Abstract
Objective
To quantify the role of diuretic use on gout development in an adult population with hypertension.
Methods
ARIC, a prospective population-based cohort from 4 US communities, consists of 4 visits over a 9-year period. Participants were included in this analysis if they answered the gout query, were free of gout at baseline, and had hypertension (medication to treat hypertension or a blood pressure ≥ 140/90 mmHg). Trained interviewers recorded antihypertensive use. Incident gout was defined as self-reported onset after baseline. Using a time-dependent Cox Proportional Hazards model, we estimated the hazard rate ratio (HR) of incident gout by time-varying diuretic use, adjusted for confounders, and tested for mediation by serum urate level.
Results
There were 5,789 hypertensive participants; 37% were treated with a diuretic. Use of any diuretic (HR=1.48, 95% CI: 1.11, 1.98), thiazide diuretic (HR=1.44, 95% CI: 1.00, 2.10), and loop diuretic (HR=2.31, 95% CI: 1.36, 3.91) was associated with incident gout compared with not using any diuretic, thiazide diuretic or loop diuretics, respectively. After adjusting for serum urate, the association between diuretic use and gout was null. Use of antihypertensive medication other than diuretic agents was associated with decreased gout risk (adjusted HR=0.64 95% CI: 0.49, 0.86) compared to untreated hypertension. The longitudinal change in serum urate was 0.72 mg/dL (95% CI: 0.57, 0.87) higher in those who initiated a diuretic compared with those who did not (p-value<0.001).
Conclusions
Thiazide and loop diuretics were associated with increased gout risk, an association mediated by a change in serum urate.
Keywords: gout, hypertension, diuretics, uric acid
Diuretic agents reduce morbidity and mortality related to stroke and congestive heart failure in hypertensive patients (1). This class of antihypertensive medication is recommended as initial therapy for hypertension (1, 2). Notwithstanding their favorable control of blood pressure, these medications may increase the risk of gout. Diuretics, particularly thiazide diuretics, are associated with an increase in serum urate levels (3–6). Moreover, hyperuricemia is the leading risk factor for gout (7). The association of thiazide diuretic use and gout was first noted in case series from the medical literature (8, 9). In trials and observational studies, diuretic use was associated with an increased risk of gout (3, 7, 10, 11). However, 1 observational case-control study found that diuretic use was not associated with gout after adjusting for comorbid conditions (12). Thus, it remains uncertain whether diuretic use is independently associated with the development of gout.
While hypertension is the main indication for diuretic use, it is also an independent risk factor for gout (10). Previous observational studies have not been able to differentiate whether diuretic use or the underlying hypertension causes gout, leading to confounding by indication, a common bias in observational studies of prescription drugs (13). Additionally, the observational studies neither reported the type of diuretic used by study participants, adjusted for time-varying blood pressure nor tested whether serum urate was on the intermediate pathway between diuretic use and gout (10, 11). Studies of hypertensive patients that can control for changes in blood pressure due to antihypertensive treatment may be better suited to quantify the association of diuretic use with gout. Additionally, previous clinical trials have not been designed to study gout as an outcome but rather focused on the change in serum urate levels (3–5, 14). Furthermore, the studies of diuretics have focused on thiazide diuretics, and few studies have assessed the association of loop diuretics with serum urate and the risk of gout (15, 16). To our knowledge, no population-based study has jointly evaluated the association of diuretic use with serum urate level and risk of incident gout.
We quantified the hazard of incident gout by diuretic use, and class of diuretic agent, over 9-years of follow-up in a longitudinal population-based cohort of middle-aged adults. To limit confounding by indication, the study was restricted to participants with hypertension and included multiple measures of diuretic use. Additionally, we tested whether serum urate acts as an intermediate on the pathway between diuretic use and incident gout.
Materials and Methods
Setting and Participants
The Atherosclerosis Risk in the Communities study (ARIC) is a prospective population-based cohort study of 15,792 individuals recruited from 4 US communities (Washington County, Maryland; Forsyth County, North Carolina; Jackson, Mississippi; and suburbs of Minneapolis, Minnesota). The Institutional Review Board of the participating institutions approved the ARIC study protocol and study participants provided written informed consent. Participants aged 45 to 64 were recruited to the cohort in 1987–1989. This cohort was established to study the natural history of atherosclerosis, and consisted of 1 baseline visit (visit 1) between 1987 and 1989 and 3 follow-up visits (visits 2, 3, and 4) administered 3 years apart.
This analysis was limited to participants who were Caucasian or African American; few participants reported other races (n=48). We excluded participants who did not report their gout status at visit 4 (n=2,356) and those with prevalent gout at cohort entry, defined as the self-report of gout onset prior to the baseline visit (n=310).
We limited our study sample to those with hypertension at 1 or more visits. At each visit, technicians used a random-zero sphygmomanometer to take 3 blood pressure measures. An average of the second and third measurements was recorded for the first 3 visits and the first and second measurement at the fourth visit. Hypertension was defined as the self-report of medication to treat hypertension, or a measured systolic blood pressure greater than or equal to 140 mm Hg or diastolic blood pressure greater than or equal to 90 mm Hg. Previous work has suggested that restriction is a better method than propensity score to control for confounding by indication when a drug is the best marker of the disease (17); antihypertensive medications are clear markers of hypertension. As such, we excluded those who were free of hypertension during follow-up (n=7,289). Therefore, there were 5,789 hypertensive participants included in our study.
