Abstract
Objective
To determine whether demographic or clinical characteristics of primary care patients are associated with depression treatment quality and outcomes within a collaborative care model.
Methods
Collaborative depression care, based on principles from the IMPACT trial, was implemented in six community health organizations serving disadvantaged patients. Over three years, 2821 patients were treated. Outcomes were receipt of quality treatment and depression improvement.
Results
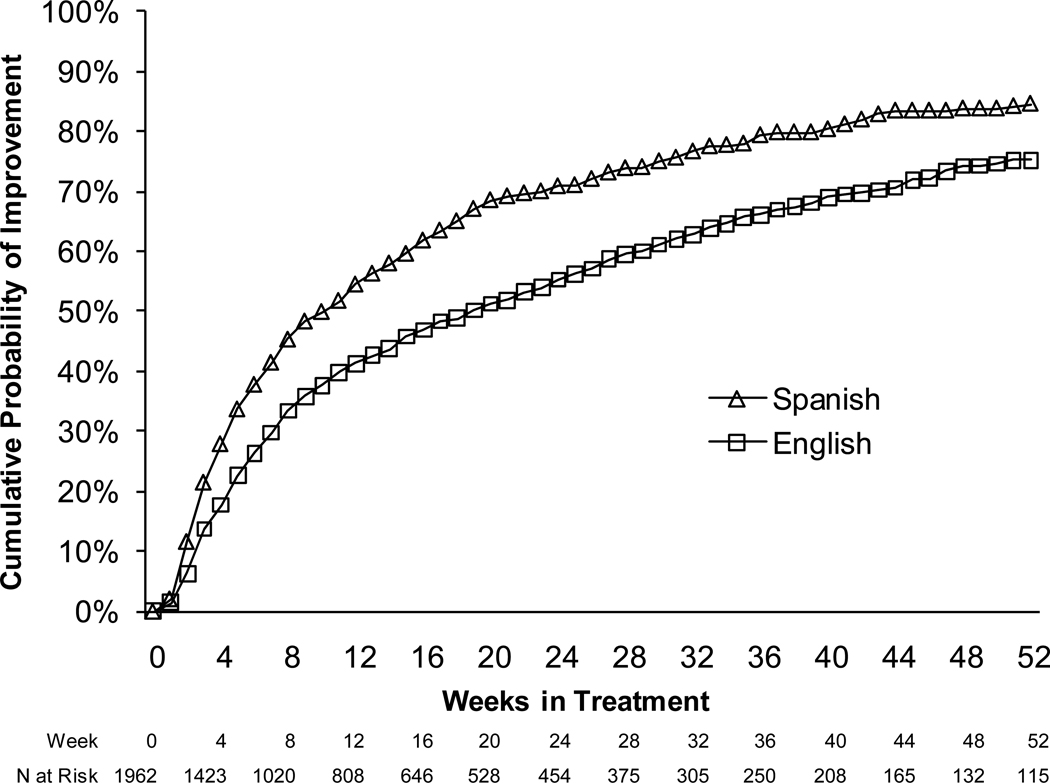
Logistic regression analyses revealed that patients who were older, more depressed, or more anxious were more likely to be retained in treatment and to receive appropriate pharmacotherapy. Whereas gender and depression severity were unrelated to depression outcomes, significantly more patients who preferred Spanish (59.1%) than English (48.5%, p<0.01) improved within 12 weeks in multivariate analyses. High baseline anxiety was associated with a lower probability of improvement and older age showed a similar trend. Survival analyses demonstrated that patients who preferred Spanish or were less anxious improved significantly more rapidly than their counterparts (ps<0.001).
Conclusions
Patients with more anxiety received higher quality care but experienced worse depression outcomes than less anxious patients. Spanish language preference was strongly associated with depression improvement. This collaborative care program attained admirable outcomes among disadvantaged Spanish-speaking patients without extensive cultural tailoring of care.
