectomy is performed in the presence of severe inflammation. Contractive inflammation thickens and shortens the cystic plate, making separation of the gallbladder from the liver hazardous.
Keywords: laparoscopic cholecystectomy, bile duct injury, fundus down cholecystectomy, top down cholecystectomy, antegrade cholecystectomy, gallbladder
Introduction
Vasculobiliary injuries may be classified into two types, of which one is common and the other very uncommon.1 In the common variety, the right hepatic artery and a bile duct are injured. This variant accounts for about 90% of vasculobiliary injuries.1 The pathogenesis and consequences of right hepatic artery vasculobiliary injuries are well described.1–3 The most common consequence is biliary ischaemia, which may lead to anastomotic problems such as bile leakage and stenosis. Clinically significant hepatic ischaemia is uncommon and, when it occurs, it tends to evolve slowly.1 Death is a very infrequent consequence.1,3
The uncommon type of vasculobiliary injury involves a bile duct(s) and the proper hepatic artery, the common hepatic artery, the main portal vein, the right portal vein, or one of these veins as well as a hepatic artery, possibly including the right hepatic artery.1 A recent review1 identified 25 such patients in the literature.4–18 The consequences of such injuries are much more extreme. Hepatic infarction is common, often with rapid onset and frequently necessitating emergency right hepatectomy or urgent liver transplantation.1 Death occurred in about 50% of the patients reported.1
The pathogenesis and mechanism of injury of the extreme type of vasculobiliary injury are not well described. As a result, strategies for avoidance are not highly developed or based on evidence. The purpose of this study was to elucidate the mechanism or mechanisms of injury through an analysis of clinical records with particular reference to the operative notes of patients who suffered the extreme type of injury.
Materials and methods
The biliary injury databases of two institutions, the Academic Medical Centre, Amsterdam and Washington University in St Louis/Barnes Jewish Hospital, were searched for data on vasculobiliary injuries that involved the proper hepatic artery, the common hepatic artery, the main or right portal vein, or one of these veins and one of the arteries including the right hepatic artery. Operative notes for the index procedure (cholecystectomy) were requested from the primary institutions. These and the treatment records of the tertiary centres to which the patients had been referred were examined. Radiographs from the primary institutions, when available, as well as those from the tertiary centres, were studied.
The term ‘fundus-down’ will be used to describe a cholecystectomy that was performed by separating the gallbladder from the liver beginning at the fundus, without initially successfully displaying a putative cystic artery and cystic duct in the triangle of Calot. This type of cholecystectomy has also been called ‘dome-down’ cholecystectomy and ‘antegrade’ cholecystectomy.
Results
Demographics
Eight patients were identified in the databases. All patients were female. Their mean age was 56.8 years (range: 37–77 years). Three of the patients were treated in Amsterdam and five in Saint Louis in the years 1999–2010. All patients had symptomatic cholelithiasis. Operative notes for the cholecystectomy were obtained for seven of the eight patients. The operative notes for the final patient had been ‘lost’. However, the surgeon who had performed the cholecystectomy was interviewed to obtain the details of the procedure. Approximately 400 operative repairs of major bile duct injuries have been performed at these institutions (250 at the Academic Medical Centre in Amsterdam and 150 at Washington University in St Louis). Therefore, these eight patients represent 2% of patients referred to these institutions with biliary injuries requiring operative reconstruction. Based on an estimate that 25% of biliary injuries are vasculobiliary injuries,1 these extreme injuries would account for about 8% of vasculobiliary injuries.
Degree of inflammation of the gallbladder
Seven of eight operative notes described severe inflammation of the gallbladder. In five patients the inflammation was chronic. This manifested as dense scarring. Two of the five patients were noted to have contracted gallbladders; in another patient the gallbladder was hard and white and the surgeon became concerned about the possibility of gallbladder cancer. In retrospect, these symptoms were found to reflect severe chronic inflammation. Acute cholecystitis was present in two other patients, in combination with chronic inflammation in one of them. The severity of inflammation was evidenced by other remarks in the operative notes, which referred to the presence of adhesions (in five patients), adherence of other organs to the gallbladder (in five patients), especially the colon, and difficulty in identifying the gallbladder at all. Once the gallbladder was identified, difficulty in finding a plane between the gallbladder and liver was noted in four patients.
