Abstract
Objectives
To examine the public health burden of major depressive disorder (MDD) among mothers: its prevalence and sociodemographic patterns; associated functioning, comorbidities, and adversities; and racial/ethnic disparities.
Methods
This was a cross-sectional analysis of 8916 mothers in the National Epidemiologic Survey of Alcohol and Related Conditions, a nationally representative survey of the civilian U.S. population in 2001–2002. Past-year MDD was assessed with a structured interview protocol.
Results
Ten percent of mothers experienced depression in the past year. White and Native American women, those with low education or income, and those not married had high rates of depression. Depression was not strongly patterned by number of or age of children. Depressed mothers experienced more adversities (poverty, separation or divorce, unemployment, financial difficulties) and had worse functioning. Half of depressed mothers received services for their depression. Black and Hispanic depressed mothers were more likely to experience multiple adversities and less likely to receive services than white depressed mothers.
Conclusions
Maternal depression is a major public health problem in the United States, with an estimated 1 in 10 children experiencing a depressed mother in any given year. Professionals who work with mothers and children should be aware of its prevalence and its detrimental effects.
Introduction
Depression among mothers and other caregivers of young children is increasingly recognized as a common and devastating public health problem affecting not only women but also the children in their care. Salient features and correlates of depression have significant potential to impair a mother's ability to effectively and adequately care for children. Major depression causes severe impairments in functioning,1 has high rates of comorbidity with other psychologic disorders,1,2 and is associated with stressful life events, including job loss and divorce.3 Studies of depressed mothers have documented impairments in maternal functioning. Depressed mothers provide less stimulation, are less responsive to infants, and show more parenting difficulties.4–6 Additionally, depressed mothers are less likely to seek and receive appropriate medical care for their infants7 and less likely to engage in prevention practices, such as using a car seat and having a working smoke alarm in the home.8–10 Children exposed to maternal depression are at higher risk of delayed cognitive and language development,11 mental health problems,12,13 suboptimal physical growth,14–16 and a wide range of interpersonal, neuroendocrine, and behavioral problems.17 Maternal depression has been associated with offspring's poorer outcomes in infancy, childhood, adolescence, and adulthood. Because of the serious and potentially lifelong adverse effects of maternal depression on children, it is imperative that we have accurate information about rates of maternal depression, risk factors for maternal depression, and comorbidities and other adversities that frequently co-occur with depression among mothers. This information is critical for research, policy, and intervention activities to promote well-being among children and their mothers.
National studies of psychiatric disorders have not focused on depression among mothers; thus, we have limited understanding of the national burden of this disorder among mothers caring for children. Studies of depression among mothers have largely focused on local community or clinic-based samples. There is a large body of research specific to depression in the perinatal period, with a meta-analysis of 59 studies reporting a prevalence of 13% for postpartum depression18; however, there is a wide range in prevalence estimates across studies,18,19 which likely is due in part to a lack of generalizability of previous studies.20 There are fewer estimates of the prevalence of depression among mothers of older children, although rates of depression appear to be similar throughout the childbearing years.20–22 Lack of information about the prevalence of maternal depression has hindered an appropriately scaled public health response to this disorder.20
Surveys of mothers have typically assessed depressive symptomatology rather than the diagnosis of major depression.23–30 These studies provide critical information, but it is important to make the distinction between depressive symptomatology and major depression because prevalence estimates as well as predictive factors may vary considerably whether based on depressive symptomatology or diagnostic criteria.31 Further, despite a longstanding interest in racial and ethnic disparities in mental health,32–35 we have very limited understanding of racial or ethnic disparities in depression among mothers.
This article examines the public health burden of depression and its correlates among a nationally representative sample of U.S. mothers. We used data from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC) to (1) examine the overall prevalence and sociodemographic patterns of depression among mothers, (2) assess the functioning of mothers with depression, as well as the prevalence of maternal comorbidities and adversities that may impair mothering, the mother-child relationship, or the child directly, and (3) evaluate racial/ethnic disparities related to maternal depression.
Materials and Methods
Sample
We used data from the 2001–2002 Wave of the NESARC, conducted by the National Institute on Alcohol Abuse and Alcoholism.36 The NESARC used a multistage sampling design to yield a nationally representative sample of the civilian, noninstitutionalized adult (aged ≥18 years) U.S. population, including citizens and noncitizens. NESARC staff conducted in-person interviews with 43,093 subjects and had an overall response rate of 81%. Several subpopulations were oversampled, including racial/ethnic minority groups. We included 8916 women who were mothers to children < age 18 at the time of the survey. We identified mothers as female respondents (n=24,575) who at the time of the interview had at least one child (including biologic, adoptive, step, and foster children) <18 years of age (n=9,205). We further defined childcaring mothers as those who were currently living in the same household as a child < age 18 years (n=8,480). If a female respondent did not report having a child but was either the only adult or the only female adult in the household with a child < age 18, we considered her to be the primary female caregiver for that child and included her as a childcaring mother (n=436). These childcaring mothers were older, less educated, and more likely to be black or African American and had lower rates of past-year depression compared to childcaring mothers who reported having children. The current study considers depression among childcaring mothers, (n=8,480+436=8,916) and does not consider depression among women who do not currently live with a child. Results restricted to mothers who reported having children (n=8,480) do not differ from results that include both types of mothers; thus, all results reported are for all childcaring mothers (n=8,916).