Keywords: Depression, anxiety, disease management, primary health care, healthcare disparities
Introduction
Both sociodemographic and clinical characteristics of patients influence depression treatment outcomes. One of the most interesting issues in depression treatment is whether members of ethnic minorities, particularly non-English speaking language minorities, benefit from treatment as much as white individuals with depression. A corollary is whether specially targeted services are needed to provide effective treatment for such patients. This paper explores these issues in the context of a demonstration program of collaborative care for individuals with depression in six community-based primary care organizations serving a high proportion of patients from ethnic minority groups.
In the STAR-D trial, conducted largely in specialty mental health settings, higher rates of remission from depression with citalopram treatment occurred among patients who were female, Caucasian, socially advantaged, and privately insured, as well as patients with less psychiatric comorbidity, lower anxiety, and lower depression severity at baseline.[1, 2] Although Spanish-speaking Latino patients experienced worse outcomes than English-speaking Latinos, differences based on language did not persist when other sociodemographic and clinical characteristics were controlled.[3]
In contrast, different patterns of association between patient-level characteristics and depression outcomes have emerged from collaborative care trials in primary care settings. For example, in the Partners in Care study, in usual care settings, men were less likely than women to receive depression treatment, yet a quality improvement intervention reduced this gender-based disparity in care and yielded similar overall outcomes.[4] In addition, African-American and Latino patients were more likely to benefit from the program than white patients.[5] Similarly, the IMPACT trial demonstrated that a collaborative care model improved engagement in depression treatment and outcomes among elderly ethnic minorities (predominantly African-American and Latino) compared to usual care, and that the program yielded benefits similar to those observed among elderly non-Latino white patients. [6] Whereas language proficiency and access to language services are known to be associated with the quality of general medical care,[7, 8] it is not known whether preferred language is associated with the quality of mental health care or depression outcomes in primary care settings.[9] Therefore, research is needed to examine how primary care quality improvement initiatives may impact mental health care for patients with limited English proficiency, a group that receives few specialty mental health services.[10–12]
In addition to determining the sociodemographic correlates of depression treatment and outcomes, it is important to determine how patients’ clinical characteristics are associated with the process of care and outcomes when quality improvement initiatives are initiated in community practice settings. Although there is little evidence that antidepressant medications are more beneficial than placebo in patients with subthreshhold depression,[13] the Partners in Care study found that a quality improvement initiative was beneficial to such patients and was cost-effective.[14, 15] In the IMPACT collaborative care trial, elderly patients with greater depression severity at baseline received a greater intensity of depression treatment yet had worse outcomes.[16] The relationship between depression severity and outcomes within quality improvement initiatives is not well understood and further examination among heterogeneous and complex patients is needed.
Although a strong evidence base supports the value of collaborative care models for enhancing the delivery of mental health services in primary care settings under experimental conditions, less is known about the effects such models have when implemented in real-world clinical practice settings. The heterogeneity of patients and practices is far greater than can be studied in controlled research settings and it is not known whether certain types of patients may be more likely to benefit from such programs than others. For example, some studies have been restricted to patients meeting research diagnostic criteria for major depressive disorder,[17, 18] which is not a practical or relevant means of identifying patients in real-world clinical settings. Therefore, it is important to understand how these programs function when patient selection occurs based on primary care physicians’ diagnosis and referral or based on use of a brief screening instrument. To target resources efficiently, it will be important to gain understanding of whether patient characteristics are associated with outcomes.
To address this gap in knowledge and gain understanding of the real-world effects of implementing collaborative care models in community-based settings, the Hogg Foundation for Mental Health sponsored a demonstration project at community-based primary care clinics in six communities through the Integrated Health Care Initiative. Many of the patients in the demonstration program were African-American or Latino – and many expressed a language preference for Spanish. Here, we examine associations between demographic and clinical characteristics of patients, metrics of high-quality depression care, and depression outcomes within a collaborative care framework implemented in real-world settings.