Conversions
All cholecystectomies had commenced as laparoscopic procedures and all had been converted to open cholecystectomy. Conversion was performed because of the severity of inflammation in seven patients and after bleeding from the portal vein during the laparoscopic portion of the procedure in one patient. In one patient conversion occurred after an abscess was entered. The events leading to conversion were well described in some of the operative notes (Table 1).
Table 1.
Paraphrased statements sourced from operative notes on the reasons for conversion from laparoscopic to open cholecystectomy
| Patient 1 | Dissecting the gallbladder from the gallbladder bed during the laparoscopic phase caused severe bleeding from the portal vein, leading to conversion |
| Patient 2 | The gallbladder was inflamed and there were adhesions to surrounding structures. Structures could not be adequately recognized and conversion was performed after inspection of the severity of the inflammation |
| Patient 3 | The gallbladder could not be seen as a result of adhesions. After blunt dissection a fibrotic/inflamed gallbladder was found. Puncture revealed pus and the patient was converted |
| Patient 4 | On examination there was significant inflammatory reaction, and adhesions as well as scars from the previous gastrectomy. The procedure was converted |
| Patient 5 | This operation could not be performed laparoscopically secondary to adhesions, inflammation and the inability to identify the ductal structures adequately |
| Patient 6 | The gallbladder was severely contracted and contorted. It was obvious that it would not be possible to identify the critical structures. Thus the operation was converted to an open procedure |
| Patient 7 | No operative note |
| Patient 8 | A laparoscopic cholecystectomy was attempted, but it became obvious after trying to dissect the tissue from the gallbladder that this would be unsuccessful |
Method of open cholecystectomy
The operative notes of seven patients clearly stated that, after conversion, a fundus-down cholecystectomy had been performed. In the eighth patient, the fundus-down technique had been attempted laparoscopically. In two of the seven patients, the surgeon had attempted to dissect structures at the lower end of the gallbladder, but had abandoned this approach for lack of progress as a result of inflammation. In the other patients, fundus-down cholecystectomy had been undertaken without an attempt to first dissect in the triangle of Calot.
Haemorrhage during open cholecystectomy
Troublesome haemorrhage was encountered in seven of the eight patients during the fundus-down dissection of the gallbladder. In six of these the blood loss was noted to be severe. Estimated blood loss was available in five of the procedures and ranged from 1500 ml to 3000 ml. In the seventh patient, bleeding vessels in the liver bed had to be oversewn, which suggests that the haemorrhage was also serious. The right portal vein was identified intraoperatively as the source of blood loss in three patients. Two of these patients also suffered haemorrhage from an artery identified in one note as the right hepatic artery. The artery involved in the other patient was probably also the right hepatic artery as this vessel was later shown to be injured. In two other patients, bleeding occurred from an unidentified vein. In both of these patients and in the patient in whom vessels in the liver were oversewn, the right portal vein or main portal vein were later determined to have been injured. Therefore, the portal vein was the major source of blood loss in six of seven patients with serious intraoperative haemorrhage.
Extent of vascular and biliary injuries
Vascular injuries
Vascular injuries consisted of a combined injury to an artery and a vein except in one patient, who suffered an injury to the proper hepatic artery only. In five patients the right hepatic artery and the right portal vein were injured. In the other two patients the main portal vein and either the proper or right hepatic artery were injured (Table 2).
Table 2.
