Abstract
Background
Right-sided ligamentum teres (RSLT) is a congenital anomaly that is sometimes encountered during hepatobiliary surgeries. However, a valid protocol for describing the segmental anatomy of livers with RSLT has not been established, and confusions or anatomic misunderstandings have been a major problem.
Methods
The vascular architecture and morphological characteristics were investigated in 35 livers with RSLT using three-dimensional (3D) simulations.
Results
Couinaud's four sectors and three hepatic veins were clearly distinguished in the liver with RSLT using 3D simulations. The ligamentum teres was connected with the right paramedian portal pedicle, and the long axis of the cystic fossa was always observed on the left of the ligamentum teres in all 35 livers. However, when the main portal scissura was visualized using 3D simulation, the gallbladder was always located on the border of either side of the hemilivers, and the malposition of the gallbladder was not confirmed.
Conclusions
Although the right-sided components of the livers are well developed as a result of the right-dominant distribution of the feeding vessels in livers with RSLT, the basic segmental structure defined by the four sectors and the three hepatic veins are as well preserved as those in the typical liver anatomy.
Keywords: right-sided round ligament, left-sided gallbladder, liver anatomy, liver resection, 3D simulation
Introduction
Right-sided ligamentum teres (RSLT) is a congenital anomaly in which the foetal umbilical vein is connected to the right paramedian trunk of the portal vein. The reported frequency of this anomaly ranges from 0.2% to 1.2%1,2 and is known to accompany several intrahepatic vascular anomalies.1–7 Several observational studies on the vascular architecture and embryologic origin of RSLT have been reported,1–8 and reports of laparoscopic cholecystectomy or hepatectomy have been described. However, because of the rarity of this anomaly, previous reports have been unable to prove anatomic hypotheses. Therefore, a conclusive theory for the embryologic origin and vascular architecture of RSLT has not yet been established.
When liver tumours are associated with major vascular anomaly, such as RSLT, precise knowledge of the principle vascular architecture is essential for surgeons to conduct safe liver resection. However, confusion remains regarding the segmental anatomy of the liver accompanying RSLT,1 and as a result, this anomaly has been incorrectly termed as ‘left-sided gallbladder’ or ‘fusion of the planes’ in previous reports.4
New anatomic evidence is provided from three-dimensional (3D) analyses of 35 livers with RSLT and a valid segmental anatomy for livers with RSLT is proposed.
Patients and methods
Subjects and 3D image reconstruction
The subjects were 35 patients (median age, 71 years; range, 32–86; male/female ratio, 21 : 14) who were incidentally diagnosed as having RSLT among 8050 consecutive image readings performed by one radiologist (M.A.) between May 2002 and January 2009 at the University of Tokyo Hospital.
In addition, 100 consecutive healthy donor candidates for living donor liver transplantation (median age, 37 years; range, 20–63 years; male : female ratio, 52 : 48) who underwent dynamic computed tomography (CT) scanning as pre-operative assessment between February 2004 and May 2009 were included as a reference group with typical liver anatomy.
Three-dimensional reconstruction of the vascular structures and volumetric measurements of the liver segments were performed using 3D-CT software (Organs Volume Analysis; Hitachi Medico Inc, Tokyo, Japan), as previously reported.9
Terminology and anatomic exploration
Because the 3D simulations used in the present study were based on the ‘portal’ or ‘venous’ distributions, Couinaud's conventional terminologies ‘sector’ and ‘segment’ were used and are defined in the addendum in Brisbane 2000 Terminology of Liver Anatomy and Resections,10 to describe the basic structure of the liver.
Vascular definition based on the 3D vascular simulations
Because of the coexisting anomalies in the vascular ramification patterns of livers with RSLT, the identification of significant vessels corresponding to the sectoral portal pedicles and venous trunks in the typical liver anatomy is sometimes difficult. Therefore, an original vascular naming algorithm was devised for anatomic exploration based on the anatomic principles described by Couinaud.11
Couinaud defined four sectors [right lateral sector (S6 + 7), right paramedian sector (S5 + 8), left paramedian sector (S3 + 4), and left lateral sector (S2)] which are outlined by three hepatic veins (right, middle and left hepatic veins). In the present study, these four sectors and three hepatic veins were sought using 3D simulation images.12
First, the right lateral portal pedicle (PRL) is identified (Fig. 1a) and its territory (i.e. the right lateral sector) is visualized in a 3D fashion (Fig. 1b). According to Couinaud's theory, the hepatic veins usually border the sectors. Therefore, a prominent vein running on the intersectoral surface of the right lateral sector can be defined as the right hepatic vein (RHV) (Fig. 1c). Once the drainage areas of the RHV have been visualized (Fig. 1d, e), another significant portal branch can be confirmed next on the border of the RHV region. Because either side of the paramedian portal pedicles indicates the watersheds of the hepatic veins, the portal branch identified here is the right paramedian portal pedicle (Fig. 1f). Continuing with the same ‘identification and 3D visualization procedures’, the middle hepatic vein (MHV), the left paramedian portal pedicle (PLPM) and the left hepatic vein (LHV) can be confirmed in this order, and finally, the left lateral portal pedicle (PLL) can be identified on the left of the LHV (Fig. 1g–i).