Methods
Sites
Six community health organizations in Texas, described in detail elsewhere, participated in this project.[19] One organization had two participating clinics. Three of the organizations are located in large urban areas while three are in small urban and rural areas along the US-Mexico border. The organizations treat disadvantaged patients who are predominantly uninsured. Latino patients make up a substantial proportion of the population served at all clinics except one. Because the program was implemented as a quality improvement initiative and did not require collection of data apart from clinical care, patients signed informed consent forms to receive clinical services. The program was implemented as part of larger research studies at two organizations and patients at those sites consented to participate in the research. The institutional review board at Harvard Medical School reviewed and approved the program evaluation.
Participants
Patients identified by their primary care provider teams as having symptoms of depression were referred to the program. Patients for whom the program was clinically inappropriate, for example, patients with schizophrenia or bipolar disorder, were not included. A total of 2821 patients aged 18 and above were enrolled and treated between 2006 and 2009.
Intervention
The quality improvement program, described elsewhere in greater detail, was based on a collaborative care model and implemented key features including the use of a web-based depression registry by care managers with organized psychiatric consultation.[19] Care managers based in each primary care clinic performed an initial assessment of patients to collect demographic and clinical information at baseline. The care managers subsequently followed up with patients in clinic and over the telephone to track patients’ progress. The timing and number of follow-ups was at the discretion of the care manager. The care managers coordinated medication management with primary care providers and arranged referrals for psychotherapy, either on-site or in the community, where indicated. Care managers who were licensed could also provide brief psychotherapy (primarily cognitive-behavioral therapy). Most sites had at least one bilingual care manager who provided services in Spanish. Patients were tracked using a web-based depression registry.[20] At each clinic, a designated psychiatrist provided supervision to the care managers either in-person or via telephone and consulted on select patients who were not improving. Primary care providers and care managers received trainings on evidence-based depression management. A Technical Assistance Team from the University of Washington provided training for care managers and primary care providers, access to the depression registry, and logistical support for implementing the collaborative care program through annual in-person training and monthly conference calls.
Data Collection
Data was obtained from a web-based patient registry database used by care managers to track patients. All data was collected in the routine course of delivering clinical care. Clinics did not collect additional data for the evaluation. Analyses used data on patient demographics (age, gender, preferred language, insurance status), service dates, and when applicable, the type and dose of antidepressant medication prescribed.
Measures
Two indicators were constructed to assess the receipt of high quality care. The first few weeks of treatment are a critical time in depression treatment and a time when many patients discontinue care. Because collaborative care programs aim to enhance treatment engagement and retention, receipt of a follow-up care manager contact within the first 3 weeks of treatment was identified as an indicator of quality care. Second, patients were considered to have received appropriate pharmacotherapy if the treatment plan at the follow-up visit preceding measurement of outcomes included an antidepressant medication at a therapeutic dose based on published guidelines.[21–23]
Depression severity was assessed with the Patient Health Questionnaire – 9 (PHQ-9). The PHQ-9 is a widely used measure of depression severity and response to treatment designed for use in primary care settings and has been validated in Spanish.[24–28] The nine items reflect the core symptoms of DSM-IV Major Depressive Disorder and are scored on a scale ranging from zero (“not at all”) to three (“nearly every day”), for a total score of zero to 27. A score of 10 is the most commonly used cutoff for identifying the presence of a probable depressive disorder.[24] However, scores in the range of 10 to 14 may represent a “gray zone”.[24] Based on PHQ-9 scores at baseline, patients were classified as having symptoms that were mild (0–9), moderate (10–14), or severe (15–27). Anxiety was assessed using the Overall Anxiety Severity and Impairment Scale (OASIS). The OASIS is a 5-item self-report measure of anxiety symptoms that has been validated in primary care patients and used to monitor anxiety treatment.[29, 30] A higher score on the OASIS reflects more severe anxiety symptoms. The OASIS and PHQ-9 scores were recorded in the patient registry, when administered, at each follow-up, whether in person or via telephone.
Acute-phase depression outcomes were obtained from follow-ups that occurred at least 6 weeks but no more than 12 weeks following the initial assessment. Because the benefits of both antidepressant medications and psychotherapy necessitate at least 4 to 8 weeks of treatment,[21–23] patients who were followed for less than 6 weeks were not in treatment for a sufficient duration and were considered drop-outs for acute phase analyses. Patients who achieved a 50% reduction in PHQ-9 score between baseline and follow-up or had a follow-up PHQ-9 score less than or equal to 5 were considered to have improved.