Exposure: Diuretic Use
Trained interviewers collected information on the medications that participants used in the 2 weeks prior to the visit. Participants reported whether they used a medication to treat hypertension. We considered this exposure to be time-varying and defined diuretic use as the report of a diuretic at visit 1, 2, or 3. Diuretic use had to occur prior to the onset of gout to be considered in this analysis. We did not include diuretic use at visit 4 in our analysis because we wanted to ensure that use of this medication occurred prior to gout onset (reported at visit 4). Participants that were missing data on diuretic use at visit 2 or 3 had their previous reported diuretic carried forward. Additionally, we considered thiazide and loop diuretics as separate classes of diuretics. In the class-specific analyses we considered thiazide and loop diuretics as monotherapy, and we did not include participants with use of more than 1 diuretic class, to isolate the effects. However, there were very few participants at each visit who were on more than 1 diuretic, (less than 0.5% of participants at each visit).
Outcome: Incident Gout
At visit 4, participants were asked, “Has a doctor ever told you that you had gout?” Participants who answered, “Yes,” to the gout query then reported the age of gout diagnosis. The outcome of interest was incident gout based on self-report. Incident gout was defined as the onset of gout after baseline. Our previous research suggests that self-report of a physician diagnosis of gout is a reliable (3-year reliability kappa=0.73) and a sensitive (sensitivity=84%) measure of gout (18).
Other Measures
Other covariates of interest that were assessed at baseline (1989) included age (in years), sex (male or female), race (White or African American), alcohol intake (grams/week), diabetes (present or absent), body mass index (BMI in kg/m2). Additionally, blood pressure was measured at each visit and thus was considered to be time-varying. Serum creatinine was estimated using a modified kinetic Jaffé reaction. Glomerular filtration rate (eGFR) was estimated by using the 4-variable Modification of Diet in Renal Disease (MDRD) study equation adjusted to the ARIC study (19) and categorized as <60 mg/dL, 60–90 mg/dL, and >90 mg/dL. Additionally, the self-report of a history of congestive heart failure (CHF present or absent) at visit 4 was also considered as a covariate of interest. These variables were considered to be potential confounders and the categories were chosen to reduce residual confounding.
Serum urate concentrations were measured with the uricase method at visit 1 and 2 in mg/dL. The reliability coefficient of serum urate was 0.91, and the coefficient of variation was 7.2% in a sample of 40 individuals with repeated measures taken at least 1 week apart (20). In the complete ARIC cohort, the mean serum urate levels were 0.36 mg/dL higher at visit 2 due to lab drift compared with visit 1 after adjustment for age at the visit. Therefore, we subtracted 0.36 mg/dL from the visit 2 serum urate levels to make them comparable to visit 1 values to correct for lab drift.
Statistical Methods
First, the mean and standard deviation (SD) as well as the prevalence of the covariates were calculated and compared by diuretic use at either visit 1, 2, or 3. The mean of continuous variables in those exposed to a diuretic was compared with the mean of those who were not exposed to a diuretic using a t-test; the prevalence of categorical factors was compared using chi-squared tests.
Using a time-dependent Cox Proportional Hazards model, the hazard rate ratio (HR) and 95% confidence intervals (CI) of incident gout by time-varying diuretic use was estimated with age as the time scale. The comparator group was those not using any diuretic. Diuretic use and measured blood pressure were treated as time-varying and updated at each of the ARIC study visits. Results did not change when BMI was considered as time-varying. Therefore, the BMI and the other variables were considered time-fixed at baseline. The HR of incident gout by thiazide and the HR of incident gout by loop diuretics were estimated separately. For the thiazide and loop diuretic analyses, the comparator groups were those who were not taking a thiazide or loop diuretic agent, respectively. These comparator groups include those treated with other antihypertensive medications or untreated hypertension. This comparator group was selected because there is thought to be an increased risk with all classes of diuretics and there was little power for head to head comparisons between diuretics and other antihypertensive medications (exposed sample, n=557). However, to allow for direct comparison of the risk of gout by any, thiazide and loop diuretics, we estimated the HR of incident gout using those that were not taking any antihypertensive medication to treat their hypertension (participants with untreated hypertension) as the comparator group. Models were adjusted for confounders of the association of diuretic use and incident gout including sex, race, baseline BMI, categorical eGFR, and time-varying blood pressure. The unadjusted cumulative incidence function was plotted using a Kaplan-Meier approach. Alcohol and diabetes were not included in the adjusted model because they were not strong confounders in this study. The model with loop diuretics as the exposure was also adjusted for history of congestive heart failure. The Cox Proportional Hazards Models did not violate the proportional hazards assumptions; although only the analysis with loop diuretics as the exposure of interest did not satisfy the assumption early in the follow-up period.
Additionally, the association of antihypertensive medications other than diuretics with incident gout was examined; the comparator group was those that were not taking any antihypertensive medication to treat their hypertension (participants with untreated hypertension). Primarily, the other antihypertensive medications were from the Angiotensin Converting Enzyme (ACE) inhibitor class and included captopril, lisinopril and enalapril, as well as the Beta Blocker class, including atenolol, nadolol, propranolol, metoprolol.