Measures
Psychiatric disorders were assessed with the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV),37 a structured interview protocol that allows diagnoses based on the Diagnostic and Statistical Manual of Mental Disorders, Revised 4th ed. In this analysis, the presence of major depression in the past 12 months was our primary focus. Test-retest reliability of the AUDADIS-IV measure of past-year major depression has been shown to be good (kappa=0.59 38). Comorbid conditions considered were past-year anxiety disorder (including panic disorder, social phobia, specific phobia, and generalized anxiety disorder), substance use disorders (alcohol or drug abuse or dependence), and nicotine dependence. Kappa values for past-year anxiety disorders ranged from 0.40 to 0.52 and for alcohol and tobacco dependence and abuse ranged from 0.63 to 0.74.38 Test-retest reliability for the AUDADIS-IV diagnoses used in this analysis are similar to those reported for the World Health Organization's (WHO) Composite International Diagnostic Inventory (CIDI).39 We created an indicator for past-year use of services for depression (hereafter referred to as service use or services) among those with past-year depression if the respondent endorsed any of the following: went to counselor/therapist/doctor/other to improve mood; stayed overnight in hospital because of depression; went to emergency room for help because of depression; doctor prescribed medicine/drug to improve mood.
Sociodemographic variables of interest included age, race/ethnicity, nativity (U.S.-born or foreign-born), highest level of education, marital status, household income, and employment status. The number of children in the household and their ages were also included in our analyses. All were self-reported during the interview.
Functioning and impairment was assessed with the 12-item Short Form Health Survey (SF12-V2).40,41 This assessment tool taps several domains and was used to create the following norm-based summary scales (range 0–100, mean 50): physical disability, physical functioning, role physical, social functioning, role emotional, mental health, and a mental health component summary scale. Respondents were asked if they had experienced 12 negative life events in the 12 months preceding the interview. In this analysis, we were particularly interested in those life events likely to affect children, so we focus on whether the mother was fired, laid off, or became unemployed; got separated or divorced or broke off a steady relationship; and experienced a major financial crisis, declared bankruptcy or more than once was unable to pay her bills on time. We also created an indicator for poverty, defined as a family income <150% of the poverty line, based on number of people in the household and the poverty thresholds for the year of the survey. Because social and economic adversities tend to cluster, we created a count of the number of adversities the mother experienced in the past year by summing presence of the following: living in poverty, divorced or separated, fired or unemployed, experienced a financial crisis.
Data analysis
The NESARC provides sample weights to adjust the dataset for selection and nonresponse so that it can be generalized to the national population. We present weighted percentages and unweighted sample sizes in univariate and bivariate tabulations. We tested for group differences using chi-square tests for categorical variables and t tests for continuous variables. We examined correlates of depression among non-Hispanic white, non-Hispanic black, and Hispanic childcaring mothers; other ethnic groups were too small to allow meaningful analysis. We used logistic regression to identify sociodemographic and child characteristics associated with depression among mothers. Using the number of children < age 18 in the household, the sample weight for each mother, and the mother's past-year depression status, we estimated the number of children exposed to maternal depression in the past year in the United States. The NESARC study performed imputation for item nonresponse,36 enabling a complete case assessment for this analysis. All analyses used the statistical software SUDAAN.
Results
More than 1 in 10 mothers suffered from depression in the past 12 months. As displayed in Table 1, depression in mothers was related to sociodemographic factors, with whites and Native Americans, U.S.-born women, those with low levels of education or income, and those unemployed or unmarried showing high rates of depression. The presence of depression did not appear to be strongly associated with number of or age of children. One in 10 children, or 7,667,637 children, were exposed to mothers with major depression in the past year. Models predicting depression (Table 2) showed that unmarried mothers <35 years, with low education and low income were at higher risk of past-year depression. Black race and Hispanic ethnicity emerged as protective factors, with 0.53 and 0.63, respectively, odds of depression compared to white mothers in similar socioeconomic and marital situations. Number of children was not associated with odds of depression in mothers; there was some indication that mothers of children <1 year of age were at higher risk of depression, although the confidence interval included the null (Table 2).
Table 1.
