Abstract
Background
En-bloc liver resection with the extrahepatic bile duct is mandatory to obtain tumour-free surgical margins and better long-term outcomes in hilar cholangiocarcinoma (CC). One of the most important criteria for irresectability is local extensive invasion to major vessels. As hilar CC Bismuth type IIIB often requires a major left hepatic resection, the invasion of the right hepatic artery (RHA) usually contraindicates this procedure.
Methods
The authors describe a novel technique that allowed an oncological resection in two patients with hilar CC Bismuth type IIIB and contralateral arterial invasion. Arterial reconstruction between the posterior branch of the RHA and the left hepatic artery (LHA) was performed as the first surgical step. Once arterial vascular flow was restored, a left trisectionectomy with caudate lobe resection and portal vein reconstruction was performed.
Results
In both patients an R0 resection was achieved. Both patients made a full recovery and were discharged within 14 days of surgery. Both patients remain free of disease at 18 months.
Conclusions
This new technique allows a R0 resection to be achieved in patients with Bismuth type IIIB hilar CC with contralateral arterial involvement.
Keywords: cholangiocarcinoma < liver, resection < liver
Introduction
Recent advances in liver surgery have led to a more efficient approach to hilar cholangiocarcinoma (CC). There is strong evidence of better survival and long-term outcomes when microscopically tumour-free surgical margins are obtained in these patients.1 En-bloc resections of liver parenchyma with the extrahepatic bile duct is mandatory to manage those tumours with direct hepatic invasion, as well as to accomplish an R0 resection. As a consequence of the frequent invasion of the vascular structures that enter the liver, the achievement of negative surgical margins in these patients is technically demanding and sometimes requires combined vascular resection and reconstruction.2
In hilar CC Bismuth type IIIB, the tumour invades the left bile duct and in some circumstances compromises the left hepatic vascular structures leading to parenchymal atrophy. Given the posterior relationship of the right hepatic artery (RHA) to the common hepatic duct, the expansion of the tumour can lead to involvement of the RHA and or the portal vein (PV) or its branches. As hilar CC Bismuth type IIIB requires an extended left hepatectomy, invasion of the RHA usually renders the patient inoperable.3
The aim of the present study was to describe a novel technique that allowed an oncological resection in two patients with hilar CC Bismuth type IIIB and contralateral arterial invasion.
Methods
Operative technique
During laparotomy, mobilization of the left liver is performed. Dissection of the hepatic pedicle starts at the level of the duodenum proceeding proximally to the hilum performing a complete lymphadenectomy of the celiac axis, the hepatic artery (HA) and the gastrohepatic ligament. Pre-operative findings are confirmed by intra-operative colour-Doppler ultrasound (IOUS). The next step is to dissect and identify the posterior branch of the RHA (segments 6 and 7) inside Rouviere's sulcus. This artery is distant to the tumour and can then be dissected easily. Once this step is accomplished, the distal common bile duct is sectioned as close as possible to its entrance to the pancreas. The common hepatic artery (CHA)-left hepatic artery (LHA) usually runs at the left edge of the hepatic pedicle and is not usually involved in the tumour process. It can be mobilized and released in full length by dividing the origin of the RHA. This allows enough extent to reach Rouviere's sulcus and perform the arterial reconstruction with the posterior branch of the RHA. The LHA-CHA is rotated 90 degrees in an anti-clockwise manner in order to carry out an anastomosis with the arterial branch of segments 6 and 7 using the microscope. The LHA has a similar diameter to the right posterior artery. Occasionally, the proximal portion of the main RHA is clear such that it may also serve as an alternative for the arterial reconstruction with the posterior branch of RHA. Once anastomosis is finished, the future liver remnant (FLR) arterial blood supply is ensured (Fig. 1). Segment 1 is then mobilized to be included in the resection specimen, the left PV is sectioned and the liver parenchyma is transected (left trisectionectomy or extended left hepatectomy) (Fig. 2). If a PV resection is required, it can be done once the section of liver parenchyma is completed, with a guarantee that the remnant liver can tolerate a portal clamping because it has previously assured the arterial vascularization. After the vascular reconstruction is accomplished, the middle and left hepatic veins are divided and sutured. Finally the specimen is removed and biliary reconstruction is performed applying a Roux-en-Y loop. IOUS is then performed to certify the vascular permeability.