Location, extent and initial treatment of vasculobiliary injuries
| Patient | Injured vein | Injured artery | Biliary injury | Intraoperative recognition and treatment at primary institution |
|---|---|---|---|---|
| 1 | Right portal | Right hepatic | CBD transection LHD laceration | Sutured portal vein. Primary repair of CBD (end-to-end) and LHD (over T-tube). Postoperatively referred for management/resection; recovery eliminates need for resection |
| 2 | Right portal | Right hepatic | CBD and CHD at bifurcation | Injury recognized intraoperatively. Artery and vein completely transected. No repair possible and both were sutured off. Right hepatectomy performed 1 h later in the same hospital. Referred for biliary reconstruction |
| 3 | Right portal | Right hepatic | CHD at/above bifurcation | Right portal vein oversewn. Referred in postoperative period (PoD 16) because of biliary leakage/fistula |
| 4 | None | Proper hepatic | Necrosis of the intrahepatic biliary treea | Injury not recognized. Referred on PoD 6 for large biliary fistula |
| 5 | Main portal | Right hepatic | Above confluence | Biliary injury suspected. Bleeding vessels in liver bed oversewn. Referred on PoD 3 for biliary fistula |
| 6 | Right portal | Right hepatic | Right hepatic duct and partial laceration CHDb | Suture of large vein. CHD laceration treated with T-tube. Transection of right portal pedicle unrecognized. Referred on PoD 1 for suspected biliary injury |
| 7 | Main portal | Proper hepatic | CHDc | Ligation of vein ‘1 cm in size’. Transection of hepatoduodenal ligament unrecognized. Referred on PoD 1 for suspected vasculobiliary injury |
| 8 | Right portal | Right hepatic | Above confluenced | Excision of CHD, CBD noted. No repair. T-tube placed. Referred on PoD 4 for biliary injury recognized intraoperatively |
Proper hepatic artery occlusion resulted in necrosis of the biliary tree to the fourth-order branches.
The vasculobiliary injury resulted from division of the right portal pedicle. There was also a laceration of the CHD.
The vasculobiliary injury resulted from division of the hepatoduodenal ligament.
The vasculobiliary injury was associated with injuries to the duodenum and the right colon.
CBD, common bile duct; CHD, common hepatic duct; LHD, left hepatic duct; PoD, postoperative day.
Biliary injuries
The patient with an isolated injury to the proper hepatic artery developed diffuse bile duct necrosis extending to the fourth-order intrahepatic biliary radicals. The other biliary injuries were to the common bile duct, the common hepatic duct or the right and left hepatic ducts (Table 2).
In Patient 5, the right portal pedicle was divided, accounting for the scope of the injury; in Patient 7 the entire hepatoduodenal ligament was divided. In Patient 8 the injury involved the confluence of the right and left hepatic ducts, as well as full-thickness injuries of the anterior wall of the duodenum and the hepatic flexure of the colon. This patient presented with general peritonitis.
In seven patients, injury was diagnosed or suspected intraoperatively. The intraoperative treatments at the time of cholecystectomy are listed in Table 2.
Management at tertiary centres and outcomes
Patients were referred to the tertiary centre from 12 h to 140 days after cholecystectomy (Table 3). Infarction of the whole liver was diagnosed in one patient (Patient 7) (Fig. 1). This patient died hours after laparotomy in which the structures in the divided hepatoduodenal ligament were reconstructed. Infarction of the right liver occurred in six patients. In Patient 2, who suffered infarction of all four segments, the right liver had been resected at the primary hospital. Three other patients had complete infarction of the right liver and all underwent right hepatectomies 24 h to 3 months after the initial cholecystectomy. Two of these patients died postoperatively (Table 3). In two other patients, the infarction of the right liver was partial. One patient survived with conservative treatment (Fig. 2). The other patient also suffered extensive bowel injuries with acute peritonitis (Patient 8). She underwent an emergency liver debridement (Fig. 3) in the course of treatment for the bowel injuries, but no attempt was made to reconstruct the biliary injuries during the emergency operation. Three months after presentation, bowel continuity was restored at a second operation. This patient is awaiting bile duct reconstruction and possible resection of the remnant right liver because of the high level of the injuries on the right side (Fig. 4), as well as partial infarction of that hemiliver. Thus, all seven patients who suffered a combined portal vein and hepatic artery injury developed partial or complete infarction of the liver, six of the right liver and one of the entire liver, and three of these patients died. The patient who had infarction of the bile ducts after injury to the proper hepatic artery underwent an urgent liver transplantation and died of sepsis in the postoperative period. In all, four of the eight patients died after referral. The prognosis for the one patient who remains under treatment is guarded for reasons of age, comorbidities and extent of injury.