We assessed whether serum urate levels mediated the association of diuretic use and incident gout. We added visit 2 serum urate level to the adjusted Cox Proportional Hazards model to test for mediation. Additionally, using a t-test and linear regression, we tested if the change in serum urate between visit 1 and 2 differed by the initiation of a diuretic between visit 1 and 2; the comparison group was those who did not report diuretic use at either visit 1 or 2. Finally, we assessed the percentage of participants with incident gout who were taking a diuretic at the visit prior to gout onset, at the visit after gout onset and at both visits.
All analyses were performed in SAS, version 9.1 (SAS Institute, Cary, North Carolina).
Results
Study Population Characteristics
A total of 5,789 ARIC participants were hypertensive and met the study criteria. The study population was 42% male and 31% African American. The mean age at cohort entry was 55 years (SD=5.7) and the mean BMI was 29 kg/m2 (SD=5.5).
There were 2,169 (37%) participants exposed to a diuretic during follow-up; 1,212 participants who were exposed to a thiazide diuretic and 339 to loop diuretic and only 89 who switched between loop and thiazide diuretics during follow-up. The most common diuretic listed by participants was hydrochlorothiazide. The frequency of diuretic use (27%, 25%, 26%) remained the same over the 3 follow-up visits, respectively. However, there was an increase in the percentage of participants that used an antihypertensive medication (42%, 47%, and 56%) over follow-up. Reflecting the dynamic nature of antihypertension treatment, there were 2,252 participants who were exposed to a non-diuretic antihypertensive medication during follow-up with many participants using more than 1 class of antihypertensive medication over follow-up. For example, 1,062 used an ACE inhibitor and 1,430 were exposed to a beta-blocker; 331 were exposed to both these classes over follow-up.
Table 1 lists the characteristics of ARIC cohort participants by diuretic use during follow-up. Baseline study population characteristics were similar for those participants with any diuretic use (Table 1), as well as for thiazide and loop diuretic use compared to no diuretic use (data not shown). The 9-year cumulative incidence of gout was 3.9%; 2.8% in women and 5.3% in men.
Table 1.
Baseline gout risk factors by diuretic use at baseline or follow-up in ARIC participants with hypertension (n=5,789)
| Baseline risk factors | No diuretic use (n=3,620) | Diuretic use (n=2,169) |
|---|---|---|
| Male sex, n (%) | 1,727 (48) | 718 (33)† |
| Mean age, years (SD) | 54.5 (5.7) | 55.0 (5.7)* |
| African American race, n (%) | 955 (26) | 836 (39)† |
| Mean blood pressure, mm Hg (SD) | ||
| Systolic | 128 (16.1) | 129 (18.2) |
| Diastolic | 77 (10.4) | 78 (10.9)† |
| Mean BMI, kg/m2 (SD) | 27.8 (4.9) | 30.1 (6.1)† |
| Estimated glomerular filtration rate, mL/min, n (%) | ||
| <60 | 70 (2.0) | 95 (4.4)† |
| 60–90 | 1,770 (49.3) | 1,042 (48.5) |
| >90 Mean serum urate, mg/dL, (SD) | 1,745 (48.7) | 1,010 (47.0) |
| Mean alcohol intake, grams/week, (SD) | 44.6 (95) | 32.0 (84)† |
| Mean serum urate, mg/dL, (SD) | 6.0 (1.4) | 6.6 (1.6)† |
| 9-year cumulative incident gout, n (%) | 105 (2.9) | 120 (5.5)† |
p-value <0.05 comparing diuretic use with no diuretic use.
p-value <0.001 comparing diuretic use with no diuretic use
ARIC=Atherosclerosis Risk in Communities Study; BMI=Body Mass Index
Association of Diuretic Use and Gout
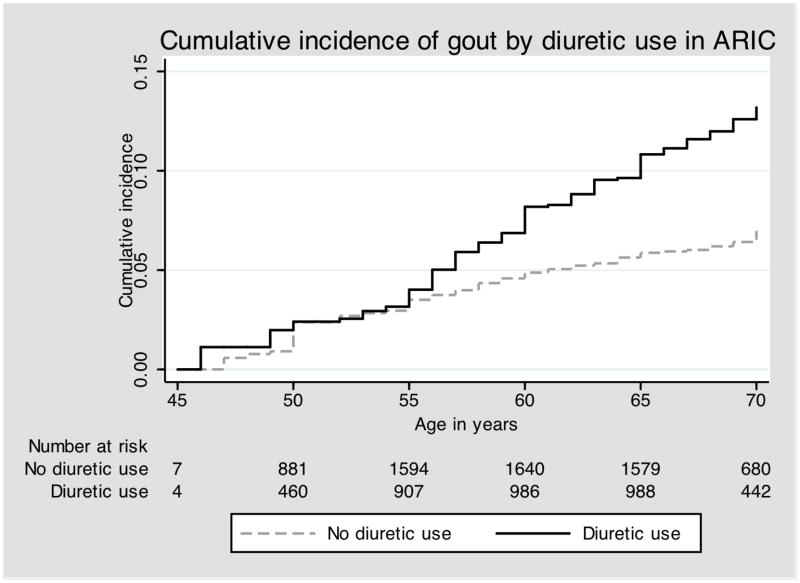
The data in Table 1 suggests that the cumulative incidence of gout occurred more frequently in participants with diuretic use during follow-up compared with those without diuretic use (5.5% vs. 2.9%, log rank p-value <0.001). Figure 1 presents the Kaplan-Meier cumulative incidence function of gout by any diuretic use, suggesting a higher rate of gout among those who are exposed to a diuretic (log rank p-value <0.0001). Table 2 lists the unadjusted and adjusted HR of incident gout by diuretic use. The unadjusted HR of incident gout was 1.72 (95% CI: 1.32, 2.25) comparing diuretic use to no diuretic use. Use of any diuretic was associated with a 1.48-fold (95% CI: 1.11, 1.98) increase in the hazard of incident gout after adjusting for time-varying blood pressure and confounders of the diuretic and gout association. After further adjustment for serum urate level, use of a diuretic compared to no diuretic use was no longer associated with incident gout (HR=0.96, 95% CI: 0.71, 1.28), suggesting that serum urate may be a key intermediate on the pathway between diuretic use and incident gout.