Figure 1.
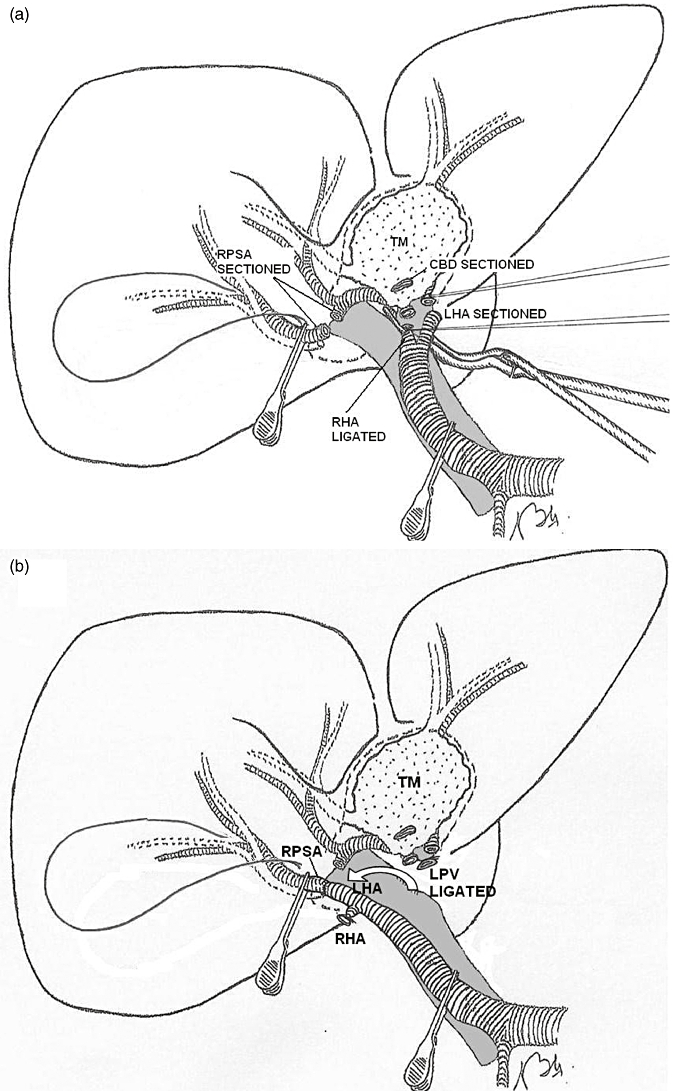
(a) Once a cholecystectomy is performed, the right posterior segment artery (RPSA) is individualized within Rouviere's sulcus. The common bile duct (CBD) is sectioned distally and turned away from the operative field with the specimen. After this, the right hepatic artery (RHA) and the left hepatic artery (LHA) are sectioned with tumour-free margins. (b) The LHA is rotated to the right side of the porta hepatis. This manoeuver allows arterial reconstruction between the LHA and the RPSA. LPV: left portal vein; TM, tumour; HA, hepatic artery
Figure 2.