Sociodemographic Characteristics of Mothers by Past-Year Depression Status: National Epidemiologic Survey on Alcohol and Related Conditions, 2001–2002
| |
Mothers by past-year depression |
|
|||
|---|---|---|---|---|---|
| |
No (n=8008, 89.8%) |
Yes (n=908, 10.2%) |
|
||
| % | n | % | n | p value | |
| Age | <0.01 | ||||
| 18–24 | 85.70 | 856 | 14.30 | 131 | |
| 25–34 | 88.07 | 2615 | 11.93 | 345 | |
| 35–44 | 90.87 | 3179 | 9.13 | 311 | |
| 45+ | 92.31 | 1358 | 7.69 | 121 | |
| Race/ethnicity | <0.01 | ||||
| White | 88.54 | 3582 | 11.46 | 481 | |
| Black | 91.36 | 1899 | 8.64 | 177 | |
| Native American | 81.83 | 118 | 18.17 | 31 | |
| Asian/Hawaiin/Pacific Islander | 93.62 | 260 | 6.38 | 17 | |
| Hispanic | 92.92 | 2149 | 7.08 | 202 | |
| Education | <0.01 | ||||
| <High school | 86.87 | 1370 | 13.13 | 175 | |
| Completed high school | 88.81 | 2267 | 11.19 | 279 | |
| Some college | 88.96 | 2608 | 11.04 | 327 | |
| Completed 4-year college+ | 93.28 | 1763 | 6.72 | 127 | |
| Marital status | <0.01 | ||||
| Married | 91.34 | 4806 | 8.66 | 425 | |
| Living together | 87.47 | 312 | 12.53 | 34 | |
| Widowed | 86.70 | 151 | 13.30 | 22 | |
| Divorced or separated | 83.12 | 1410 | 16.88 | 257 | |
| Never married | 88.00 | 1329 | 12.00 | 170 | |
| Household income | <0.01 | ||||
| Lowest quartile (<$20,000) | 85.20 | 2019 | 14.80 | 334 | |
| Mid-low quartile ($20,000–39,999) | 88.96 | 2239 | 11.04 | 245 | |
| Mid-high quartile ($40,000–69,999) | 89.72 | 1965 | 10.28 | 205 | |
| Highest quartile (>$70,000) | 93.44 | 1785 | 6.56 | 124 | |
| Current employment status | <0.01 | ||||
| Employed full-time | 91.95 | 4162 | 8.05 | 368 | |
| Employed part-time | 89.75 | 1230 | 10.25 | 150 | |
| Unemployed | 75.44 | 650 | 24.56 | 184 | |
| Retired or other | 89.87 | 1966 | 10.13 | 206 | |
| Nativity | <0.01 | ||||
| Foreign-born | 95.29 | 1801 | 4.71 | 107 | |
| U.S.-born | 88.47 | 6184 | 11.53 | 801 | |
| Number of children | 0.37 | ||||
| One | 89.80 | 3121 | 10.20 | 365 | |
| Two | 89.75 | 2952 | 10.25 | 318 | |
| Three | 90.57 | 1327 | 9.43 | 140 | |
| Four+ | 86.81 | 608 | 13.19 | 85 | |
| Age of child(ren)a | |||||
| <1 | 85.31 | 352 | 14.69 | 54 | 0.07 |
| 1–4 | 89.03 | 3113 | 10.97 | 369 | 0.21 |
| 5–12 | 90.08 | 4993 | 9.92 | 542 | 0.25 |
| 13–15 | 89.78 | 2190 | 10.22 | 250 | 0.90 |
| 16–17 | 89.59 | 1388 | 10.41 | 163 | 0.91 |
Weighted percentages and actual sample sizes are presented.
Chi-square p values account for the weighted sample.
Categories are not mutually exclusive for mothers who have children in more than one age group.
Table 2.
Models Predicting Past-Year Depression Among Mothers: National Epidemiologic Survey on Alcohol and Related Conditions, 2001–2002
| |
Model 1: Sociodemographic factors |
Model 2: Sociodemographic + child factors |
||
|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |
| Age | ||||
| 18–24 | 1.38 | (1.02-1.85) | 1.40 | (0.97-2.02) |
| 25–34 | 1.34 | (1.09-1.65) | 1.43 | (1.11-1.84) |
| 35–44 | 1 (ref) | 1 (ref) | ||
| 45+ | 0.80 | (0.59-1.09) | 0.78 | (0.57-1.06) |
| Race/ethnicity | ||||
| White | 1 (ref) | 1 (ref) | ||
| Black | 0.53 | (0.41-0.70) | 0.53 | (0.40-0.69) |
| Native American | 1.29 | (0.76-2.20) | 1.26 | (0.74-2.16) |
| Asian/Hawaiin/Pacific Islander | 1.05 | (0.56-1.97) | 1.04 | (0.55-1.96) |
| Hispanic | 0.63 | (0.48-0.82) | 0.62 | (0.48-0.81) |
| Education | ||||
| <High school | 1.65 | (1.16-2.36) | 1.61 | (1.12-2.33) |
| Completed high school | 1.30 | (0.99-1.70) | 1.29 | (0.98-1.69) |
| Some college | 1.39 | (1.07-1.79) | 1.38 | (1.07-1.78) |
| Completed 4-year college+ | 1 (ref) | 1 (ref) | ||
| Marital status | ||||
| Married | 1 (ref) | 1 (ref) | ||
| Living together | 1.23 | (0.79-1.93) | 1.22 | (0.78-1.91) |
| Widowed | 1.58 | (0.78-3.23) | 1.58 | (0.78-3.22) |
| Divorced or separated | 1.87 | (1.47-2.39) | 1.85 | (1.45-2.37) |
| Never married | 1.10 | (0.83-1.46) | 1.10 | (0.83-1.47) |
| Household income | ||||
| Lowest quartile (<$20,000) | 1.53 | (1.09-2.15) | 1.54 | (1.10-2.16) |
| Mid-low quartile ($20,000–39,999) | 1.35 | (0.99-1.83) | 1.36 | (1.00-1.85) |
| Mid-high quartile ($40,000–69,999) | 1.39 | (1.02-1.89) | 1.39 | (1.03-1.89) |
| Highest quartile (>$70,000) | 1(ref) | 1(ref) | ||
| Current employment status | ||||
| Employed full-time | 1 (ref) | 1(ref) | ||
| Employed part-time | 1.32 | (1.04-1.68) | 1.31 | (1.04-1.66) |
| Unemployed | 3.27 | (2.50-4.28) | 3.24 | (2.48-4.24) |
| Retired or other | 1.35 | (1.07-1.71) | 1.34 | (1.05-1.72) |
| Nativity | ||||
| Foreign-born | 0.41 | (0.29-0.57) | 0.41 | (0.30-0.57) |
| U.S.-born | 1 (ref) | 1 (ref) | ||
| Number of children | ||||
| One | 1 (ref) | |||
| Two | 1.03 | (0.80-1.32) | ||
| Three | 0.89 | (0.61-1.31) | ||
| Four+ | 1.12 | (0.69-1.81) | ||
| Age of child(ren)a | ||||
| <1 | 1.31 | (0.84-2.04) | ||
| 1–4 | 1.02 | (0.76-1.37) | ||
| 5–12 | 0.95 | (0.72-1.25) | ||
| 13–15 | 1.14 | (0.86-1.51) | ||
| 16–17 | 1.19 | (0.87-1.62) | ||
Catagories are not mutually exclusive.