Figure 1.
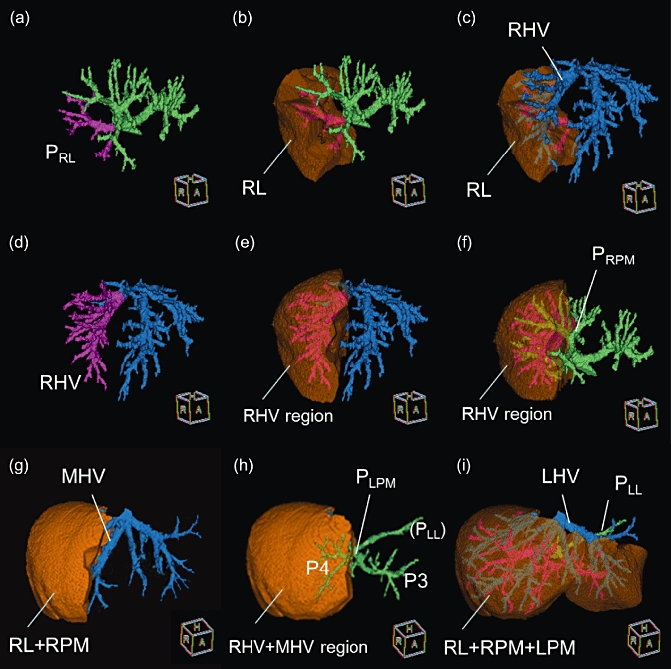
Step-by-step definitions of the vasculature in livers with right-sided ligamentum teres (RSLT). (a) Three-dimensional configurations of portal branches (green) and the right lateral portal pedicle (PRL) (pink). (b) Visualization of the right lateral sector. (c) When the hepatic veins (blue) are superimposed on the 3D images of right lateral sector, the right hepatic vein (RHV) is visible on the sectoral border. (d) The RHV (pink) is identified. (e) The drainage area of the RHV is then visualized. (f) The right paramedian portal pedicle (PRPM) is visible on the intersectoral plane emerging after visualizing of the RHV. (g) The MHV was confirmed after visualization of the right hemiliver (RL + RPM). RL, right lateral sector; RPM, right paramedian sector. (h) The left paramedian portal pedicle (PLPM) is visible in the umbilical fissure. (i) The left hepatic vein (LHV) was exposed on the sectoral border and the left lateral portal pedicle (PLL) can also be seen behind the LHV
After full confirmation of the four sectoral portal pedicles and three venous trunks, the portal branches and venous tributaries on either side of the paramedian sector can be further sub-classified. First, prominent veins along the respective paramedian portal pedicles and the watersheds of the main venous trunks (i.e. RHV. MHV and LHV) are called V8i13 on the right and the umbilical fissure vein (UFV)11,14 on the left, according to the definitions used for the typical liver anatomy, respectively. Second, the third-order portal tributaries are divided into two groups in relation to these landmark veins. The branches from the right paramedian portal pedicle are subclassified into ventral or dorsal branches on the right in relation to the V8i, and those from the left paramedian portal pedicle are named as P3 or P4 as in the typical liver anatomy in relation to the UFV.
The definitions of the accessory right hepatic veins such as middle right hepatic vein (MRHV) and the inferior right hepatic vein (IRHV), are made in accordance with Couinaud's original descriptions.11
Definition of the liver segment
In the present study, the liver was divided into four sectors and the caudate lobe (Segment 1) according to the 3D distributions of the portal branches. Additionally, either side of the paramedian sector was sub-divided according to venous drainage patterns as represented in Fig. 2. The right paramedian sector was subdivided into ventral and dorsal portions (i.e. MHV and RHV drainage areas, respectively) and the left paramedian sector was subdivided into Segment 3 and 4 (LHV and MHV drainage areas, respectively). Segment 4, the key segment to explore the segmental architectures of the liver with RSLT, was defined as the region which is fed by the left paramedian portal pedicle and drained by the MHV.
Figure 2.
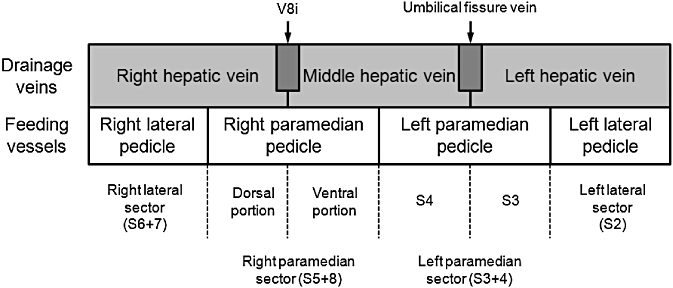
Classification of liver segments according to feeding and drainage patterns. Four sectors were first defined as the regions fed by 2nd-order portal pedicles. Then, either side of the paramedian sector was further sub-divided according to the drainage veins. The right paramedian sector is divided into ‘longitudinal’ two parts: ventral and dorsal portions based on the venous drainage patterns
Data analysis
Clinical data were recorded using an Excel 2010 (Microsoft) spreadsheet and analysed using the statistical software JMP 9 (SAS Institute Japan, Tokyo, Japan). For the statistical analysis, a non-parametric method was used. A value of P < 0.05 was considered statistically significant. All the analyses in the present study were performed in accordance with the ethical guidelines for clinical studies at the University of Tokyo Hospital.