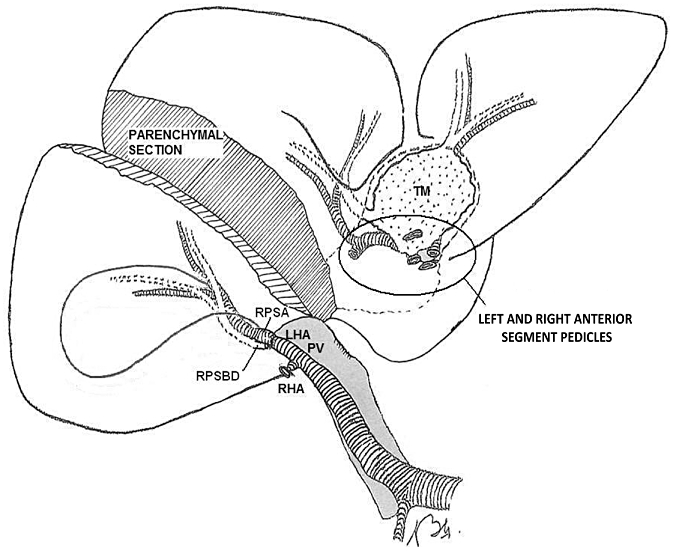
After vascular reconstruction is complete and arterial blood flow is restored, the liver parenchyma is transected. TM, tumour, RHA, right hepatic artery; LHA, left hepatic artery; RPSA: right posterior segment artery; PV, portal vein; RPSBD: right posterior segment bile duct
Patients
A 78-year-old man and a 64-year-old woman presented with jaundice. The pre-operative computed tomography (CT) scan and magnetic resonance imaging (MRI) confirmed hilar CC type IIIB with contralateral vascular invasion. During the surgical procedure, microvascular reconstruction of the right posterior branch of the RHA with the technique described previously was performed (arterial clamping time 18 & 20 min). Both patients underwent a left hepatic trisectionectomy with caudate lobe resection, without the Pringle manoeuver. The tumour was resected en-bloc with the liver parenchyma, the involved PV and the extrahepatic bile duct. PV reconstruction was accomplished by end-to-end anastomosis. The portal clamping time was 22 and 26 min. The operative time was between 5–6 h. No blood transfusion was required for either patient. At the end of the procedure, a Doppler ultrasonography confirmed a patent HA and PV with an adequate blood flow. Both patients made a full recovery and were discharged between 12–14 days after surgery. Pathological examination confirmed hilar CC with disease-free vascular and surgical margins in both patients. At 18 months both patients remain disease free.
Discussion
Achieving negative margins during surgical treatment of hilar CC is not always possible because of the close relationship between the biliary confluence and the afferent liver vascular structures. Unresectablity in most patients is determined by local invasion to major vessels, such as the HA and the PV.1 Therefore, hilar CC occasionally requires combined vascular resection and reconstruction to obtain negative resection margins as a result of involvement of the hilar vasculatures.2
Currently, while resection of the PV is considered a routine procedure when it is compromised,3,4 associated resection of the HA remains controversial because is associated with a higher operative mortality rate, reported to be as high as 33–55%.5
The absence of arterial blood flow can cause liver necrosis and hepatic abscess formation as well as an increase in the complications of biliary anastomosis.6,7 However, Majno et al.6 consider that after resection of the HA, the remaining liver can function adequately with the normal flow of the PV and collateral arteries. Wang et al.8 presented two patients with hilar CC Bismuth type IIIB with contralateral vascular invasion. They performed a left hepatectomy including RHA resection without vascular reconstruction and one of these patients developed liver necrosis and an abscess 3 months later. In the same year, Young et al.9 reported arterialization of the PV as a salvage procedure for a left trisectionectomy as the treatment of a hilar CC because the arterial reconstruction was not possible. Miura et al.10 reported the resection of locally advanced hilar CC after the stepwise arterial embolization. Recent series report the use of arterial vascular reconstruction techniques to increase the resectability of hilar CC when the HA is an obstacle to obtain negative margins.3,5,11,12 In these series vascular reconstruction was performed as the last step after the PV was reconstructed.
In some patients once oncological resection of the tumour is complete, the surgeon might realize that the FLR does not have distal arterial vascular structures for reconstruction. This is a dramatic situation not easily solved.9 It is the authors opinion that one of most important contribution of the described technique is to perform the arterial anastomosis as the first surgical manoeuver before parenchymal transection, in order to avoid the previously described situation.
As liver failure is the leading cause of death in these patients,5 decreasing the ischaemic time during portal reconstruction by ensuring the arterial blood supply to the remnant liver might have a positive impact in the early and late post-operative outcomes as well as limiting the ischaemic insult to the biliary tree.
The reported technique was clinically and technically feasible allowing an oncological resection to be performed in two patients previously judged to be unresectable. If these findings are corroborated in larger series, this novel approach might offer these patients a hope for cure lowering the negative effects of prolonged liver ischaemia.