CI, confidence interval; OR, odds ratio; ref, reference.
Factors associated with depression that are likely to impair a mother's ability to care for children are considered in Table 3. Depressed women were more likely to experience adversities, including those related to employment, personal relationships, and financial security. They were also more likely to have comorbid conditions, including anxiety disorder, substance use/disuse disorders, and nicotine dependence. The clustering of adversities among those with depression was also evident, with less than half of mothers without depression experiencing any of these adversities, and over two thirds of depressed mothers experiencing at least one adversity (data not shown). Among mothers with past-year depression, 49.6% received services in the 12 months preceding the interview. Those with depression had statistically significantly worse functioning on all SF-12 scales and were particularly worse in terms of social functioning, role limitations due to emotional problems, and mental health (data not shown).
Table 3.
Risk Factors Associated with Maternal Depression: National Epidemiologic Survey on Alcohol and Related Conditions, 2001–2002
| |
Mothers by past-year depression |
|
Mothers with depression by race/ethnicity |
|
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |
No (n=8008) |
Yes (n=908) |
|
NH white (n=481) |
NH black (n=177) |
Hispanic (n=202) |
|
|||||
| % | n | % | n | p value | % | n | % | n | % | n | p value | |
| Adversities in past year | ||||||||||||
| Fired or unemployed | 11.45 | 1055 | 25.93 | 244 | <0.01 | 21.31 | 111 | 36.04 | 55 | 33.37 | 59 | 0.02 |
| Separated or divorced | 5.81 | 611 | 18.72 | 204 | <0.01 | 17.58 | 104 | 25.15 | 46 | 21.16 | 44 | 0.19 |
| Financial crisis | 14.23 | 1306 | 42.25 | 423 | <0.01 | 38.47 | 206 | 54.02 | 98 | 45.65 | 88 | 0.02 |
| Income <150% poverty threshold | 27.35 | 2730 | 38.52 | 411 | <0.01 | 32.47 | 176 | 59.22 | 108 | 52.79 | 106 | <0.01 |
| Psychologic comorbidities in past year | ||||||||||||
| Anxiety disorder | 12.18 | 928 | 43.25 | 367 | <0.01 | 45.84 | 219 | 38.37 | 63 | 33.20 | 65 | 0.03 |
| Substance or alcohol use/misuse | 4.25 | 334 | 14.76 | 138 | <0.01 | 15.29 | 84 | 14.59 | 22 | 14.03 | 26 | 0.94 |
| Nicotine dependence | 11.34 | 838 | 34.79 | 274 | <0.01 | 38.86 | 178 | 27.28 | 45 | 22.75 | 37 | <0.01 |
| Past-year service use among those with past-year depressiona | ||||||||||||
| No service use | 50.37 | 472 | 46.92 | 224 | 64.53 | 113 | 58.63 | 111 | <0.01 | |||
| Received services | 49.63 | 430 | 53.08 | 255 | 35.47 | 62 | 41.37 | 90 | ||||
Weighted percentages and actual sample sizes are presented.
Six subjects have missing data for past-year treatment because they did not provide information about when they sought treatment for their depression.
NH, non-Hispanic.
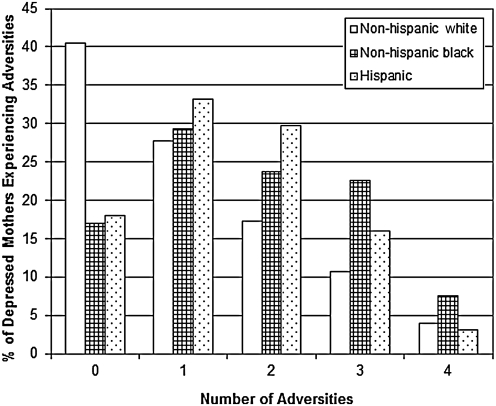
When examined by race, we found that depressed non-Hispanic black mothers, compared to depressed non-Hispanic white and Hispanic mothers, had elevated rates of adversities and were less likely to receive services for their mood disorder in the past year (Table 3). Depressed non-Hispanic white mothers were the most likely to have comorbid conditions. Clustering of adversities was pronounced among depressed non-Hispanic black and Hispanic mothers, with 54% and 49%, respectively, experiencing two or more adversities compared to 32% of non-Hispanic white mothers (Fig. 1). Depressed non-Hispanic black mothers, compared to depressed white and Hispanic mothers, also showed worse functioning on the physical functioning (46.8 vs. 49.9 and 50.4, respectively, p<0.05 for both comparisons) and role physical (46.4 vs. 48.8 and 49.2, respectively, p<0.05 for both comparisons) SF-12 scales.