Data Analysis
Models were constructed to estimate the effects of patient characteristics on the probability of receipt of each quality indicator; on acute-phase depression outcomes (coded as improved, not improved, or dropped out); and on time to improvement from depression. Independent variables were patient age, gender, preferred language, baseline OASIS score, baseline PHQ group and clinic. Logistic regression models were constructed to estimate the impact of patient characteristics on the receipt of the two quality indicators; and a multinomial regression model estimated acute phase outcomes (improved, not improved, or dropped out). We generated adjusted probabilities for receipt of each quality indicator and for acute phase improvement. We used a conservative modeling strategy to account for the clustering of patients within clinics by treating clinic as a fixed effect. In supplementary analyses, we conducted additional models which treated clinic effects as random. Cox proportional hazards models were used to estimate the time to improvement. Survival curves were constructed separately among patients who preferred English versus Spanish to display the time to improvement for each group.
Results
Patients with initial PHQ-9 scores of 5 or lower met criteria for remission at baseline and therefore were excluded from analyses, yielding a final sample of 2550 patients. The OASIS was incomplete or not administered 489 patients. Thus, the valid sample for the regression models was 2010 due to missing data for the OASIS or another predictor variable.
Patient Demographic and Clinical Characteristics
The baseline demographic and clinical characteristics of patients are displayed in Table 1. Patients were predominantly female (83.0%), ranging in age from 18 to 88 years. Nearly half of patients (47.0%) reported Spanish as their preferred language. Overall, patients endorsed high levels of depression (PHQ-9 mean = 16.3, SD = 5.4) and anxiety (OASIS mean = 11.0, SD = 4.8), with 61.6% categorized as severely depressed based on PHQ-9 scores at baseline. Few patients had previously been treated for depression with either medications (28.9%) or psychotherapy (11.5%). Relative to patients who preferred English, those who preferred Spanish were older, more likely to be female, had less severe depression and anxiety symptoms, and were more likely to be treatment-naïve (Table 1).
Table 1.
Baseline Demographic and Clinical Characteristics of Patients
| Characteristics | All Patients (n = 2550) |
English (n = 1324) |
Spanish (n = 1175) |
P value a |
|---|---|---|---|---|
| Demographics | ||||
| Age | ||||
| Mean (SD) | 45.2 (13.2) | 44.3 (13.5) | 46.2 (12.9) | 0.0003 |
| Range | 18–88 | 18–88 | 18–87 | |
| Sex: Female, N (%) | 2101 (83.0) | 1039 (79.3) | 1017 (86.9) | < 0.0001 |
| Preferred Language: Spanish, N (%) | 1175 (47.0) | |||
| Severity | ||||
| OASIS Score, mean (SD) | 11.0 (4.8) | 11.5 (4.8) | 10.2 (4.7) | < 0.0001 |
| PHQ-9 Score, mean (SD) | 16.3 (5.4) | 16.9 (5.3) | 15.6 (5.3) | 0.0002 |
| PHQ-9 Severity | < 0.0001 | |||
| Mild: PHQ-9 5–9, N (%) | 319 (12.5) | 137 (10.4) | 178 (15.2) | |
| Moderate: PHQ-9 10–14, N (%) | 659 (25.8) | 306 (23.1) | 344 (29.3) | |
| Severe: PHQ-9 15–27, N (%) | 1572 (61.6) | 881 (66.5) | 653 (55.6) | |
| Treatment History | ||||
| Previous Antidepressant Treatment | 738 (28.9) | 483 (36.5) | 243 (20.7) | < 0.0001 |
| Previous Psychotherapy | 292 (11.5) | 220 (16.6) | 70 (6.0) | < 0.0001 |
Note: Due to missing data, N for some variables is lower than 2550
P-values are reported for t-tests and chi-square tests for comparisons between English and Spanish groups.