Figure 1.
Cumulative incidence of gout according to any diuretic use in the Atherosclerosis Risk in Communities Study. The log-rank p-value was <0.001 for any diuretic use.
Table 2.
Hazard rate ratio of incident gout by time-varying diuretic use in the ARIC participants with hypertension (N=5,789)
| Any diuretic use (n=2,169)‡ | Thiazide use (n=1,212) | Loop diuretic use (n=339) | Nondiuretic antihypertensive use (n=2,252)§ | |
|---|---|---|---|---|
| Model | HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) |
| Unadjusted | 1.72 (1.32, 2.25)† | 1.54 (1.08, 2.21)* | 3.65 (2.26, 5.90)† | 0.44 (0.30, 0.64)† |
| Sex- and race-adjusted | 1.72 (1.31, 2.26)† | 1.50 (1.05, 2.16)* | 3.99 (2.45, 6.51)† | 0.46 (0.31, 0.68)* |
| Adjusted for confounders|| | 1.48 (1.11, 1.98)* | 1.44 (1.00, 2.10) | 2.31 (1.36, 3.91)* | 0.64 (0.49, 0.86)* |
| Mediation by serum urate# | 0.96 (0.71, 1.28) | 0.94 (0.64, 1.38) | 1.35 (0.78, 2.34) | 0.64 (0.48, 0.84)* |
p-value <0.05 compared with no diuretic use.
p-value <0.001 compared with no diuretic use.
The analyses of thiazide and loop diuretics are subsets of the analysis for any diuretic use. Therefore, the number of participants using a loop or thiazide diuretic does not sum to the total number of participants using any diuretic. The comparator groups are no diuretic use, no thiazide diuretic use and no loop diuretic use, respectively.
The comparator group includes those who are not treated for hypertension.
Confounders: Sex, race, BMI, categorical eGFR and time-varying blood pressure. Age was the time-scale. The analysis of loop diuretics included congestive heart failure as a confounder.
To test for mediation by serum urate level, we added the serum urate level at visit 2 to the model that was adjusted for confounders.
ARIC=Atherosclerosis Risk in Communities Study; HR=Hazard Rate Ratio; CI=Confidence Interval
Furthermore, when diuretic use was compared to untreated hypertension, any diuretic use was associated with a 3-fold increase in the risk of gout (adjusted HR=3.35, 95% CI: 2.49, 4.51).
Association of Thiazide and Loop Diuretic Use and Gout
Among the participants who took a thiazide diuretic, there were 63 incident gout cases, corresponding to a cumulative incidence of 5%. Among those taking a loop diuretic there were 23 gout cases and a cumulative incidence of 7%. Table 2 presents the hazard rate ratio of gout by thiazide and loop diuretic use. After adjustment for confounders, thiazide diuretic use was associated with an approximately 1.44-fold increase in risk (95% CI: 1.00, 2.10) compared to those who were not using a loop diuretic. Loop diuretics were associated with a 2.31-fold increase in risk of incident gout (95% CI: 1.36, 3.91) when compared to those who were not taking a loop diuretic. When serum urate was added to the adjusted model, neither thiazide diuretic use nor loop diuretic use remained associated with incident gout (thiazide HR=0.94, 95% CI: 0.64, 1.38; loop diuretic HR=1.35, 95% CI: 0.78, 2.34) compared to those who were not using a thiazide or not using a loop diuretic, respectively.
Additionally, thiazide and loop diuretic use were each associated with an increased risk of gout when compared to untreated hypertension (thiazide HR=2.53, 95% CI: 1.75, 3.67; loop diuretic HR=2.09, 95% CI: 1.19, 2.83).
Association of Antihypertensive Medications Use (Other Than Diuretics) and Gout
Among these participants, there were 89 incident gout cases in those exposed to a nondiuretic antihypertensive agent, corresponding to a cumulative gout incidence of 4%. Table 2 lists the unadjusted and adjusted hazard of incident gout by nondiuretic antihypertensive use. After adjustment for confounders, nondiuretic antihypertensive use was inversely associated with incident gout (HR= 0.64, 95% CI: 0.48, 0.84) compared to untreated hypertension and remained associated even after adjusting for serum urate level.