FIG. 1.
Adversities by race/ethnicity among depressed mothers: National Epidemiologic Survey on Alcohol and Related Conditions, 2001–2002. Number of adversities is the sum of the following in the past year: <150% poverty threshold, divorced or separated, fired or unemployed, financial crisis.
Discussion
Approximately 1 in 10 mothers (10.2%) suffered from major depressive disorder (MDD) in the past year. In fact, the 12-month prevalence of depression in mothers was elevated compared to all women in the NESARC (6.9%)2 and slightly higher than among women who were pregnant in the past year (9.3%).42 The prevalence of maternal depression translates into 1 in 10 children, or 7,667,637 children, exposed to mothers with MDD in the past year. Risk of depression was higher among younger mothers (≤35 years), white mothers, those who were divorced or separated, those with less than a college education, and those who were unemployed or with low household income. Sociodemographic factors associated with depression among mothers were similar to those found for the general population in recent large epidemiologic studies.1,2
The finding that depression is higher among young mothers and mothers with young children is particularly concerning given the persistence of early symptoms. In a large, longitudinal study, Horwitz et al.22,43 documented that of mothers with high depressive symptoms early in the child's life (11–42 months), almost half continued to have elevated symptoms 1 year later, and a significant portion continued to have high depressive symptoms when the child was entering kindergarten. Exposure to chronic maternal depression has a greater negative effect on children and the mother-child relationship compared to less chronic maternal depression.44–46
Depressed mothers reported more stressful life events in the past year, including marital dissolution, poverty, and events associated with economic hardship. Family disruptions and economic hardships are independent risk factors for adverse behavioral and psychologic outcomes in children, with influences on health observed to extend into adulthood.47–51 Depressed mothers were also more likely than nondepressed mothers to have other psychologic conditions. Depression comorbid with another psychopathology may exacerbate parenting difficulties.52 Multiple psychologic conditions, as well as high levels of stressful life events, increase the likelihood of persistent depressive symptoms among mothers of young children.22,43 Thus, children with depressed mothers are significantly more likely to be exposed to a range of adversities associated with compromised caregiving and adverse behavioral and health outcomes across the life course.
Only half of depressed mothers received services in the past year for their depression; this rate was even lower among black and Hispanic mothers. Service use rates among mothers were lower than the estimated 57% rate among all past-year depressed individuals.1 It is important to note that the measure of service use is broad (including seeing a counselor/therapist/doctor/other, visiting the emergency room or hospital, and doctor-prescribed medicine/drug for depression) and is self-reported; thus, it does not indicate type of treatment received, dose, duration, or quality, nor do we have verification that services were actually received. Successful treatment of maternal depression is crucial and has been shown to positively affect psychiatric symptoms and disorders in middle childhood and adolescence.53,54 However, there is evidence that treatments that focus solely on treating maternal depression may not adequately address problems in the mother-child relationship that emerge as a result of maternal depression.55,56
Consistent with the U.S. population of women in general, we found that Hispanic and black mothers were less likely to suffer from depression in the past year compared to non-Hispanic white mothers.2 This racial/ethnic pattern has also been reported for lifetime rates of depression in other samples not stratified by gender.32,34,57,58 An item-response examination in the NESARC dataset revealed few differences in response likelihood when comparing white, black, and Hispanic individuals, suggesting these observed differences are not explained by racial or cultural differences in experience or reporting of symptoms of depression.59 A similar study in the National Comorbidity Survey concluded that differences in response to depression questions did not account for the lower rates of depression among non-Hispanic black and Hispanic individuals compared to non-Hispanic white individuals.60 The reasons for these patterns are yet to be fully illuminated, although protective factors operating early in life have been hypothesized to play a role.32 For immigrants, one protective factor may be remaining in their home country through childhood.61 Future research should explore whether strong family or cultural ties, religious participation, and other social support networks play a protective role among black and Hispanic populations and if this helps account for their lower rates of depression.35,62 Such factors may be particularly powerful in promoting mental health among mothers.
Hispanic and non-Hispanic black mothers who were depressed experienced more adversities, had worse functioning, and were less likely to receive services for their depression compared to non-Hispanic white mothers. These patterns, again, reflect findings from studies not restricted to mothers58,63 yet raise important questions about the implications of these riskier profiles among racial/ethnic minority mothers for the children in their care. Exposure to multiple adversities in childhood may greatly increase risk of poor health and health-related behavior in adulthood.64 Research that addresses racial and ethnic disparities in the impact of maternal depression on children is needed and may lead to the formulation of targeted prevention and intervention efforts, particularly among children most at risk of adverse outcomes.
Several limitations of this study should be considered. NESARC focused on adults and their psychopathologies; thus, we have very little information about the children, precluding analysis of their health status, living conditions, and interactions with their mothers. Also, as NESARC does not ask participants directly if they are currently parenting children in the household, we relied on report of births or adoptions and household composition. Thus, it is possible that we included some women who were not the primary female caregiver of the children in the household. Inclusion of paternal depression was beyond the scope of this analysis; however, paternal depression is positively correlated with maternal depression and may pose additional developmental risk to children.65 All data are self-reported, and as it is a cross-sectional study, we cannot establish temporality or causal relations.