Table 3.
Findings and treatment at tertiary centres and outcomes
| Patient | Findings at tertiary centre | Treatment at tertiary centre | Outcome |
|---|---|---|---|
| 1 | T-tube in CBD and LHD Infarction in right liver | Removal of T-tube ERCP insertion of stents on PoD 95 Stenting for 73 days | Conservative treatment of infarction At the 6-month follow-up, partial revascularization/atrophy of the right liver and hypertrophy of the left liver were noted No complaints; normal liver function tests |
| 2 | Right liver absent Hypertrophy of left liver Biliary injury (E1–2) | Hepaticojejunostomy on PoD 140 after initial right hepatectomy | Alive and well 24 months after surgery |
| 3 | Right liver infarction Biliary injury (E1–2) | Right hepatectomy (PoD 76) Hepatico-jejunostomy | Postoperative biloma/leakage percutaneous drainage Died 175 days after hepatectomy Cardiopulmonary failure (after intra-abdominal abscess caused by bile leakage) |
| 4 | Biloma Infarction of biliary tree | Liver transplant (PoD 39) | Postoperative death caused by sepsis at day 14 post-transplant |
| 5 | Infarction of right liver Biliary injury above confluence | Biloma drainage Right hepatectomy and bile duct repair (PoD 90) | Died 6 weeks after hepatectomy and reconstruction |
| 6 | Infarction of right liver | Emergency right hepatectomy (PoD 1) | Alive and well 4 years postoperatively |
| 7 | Infarction of liver | Emergency reconstruction of portal vein, proper hepatic artery and bile duct 20 h after cholecystectomy | Died on PoD 2 |
| 8 | Infarction of right anterior section | Right colectomy with ileostomy Debridement of duodenum and liver Drainage of bilomas; feeding tube | Alive 5 months after injury Intestinal continuity restored 3 months after injury Awaiting bile duct reconstruction |
CBD, common bile duct; LHD, left hepatic duct; ERCP, endoscopic retrograde cholangiopancreatography; PoD, postoperative day.
Figure 1.
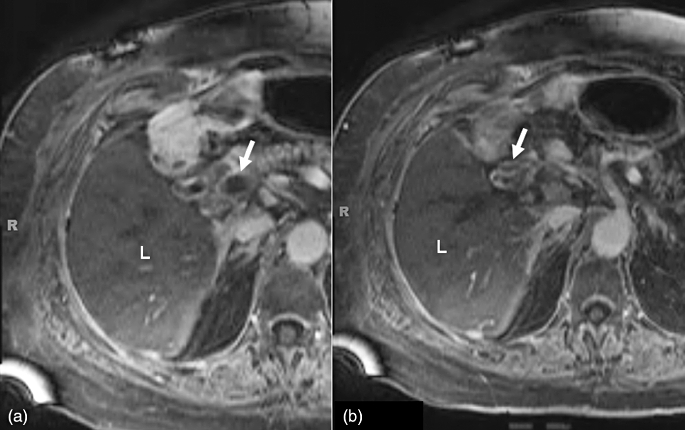
Patient 7. Magnetic resonance imaging shows (a) occluding thrombus in the main portal vein proximal to the site of transection (arrow) and (b) occluding thrombus in the proper hepatic artery proximal to the site of transection (arrow). The liver (L) shows minimal contrast in the veins and was found to be infarcted at surgery
Figure 2.
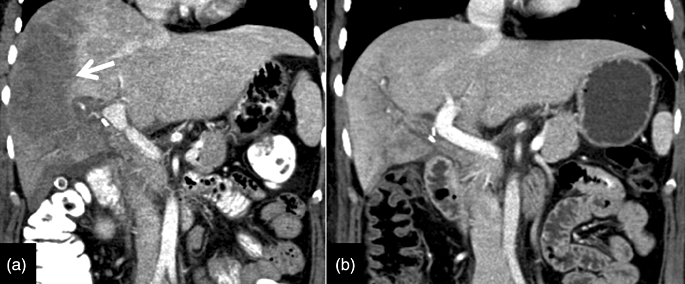
Patient 1. Computed tomography shows (a) partial infarction of the right liver (arrow) on day 6 and (b) revascularization and atrophy of the right liver and mild hypertrophy of the left liver on day 76
Figure 3.