Initiation of Diuretics and Change in Serum Urate Level
There were 330 new initiators of any diuretic and 3,827 noninitiators between visits 1 and 2. The mean serum urate levels at these visits are listed in Table 3. The change in serum urate was 0.72 mg/dL (95% CI: 0.57, 0.87) higher in those who initiated a diuretic compared with those who did not (p-value<0.001). Similarly, the increase in serum urate was greater in those who initiated thiazide (0.65 mg/dL, 95% CI: 0.45, 0.85) and loop diuretics (0.96 mg/dL, 95% CI: 0.44, 1.48) compared with those who did not (p-value<0.001 for both thiazide and loop diuretics). However, the initiation of a nondiuretic antihypertension medication was associated with a decrease in serum urate levels (−0.21 mg/dL, 95% CI: −0.32, −0.11) compared with untreated hypertension at visit 2. Additionally, the mean change in serum urate level between visit 1 and visit 2 was similar, although slightly attenuated, after adjusting for age, sex, race, eGFR, previous non-diuretic antihypertensive use and BMI.
Table 3.
Change in serum urate level associated with new diuretic use in the ARIC participants with hypertension (N=4,257)
| No diuretic use (n=3,827)† | New diuretic use (n=330) | New thiazide use (n=171) | New loop use (n=43) | |
|---|---|---|---|---|
| Serum urate | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) |
| Visit 1 | 5.95 (1.40) | 6.23 (1.51) | 6.34 (1.64) | 6.41 (1.41) |
| Visit 2 | 6.09 (1.49) | 7.08 (1.66) | 7.10 (1.74) | 7.87 (1.79) |
| Change‡ | 0.13 (0.98) | 0.85 (1.35)* | 0.78 (1.29)* | 1.09 (1.68)* |
| Difference in change (95% CI)§ | reference | 0.72 (0.57, 0.87)* | 0.65 (0.45, 0.85)* | 0.96 (0.44, 1.48)* |
| Adjusted difference in change (95% CI)§ | reference | 0.59 (0.43, 0.74)* | 0.55 (0.35, 0.75)* | 0.73 (0.32, 1.14)* |
p-value <0.001 (for Change and Difference in change)
See footnote 1 from Table 2.
Change = Visit 2 serum urate level minus visit 1 serum urate level. P-value tests the hypothesis that the change in serum urate from visit 1 to visit 2 is different from 0.
Difference = Change in serum urate level for diuretic use minus change in serum urate level for no diuretic use. P-value tests the hypothesis that the unadjusted difference change in serum urate is different for those taking a diuretic compared with those not taking a diuretic. Adjusted change accounted for age, sex, race, eGFR, previous non-diuretic antihypertensive use and BMI.
ARIC=Atherosclerosis Risk in Communities Study; SD=Standard Deviation; CI=Confidence Interval
Diuretic Use Before and After the Onset of Gout
Overall, 86 (38%) participants used a diuretic at the visit prior to the onset of gout. At the visit after gout diagnosis, 105 (47%) participants were taking a diuretic. Additionally, 74 of the 86 (86%) participants who were taking a diuretic prior to the onset of gout were still on a diuretic at the visit after their gout onset. Finally, only 3 (3%) of the participants with gout switched from a diuretic at the visit prior to gout onset to another antihypertensive medication at the visit after gout onset.
Sensitivity Analyses
The study results did not differ, 1) after adjustment for alcohol intake (grams/week) and diabetes, 2) after adjustment for history of thiazide use among those using a loop diuretic, and 3) when visit 1 serum urate levels were substituted for visit 2 serum urate levels. The results did not differ by sex or race in stratified analyses, inasmuch as the sex and race interactions were not statistically significant.
Discussion
In a large prospective population-based study of middle-aged adults with hypertension, we found that both thiazide and loop diuretics were independently associated with an increased risk of incident gout. The results suggest that the initiation of a diuretic raises serum urate levels. Other antihypertensive medications were associated with a decreased risk of gout, which may reflect the protective effect of reducing blood pressure in hypertensive patients and the resulting decrease in serum urate level achieved after initiation of these medications. Additionally, findings from this large biracial cohort suggest that elevation of serum urate may mediate the association of diuretic use with incident gout in hypertensive patients. Finally, few participants with gout discontinued the use of a diuretic after the onset of gout.
Epidemiologic studies have suggested that a history of diuretic use is associated with gout (7, 10, 11). For example in a community-based cohort of white adults, the history of any diuretic use was associated with a 2.4-fold increased risk of gout in women and 3.4-fold increased risk in men after adjustment for hypertension and other gout risk factors (11). The results may be biased away from the null due to confounding by indication, because this cohort is relatively healthy and diuretic use may be a marker of worse health. In contrast, a pharmacoepidemology case-control study using records from a single Dutch primary care center reported that the association between being prescribed a diuretic and a diagnosis of gout was null after adjusting for history of hypertension and other confounders (12). Our results may differ from this previous study because of the control selection utilized in this Dutch case-control study: matching on comorbid conditions rather than adjusting for these conditions will allow for a more accurate comparison in which both the case and the control are likely to be exposed to a diuretic. By restricting our study to participants with hypertension and adjusting for time-varying blood pressure, we were better able to control for confounding by indication. However, our results were similar to a community-based cohort reporting that diuretic use was associated with the development of gout in men (HR=1.77, 95% CI: 1.42, 2.20) (10).