Quality of Care
Demographic variables were not significantly associated with receipt of early follow-up. The probability of receiving appropriate pharmacotherapy was significantly higher among older patients (Tables 2 and 3). Specifically, for each decade of age, the odds of receiving appropriate pharmacotherapy increased by 9.6%. In contrast, gender and language preference were not associated with receipt of appropriate pharmacotherapy. Anxious patients were significantly more likely to receive both quality metrics than their less-anxious counterparts. For each 5-point increase in baseline OASIS score, the odds of having a follow-up within 3 weeks increased by 18.4% and the odds of receiving appropriate pharmacotherapy increased by 38.3%. Although mildly and severely depressed patients were equally likely to receive early follow-up, among those with severe depression, the probability of receiving appropriate pharmacotherapy was 11.1% higher than among those with mild depression. These results remained unchanged in sensitivity models that included prior treatment with antidepressant medications and psychotherapy and in mixed effects models treating clinic effects as random. Prior treatment was not associated with early follow-up, but prior antidepressant treatment was positively associated with receipt of appropriate pharmacotherapy (OR 1.67, p < 0.001; data not shown in Table).
Table 2.
Predicted Probability of Acute Phase Depression Treatment and Outcomes by Patient Characteristics (N = 2010)
| Depression Treatment Quality Indicators |
Acute Phase Outcomes | |||
|---|---|---|---|---|
| Characteristics | Received Follow-Up Within 21 Days |
Received Appropriate Pharmacotherapy |
12-Week Outcome Measured |
Depression Improved † |
| Age = 20 | 57.0% | 45.4% | 34.6% | 59.7% |
| Age = 40 | 55.2% | 49.9% | 39.5% | 54.4% |
| Age = 60 | 53.4% | 54.5% | 44.8% | 49.0% |
| Age = 80 | 51.6% | 59.0% | 50.6% | 43.6% |
| Gender = Male | 51.8% | 49.0% | 37.4% | 55.7% |
| Gender = Female | 55.4% | 51.4% | 41.5% | 52.5% |
| Preferred Language = English | 54.7% | 53.2% | 41.1% | 48.5% |
| Preferred Language = Spanish | 54.8% | 48.1% | 40.6% | 59.1% |
| Baseline OASIS Score | ||||
| Low (Mean − SD) | 50.7% | 43.3% | 39.1% | 61.1% |
| Average (Mean) | 54.8% | 51.0% | 40.7% | 53.1% |
| High (Mean + SD) | 58.8% | 58.7% | 43.0% | 45.0% |
| Baseline PHQ-9 Group | ||||
| Mild (5–9) | 51.0% | 42.0% | 33.4% | 59.9% |
| Moderate (10–14) | 54.4% | 49.7% | 39.1% | 48.3% |
| Severe (15–27) | 55.6% | 53.1% | 42.8% | 53.8% |
Predicted probabilities are adjusted for all remaining variables in the table (age, gender, preferred language, baseline OASIS score and baseline PHQ group)
Percentage of patients with 12-Week Measurement (N = 1063)
Table 3.