Patient 8. Computed tomography on the day after referral shows partial infarction of the right liver. Long arrow points to infarcted liver. Short arrow points to t-tube inserted at original cholecystectomy
Figure 4.
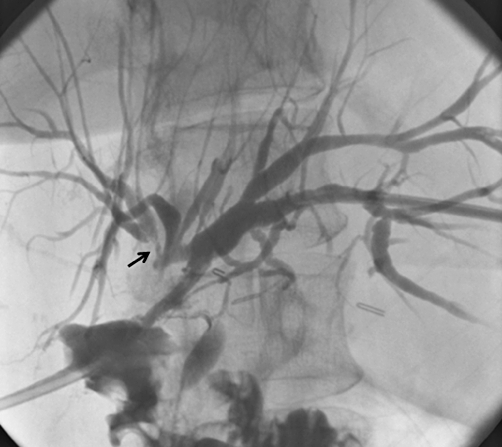
Patient 8. Percutaneous cholangiogram demonstrates an injury above the confluence of the hepatic ducts. The injury is especially high on the right; the end of one of the right ducts shows narrowing, probably indicative of ischaemia
Discussion
Extreme vasculobiliary injuries comprise a small percentage of all vasculobiliary injuries. A recent analysis of the literature1 identified 25 patients with such injuries,4–18 accounting for about 10% of all vasculobiliary injuries reported in the literature.1 This figure corresponds closely to the incidence of 8% estimated in this paper.
This is the first report to focus on the pathogenesis of extreme vasculobiliary injury. The main original finding of this study is that extreme vasculobiliary injuries gathered from two tertiary care centres specializing in repair of biliary injuries19–22 seem to have a number of features in common. All of the cholecystectomies began as laparoscopic procedures. Severe inflammation of the gallbladder, often with contraction of the gallbladder, was present in nearly all patients. Seven of eight procedures were converted because of the severe inflammation and the vasculobiliary injuries in these patients occurred after conversion. A fundus-down cholecystectomy technique was used in all patients. In one patient the fundus-down technique was commenced laparoscopically, whereas in the others it was performed after conversion to an open procedure. There was no clear dissection plane between the liver bed and gallbladder. Serious haemorrhage was encountered when taking the gallbladder off the liver in seven of eight patients. A vasculobiliary injury involving a major hepatic artery and a portal vein occurred in seven of eight patients. Infarction of the liver occurred in seven patients. In the final patient, an injury to the proper hepatic artery resulted in diffuse bile duct infarction. As a consequence of these injuries, one liver transplant and four right hepatectomies were required, four patients died and one patient has not yet completed definitive reconstruction.
In terms of the pathogenesis of these injuries, there are two prominent variables: severe inflammation, and fundus-down cholecystectomy. The authors have previously proposed that these factors in combination may lead to serious biliary or vasculobiliary injury and illustrated the problem in two patients, one of whom is included in this study (the other had a purely biliary injury).23 This study expands our understanding of the mechanism of the injury based on the anatomy of the plate sheath system of the liver and the contents of the right portal pedicle. All but one of the injuries involved a portal vein and a hepatic artery and most involved the right portal vein and right hepatic artery. Thus, this type of injury occurs predominantly to the right portal pedicle or structures close to the right portal pedicle. In the patients in whom the main portal vein or proper hepatic artery were involved, it is likely that these structures were drawn into the area behind and below the gallbladder by contractive inflammation. Comments on the difficulty of finding the plane between the gallbladder and liver are also helpful in elucidating the mechanism of injury.