In clinical trials, gout was associated with the use of a thiazide diuretic compared with standard care or placebo (3, 4). However, these studies were not designed to assess gout as an outcome. A pharmacoepidemiology study using New Jersey Medicaid prescription data, found a 1.99 relative risk (95% CI: 1.21, 3.26) of initiating an antigout medication for patients taking thiazide agents, but no increased risk for nonthiazide antihypertensive agents (21). This study is missing the more clinically relevant outcome of incident gout, and was limited to treated cases of gout defined by a prescription claim for allopurinol, colchicine, or an uricosuric agent. Thiazide and loop diuretics were also associated with recurrent attacks in patients with gout (22). In a case-control study, gout was more strongly related to the use of loop diuretics (15).
The increase of serum urate due to diuretics has been noted in case studies, clinical trials, and epidemiology studies and is most often attributed to thiazide diuretics (3–6, 23). For example, the Systolic Hypertension in the Elderly Program randomized trial of community-living adults with hypertension aged 60 years or older found that the 3-year increase in serum urate level was 0.90 mg/dL in those randomized to the thiazide arm compared with the placebo arm, a rise in serum urate levels similar to our own findings (5). Data on loop diuretics and serum urate are, however, more limited. Pooled analysis of 2 small studies found no change in serum urate after the initiation of a loop diuretic (16). A UK study of the 25 participants using a diuretic before the onset of gout, found that 16 (64%) continued the diuretic (24). These results were consistent with our findings in hypertensive middle-aged adults with the slight differences perhaps attributable to different practices in the management of gout in the UK.
Hyperuricemia occurs when there is an over-production or under-excretion of uric acid. Hypertension decreases renal blood flow, which may augment urate reabsorption and thus lead to urate under-excretion (25). Diuretics cause water loss and this leads to volume depletion. In particular, loop diuretics are often prescribed for volume control. Additionally, diuretics are thought to affect ion exchanger proteins at the proximal tubule lumen membrane in the kidney. This would increase both sodium and urate reabsorption and thus increase serum urate levels (25). These mechanisms may be associated with an increase in serum urate and the development of gout beyond the effects of hypertension. However, blood pressure control may increase serum urate excretion and decrease the risk of gout.
To our knowledge, this is the first study to jointly quantify the association of diuretic use on both serum urate levels and incident gout in hypertensive participants in a prospective, population-based cohort. Additionally, ARIC is a well-characterized cohort with very high response rates. This is one of the largest biracial studies of gout, which included both men and women with gout. Restricting our study population to those with hypertension allowed us to better control for confounding by indication than previous studies. Additionally, we used a broad definition of hypertension that included both measured blood pressure and antihypertension medications. We were able to control for the treatment effects of antihypertensive medications by adjusting for measured blood pressure at each ARIC study visit. Additionally, we controlled for eGFR, which has previously been thought to explain the association of diuretic use and gout (26). Two measures of serum urate allowed for analysis of new initiators of diuretics and to quantify the change in serum urate levels associated with diuretic initiation. Finally, we were able to show that the elevated risk of gout in hypertensive participants was specific to the diuretic class of antihypertensive agents and not associated with the use of other antihypertensive medications.
The main limitation of our study was that gout was self-reported by participants at visit 4. However, previous work has suggested that self-reported gout and age of onset is both sensitive and reliable (18). Participants had to survive until visit 4 and be healthy enough to attend the follow-up assessment to be included in this study. This may induce selection bias if those who attended visit 4 were different from the baseline study population with respect to their health status profile (i.e. hypertension, renal function and obesity status). However, such a bias, with non-participation at follow-up of the more comorbid participants, those at greater risk to develop gout, would lead to an attenuation of the true association. Additionally, the study collected information on diuretic use in the 2 weeks prior to the visit and not detailed information on diuretic use each month after baseline. However, antihypertension medications are often taken for years and there is moderate persistence with this class of drugs (27). Additionally, the cohort did not collect data on whether participants were treated for hypertension through lifestyle interventions. We cannot be assured that we have fully controlled for confounding by indication, although we have adjusted for the main confounders and restricted the population to those with hypertension. In particular, there may be confounding by indication due to CHF for the association of loop diuretics and gout. However, there was insufficient data – only 22 cases of gout among those with CHF, of whom only 4 were exposed to a diuretic – to examine the association of diuretic use with incident gout among those participants with CHF. We could not rule out the possibility that serum urate is a confounder and not a mediator of this association. However, it is unlikely that physicians would be selectively prescribing a diuretic to those with elevated serum urate, as this would be the source of the confounding. Although serum urate has been found to predict the onset of hypertension, (25) a randomized controlled trial would be necessary to determine the directionality of the uric acid and hypertension association. Our analysis was not designed to test whether the urate level was a consequence of changing blood pressure levels. However, in new initiators with hypertension, those who initiated a diuretic experienced, on average, a greater escalation in serum urate levels than those who did not initiate a diuretic. We were not able to test whether dose or a specific brand of thiazide or loop diuretic was associated with higher gout risk. We did not assess the association of other classes of antihypertensives because diuretics were the most commonly used class of antihypertensive. Additionally, the first angiotensin receptor blockers (ARBs), some of which have uricosuric properties, were approved in 1995. As such, we were unable to assess the association of ARBs, such as losartan, with incident gout because we only considered diuretic exposure prior to the last ARIC study visit, which occurred prior to the introduction of these agents (28). Finally, we are unable to rule out the possibility that the inverse association of other antihypertensive medications is due to the fact that use of an antihypertension medication is also associated with other healthy behaviors beyond what we can adjust for in this analysis. This healthy-user bias often occurs in observational studies of the protective effects of prescription medications (29).