Results
Morphological overview
Livers with RSLT had a bilobar shape with a deep umbilical fissure at the site where the ligamentum teres was attached. The fundus of the gallbladder was always located to the left or just beneath the ligamentum teres (Fig. 3a). When observing the gallbladder in relation to the ligamentum teres, the cholecystic axis (the long axis of the gallbladder attaching site to the liver) was deviated by 31.1 ± 13.7 [mean ± standard deviation (SD)] (range, 6–64°) to the left from the umbilical portion of the portal vein in the RSLT, whereas this axis was deviated by 39.3 ± 23.0°(range, 16 −98°) to the right in the typical liver anatomy (Fig. 3b).
Figure 3.
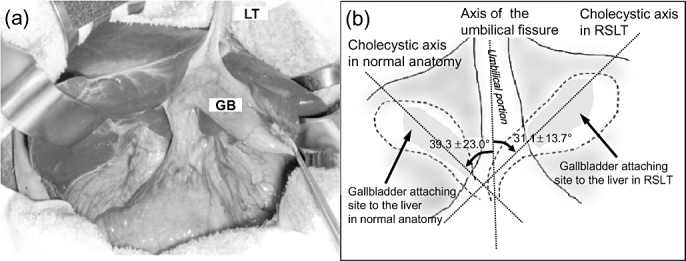
Relation between the umbilical portion and the gallbladder in livers with right-sided ligamentum teres (RSLT) and those with the typical liver anatomy. (a) Surgical picture of RSLT. The gallbladder (GB) is located to the left of the ligamentum teres (LT). (b) Angles between the umbilical axis and the cholecystic axis. The gallbladder was always located to the left in relation to the ligamentum teres
The shape of the caudate lobe and the position of the ligamentum venosum (LV) in the livers with RSLT were similar to those in the typical liver anatomy. When observed in axial images, the umbilical portion was always tilted to the right (49.7 ± 20.1°from the vertical plane) in the livers with RSLT (Fig. 4b), whereas that in the typical liver anatomy was almost parallel to the vertical plane (5.2 ± 11.4°to the left from the vertical plane) (Fig. 4a). In the livers with RSLT, the groove between the left lobe and the caudate lobe (i.e. the groove of the LV) always reached deeply into the portal bifurcation (Fig. 4b), whereas it usually terminated at the level of the P2 branches from the left portal vein in the typical liver anatomy (Fig. 4a). As the left lobe is usually hypoplastic with RSLT, an extrahepatic approach to the portal bifurcation is relatively easy as in the typical anatomy. When the foetal umbilical circulation (i.e. the umbilical vein to the umbilical portion to the ductus venosum) was traced in 3D images, this exhibited a ‘twisted’ shape in the livers with RSLT (Fig. 4d), whereas the route was relatively straight in the typical liver anatomy (Fig. 4c).
Figure 4.
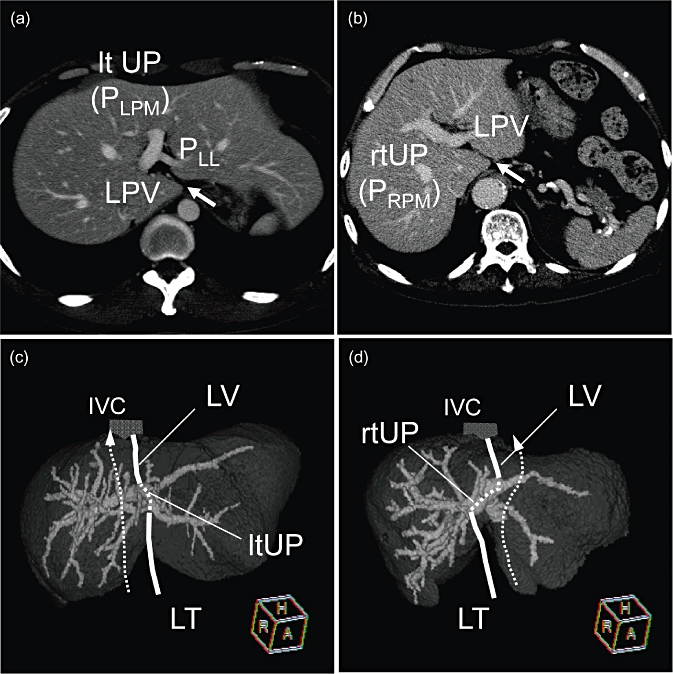
Characteristics of the positions of the umbilical portion and the ligamentum venosum. (a) Typical liver anatomy. The groove containing the ligamentum venosum (arrow) usually terminates where the left portal vein curves to form the umbilical portion (ltUP) ramifying with the left lateral pedicle (PLL). (b) Right-sided ligamentum teres (RSLT). The umbilical portion (rtUP) was always directed to the left towards the ligamentum venosum. The groove for the ligamentum venosum (arrow heads) was deeply cleaved reaching the bifurcation between the rtUP and the left portal vein (LPV). (c, d) The course of umbilical circulation. Intrahepatic portal veins are visualized in a 3D manner. Although the umbilical circulation course was relatively straight in the typical liver anatomy (c), that in the livers with RSLT always exhibited a ‘twisted’ course (d) when observed in 3D images
Portal vein anatomy in livers with RSLT
All four sectoral portal pedicles [i.e. right lateral (PRL), right paramedian (PRPM), left paramedian (PLPM) and left lateral (PLL)] could be distinguished in all 35 RSLT livers. The ligamentum teres was always attached to the PRPM, which formed the umbilical portion in all 35 livers. The PLPM and PLL usually formed various lengths of the common trunk [i.e. the left portal vein (LPV)]. The portal venous ramification patterns at the hepatic hilum were classified into three types according to the origin of the PRL, as demonstrated in Fig. 5: (i) bifurcation type (10, 28.6%), (ii) trifurcation type (8, 23%) and (iii) independent right lateral type (17, 48.6%).