The bottom of the cystic plate upon which the gallbladder rests inserts into the front of the right portal pedicle (Fig. 5). Should the plane of dissection in a cholecystectomy be behind rather than in front of the cystic plate and the dissection continued downward behind the plate, the fibrous sheath around the right portal pedicle will eventually be encountered (Fig. 5). If this structure is breached, the bile duct and blood vessels within the sheath can be injured. The situation is more hazardous when there is severe chronic inflammation with contractive fibrosis. Under these circumstances, the cystic plate may become short and thick (Fig. 5b). The plane between the gallbladder and the plate is obliterated and it is very difficult to ascertain whether the dissection is on or within the plate. If it is within the cystic plate, the right portal pedictable will be reached. Because the cystic plate is shortened by contractive inflammation, the distance from the top of the cystic plate to the right portal pedicle may be markedly reduced to ≤3–4 cm (Fig. 5b). Thus, all may appear to be going well as the thickened gallbladder appears to be coming off the cystic plate until the almost inevitable large haemorrhage occurs from the right portal vein and/or an adjacent vessel. Control of haemorrhage almost always results in the obstruction of one of the major arteries and veins, with consequent hepatic ischaemia, as well as biliary injury.
Figure 5.
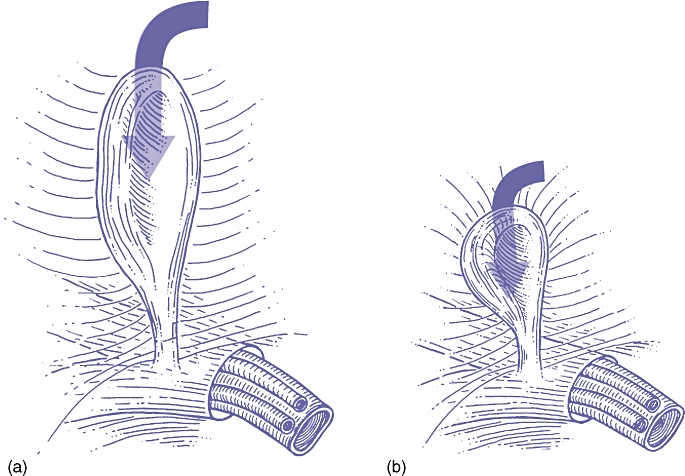
The relationship between the cystic plate and the right portal pedicle (a) under normal circumstances and (b) in the presence of severe contractive inflammation. The cystic plate attaches to the anterior surface of the right portal pedicle. Dissection downward in the plane deep to the plate (arrow) will lead to the pedicle, with injury to the vessels and bile duct. When inflammation is mild, as in (a), entry into the plane is usually readily detected by visualization of liver tissue. When there is severe contractive inflammation the cystic plate is thickened, as in (b), and determining the position of the dissection in relation to the plate is difficult. In addition, the plate is foreshortened so that the distance from the top of the plate to the pedicle is very short. Both of these factors greatly increase the likelihood of injury to the pedicle
To prevent this injury, surgeons must be aware that fundus-down cholecystectomy in the face of severe inflammation will tend to bring the dissection onto the right portal pedicle with predicable consequences. The desire to complete a cholecystectomy should be very secondary to the aim of completing the operation safely. This aim reflects an attitude we have referred to as having a proper ‘culture of cholecystectomy’.24 Contracture of the gallbladder, with puckering of the liver, adhesion of pericholecystic structures and difficulty in finding the gallbladder can serve as signs to warn the surgeon not to attempt to remove the gallbladder from above, but, instead, to perform a limited safe procedure such as cholecystostomy or subtotal cholecystectomy, in which the gallbladder is not taken off the liver bed at all.25 If open cholecystectomy is attempted in the presence of severe inflammation, a trial dissection in the triangle of Calot should be made. Difficulty in this dissection should alert the surgeon to the danger of proceeding further and the potential hazard of taking the gallbladder down from above under these circumstances. Opening the gallbladder at an early stage during dissection from the liver may be helpful. This permits the introduction of a finger into the gallbladder, which may help the surgeon to localize the gallbladder wall. This might prevent dissection towards the liver and the right portal pedicle. It is also a first step in the performance of subtotal cholecystectomy. When the gallbladder is very sclerotic and bound down to surrounding tissues, serious consideration should be given to discontinuing the laparoscopic procedure and referring the patient to a hepatobiliary centre rather than attempting an open procedure under these difficult circumstances. This advice is becoming more relevant as the number of surgeons with substantial experience in difficult open cholecystectomy is continuously diminishing.