The results from this population-based, longitudinal study support the hypothesis that diuretic use increases serum urate levels and is related to an increase in incidence of gout. Future studies should not only confirm the risk of gout associated with diuretic-induced hyperuricemia but also further elucidate the complicated relationship of hypertension, diuretics, uric acid, and gout. Although diuretic use has proven to be a safe and effective first-line treatment for hypertension, our results contribute to the evidence that diuretic use is associated with an increased risk of gout independent of hypertension and other chronic conditions.
Acknowledgments
The authors thank the staff and participants of the ARIC study for their important contributions.
Source of Funding: The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201100005C, HHSN268201100006C, HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C, and HHSN268201100012C). Mara McAdams DeMarco was supported by a T32 training grant from the National Heart, Lung, and Blood Institute grant (5T32HL007024). Janet Maynard, Allan Gelber and Alan Baer were supported by the Donald B. and Dorothy Stabler Foundation. Allan Gelber was also supported by the Ira T. Fine Discovery Fund.
Footnotes
Conflict of Interest: No authors have a conflict of interest to declare.
This work was presented as a poster presentation at American College of Rheumatology Annual Scientific Meeting in Atlanta, Georgia (November 9, 2010).
References
- 1.Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002;288(23):2981–97. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]
- 2.Ong HT. The JNC 7 hypertension guidelines. JAMA. 2003;290(10):1312. doi: 10.1001/jama.290.10.1312-a. author reply 1314–5. [DOI] [PubMed] [Google Scholar]
- 3.Staessen J. The determinants and prognostic significance of serum uric acid in elderly patients of the European Working Party on High Blood Pressure in the Elderly trial. Am J Med. 1991;90(3A):50S–54S. [PubMed] [Google Scholar]
- 4.Langford HG, Blaufox MD, Borhani NO, Curb JD, Molteni A, Schneider KA, et al. Is thiazide-produced uric acid elevation harmful? Analysis of data from the Hypertension Detection and Follow-up Program. Arch Intern Med. 1987;147(4):645–9. doi: 10.1001/archinte.147.4.645. [DOI] [PubMed] [Google Scholar]
- 5.Savage PJ, Pressel SL, Curb JD, Schron EB, Applegate WB, Black HR, et al. Influence of long-term, low-dose, diuretic-based, antihypertensive therapy on glucose, lipid, uric acid, and potassium levels in older men and women with isolated systolic hypertension: The Systolic Hypertension in the Elderly Program. SHEP Cooperative Research Group. Arch Intern Med. 1998;158(7):741–51. doi: 10.1001/archinte.158.7.741. [DOI] [PubMed] [Google Scholar]
- 6.Berglund G, Andersson O, Widgren B. Low-dose antihypertensive treatment with a thiazide diuretic is not diabetogenic. A 10-year controlled trial with bendroflumethiazide. Acta Med Scand. 1986;220(5):419–24. doi: 10.1111/j.0954-6820.1986.tb02790.x. [DOI] [PubMed] [Google Scholar]
- 7.Lin KC, Lin HY, Chou P. The interaction between uric acid level and other risk factors on the development of gout among asymptomatic hyperuricemic men in a prospective study. J Rheumatol. 2000;27(6):1501–5. [PubMed] [Google Scholar]
- 8.Macfarlane DG, Dieppe PA. Diuretic-induced gout in elderly women. Br J Rheumatol. 1985;24(2):155–7. doi: 10.1093/rheumatology/24.2.155. [DOI] [PubMed] [Google Scholar]
- 9.Scott JT, Higgens CS. Diuretic induced gout: a multifactorial condition. Ann Rheum Dis. 1992;51(2):259–61. doi: 10.1136/ard.51.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Choi HK, Atkinson K, Karlson EW, Curhan G. Obesity, weight change, hypertension, diuretic use, and risk of gout in men: the health professionals follow-up study. Arch Intern Med. 2005;165(7):742–8. doi: 10.1001/archinte.165.7.742. [DOI] [PubMed] [Google Scholar]
- 11.Bhole V, de Vera M, Rahman MM, Krishnan E, Choi H. Epidemiology of gout in women: Fifty-two-year followup of a prospective cohort. Arthritis Rheum. 62(4):1069–76. doi: 10.1002/art.27338. [DOI] [PubMed] [Google Scholar]