Demographic and Clinical Correlates of Acute Phase Depression Treatment and Outcomes (n = 2010)
| Model 1. | Model 2. | Model 3. Multinomial Model | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Follow-Up Within 21 Days |
Appropriate Pharmacotherapy |
Acute Phase Outcome: Drop-Out (reference: Not Improved) |
Acute Phase Outcome: Improved (reference: Not Improved) |
|||||||||
| Variable | Coef | OR | p | Coef | OR | p | Coef | OR | p | Coef | OR | p |
| Age | 0.00 | 1.00 | 0.35 | 0.01 | 1.01 | 0.02 | −0.02 | 0.98 | 0.001 | −0.01 | 0.99 | 0.06 |
| Gender | ||||||||||||
| Female – reference | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Male | −0.14 | 0.87 | 0.25 | −0.10 | 0.91 | 0.43 | 0.24 | 1.27 | 0.13 | 0.13 | 1.14 | 0.49 |
| Preferred Language | ||||||||||||
| Spanish - reference | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| English | 0.00 | 1.00 | 0.99 | 0.20 | 1.22 | 0.07 | −0.25 | 0.78 | 0.08 | −0.43 | 0.65 | 0.008 |
| Baseline OASIS score | 0.03 | 1.03 | 0.004 | 0.06 | 1.07 | <0.001 | −0.05 | 0.95 | <0.001 | −0.07 | 0.93 | <0.001 |
| Baseline PHQ group | ||||||||||||
| Mild (5–9) - reference | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Moderate (10–14) | 0.14 | 1.15 | 0.44 | 0.31 | 1.36 | 0.07 | −0.50 | 0.61 | 0.06 | −0.47 | 0.63 | 0.12 |
| Severe (15–27) | 0.18 | 1.20 | 0.29 | 0.45 | 1.56 | 0.008 | −0.54 | 0.58 | 0.03 | −0.25 | 0.78 | 0.39 |
| Clinic Site | ||||||||||||
| Clinic 1 – reference | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Clinic 2 | −0.40 | 0.67 | 0.02 | 0.11 | 1.12 | 0.49 | 0.33 | 1.39 | 0.11 | −0.14 | 0.87 | 0.63 |
| Clinic 3 | 2.26 | 9.62 | <0.001 | 0.76 | 2.15 | <0.001 | −0.98 | 0.38 | <0.001 | 1.16 | 3.17 | <0.001 |
| Clinic 4 | 0.61 | 1.84 | <0.001 | −0.80 | 0.45 | <0.001 | −0.11 | 0.90 | 0.59 | 0.45 | 1.58 | 0.08 |
| Clinic 5 | 1.15 | 3.17 | <0.001 | 0.74 | 2.09 | <0.001 | 0.63 | 1.87 | 0.04 | 2.09 | 8.06 | <0.001 |
| Clinic 6 | −0.10 | 0.91 | 0.53 | −0.13 | 0.88 | 0.40 | −0.42 | 0.66 | 0.04 | 0.77 | 2.16 | 0.002 |
| Clinic 7 | 0.09 | 1.09 | 0.74 | −1.03 | 0.36 | 0.001 | 0.41 | 1.51 | 0.27 | 0.05 | 1.05 | 0.93 |
| constant | −0.59 | −1.56 | 3.10 | - | <0.001 | 1.29 | - | 0.003 | ||||
Acute Phase Outcomes
Table 3 summarizes a multinomial logistic regression model examining correlates of three acute phase outcomes: dropping out of care, having improvement in depression, or having no improvement in depression (the reference group). This method estimates the probability of improvement while simultaneously taking into account the fact that many people drop out of care. The probability of dropping out of care before 6 weeks was lower among individuals who were older and those who were more anxious at baseline. Specifically, for each decade of age, the odds of dropping out decreased by 15.3%. The odds of dropping out of treatment decreased by 23.3% for each 5-point increase on baseline OASIS score. Relative to mildly depressed patients, 9.3% fewer severely depressed patients dropped out. The probability of dropping out was no higher among men than women or patients preferring English versus Spanish.
Older patients tended to have a somewhat lower probability of improvement during the acute phase, but gender was not associated with the probability of improvement. In contrast, preferred language was significantly and strongly associated with improvement. Relative to patients who preferred English, the odds of improvement were 54% higher among patients who preferred Spanish (p < 0.01). Whereas slightly less than half of patients preferring English (48.5%) improved, 59.1% of patients who preferred Spanish improved (OR = 0.65, p < 0.01; Tables 2 and 3) after adjusting for age, gender, clinic, and baseline severity. Higher anxiety at baseline significantly lowered the odds of improvement, such that for each 5-point increase in baseline OASIS score, the odds were 28.8% lower. Patients with baseline PHQ-9 scores in the severe range experienced similar rates of improvement as patients with scores in the mild and moderate ranges. Results were unchanged in sensitivity analyses with multinomial models controlling for the number of days until outcome measurement. In sensitivity analyses controlling for prior treatment history (data not shown in Table), the probability of dropping out was significantly lower among patients in both the moderate and severe PHQ-9 groups, but results were otherwise unchanged. Prior antidepressant treatment was significantly and negatively associated with dropping out of treatment, but was unrelated to improvement. In a multinomial model that accounted for the clustering of patients within clinics by treating clinic effects as random, minor changes affected the statistical significance for two variables. The effect of age on attrition was no longer significant (OR = 0.99, p = 0.063) but older patients were less likely to improve (OR = 0.99, p = 0.043). Attrition was also less common among moderately depressed patients than mildly depressed patients (OR = 0.57, p = 0.015). Together, these sensitivity analyses demonstrated no clinically substantive changes in the overall patterns.