In summary, extreme vasculobiliary injuries seem to occur when fundus-down cholecystectomy is attempted in the presence of severe inflammation in and around the gallbladder, usually after conversion from laparoscopic cholecystectomy. Severe haemorrhage is common and is caused by dissection behind the cystic plate into the right portal pedicle. The prevention of such injuries requires the surgeon to recognize the features of severe inflammation, particularly severe contractive inflammation, and to avoid using the fundus-down technique when these are present.
Conflicts of interest
None declared.
References
- 1.Strasberg SM, Helton WS. An analytical review of vasculobiliary injury in laparoscopic and open cholecystectomy. HPB. 2011;13:1–14. doi: 10.1111/j.1477-2574.2010.00225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davidoff AM, Pappas TN, Murray EA, Hilleren DJ, Johnson RD, Baker ME, et al. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215:196–202. doi: 10.1097/00000658-199203000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stewart L, Robinson TN, Lee CM, Liu K, Whang K, Way LW. Right hepatic artery injury associated with laparoscopic bile duct injury: incidence, mechanism, and consequences. J Gastrointest Surg. 2004;8:523–530. doi: 10.1016/j.gassur.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 4.Felekouras E, Megas T, Michail OP, Papaconstantinou I, Nikiteas N, Dimitroulis D, et al. Emergency liver resection for combined biliary and vascular injury following laparoscopic cholecystectomy: case report and review of the literature. South Med J. 2007;100:317–320. doi: 10.1097/01.smj.0000242793.15923.1a. [DOI] [PubMed] [Google Scholar]
- 5.Frilling A, Li J, Weber F, Fruhauf NR, Engel J, Beckebaum S, et al. Major bile duct injuries after laparoscopic cholecystectomy: a tertiary centre experience. J Gastrointest Surg. 2004;8:679–685. doi: 10.1016/j.gassur.2004.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Madariaga JR, Dodson SF, Selby R, Todo S, Iwatsuki S, Starzl TE. Corrective treatment and anatomic considerations for laparoscopic cholecystectomy injuries. J Am Coll Surg. 1994;179:321–325. [PMC free article] [PubMed] [Google Scholar]
- 7.Laurent A, Sauvanet A, Farges O, Watrin T, Rivkine E, Belghiti J. Major hepatectomy for the treatment of complex bile duct injury. Ann Surg. 2008;248:77–83. doi: 10.1097/SLA.0b013e31817b65f2. [DOI] [PubMed] [Google Scholar]
- 8.Strasberg SM, Helton WS. Error traps and vasculobiliary injury in laparoscopic and open cholecystectomy. J HPB Surg. 2008;15:284–292. doi: 10.1007/s00534-007-1267-9. [DOI] [PubMed] [Google Scholar]
- 9.Ragozzino A, Lassandro F, De Ritis R, Imbriaco M. Value of MRI in three patients with major vascular injuries after laparoscopic cholecystectomy. Emerg Radiol. 2007;14:443–447. doi: 10.1007/s10140-007-0617-x. [DOI] [PubMed] [Google Scholar]
- 10.Nishio H, Kamiya J, Nagino M, Uesaka K, Kanai M, Sano T, et al. Right hepatic lobectomy for bile duct injury associated with major vascular occlusion after laparoscopic cholecystectomy. J HPB Surg. 1999;6:427–430. doi: 10.1007/s005340050145. [DOI] [PubMed] [Google Scholar]
- 11.Robertson AJ, Rela M, Karani J, Steger AC, Benjamin IS, Heaton ND. Laparoscopic cholecystectomy injury: an unusual indication for liver transplantation. Transpl Int. 1998;11:449–451. doi: 10.1007/s001470050173. [DOI] [PubMed] [Google Scholar]