Figure 5.
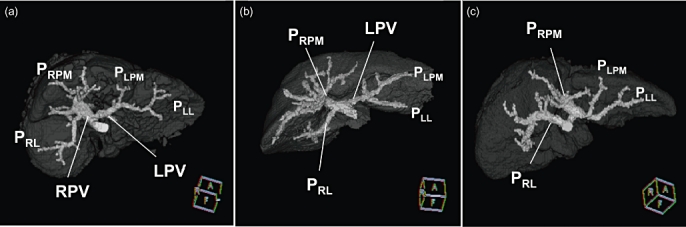
Three portal ramification patterns in livers with right-sided ligamentum teres (RSLT). (a) Bifurcation type (n = 10), (b) trifurcation type (n = 8) and (c) independent right lateral type (n = 17). PRL, right lateral portal pedicle; PRPM, right paramedian portal pedicle; PLPM, left paramedian portal pedicle; PLL, left lateral portal pedicle; LPV, left portal vein; and RPV, right portal vein
In the bifurcation type, two portal trunks (i.e. the right and left portal veins) were formed. The PRL originated from the right umbilical portion as already reported by Nagai et al.1 The trifurcation type had a significant umbilical portion as an extension of the main portal vein. The PRL and the left portal vein originated from the umbilical portion at the same level. This ramification pattern corresponds to the anomaly reported by Yang et al.7 The independent right lateral type was the most common pattern in livers with RSLT, as reported previously.1–6
Because the right side of the liver was well developed and the left side was relatively hypoplastic in the livers with RSLT, the third-order tributaries from the PRPM were usually thick and were easily subclassified into ventral or dorsal branches. On the other hand, the tributaries from the PLPM were relatively thin and difficult to distinguish clearly in the livers with RSLT.
Classification of the branches derived from the umbilical portion (i.e. the right paramedian branches in RSLT and left ones in typical anatomy) seemed relatively easy because of the presence of an umbilical fissure which clearly marks the watershed of the venous drainage area. On the other hand, clear classification of the opposite side of the paramedian branches (i.e. the left paramedian pedicle in RSLT and right ones in typical anatomy) was relatively difficult as a consequence of the hypoplasia and the absence of extrahepatic landmarks such as a umbilical fissure.
Hepatic vein anatomy in livers with RSLT
In contrast to the various morphologies of the portal venous system, the ramification patterns of the hepatic veins in the livers with RSLT were relatively constant and were similar to those in the typical liver anatomy. In all 35 livers, the LHV and the MHV formed a common trunk and the RHV was originated independently from the right wall of the IVC.
As shown in Fig. 6, the venous drainage areas in the livers with RSLT were symmetrical on either side of the Rex-Cantlie line, similar to the symmetry observed in the typical liver anatomy. The umbilical fissure was always located at the watershed between the MHV and the RHV in the livers with RSLT, whereas it was usually observed between the MHV and the LHV in the typical liver anatomy.
Figure 6.
