Abstract
Purpose
High-risk prostate cancer patients undergoing treatment often experience biochemical recurrence. The use of bisphosphonates as an adjuvant treatment delays skeletal events, yet whether or not bisphosphonates also delay metastastic development remains to be determined.
Materials and Methods
A total of 140 high-risk prostate cancer patients who were undergoing definitive treatment and who had clinically organ-confined disease and who suffered from biochemical recurrence were administered intravenous (IV) clodronate. The patients were treated with a radical retropubic prostatectomy (RP) or curative radiotherapy (RTx). Upon androgen deprivation therapy initiation, tri-monthly IV clodronate was added to the treatment to prevent bone demineralization. Twenty-six out of 60 operated cases and 45 out of 80 irradiated cases received bisphosphonate. The length of time until the first bone metastasis was recorded and analyzed.
Results
No statistical difference was found for the type of primary treatment (RP or RTx) on the time to the first bone metastasis (95% confidence interval [CI], 0.40 to 2.43; p=0.98). However, there was a clear advantage favoring the group that received bisphosphonate (p<0.001). The addition of bisphosphonate delayed the appearance of the first bone metastasis by seven-fold (95% CI, 3.1 to 15.4; p<0.001).
Conclusion
Treatment with tri-monthly IV clodronate delayed the time to the first bone metastasis in high-risk prostate cancer patients who were experiencing an increase in the prostate specific antigen level after definitive treatment.
Keywords: Prostatic neoplasms, Clodronic acid, Osteoporosis, Androgen antagonists, Zoledronic acid, Hormone antagonists
Introduction
Biochemical (prostate specific antigen [PSA]-only) relapse is currently the most common form of advanced prostate cancer. Every third patient will experience rising PSA levels after prostatectomy [1] or radiotherapy [2]. Approximately 40% of the patients who receive definitive treatment for prostate cancer with an intention to cure show a recurrence, and of these cases more than 90% will progress to bone metastasis [2]. Hormonal therapy and chemotherapy are well-established treatment options that prolong survival in combination with radiotherapy or operation [3]. However, timing the initiation of these therapies is still a matter of debate and their roles as adjuvant therapies to prevent metastasis are not well defined.
Bisphosphonates were recently incorporated into the concept of multimodality therapy for the treatment of prostate cancer because they delay the time and frequency of fractures due to bone metastasis. Moreover, bisphosphonates may have a role in the prevention of bone metastasis due to their well-known in vitro effects on cancer cells [4,5]. We report here on the effects of intravenous (IV) bisphosphonate on the time to develop bone metastasis in a high-risk group of patients who were subjected to definitive therapy with the intention to cure.
Materials and Methods
A total of 140 patients with high-risk prostate cancer [6] and clinically organ-confined disease were enrolled in a prospective sequential open-label study. The patients were recruited from a larger pool where some of them were prospectively studied for their bone mineral density. High-risk patients were identified based on the following: a patient with a Gleason score of 8, 9 or 10, or a patient with a Gleason score of 7 (4+3 or 3+4) and an additional finding of minor components with a Gleason score of 5 on the sample biopsy (for those submitted to radiotherapy) or at a pathological exam [7]. This study was approved by the local ethics committee for research.
The selected patients with no prior neoadjuvant treatment were treated with either consensual radical retropubic prostatectomy (RP) or external beam radiotherapy (RTx) with the intention to cure.
Recurrence of the disease was defined as three consecutive increases in serum PSA levels.
After the verified recurrence of increased PSA levels, all the patients received androgen deprivation therapy (ADT) with an luteinizing-hormone-releasing hormone-analog to achieve a testosterone level <50 ng/mL, which was regularly checked.
Each branch of definitive therapy, either radiotherapy or surgical, was administered at the same time the ADT was started, with or without clodronate infusions.
Routine densitometry and bone scans were routinely done every 6 months regardless of the presence of pain. Site-specific exams were requested when pain appeared.
Metastatic confirmation was performed by two single-blinded radiologists using serial bone scintigraphy and image progression. When uncertainty persisted, regional magnetic resonance imagings and/or bone biopsies were done for confirmation.
The patients were analyzed according to the primary therapy that they received: radical RP or conformal RTx. External beam radiotherapy treatment was planned at a conformational station to deliver 6,800 cGy.
Inside each modality arm of primary treatment (we intended to treat 70 cases in each arm), all the patients were randomly assigned to receive adjuvant bisphosphonate infusions every three months after the detection of biochemical recurrence. Other patients did not receive infusions and they had no clinical variables conflicting with their treatment choice.