- 12.de Santibanes E, Palavecino M, Ardiles V, Pekolj J. Bile duct injuries: management of late complications. Surg Endosc. 2006;20:1648–1653. doi: 10.1007/s00464-006-0491-8. [DOI] [PubMed] [Google Scholar]
- 13.Thomson BN, Parks RW, Madhavan KK, Garden OJ. Liver resection and transplantation in the management of iatrogenic biliary injury. World J Surg. 2007;31:2363–2369. doi: 10.1007/s00268-007-9234-9. [DOI] [PubMed] [Google Scholar]
- 14.Buell JF, Cronin DC, Funaki B, Koffron A, Yoshida A, Lo A, et al. Devastating and fatal complications associated with combined vascular and bile duct injuries during cholecystectomy. Arch Surg. 2002;137:703–708. doi: 10.1001/archsurg.137.6.703. [DOI] [PubMed] [Google Scholar]
- 15.Yan JQ, Peng CH, Ding JZ, Yang WP, Zhou GW, Chen YJ, et al. Surgical management in biliary restricture after Roux-en-Y hepaticojejunostomy for bile duct injury. World J Gastroenterol. 2007;13:6598–6602. doi: 10.3748/wjg.v13.i48.6598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wudel LJ, Jr, Wright JK, Pinson CW, Herline A, Debelak J, Seidel S, et al. Bile duct injury following laparoscopic cholecystectomy: a cause for continued concern. Am Surg. 2001;67:557–563. [PubMed] [Google Scholar]
- 17.Salman B, Akyurek N, Onal B, Cindoruk M. Combined proper hepatic artery and common hepatic duct injury in open cholecystectomy: case report and review of the literature. Adv Ther. 2007;24:639–647. doi: 10.1007/BF02848789. [DOI] [PubMed] [Google Scholar]
- 18.Mathisen O, Soreide O, Bergan A. Laparoscopic cholecystectomy: bile duct and vascular injuries: management and outcome. Scand J Gastroenterol. 2002;37:476–481. doi: 10.1080/003655202317316123. [DOI] [PubMed] [Google Scholar]
- 19.de Reuver PR, Grossmann I, Busch OR, Obertop H, van Gulik TM, Gouma DJ. Referral pattern and timing of repair are risk factors for complications after reconstructive surgery for bile duct injury. Ann Surg. 2007;245:763–770. doi: 10.1097/01.sla.0000252442.91839.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Reuver PR, Rauws EA, Bruno MJ, Lameris JS, Busch OR, van Gulik TM, et al. Survival in bile duct injury patients after laparoscopic cholecystectomy: a multidisciplinary approach of gastroenterologists, radiologists, and surgeons. Surgery. 2007;142:1–9. doi: 10.1016/j.surg.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 21.de Reuver PR, Sprangers MA, Rauws EA, Lameris JS, Busch OR, van Gulik TM, et al. Impact of bile duct injury after laparoscopic cholecystectomy on quality of life: a longitudinal study after multidisciplinary treatment. Endoscopy. 2008;40:637–643. doi: 10.1055/s-2008-1077444. [DOI] [PubMed] [Google Scholar]
- 22.Winslow ER, Fialkowski EA, Linehan DC, Hawkins WG, Picus DD, Strasberg SM. ‘Sideways’: results of repair of biliary injuries using a policy of side-to-side hepatico-jejunostomy. Ann Surg. 2009;249:426–434. doi: 10.1097/SLA.0b013e31819a6b2e. [DOI] [PubMed] [Google Scholar]
- 23.Strasberg SM. Error traps and vasculobiliary injury in laparoscopic and open cholecystectomy. J HPB Surg. 2008;15:284–292. doi: 10.1007/s00534-007-1267-9. [DOI] [PubMed] [Google Scholar]
- 24.Strasberg SM. Biliary injury in laparoscopic surgery: part 2. Changing the culture of cholecystectomy. J Am Coll Surg. 2005;201:604–611. doi: 10.1016/j.jamcollsurg.2005.04.032. [DOI] [PubMed] [Google Scholar]
- 25.Bornman PC, Terblanche J. Subtotal cholecystectomy: for the difficult gallbladder in portal hypertension and cholecystitis. Surgery. 1985;98:1–6. [PubMed] [Google Scholar]