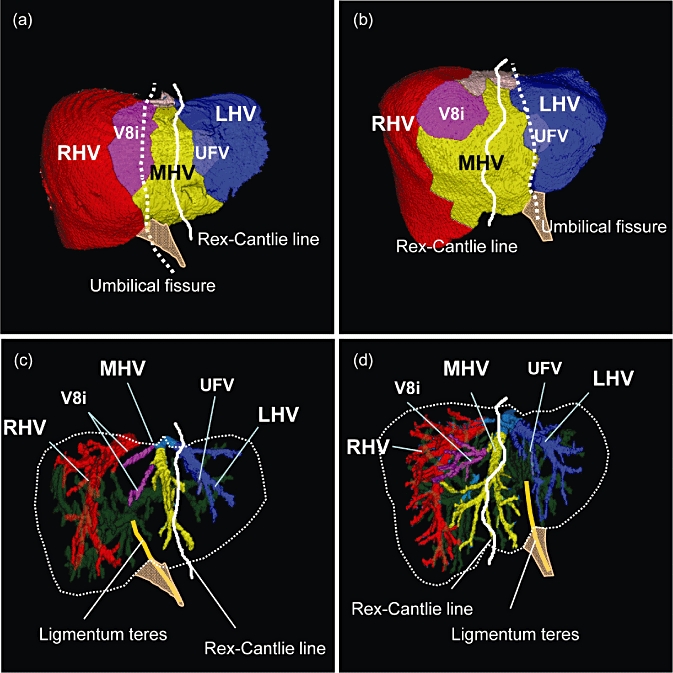
The distribution of venous drainage areas. (a, c) RSLT case, (b, d) typical liver anatomy. Each venous drainage area is represented in a different colour on the liver surface. The white line represents the simulated Rex-Cantlie line and the dotted line indicates the umbilical fissure. The umbilical fissure is located between the areas of the middle hepatic vein (MHV) and the right hepatic vein (RHV) in the livers with right-sided ligamentum teres (RSLT), while it is usually observed between the MHV and the LHV in the typical liver anatomy
Hepatic arterial anatomy in the livers with RSLT
In all, 32 out of 35 RSLT livers had CT arterial phase images or available angiograms (Fig. 7). In the livers with RSLT, the artery for the right paramedian sector was well developed and usually had two distinct branches feeding either the ventral or dorsal regions, respectively (ARPM-v and ARPM-d). In most instances, the hepatic arteries for the left hemiliver branched independently from the proper hepatic artery or from the left gastric artery (Type 1-i, ii, iii and Type 3-i, ii) (26, 81%). In the remaining livers, the left hepatic arteries were derived from the ARPM-v (Type 2) (5, 16%) or the left paramedian artery formed a common trunk with the right paramedian artery (Type 3-iii) (1, 3%). No specific correlation between the portal ramification and the arterial branching pattern was identified in the present series.
Figure 7.
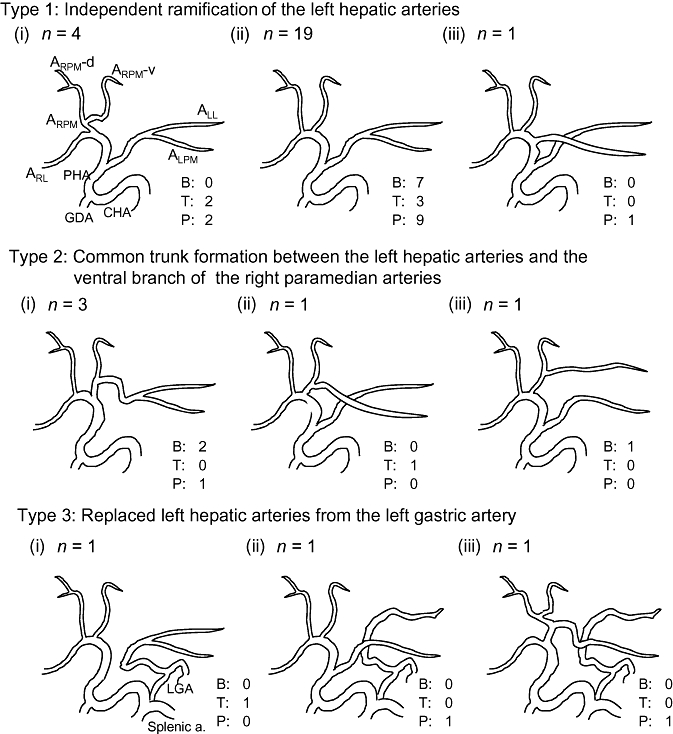
Ramification patterns of the hepatic arteries in 32 right-sided ligamentum teres (RSLT) patients. The frequency of each ramification pattern is indicated on the right lower side of the respective schemes, stratified according to the portal ramification pattern. B, bifurcation type; T, trifurcation type; P, independent right lateral type. ARL, right lateral artery; ARPM, right paramedian artery; ARPM-v, ventral branch; ARPM-d, dorsal branch; ALPM, left paramedian artery; ALL, left lateral artery; PHA, proper hepatic artery; CHA, common hepatic artery; GDA, gastroduodenal artery; LGA, left gastric artery
Position of the gallbladder
When the right or left hemiliver was visualized in 3D simulations, the gallbladder was always observed on the main portal scissura between each side of the hemiliver (Fig. 8). Malposition of the gallbladder was not observed in the present series of 35 livers.
Figure 8.
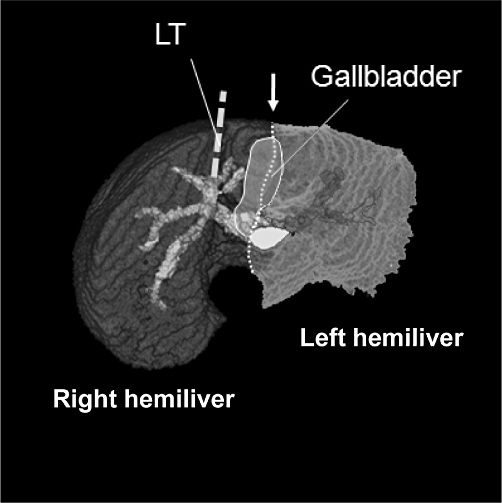
Position of the gallbladder in relation to vascular distributions. When the intersectoral plane between each side of the hemiliver (arrow) is visualized in 3D simulation, the gallbladder was always observed on the sectoral border in 35 right-sided ligamentum teres (RSLT) cases. LT, ligamentum teres
Segmental anatomy and volume data in livers with RSLT
The segmental volume data for the RSLT patients and 100 healthy donors are summarized in Table 1. The mean total liver volumes were similar between the two groups (1040 mL vs. 1138 mL, P = 0.05). In RSLT livers, the proportion of the left lobe (S2-3) was larger and the left hemiliver (S2-4) was smaller than those in the typical liver anatomy (P < 0.0001). Regarding the segmental proportions, either side of the lateral sectors and the dorsal segment of the right paramedian sector were larger than those in the typical liver anatomy, whereas the left paramedian sector (S3-4) and the ventral segment of the right paramedian sector were significantly smaller.