- 12.Janssens HJ, van de Lisdonk EH, Janssen M, van den Hoogen HJ, Verbeek AL. Gout, not induced by diuretics? A case-control study from primary care. Ann Rheum Dis. 2006;65(8):1080–3. doi: 10.1136/ard.2005.040360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salas M, Hofman A, Stricker BH. Confounding by indication: an example of variation in the use of epidemiologic terminology. Am J Epidemiol. 1999;149(11):981–3. doi: 10.1093/oxfordjournals.aje.a009758. [DOI] [PubMed] [Google Scholar]
- 14.Fletcher AE. Adverse treatment effects in the trial of the European Working Party on High Blood Pressure in the Elderly. Am J Med. 1991;90(3A):42S–44S. doi: 10.1016/0002-9343(91)90435-z. [DOI] [PubMed] [Google Scholar]
- 15.Waller PC, Ramsay LE. Predicting acute gout in diuretic-treated hypertensive patients. J Hum Hypertens. 1989;3(6):457–61. [PubMed] [Google Scholar]
- 16.Musini VM, Wright JM, Bassett K, Jauca CD. Blood pressure lowering efficacy of loop diuretics for primary hypertension. Cochrane Database Syst Rev. 2009;(4):CD003825. doi: 10.1002/14651858.CD003825.pub2. [DOI] [PubMed] [Google Scholar]
- 17.Psaty BM, Siscovick DS. Minimizing bias due to confounding by indication in comparative effectiveness research: the importance of restriction. JAMA. 2010;304(8):897–8. doi: 10.1001/jama.2010.1205. [DOI] [PubMed] [Google Scholar]
- 18.McAdams MA, Maynard JW, Baer AN, Kottgen A, Clipp S, Coresh J, et al. Reliability and sensitivity of the self-report of physician-diagnosed gout in the campaign against cancer and heart disease and the atherosclerosis risk in the community cohorts. J Rheumatol. 2011;38(1):135–41. doi: 10.3899/jrheum.100418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Astor BC, Arnett DK, Brown A, Coresh J. Association of kidney function and hemoglobin with left ventricular morphology among African Americans: the Atherosclerosis Risk in Communities (ARIC) study. Am J Kidney Dis. 2004;43(5):836–45. doi: 10.1053/j.ajkd.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 20.Eckfeldt JH, Chambless LE, Shen YL. Short-term, within-person variability in clinical chemistry test results. Experience from the Atherosclerosis Risk in Communities Study. Arch Pathol Lab Med. 1994;118(5):496–500. [PubMed] [Google Scholar]
- 21.Gurwitz JH, Kalish SC, Bohn RL, Glynn RJ, Monane M, Mogun H, et al. Thiazide diuretics and the initiation of anti-gout therapy. J Clin Epidemiol. 1997;50(8):953–9. doi: 10.1016/s0895-4356(97)00101-7. [DOI] [PubMed] [Google Scholar]
- 22.Hunter DJ, York M, Chaisson CE, Woods R, Niu J, Zhang Y. Recent diuretic use and the risk of recurrent gout attacks: the online case-crossover gout study. J Rheumatol. 2006;33(7):1341–5. [PubMed] [Google Scholar]
- 23.Franse LV, Pahor M, Di Bari M, Shorr RI, Wan JY, Somes GW, et al. Serum uric acid, diuretic treatment and risk of cardiovascular events in the Systolic Hypertension in the Elderly Program (SHEP) J Hypertens. 2000;18(8):1149–54. doi: 10.1097/00004872-200018080-00021. [DOI] [PubMed] [Google Scholar]
- 24.Roddy E, Zhang W, Doherty M. Concordance of the management of chronic gout in a UK primary-care population with the EULAR gout recommendations. Ann Rheum Dis. 2007;66(10):1311–5. doi: 10.1136/ard.2007.070755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson RJ, Kang DH, Feig D, Kivlighn S, Kanellis J, Watanabe S, et al. Is there a pathogenetic role for uric acid in hypertension and cardiovascular and renal disease? Hypertension. 2003;41(6):1183–90. doi: 10.1161/01.HYP.0000069700.62727.C5. [DOI] [PubMed] [Google Scholar]
- 26.Pascual E, Perdiguero M. Gout, diuretics and the kidney. Ann Rheum Dis. 2006;65(8):981–2. doi: 10.1136/ard.2005.049023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bramlage P, Hasford J. Blood pressure reduction, persistence and costs in the evaluation of antihypertensive drug treatment--a review. Cardiovasc Diabetol. 2009;8:18. doi: 10.1186/1475-2840-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McAdams MA, Governale LA, Swartz L, Hammad TA, Dal Pan GJ. Identifying patterns of adverse event reporting for four members of the angiotensin II receptor blockers class of drugs: revisiting the Weber effect. Pharmacoepidemiol Drug Saf. 2008;17(9):882–9. doi: 10.1002/pds.1633. [DOI] [PubMed] [Google Scholar]
- 29.Garbe E, Suissa S. Hormone replacement therapy and acute coronary outcomes: methodological issues between randomized and observational studies. Hum Reprod. 2004;19(1):8–13. doi: 10.1093/humrep/deh022. [DOI] [PubMed] [Google Scholar]