Twenty-six out of 60 operated patients received bisphosphonate, whereas 45 out of 80 irradiated patients received the same treatment regimen: 1,500 mg of clodronate every three months in two hour infusions. The median follow up in the RP group was 78 months (range, 50 to 124 months), whereas in the irradiated group, the patients were followed for a median time of 67 months (range, 50 to 119 months). The time to the first bone metastasis was recorded and statistically analyzed using the Kaplan-Meier curve and log-rank statistical tests to differentiate the time to the first bone metastasis for each group with each type of primary treatment and by differentiating those with or without bisphosphonates. Cox's regression analysis was used to determine whether or not the primary type of treatment and usage of bisphosphonate might delay the time until the first bone metastasis. p-values<5% were considered statistically significant.
Results
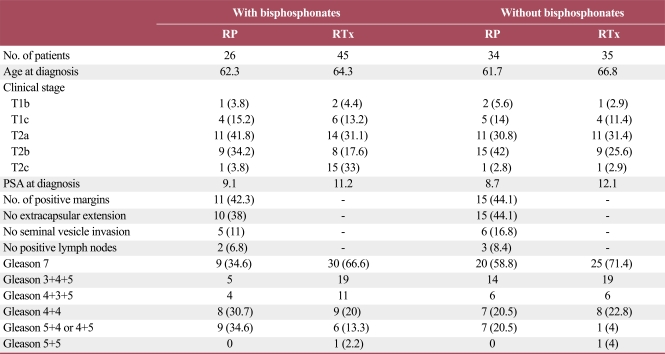
Although this study was not double-blinded, the four groups were well-balanced with regards to age, the clinical stage, positive margins, seminal vesicle invasion, lymph nodes involvement, and the histological pattern in each comparison depicted in Table 1.
Table 1.
Pretreatment variables and cancer characteristics of the treated groups of high-risk cancer patients
Values are presented as number (%). RP, radical retro-pubic prostatectomy; RTx, radiotherapy; PSA, prostate specific antigen; Gleason, score de Gleason.
Only one patient demonstrated chills on the third infusion, which was a minor adverse effect that did not require clodronate treatment to stop it.
One patient in the RP treatment group and three in the RTx treatment group with bisphosphonate infusions presented pain as the initial sign of bone metastasis before the regular exam identified the metastasis. Pain was the first manifestation of bone metastasis for patients who did not receive bisphosphonate.
For this specific subset of high-risk prostate cancer patients, there was no statistical difference concerning the type of primary treatment for prostate cancer and the time to the first bone metastasis (95% confidence interval [CI], 0.40 to 2.43; p=0.98).
The primary treatment modality (RP or RTx) did not significantly affect the time to the first bone metastasis. However, the addition of bisphosphonate significantly affected this measure. There was a clear advantage for the group that received bisphosphonate compared to those who did not receive it (p<0.001) regardless of the type of primary treatment (p<0.001).
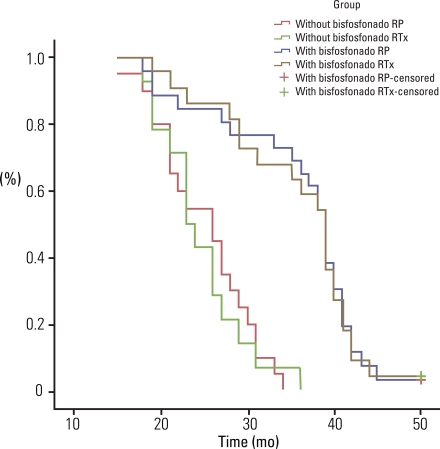
During long-term follow-up, the regular use of bisphosphonate delayed the appearance of the first bone metastasis seven-fold over the lag time for those patients who did not receive bisphosphonate, despite the type of the primary treatment (95% CI, 3.1 to 15.4; p<0.001), as depicted in Fig. 1.
Fig. 1.
Number of participants by health insurance type and age from the National Cancer Screening Program, 2008. RP, radical retro-pubic prostatectomy; RTx, radiotherapy.
Only one case progressed to death during the analyzed follow-up time.
Discussion
Prostate and breast cancer are well-known cancers that regularly metastasize to bone.
Skeletal complications of bone metastases increase the risk of death and undermine the patients' functional independence and quality of life [8]. Bisphosphonates have been used for more than fifteen years to improve the outcome of patients with bone metastasis from solid tumors.
Emerging evidence indicates that the potential benefits of bisphosphonate therapy extend beyond the treatment of metastatic bone lesions.
The benefits of bisphosphonates as an adjuvant therapy to treat the progression of prostate cancer showed clinical benefits such as the delay of the first skeletal event [9], pain control [10], and delay or reversal of bone demineralization due to the anti-hormonal agents that are regularly used for treating advanced stages of prostate cancer [11].