Table 1.
Comparison of segmental proportions in the whole liver
| RSLT (n = 35)* | Typical anatomy (n = 100) | P | |
|---|---|---|---|
| Total liver volume (ml) | 1040 ± 183 ml | 1138 ± 209 ml | 0.05 |
| Left lobe (S2-3) | 29.8 ± 7.3% | 18.3 ± 3.9% | <0.0001 |
| Right lobe (S4-8) | 70.1 ± 7.3% | 75.7 ± 5.5% | |
| Left hemiliver (S2-4) | 22.7 ± 6.4% | 33.2 ± 4.8% | <0.0001 |
| Right hemiliver (S5-8) | 74.3 ± 7.5% | 63.0 ± 5.3% | |
| Left lateral sector (S2) | 11.3 ± 5.6% | 8.3 ± 3.0% | 0.014 |
| Left paramedian sector (S3 + 4) | 10.0 ± 4.1% | 21.3 ± 4.1% | <0.0001 |
| Segment 3 | 5.4 ± 3.4% | 12.4 ± 4.2% | <0.0001 |
| Segment 4 | 5.5 ± 4.4% | 9.0 ± 0.4% | <0.0001 |
| Right paramedian sector (S5 + 8) | 39.4 ± 13.4% | 35.9 ± 6.3% | 0.68 |
| Ventral segment | 13.1 ± 8.9% | 15.2 ± 4.2% | 0.001 |
| Dorsal segment | 22.8 ± 10.2% | 20.4 ± 5.1% | 0.03 |
| Right lateral sector (S6 + 7) | 30.8 ± 13.5% | 25.4 ± 5.5% | 0.14 |
| Caudate lobe (S1) | 2.7 ± 1.7% | 2.4 ± 1.3% | 0.67 |
Figures represent mean ± standard deviation (SD).
Wilcoxon's rank-sum test. RSLT, right-sided ligamentum teres.
Discussion
Historically, topographical reversal between the ligamentum teres and the gallbladder has been attributed to the displacement of the gallbladder and has been termed as a ‘left-sided gallbladder’ since its first description by Hochstetter in 1886.15 A left-sided gallbladder has been defined as ‘the displacement of the gallbladder to the left side of the ligamentum teres without ‘situs inversus viscerum’.16,17 Many case reports have been made, but with advancements in diagnostic modalities, the left-sided gallbladder has begun to be described as an anomaly that is closely associated with right-sided ligamentum teres.18,19
In 1997, Nagai et al.1 reported that the left-sided gallbladder may not represent a true displacement of the gallbladder itself but instead might be attributed to the anomalous connection of the ligamentum teres with the right paramedian portal pedicle. Nevertheless, confusion persists regarding the left-sided gallbladder and RSLT. Because this anomaly is rare, the number of livers reported in previous studies1–7 has been relatively limited and anatomical data have been sparse.
The incidence of RSLT in the present series (0.4% among 8050 consecutive patients) was similar to previously reported frequencies of this anomaly.1,2 Morphologically, the liver had two distinct lobes separated by the umbilical fissure in all 35 RSLT livers. Except for the position of the gallbladder, the external appearances of the livers were almost the same as that for the typical liver anatomy. Although the position of the fundus of the gallbladder varies among individuals, its long axis was always deviated to the left of the umbilical fissure.
The fundus of the gallbladder was always located very close to the ligamentum teres and was frequently located in the groove of the umbilical fissure, because the quadrate lobe was not formed between the umbilical portion and the gallbladder and related to hypoplasia of the ventral segment in the right paramedian sector. However, when the topographical relation with the main portal scissura was confirmed using 3D simulation, the gallbladder was always observed on the border line of either side of the hemiliver, and malposition was not confirmed.
A new theory4,20 from Savier et al. explains the origin of the RSLT to the agenesis of segment 4 as a result of the fusion of the midplane (Rex-Cantrie line) with the umbilical fissure. Applying this theory, however, leads to the 3D relation between the fundus of the gallbladder (not the long axis of the cystic fossa) and the ligamentum teres being referred to as the basis of the fusion of the planes, and the V8i, a significant tributary of the MHV, is misinterpreted as the main trunk of the MHV itself. Also, a prominent vein consisting of two distinct tributaries, which should be identified as the confluence of the MHV and the LHV, is incorrectly identified as the LHV.
In the present study, all four sectoral portal pedicles and three venous trunks could be identified in each of the 35 livers when analysed using 3D simulations. Segment 4, the segment fed by the left paramedian portal pedicle and drained by the MHV, was also constantly identified although its segmental proportion against the whole liver tended to be smaller in the liver with RSLT. Because the fusion of the plane theory was based on subjective morphological observations of the intrahepatic vessels and lacked objective data, such as the shapes of the vascular territories, segmental volumes or embryological explanations, this theory seems to be incorrect. Instead, the origin of the RSLT can be attributed to the mal-connection of the umbilical vein to the right paramedian portal pedicle.