Conclusions
This study is the first to examine the public health burden of maternal depression in a nationally representative sample using a structured diagnostic instrument to assess major depression. The information that 1 in 10 mothers suffered from past-year depression argues for routine screening for depression among mothers in the pediatric and primary care settings. Similarly, the information that 1 in 10 children experience a depressed mother in any given year highlights the importance of research in this arena to understand the broad array of child health and development outcomes affected by exposure to a depressed parent.
Acknowledgments
K.A.E. is supported by the Kellogg Health Scholars Program. K.C.K. is supported by MH070627. The authors would like to thank Dr. Natalie Slopen and Dr. Andrea Roberts for their assistance with data analysis.
Disclosure Statement
No competing financial interests exist.
References
- 1.Kessler R. Berglund P. Demler O, et al. The epidemiology of major depressive disorder: Results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 2.Hasin D. Goodwin RD. Stinson FS. Grant BF. Epidemiology of major depressive disorder: Results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry. 2005;62:1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 3.Kessler R. Zhao S. Blazer DG. Swartz M. Prevalence, correlates, and course of minor depression and major depression in the National Comorbidity Survey. J Affect Disord. 1997;45:19–30. doi: 10.1016/s0165-0327(97)00056-6. [DOI] [PubMed] [Google Scholar]
- 4.Bettes B. Maternal depression and motherese: Temporal and intonational features. Child Dev. 1988;59:1089–1096. doi: 10.1111/j.1467-8624.1988.tb03261.x. [DOI] [PubMed] [Google Scholar]
- 5.Lovejoy M. Graczyk PA. O'Hare E. Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clin Psycho Rev. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 6.Reck C. Hunt A. Fuchs T, et al. Interactive regulation of affect in postpartum depressed mothers and their infants. Psychopathology. 2003;37:272–280. doi: 10.1159/000081983. [DOI] [PubMed] [Google Scholar]
- 7.Minkovitz C. Strobino D. Scharfstein D, et al. Maternal depressive symptoms and children's receipt of health care in the first 3 years of life. Pediatrics. 2005;115:306–314. doi: 10.1542/peds.2004-0341. [DOI] [PubMed] [Google Scholar]
- 8.McLennan J. Kotelchuck M. Parental prevention practices for young children in the context of maternal depression. Pediatrics. 2000;105:1090–1095. doi: 10.1542/peds.105.5.1090. [DOI] [PubMed] [Google Scholar]
- 9.Chung E. McCollum KF. Elo IT. Lee HJ. Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113:e523–e529. doi: 10.1542/peds.113.6.e523. [DOI] [PubMed] [Google Scholar]
- 10.Leiferman J. The effect of maternal depressive symptomatology on maternal behaviors associated with child health. Health Edu Behav. 2002;29:596–607. doi: 10.1177/109019802237027. [DOI] [PubMed] [Google Scholar]
- 11.Sohr-Preston S. Scaramella LV. Implications of timing of maternal depressive symptoms for early cognitive and language development. Clin Child Fam Psychol Rev. 2006;9:65–83. doi: 10.1007/s10567-006-0004-2. [DOI] [PubMed] [Google Scholar]
- 12.Hammen C. Burge D. Burney E. Adrian C. Longitudinal study of diagnoses in children of women with unipolar and bipolar affective disorder. Arch Gen Psychiatry. 1990;47:1112–1117. doi: 10.1001/archpsyc.1990.01810240032006. [DOI] [PubMed] [Google Scholar]
- 13.Lieb R. Isensee B. Hofler M. Pfister H. Wittchen HU. Parental major depression and the risk of depression and other mental disorders in offspring: A prospective-longitudinal community study. Arch Gen Psychiatry. 2002;59:365–374. doi: 10.1001/archpsyc.59.4.365. [DOI] [PubMed] [Google Scholar]
- 14.Ertel KA. Koenen KC. Rich-Edwards JW. Gillman MW. Antenatal and postpartum depressive symptoms are differentially associated with early childhood weight and adiposity. Paediatr Perinat Epidemiol. 2010;24:179–189. doi: 10.1111/j.1365-3016.2010.01098.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Field T. Diego M. Hernandez-Reif M. Prenatal depression effects on the fetus and newborn: A review. Infant Behav Dev. 2006;29:445–455. doi: 10.1016/j.infbeh.2006.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Stewart R. Maternal depression and infant growth—A review of recent evidence. Matern Child Nutr. 2007;3:94–107. doi: 10.1111/j.1740-8709.2007.00088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goodman S. Tully EC. Depression in women who are mothers: An integrative model of risk for the development of psychopathology in their sons and daughters. In: Keyes CLM, editor; Goodman HG, editor. Women and depression: A handbook for the social, behavioral, and biomedical sciences. New York: Cambridge University Press; 2006. pp. 241–282. [Google Scholar]
- 18.O'Hara M. Swain AM. Rates and risk of postpartum depression—A meta-analysis. Int Rev Psychiatry. 1996;8:37–54. [Google Scholar]
- 19.Gavin N. Gaynes B. Lohr K. Meltzer-Brody S. Gartlehner G. Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obste Gynecol. 2005;106:1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- 20.McLennan J. Kotelchuck M. Cho H. Prevalence, persistence, and correlates of depressive symptoms in a national sample of mothers of toddlers. J Am Acad Child Adolesc Psychiatry. 2001;40:1316–1323. doi: 10.1097/00004583-200111000-00012. [DOI] [PubMed] [Google Scholar]