The use of bisphosphonates effectively inhibits osteoclast-mediated bone resorption, and so this provides the rationale for their use for skeletal protection in the endless bone remodeling process.
Preliminary preclinical studies with zoledronic acid and other bisphosphonates have demonstrated that they have in vitro anti-tumor properties, and their effects extend beyond the treatment of bone metastasis [12,13], and bisphosphonates even delay the development of metastasis. This previously unrecognized, but fortuitous anti-angiogenic [14], anti-adherence, and anti-invasion adjuvant effects on cancer cells [15] may be the key to preventing the formation of metastatic niches in the bone.
Animal studies have shown that bisphosphonates can reduce the rate of developing bone metastases (for example, in Walker 256 carcinoma), but there is little evidence of an effect at non-osseous sites. The hypothesis that the growth of sub-clinical osseous metastases is augmented by products of bone resorption ("the vicious cycle") and that it may be diminished by a local reduction of these substances with bisphosphonates, has led to clinical trials involving patients with no clinical evidence of bone metastases, yet definitive results have not yet been reported.
In breast cancer treatment, the use of oral clodronate was shown to delay the occurrence of bone metastases in patients subjected to radical mastectomy, except for those patients with cancer cells already in the bone marrow, which is a well-known high-risk factor for the development of distant metastases [16].
A significant number of patients with organ-confined prostate cancer have been identified to be at high-risk of treatment failure (exceeding 50%) at three years. This figure includes those who patients who presented with an initially increased PSA level greater than 20 µg/L, a Gleason score greater than 7, multiple positive biopsies and clinical extra-prostatic extension of the disease [6].
Our study included only cases of high-risk prostate cancer with the potential for quickly developing bone metastases due to the cancer's aggressive biological nature.
Most patients with elevated PSA levels are given anti-ADT. Anti-hormone therapy may delay progression, but it is not curative for those with rising PSA levels after definitive treatment [17]. There is no consensus on when to start or add bisphosphonates on these patients, but adding bisphosphonates for early therapy is an emerging trend. Previous reports have shown that zoledronic acid has the greatest effect in delaying skeletal-related events, and so this puts in perspective the early use of bisphosphonates to prevent demineralization and pain [18]. Our study concentrated on high-risk cases that began IV clodronate treatment trimonthly with the intent to reduce the secondary untoward effects of demineralization. After a minimum of 50 months of follow-up, a clear statistical difference could be observed in favor of the regular use of bisphosphonates, regardless of the type of therapy administered for localized prostate cancer (Fig. 1).
Some pharmaceutical companies recommend monthly or three-week scheduled infusions when pain is present and three-month or an annual dose when the protective effect on demineralization is the goal; however, there are an insufficient number of reports that have focused on the time of initiation and treatment duration as well as the ideal treatment schedule [19,20]. The tri-monthly schedule was empirically chosen for our patients due to the absence of pain and the high adherence rate. This high adherence rate was achieved because clodronate was administered intravenously, which narrowed the patient's choices or self-administration options observed for oral administration. Our intravenous treatment reinforced our previous experience that there is a high rate of patients abandoning treatment with the oral route of drug administration [21] due to the necessity of a regular intake of oral bisphosphonates, and the patients with oral administration showed poor adherence/persistence in taking the drugs for this slowly-progressing disease. Furthermore, prevention of bone metastasis with oral clodronate in an ongoing trial (MRC PR04) revealed no adjuvant benefit compared to a placebo [22], which encouraged us to study the IV route.
Our study supports the notion that bisphosphonates prevent bone metastasis, as has been previously demonstrated with breast cancer [23,24]. Thus, the early use of bisphosphonates for the prevention of bone metastasis is logical, yet clodronate is a bisphosphonate that does not contain nitrogen. Nitrogen-containing bisphosphonates target the mevalonate pathway, whereas clodronate promotes osteoclast apoptosis and ultimately impairment of bone resorption.
Our long-term follow-up may be considered rather short with regard to prostate cancer analysis, but we achieved statistically-significant results. Our findings demonstrate the strong impact of bisphosphonate therapy in a high-risk patient group for recurrence of treated prostate cancer, and the bisphosphonate therapy delayed the time to the first bone metastasis seven-fold as compared to those patients who did not receive bisphosphonates. This is the first report showing the adjuvant effect of bisphosphonates on the delay of bone metastasis.