To explain the origin of this anomaly, Hochstetter14 and later Matsumoto21 hypothesized that the persistence of the right umbilical vein instead of the left one may result in the malconnection of the ligamentum teres to the right side. According to our results, the ligamentum teres apparently connected with the right paramedian portal pedicle, and the relation between the ligamantum teres and the portal/hepatic veins was an exact mirror image of the typical liver anatomy on either side of the Rex-Cantlie line. Also, the arterial branching patterns revealed that the right and left arterial branches were clearly separated, as in the typical liver anatomy, in most of the cases, and the liver parenchyma around the umbilical portion was nourished by the branches from the right hepatic artery. This supports the hypothesis that the RSLT is derived from the right-sided foetal components of the liver.
In the field of neonatology, a growing number of cases with persistent right umbilical vein (PRUV) have been diagnosed by ultrasound.22,23 In PRUV, the umbilical vein was notably connected to the right paramedian portal pedicle on the right side of the gallbladder, representing a mirror image of the typical liver anatomy.23 One of the typical findings of PRUV has been described as a ‘twist’ formed by the anomalous umbilical flow coursing from the right to the left through the (right) umbilical portion and then from left to right through the ductus venosum, located in the typical position.24 These findings are compatible with our observations in adult livers with RSLT, in which the vascular sequence clearly formed a twisted route whereas the sequence in typical anatomy usually represented a relatively straight line
This anomaly may give rise to several surgical problems during liver resection. Because the independent ramification of the right lateral portal pedicle is the most common type in RSLT, ligation of the left trunk of the portal vein at the hepatic hilum will result in a lack of portal flow in the left two-thirds of the whole liver if the common trunk of the left portal vein and the right paramedian pedicle is misinterpreted as the left portal vein during a left hemihepatectomy. Similarly, because the main portal scissura is located within the left lobe of the liver in livers with RSLT, ligation of the RHA may cause deprivation of arterial flow to a considerable portion of the liver (i.e. right lobe + right side region of the left lobe). Additionally, because the right-sided components of the liver are well developed in subjects with this anomaly, the drainage area of the RHV is relatively large. Therefore, the ligation or en-bloc resection of the RHV in this anomaly may cause significant venous congestion in the remnant part of the right hemiliver.
Prediction of this anomaly is sometimes difficult. However, strong deviation of the umbilical portion towards the right, a lack of liver parenchyma between the gallbladder and the umbilical portion or a deeply fissured groove for the ligamentum venosum near the level of the portal bifurcation may suggest the presence of RSLT. In addition to these features, routine intra-operative confirmation of the vascular structures using ultrasound or a test clamp before the ligation of prominent vessels may reduce the risk of anatomic misinterpretation and subsequent problematic surgical complications.
In conclusion, 3D analyses of the vascular ramification patterns in 35 patients with RSLT confirmed the anomalous connection of the ligamentum teres with the right paramedian portal pedicle and no malposition of the gallbladder. Considering the embryological, morphological and anatomic evidence, the origin of the RSLT seems to be caused by the persistence of the right umbilical vein.
Acknowledgments
This study was supported by the Health and Labor Sciences Research Grant for Clinical Cancer Research (Grant No. H21-015), and by the grant from the Japanese Foundation for Multidisciplinary Treatment of Cancer.
Conflict of interest
None declared.
References
- 1.Nagai M, Kubota K, Kawasaki S, Takayama T, Bandai Y, Makuuchi M. Are left sided gallbladders really located on the left side? Ann Surg. 1997;225:274–280. doi: 10.1097/00000658-199703000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maetani Y, Itoh K, Kojima N, Tabuchi T, Shibata T, Asonuma K, et al. Portal vein anomaly associated with deviation of the ligamentum teres to the right and malposition of the gallbladder. Radiology. 1998;207:723–728. doi: 10.1148/radiology.207.3.9609896. [DOI] [PubMed] [Google Scholar]
- 3.Uesaka K, Yasui K, Morimoto T, Torii A, Kodera Y, Hirai T, et al. Left-sided gallbladder with intrahepatic portal venous anomalies. J Hepatobiliary Pancreat Surg. 1995;2:425–430. [Google Scholar]