Time to Improvement
A Cox proportional hazards model revealed that patients who preferred Spanish (p < 0.01) and patients with less anxiety (p < 0.01) improved more rapidly than counterparts in multivariate analyses that included age, gender, clinic, and baseline PHQ-9 score. A survival curve was constructed to estimate time to improvement from depression. Figure 1 illustrates that patients who preferred Spanish improved more rapidly than patients who preferred English, a discrepancy that appeared early during the course of treatment. At 10 weeks of treatment, half of patients who preferred Spanish were estimated to have improved, whereas it took 19 weeks for the same proportion of patients who preferred English to improve.
Figure 1.
Time to Improvement of Depression among Patients who Prefer English and Spanish
Discussion
Among a heterogeneous group of primary care patients identified as having depression and treated within a collaborative care framework, several patient-level characteristics were associated with treatment quality and depression outcomes. We found that higher anxiety and, to a lesser extent, older age were associated with lower likelihood of experiencing depression improvement, despite such patients receiving more intensive treatment. These results are consistent with prior research in suggesting that patients who are older or more anxious have conditions that are less responsive to treatment. Specifically, compared to younger patients, older patients were more likely to receive appropriate pharmacotherapy and were less likely to drop out of care, suggesting that the collaborative care model was particularly effective in engaging older patients in treatment. Nevertheless, older patients tended to experience less improvement in depression during the acute phase. The worse depression outcomes among older adults are consistent with past research demonstrating low rates of depression treatment response among elderly individuals.[18, 31] This may be explained by the higher complexity of comorbid medical problems or other aging-related life stressors (not measured in this program) that complicate depression treatment among elderly patients.
Likewise, anxious patients were more likely than less anxious patients to receive appropriate pharmacotherapy and were more likely to have early follow-up, yet they were less likely to experience improvement. Despite utilizing different measures of anxiety and depression symptoms, this latter finding is consistent with results from the STAR-D trial that demonstrated poorer response to citalopram or to subsequent antidepressant switch or augmentation among depressed patients with comorbid anxiety symptoms.[2] From a clinical perspective, the presence of anxiety appears to be a negative prognostic feature among depressed patients and may suggest that highly anxious patients comprise a subgroup requiring more aggressive management. That anxious patients in this program were more likely to receive quality treatment and less likely to drop out of care suggests that the collaborative care framework may be helpful in retaining anxious patients in treatment, although this alone may be insufficient to improve their outcomes.
Compared to mildly depressed patients, those with severe depression were more likely to receive appropriate pharmacotherapy, less likely to drop out of care, and experienced similar acute phase outcomes. A similar trend was evident among patients with moderate symptoms. Together this suggests that the collaborative care model did retain and treat patients with severe depressive symptoms.
There were no significant differences in receipt of quality care based on gender or language preference, however, we note that patients preferring Spanish were marginally less likely to receive medications than counterparts. We were unable to assess whether this small difference reflects a true disparity or an appropriate tailoring of treatments to patient preferences. Overall, our results suggest that the model was successful in providing equitable care, itself an important marker of high-quality healthcare.[32]
Although outcomes were similar for men and women, only 17% of the patients treated were men, a discrepancy greater than that observed in the Partners in Care study (30% men)[4] or among non-VA clinics in the IMPACT trial (referral sample 24% men; screened sample 32% men).[33] With our data, we are not able to examine reasons underlying this treatment gap. However, our findings are consistent with the notion that cultural barriers to care are particularly notable among Spanish-speaking men. Extra effort may be needed to identify and engage men in treatment, yet they receive similar benefits as women do once they enter treatment.