Furthermore, an additional trial recently revealed an extended survival benefit for those patients with metastases at the beginning of the trial when using oral clodronate compared to those patients who did not use the drug [25]. However, in that trial, the patients were treated with radiotherapy or ADT and they had a less favorable clinical picture, whereas the patients in our study were homogeneous, and we concentrated on only organ-confined high-risk patients treated with an intention to cure.
The high heterogeneity of the prostate cancer spectrum is a limitation of enrollment for trials and it is also a confounding factor. Few of our cases had a bone biopsy that confirmed metastasis, and this might be criticized, but the sequential comparison of routine bone scans and scintigraphy played a crucial role in determining the metastatic nature of the bone scan lesions.
Our attempt to enroll only patients with high-risk cancers enhanced our analysis of the metastasis process.
Conclusion
The addition of trimestral IV bisphosphonate infusion to the regular therapy for preventing bone demineralization in high risk cancer patients demonstrated a protective effect of delaying the bone metastasis process by 7 times compared to that of the patients who did not receive it.
Footnotes
Conflict of interest relevant to this article was not reported.
References
- 1.Han M, Partin AW, Zahurak M, Piantadosi S, Epstein JI, Walsh PC. Biochemical (prostate specific antigen) recurrence probability following radical prostatectomy for clinically localized prostate cancer. J Urol. 2003;169:517–523. doi: 10.1097/01.ju.0000045749.90353.c7. [DOI] [PubMed] [Google Scholar]
- 2.Shipley WU, Thames HD, Sandler HM, Hanks GE, Zietman AL, Perez CA, et al. Radiation therapy for clinically localized prostate cancer: a multi-institutional pooled analysis. JAMA. 1999;281:1598–1604. doi: 10.1001/jama.281.17.1598. [DOI] [PubMed] [Google Scholar]
- 3.Shahinian VB, Kuo YF, Freeman JL, Orihuela E, Goodwin JS. Increasing use of gonadotropinreleasing hormone agonists for the treatment of localized prostate carcinoma. Cancer. 2005;103:1615–1624. doi: 10.1002/cncr.20955. [DOI] [PubMed] [Google Scholar]
- 4.Diel IJ, Solomayer EF, Bastert G. Bisphosphonates and the prevention of metastasis: first evidences from preclinical and clinical studies. Cancer. 2000;88(12 Suppl):3080–3088. doi: 10.1002/1097-0142(20000615)88:12+<3080::aid-cncr27>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 5.Diel IJ. Antitumour effects of bisphosphonates: first evidence and possible mechanisms. Drugs. 2000;59:391–399. doi: 10.2165/00003495-200059030-00001. [DOI] [PubMed] [Google Scholar]
- 6.D'Amico AV, Whittington R, Malkowicz SB, Schultz D, Blank K, Broderick GA, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA. 1998;280:969–974. doi: 10.1001/jama.280.11.969. [DOI] [PubMed] [Google Scholar]
- 7.Whittemore DE, Hick EJ, Carter MR, Moul JW, Miranda-Sousa AJ, Sexton WJ. Significance of tertiary Gleason pattern 5 in Gleason score 7 radical prostatectomy specimens. J Urol. 2008;179:516–522. doi: 10.1016/j.juro.2007.09.085. [DOI] [PubMed] [Google Scholar]
- 8.Saad F, Olsson C, Schulman CC. Skeletal morbidity in men with prostate cancer: quality-oflife considerations throughout the continuum of care. Eur Urol. 2004;46:731–739. doi: 10.1016/j.eururo.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 9.Saad F, Gleason DM, Murray R, Tchekmedyian S, Venner P, Lacombe L, et al. A randomized, placebo-controlled trial of zoledronic acid in patients with hormone-refractory metastatic prostate carcinoma. J Natl Cancer Inst. 2002;94:1458–1468. doi: 10.1093/jnci/94.19.1458. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues P, Hering F, Campagnari JC. Use of bisphosphonates can dramatically improve pain in advanced hormone-refractory prostate cancer patients. Prostate Cancer Prostatic Dis. 2004;7:350–354. doi: 10.1038/sj.pcan.4500752. [DOI] [PubMed] [Google Scholar]