- 21.Somerset W. Newport DJ. Ragan K. Stowe ZN. Depressive disorders in women: From menarche to beyond the menopause. In: Keyes CLM, editor; Goodman HG, editor. Women and depression: A handbook for the social, behaviorl, and biomedical sciences. New York: Cambridge University Press; 2006. pp. 62–128. [Google Scholar]
- 22.Horwitz S. Briggs-Gowan MJ. Storfer-Isser A. Carter AS. Persistence of maternal depressive symptoms throughout the early years of childhood. J Womens Health. 2009;18:637–645. doi: 10.1089/jwh.2008.1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Heneghan A. Silver EJ. Bauman LJ. Westbrook LE. Stein RE. Depressive symptoms in inner-city mothers of young children: Who is at risk? Pediatrics. 1998;102:1394–1400. doi: 10.1542/peds.102.6.1394. [DOI] [PubMed] [Google Scholar]
- 24.Orr S. James S. Maternal depression in an urban pediatric practice: Implications for health care delivery. Am J Public Health. 1984;74:363–365. doi: 10.2105/ajph.74.4.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Deal L. Holt VL. Young maternal age and depressive symptoms: Results from the 1988 National Maternal and Infant Health Survey. Am J Public Health. 1998;88:266–270. doi: 10.2105/ajph.88.2.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Silver E. Heneghan AM. Bauman LJ. Stein RE. The relationship of depressive symptoms to parenting competence and social support in inner-city mothers of young children. Matern Child Health J. 2006;10:105–112. doi: 10.1007/s10995-005-0024-4. [DOI] [PubMed] [Google Scholar]
- 27.Dubowitz H. Feigelman S. Lane W, et al. Screening for depression in an urban pediatric primary care clinic. Pediatrics. 2007;119:435–443. doi: 10.1542/peds.2006-2010. [DOI] [PubMed] [Google Scholar]
- 28.Paulson J. Keefe HA. Leiferman JA. Early parental depression and child language development. J Child Psychol Psychiatry. 2009;50:254–262. doi: 10.1111/j.1469-7610.2008.01973.x. [DOI] [PubMed] [Google Scholar]
- 29.Lanzi R. Pasco JM. Keltner B. Ramey SL. Correlates of maternal depressive symptoms in a national Head Start Program sample. Arch Pediatr Adolesc Med. 1999;153:801–807. doi: 10.1001/archpedi.153.8.801. [DOI] [PubMed] [Google Scholar]
- 30.Huang Z. Wong FY. Ronzio CR. Yu SM. Depressive symptomatology and mental health help-seeking patterns of U.S.- and foreign-born mothers. Matern Child Health J. 2007;11:257–267. doi: 10.1007/s10995-006-0168-x. [DOI] [PubMed] [Google Scholar]
- 31.O'Hara M. Neunaber DJ. Zekoski EM. Prospective study of postpartum depression: Prevalence, course and predictive factors. J Abnorm Psychol. 1984;93:158–171. doi: 10.1037//0021-843x.93.2.158. [DOI] [PubMed] [Google Scholar]
- 32.Breslau J. Aguilar-Gaxiola S. Kendler KS. Su M. Williams D. Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Breslau J. Kendler KS. Su M. Gaxiola-Aguilar S. Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. 2005;35:317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Alegria M. Canino G. Shrout PE, et al. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino subgroups. Am J Psychiatry. 2008;165:359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alegria M. Shrout PE. Woo M, et al. Understanding differences in past year psychiatric disorders for Latinos living in the US. Soc Sci Med. 2007;65:214–230. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Grant B. Kaplan K. Shepard J. Moore T. Source and Accuracy Statement for Wave 1 of the 2001–2003 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 37.Grant B. Dawson DA. Hasin DS. The Alcohol Use Disorder and Associated Disabilities Interview Schedule—DSM-IV version. Bethesda MD: National Institute on Alcohol Abuse and Alcoholism; 2001. [Google Scholar]
- 38.Grant B. Dawson DA. Stinson FS. Chou PS. Kay W. Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 39.Wittchen H. Reliability and validity studies of the WHO Composite International Diagnostic Interview (CIDI): A critial review. J Psychiatr Res. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 40.Ware J. Kosinski M. Turner Bowker DM. Gandek B. How to score version 2 of the SF-12 Health Survey. Lincoln, RI: Quality Metrics; 2002. [Google Scholar]
- 41.Ware J. Kosinski M. Keller SD. A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Vesga-Lopez O. Blanco C. Keyes K. Olfson M. Grant BF. Hasin DS. Psychiatric disorders in pregnant and postpartum women in the United States. Arch Gen Psychiatry. 2008;65:805–815. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Horwitz S. Briggs-Gowan MJ. Storfer-Isser A. Carter AS. Prevalence, correlates, and persistence of maternal depression. J Womens Health. 2007;16:678–691. doi: 10.1089/jwh.2006.0185. [DOI] [PubMed] [Google Scholar]
- 44.National Institute of Child Health Human Development Early Child Care Research Network. Chronicity of maternal depressive symptoms, maternal sensitivity and child functioning at 36 months. Dev Psychol. 1999;35:1297–1310. doi: 10.1037//0012-1649.35.5.1297. [DOI] [PubMed] [Google Scholar]