- 4.Lucidarme O, Taboury J, Savier E, Cadi M, Hannoun L, Grenier PA. Fusion of the midplane with the left intersectional plane: a liver anatomical variation revisited with multidetector-row CT. Eur Radiol. 2006;16:1699–1708. doi: 10.1007/s00330-006-0245-y. [DOI] [PubMed] [Google Scholar]
- 5.Rocca JP, Rodriguez-Davalos MI, Burke-Davis M, Marvin MR, Sheiner PA, Facciuto ME. Living-donor hepatectomy in right-sided round-ligament liver: importance of mapping the anatomy to the left medial segment. J Hepatobiliary Pancreat Surg. 2006;13:454–457. doi: 10.1007/s00534-005-1094-9. [DOI] [PubMed] [Google Scholar]
- 6.Hwang S, Lee SG, Park KM, Lee YJ, Ahn CS, Kim KH, et al. Hepatectomy of living donors with a left-sided gallbladder and multiple combined anomalies for adult-to-adult living donor liver transplantation. Liver Transpl. 2004;10:141–146. doi: 10.1002/lt.20007. [DOI] [PubMed] [Google Scholar]
- 7.Yang DM, Kim H, Kang JH, Park CH, Chang SK, Jin W, et al. Anomaly of the portal vein with total ramification of the intrahepatic portal branches from the right umbilical portion: CT features. J Comput Assist Tomogr. 2005;29:461–463. doi: 10.1097/01.rct.0000165905.06031.b0. [DOI] [PubMed] [Google Scholar]
- 8.Gupta R, Miyazaki A, Cho A, Ryu M. Portal vein branching pattern in anomalous right-sided round ligament. Abdom Imaging. 2010;35:332–336. doi: 10.1007/s00261-009-9520-0. [DOI] [PubMed] [Google Scholar]
- 9.Shindoh J, Mise Y, Satou S, Sugawara Y, Kokudo N. Intersegmental plane of the liver is not always flat but uneven – tricks for anatomical liver resection. Ann Surg. 2010;251:917–922. doi: 10.1097/SLA.0b013e3181d773ae. [DOI] [PubMed] [Google Scholar]
- 10.The terminology committee of the IHPBA. The Brisbane 2000 terminology of liver anatomy and resections. HPB. 2000;2:333–339. doi: 10.1080/136518202760378489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Couinaud C. Surgical Anatomy of the Liver Revised. Paris. France: Couinaud; 1989. [Google Scholar]
- 12.Shindoh J, Satou S, Aoki T, Kawaguchi Y, Beck Y, Sugawara Y, et al. Step-by-step vascular naming algorithms for a precise understanding of major anomalies in the liver. Hepatogastroenterology. 2012 doi: 10.5754/hge11454. DOI: 10.5754/hge11454. [DOI] [PubMed] [Google Scholar]
- 13.Cho A, Okazumi S, Makino H, Nagata M, Takiguchi N, Kainuma O, et al. Relation between hepatic and portal veins in the right paramadian sector: proposal for anatomical reclassification of the liver. World J Surg. 2004;28:8–12. doi: 10.1007/s00268-003-7038-0. [DOI] [PubMed] [Google Scholar]
- 14.Shindoh J, Kokudo N, Satou S, Sugawara Y, Makuuchi M. Volumetric analyses of venous variations in the left liver using 3D-CT venography. Hepatogastroenterology. 2006;53:831–835. [PubMed] [Google Scholar]
- 15.Hochstetter F. Anomalien der Pfortader und der Nabelvene in Verbindung mit Defect oder Linkslage der Gallenblase. Arch Anat Entwick. 1886;3:369–384. [Google Scholar]
- 16.Gross RE. Congenital anomalies of the gallbladder. A review of 148 cases. With report of a double gallbladder. Arch Surg. 1936;32:131–162. [Google Scholar]
- 17.Newcombe JF. Left-sided gallbladder. A review of the literature and a case report of a case associated with hepatic duct carcinoma. Arch Surg. 1964;88:494–497. doi: 10.1001/archsurg.1964.01310210168027. [DOI] [PubMed] [Google Scholar]
- 18.Ozeki Y, Onitsuka A, Hayashi K. A case report of left sided gallbladder with anomalous intrahepatic portal venous branching. J Jpn Surg Soc. 1987;11:1644–1649. (in Japanese) [Google Scholar]
- 19.Ozeki Y, Onitsuka A, Hino A. Anomalous branching of intrahepatic portal vein associated with anomalous position of round ligament. Kanzo. 1989;30:372–378. (in Japanese) [Google Scholar]
- 20.Savier E, Taboury J, Lucidarme O, Kitajima K, Cadi M, Vaillant JC, et al. Fusion of the planes of the liver: an anatomic entity merging the midplane and the left intersectional plane. J Am Coll Surg. 2005;200:711–719. doi: 10.1016/j.jamcollsurg.2004.12.017. [DOI] [PubMed] [Google Scholar]
- 21.Matsumoto H. A newer concept of the segmentation of the liver. Jpn J Med Ultrasonics. 1986;13:551–552. (in Japanese) [Google Scholar]
- 22.Jeanty P. Persistent right umbilical vein: an ominous prenatal finding? Radiology. 1990;177:735–738. doi: 10.1148/radiology.177.3.2243979. [DOI] [PubMed] [Google Scholar]
- 23.Kawasaki M, Sase M. Three cases of left-sided gallbladder with persistent right umbilical vein detected antenatally. Jpn J Pediatr Surg. 2008;40:1404–1408. (in Japanese) [Google Scholar]
- 24.Sciaky-Tair Y, Cohen SM, Hochner-Celnikier D, Valsky DV, Nessing B, Yagel S. Three-dimensional power doppler (3DPD) ultrasound in the diagnosis and follow-up of fetal vascular anomalies. Am J Obstet Gynecol. 2006;194:274–281. doi: 10.1016/j.ajog.2005.08.045. [DOI] [PubMed] [Google Scholar]