- 11.Rodrigues P, Hering FO, Bruna P, Meller A, Afonso Y. Comparative study of the protective effect of different intravenous bisphosphonates on the decrease in bone mineral density in patients submitted to radical prostatectomy undergoing androgen deprivation therapy: a prospective open-label controlled study. Int J Urol. 2007;14:317–320. doi: 10.1111/j.1442-2042.2006.01721.x. [DOI] [PubMed] [Google Scholar]
- 12.Ullen A, Lennartsson L, Hjelm-Eriksson M, Kälkner KM, Lennernäs B, Nilsoon S. Additive/synergistic anti-tumoral effects on prostate cancer cells in vitro following treatment with a combination of gencitabine and zoledronic acid. Proc Am Soc Clin Oncol. 2003;22:1737. doi: 10.1080/02841860510029617. [DOI] [PubMed] [Google Scholar]
- 13.Daubiné F, Le Gall C, Gasser J, Green J, Clézardin P. Antitumor effects of clinical dosing regimens of bisphosphonates in experimental breast cancer bone metastasis. J Natl Cancer Inst. 2007;99:322–330. doi: 10.1093/jnci/djk054. [DOI] [PubMed] [Google Scholar]
- 14.Wood J, Bonjean K, Ruetz S, Bellahcène A, Devy L, Foidart JM, et al. Novel antiangiogenic effects of the bisphosphonate compound zoledronic acid. J Pharmacol Exp Ther. 2002;302:1055–1061. doi: 10.1124/jpet.102.035295. [DOI] [PubMed] [Google Scholar]
- 15.Boissier S, Magnetto S, Frappart L, Cuzin B, Ebetino FH, Delmas PD, et al. Bisphosphonates inhibit prostate and breast carcinoma cell adhesion to unmineralized and mineralized bone extracellular matrices. Cancer Res. 1997;57:3890–3894. [PubMed] [Google Scholar]
- 16.Diel IJ, Solomayer EF, Costa SD, Gollan C, Goerner R, Wallwiener D, et al. Reduction in new metastases in breast cancer with adjuvant clodronate treatment. N Engl J Med. 1998;339:357–363. doi: 10.1056/NEJM199808063390601. [DOI] [PubMed] [Google Scholar]
- 17.Brawer MK. Radiation therapy failure in prostate cancer patients: risk factors and methods of detection. Rev Urol. 2002;4(Suppl 2):S2–S11. [PMC free article] [PubMed] [Google Scholar]
- 18.Saad F. Bisphosphonates can prevent skeletal complications of malignant bone disease from prostate cancer and renal cell carcinoma. Eur Urol Suppl. 2007;6:683–688. [Google Scholar]
- 19.Smith MR, Eastham J, Gleason DM, Shasha D, Tchekmedyian S, Zinner N. Randomized controlled trial of zoledronic acid to prevent bone loss in men receiving androgen deprivation therapy for nonmetastatic prostate cancer. J Urol. 2003;169:2008–2012. doi: 10.1097/01.ju.0000063820.94994.95. [DOI] [PubMed] [Google Scholar]
- 20.Michaelson MD, Kaufman DS, Lee H, McGovern FJ, Kantoff PW, Fallon MA, et al. Randomized controlled trial of annual zoledronic acid to prevent gonadotropin-releasing hormone agonist-induced bone loss in men with prostate cancer. J Clin Oncol. 2007;25:1038–1042. doi: 10.1200/JCO.2006.07.3361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mangiapane S, Hoer A, Gothe H, Barghout V, Haeussler B. Higher persistency with I.V. bisphosphonates in patients with bone metastasis. J Clin Oncol. 2006;24(18S):18623. [Google Scholar]
- 22.Mason MD, Sydes MR, Glaholm J, Langley RE, Huddart RA, Sokal M, et al. Oral sodium clodronate for nonmetastatic prostate cancer: results of a randomized double-blind placebocontrolled trial: Medical Research Council PR04 (ISRCTN61384873) J Natl Cancer Inst. 2007;99:765–776. doi: 10.1093/jnci/djk178. [DOI] [PubMed] [Google Scholar]
- 23.Powles T, McCroskey E, Paterson A. Oral bisphosphonates as adjuvant therapy for operable breast cancer. Clin Cancer Res. 2006;12(20 Pt 2):6301s–6304s. doi: 10.1158/1078-0432.CCR-06-1211. [DOI] [PubMed] [Google Scholar]
- 24.Powles T, Paterson A, McCloskey E, Schein P, Scheffler B, Tidy A, et al. Reduction in bone relapse and improved survival with oral clodronate for adjuvant treatment of operable breast cancer [ISRCTN83688026] Breast Cancer Res. 2006;8:R13. doi: 10.1186/bcr1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dearnaley DP, Mason MD, Parmar MK, Sanders K, Sydes MR. Adjuvant therapy with oral sodium clodronate in locally advanced and metastatic prostate cancer: long-term overall survival results from the MRC PR04 and PR05 randomised controlled trials. Lancet Oncol. 2009;10:872–876. doi: 10.1016/S1470-2045(09)70201-3. [DOI] [PMC free article] [PubMed] [Google Scholar]