- 45.Ashman SB. Dawson G. Panagiotides H. Trajectories of maternal depression over 7 years: Relations with child psychophysiology and behavior and role of contextual risks. Dev Psychopathol. 2008;20:55–77. doi: 10.1017/S0954579408000035. [DOI] [PubMed] [Google Scholar]
- 46.Brennan P. Andersen MJ. Hammen C. Bor W. Najman JM. Williams GH. Chronicity, severity and timing of maternal depressive symptoms: Relationships with child outcomes at age 5. Dev Psychol. 2000;36:759–766. doi: 10.1037//0012-1649.36.6.759. [DOI] [PubMed] [Google Scholar]
- 47.Clavarino A. Hayatbakhsh MR. Williams GM, et al. Depression following marital problems: Different impacts on mothers and their children? A 21-year prospective study. Soc Psychiatry Psychiatr Epidemiol. 2010 doi: 10.1007/s00127-010-0253-8. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 48.Poulton R. Caspi A. Milne BJ, et al. Association between children's experience of socioeconomic disadvantage and adult health: A life-course study. Lancet. 2002;360:1640–1645. doi: 10.1016/S0140-6736(02)11602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zill N. Morrison DR. Coiro M. Long-term effects of parental divorce on parent-child relationships, adjustment, and achievement in young adulthood. J Fam Psychol. 1993;7:91–103. [Google Scholar]
- 50.Amato P. Sobolewski JM. The effects of divorce and marital discord on adult children's psychological well-being. Am Sociol Rev. 2001;66:900–921. [Google Scholar]
- 51.Bor W. Najman JM. Andersen M. Morrison J. Williams G. Socioeconomic disadvantage and child morbidity: An Australian longitudinal study. Soc Sci Med. 1993;36:1053–1061. doi: 10.1016/0277-9536(93)90123-l. [DOI] [PubMed] [Google Scholar]
- 52.Carter A. Garrity-Rokous E. Chazan-Cohen R. Little C. Briggs-Gowan MJ. Maternal depression and comorbidity: Predicting early parenting, attachment security, and toddler social-emotional problems and competencies. J Am Acad Child Adolesc Psychiatry. 2001;40:18–26. doi: 10.1097/00004583-200101000-00012. [DOI] [PubMed] [Google Scholar]
- 53.Weissman M. Pilowsky D. Wickramaratne P, et al. Remissions in maternal depression and child psychopathology: A STAR*D-child report. JAMA. 2006;295:1389–1398. doi: 10.1001/jama.295.12.1389. [DOI] [PubMed] [Google Scholar]
- 54.Pilowsky D. Wickramaratne P. Talati A, et al. Children of depressed mothers 1 year after the initiation of maternal treatment: Findings from the STAR*D-Child Study. Am J Psychiatry. 2008;165:1136–1147. doi: 10.1176/appi.ajp.2008.07081286. [DOI] [PubMed] [Google Scholar]
- 55.Forman D. O'Hara MW. Stuart S. Gormann LL. Larsen KE. Coy KC. Effective treatment for postpartum depression is not sufficient to improve the developing mother-child relationship. Dev Psychopathol. 2007;19:585–602. doi: 10.1017/S0954579407070289. [DOI] [PubMed] [Google Scholar]
- 56.Murray L. Cooper PJ. Wilson A. Romaniuk H. Controlled trial of the short- and long-term effect of psychological treatment of post-partum depression 2. Impact on the mother-child relationship and child outcome. Br J Psychiatry. 2003;182:420–427. [PubMed] [Google Scholar]
- 57.Riolo S. Nguyen TA. Greden JF. King CA. Prevalence of depression by race/ethnicity: Findings from the National Helath and Nutrition Examination Survey III. Am J Public Health. 2005;95:998–1000. doi: 10.2105/AJPH.2004.047225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Williams DR. Gonzalez HM. Neighbors H, et al. Prevalence and distribution of major depressive disorder in African Americans, Caribbean blacks, and non-Hispanic whites: Results from the National Survey of American Life. Arch Gen Psychiatry. 2007;64:305–315. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- 59.Uebelacker L. Strong D. Weinstock LM. Miller IW. Use of item response theory to understand differential functioning of DSM-IV major depression symptoms by race, ethnicity and gender. Psychol Med. 2009;39:591–601. doi: 10.1017/S0033291708003875. [DOI] [PubMed] [Google Scholar]
- 60.Breslau J. Javaras KN. Blacker D. Murphy JM. Normand ST. Differential item functioning between ethnic groups in the epidemiological assessment of depression. J Nerv Ment Dis. 2008;196:297–306. doi: 10.1097/NMD.0b013e31816a490e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Breslau J. Borges G. Hagar Y. Tancredi D. Gilman S. Immigration to the USA and risk for mood and anxiety disorders: Variation by origin and age at immigration. Psychol Med. 2009;39:1117–1127. doi: 10.1017/S0033291708004698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Williams D. Neighbors HW. Social perspectives on mood disorders. In: Kupfer D, editor; Schatzberg AF, editor; Stein DJ, editor. Textbook of mood disorders. Arlington, VA: American Psychiatric Publishing Inc; 2006. pp. 145–158. [Google Scholar]
- 63.Alegria M. Chatterji P. Wells K, et al. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008;59:1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Felitti V. Anda RF. Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 65.Paulson J. Bazemore SD. Prenatal and postpartum depression in fathers and its association with maternal depression: A meta-analysis. JAMA Association. 2010;303:1961–1969. doi: 10.1001/jama.2010.605. [DOI] [PubMed] [Google Scholar]