Conflicts of interest
None declared.
References
- 1.Jarnagin WR, Fong Y, DeMatteo RP, Gonen M, Burke EC, Bodniewicz BSJ, et al. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg. 2001;234:507–517. doi: 10.1097/00000658-200110000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Neuhaus P, Jonas S, Bechstein WO, Lohmann R, Radke C, Kling N, et al. Extended resections for hilar cholangiocarcinoma. Ann Surg. 1999;230:808–818. doi: 10.1097/00000658-199912000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagino M, Nimura Y, Nishio H, Ebata T, Igami T, Matsushita M, et al. Hepatectomy with simultaneous resection of the portal vein and hepatic artery for advanced perihilar cholangiocarcinoma: an audit of 50 consecutive cases. Ann Surg. 2010;252:115–123. doi: 10.1097/SLA.0b013e3181e463a7. [DOI] [PubMed] [Google Scholar]
- 4.Neuhaus P, Jonas S, Settmacher U, Thelen A, Benckert C, Lopez-Hänninen E, et al. Surgical management of proximal bile duct cancer: extended right lobe resection increases resectability and radicality. Langenbecks Arch Surg. 2003;388:194–200. doi: 10.1007/s00423-003-0383-5. [DOI] [PubMed] [Google Scholar]
- 5.Miyazaki M, Kato A, Ito H, Kimura F, Shimizu H, Ohtsuka M, et al. Combined vascular resection in operative resection for hilar cholangiocarcinoma: does it work or not? Surgery. 2007;141:581–588. doi: 10.1016/j.surg.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 6.Majno PE, Pretre R, Mentha G, Morel P. Operative injury to the hepatic artery. Consequences of a biliary-enteric anastomosis and principles for rational management. Arch Surg. 1996;131:211–215. doi: 10.1001/archsurg.1996.01430140101025. [DOI] [PubMed] [Google Scholar]
- 7.Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Yoshidome H, et al. Unilateral hepatic artery reconstruction is unnecessary in biliary tract carcinomas involving lobar hepatic artery: implications of interlobar hepatic artery and its preservation. Hepatogastroenterology. 2000;47:1526–1530. [PubMed] [Google Scholar]
- 8.Wang WL, Tang XF, Yao MY, Liang TB, Jin J, Jiang ZJ, et al. Safety and efficiency of left hemihepatectomy combined with hepatic artery resection for hilar cholangiocarcinoma with artery infiltration: report of 2 cases. Can J Surg. 2008;51:305–307. [PMC free article] [PubMed] [Google Scholar]
- 9.Young AL, Prasad KR, Adair R, Abu Hilal M, Guthrie JA, Lodge JP. Portal vein arterialization as a salvage procedure during left hepatic trisectionectomy for hilar cholangiocarcinoma. J Am Coll Surg. 2008;207:e1–e6. doi: 10.1016/j.jamcollsurg.2008.07.019. [DOI] [PubMed] [Google Scholar]
- 10.Miura T, Hakamada K, Ohata T, Narumi S, Toyoki Y, Nara M, et al. Resection of a locally advanced hilar tumor and the hepatic artery after stepwise hepatic arterial embolization: a case report. World J Gastroenterol. 2008;14:3587–3590. doi: 10.3748/wjg.14.3587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee SG, Song GW, Hwang S, Ha TY, Moon DB, Jung DH, et al. Surgical treatment of hilar cholangiocarcinoma in the new era: the Asian experience. J Hepatobiliary Pancreat Sci. 2010;17:476–489. doi: 10.1007/s00534-009-0204-5. [DOI] [PubMed] [Google Scholar]
- 12.Sakamoto Y, Sano T, Shimada K, Kosuge T, Kimata Y, Sakuraba M, et al. Clinical significance of reconstruction of the right hepatic artery for biliary malignancy. Langenbecks Arch Surg. 2006;391:203–208. doi: 10.1007/s00423-006-0026-8. [DOI] [PubMed] [Google Scholar]