In contrast to the equity in quality indicators, depression outcomes were markedly superior among patients who preferred Spanish compared to those who preferred English. The differences were robust across the acute phase and first year of treatment, appeared early in the course of treatment, were substantial in magnitude, and persisted after controlling for age, gender, primary care site, and severity of psychopathology. Consistent with a ‘healthy immigrant’ phenomenon whereby certain Latino immigrants have fewer psychiatric disorders, [34] patients who preferred Spanish, who may be recent immigrants from Mexico, had less severe symptomatology and were less likely to have received prior treatment than patients who preferred English, yet these baseline differences did not attenuate the differences in outcomes between these groups. Detailed information on age of onset and other indicators of depression chronicity were not available for analysis.
Our results should be considered within the context of several limitations. All of the data analyzed was collected during the routine clinical care of patients. Consequently, data were unavailable for some variables that may have been associated with depression treatment and outcomes, such as education, income, race/ethnicity, nativity, or concurrent medical illnesses. Although individual data on income was unavailable, the participating clinics treat socioeconomically disadvantaged patients, over 90% of whom were uninsured or on public funding sources. Likewise, although individual data on race/ethnicity was not available, Latino patients comprised a substantial proportion of the patient population at all but one clinic, as reported in more detail elsewhere. [19] Therefore, our results were obtained among an impoverished group of patients, most of whom were Latino.
Pharmacotherapy data was insufficient to determine the duration of antidepressant treatment, and therefore we were unable to construct a more rigorous measure of guideline-based pharmacotherapy. Based on site visits and the extensive contact with the clinics, it is the impression of the investigator team that the quality indicators we measured tap into broader constructs of quality of services and therefore, would have been correlated with other quality indicators that we were unable to measure as part of this evaluation. Finally, each organization developed mechanisms to identify their target patients. Because primary care team referral was involved, referral bias may have been present leading to the inclusion of more patients with classic presentations of depression, or patients who appeared more severely depressed. Alternately, patients who appeared less anxious may have been less likely to receive the OASIS and therefore excluded from the analyses.
Although some have suggested that culturally-tailored treatment delivery may be more effective than standard quality improvement initiatives,[35] we found superior outcomes among patients who preferred to speak Spanish within a general quality-improvement framework without specific cultural-tailoring. Given evidence suggesting that mental health disparities are related to receipt of lower quality care among ethnic minorities in usual care settings,[36] the importance of these findings is underscored. Organizations were provided with the same materials, training, guidance, and support and utilized the same web-based registry. However, services were provided in English and Spanish, suggesting that provision of language-concordant care may be critical to overcoming disparities in mental health care among Spanish-speaking Latino primary care patients. Similarly, although care managers were not provided with materials or instructions to tailor treatments for Latino patients as a group, the tailoring of treatment to an individual is a hallmark of collaborative care and it is likely that this general principle contributed to the effectiveness of this program among these patients. The results of this program evaluation are consistent with prior studies on quality improvement for depression in primary care that have reported equivalent or better outcomes among ethnic minorities. Moreover, these results extend the evidence for the effectiveness of collaborative care among minorities with limited English proficiency in real-world community health organizations.
Acknowledgements
We gratefully acknowledge financial support from the Hogg Foundation for Mental Health through its Integrated Health Care Initiative and training grant T32-MH019733 (PI: Richard Frank) from the National Institute of Mental Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 2.Fava M, Rush AJ, Alpert JE, et al. Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry. 2008;165:342–351. doi: 10.1176/appi.ajp.2007.06111868. [DOI] [PubMed] [Google Scholar]
- 3.Lesser I, Rosales A, Zisook S, et al. Depression outcomes of Spanish- and English-speaking Hispanic outpatients in STAR*D. Psychiatr Serv. 2008;59:1273–1284. doi: 10.1176/ps.2008.59.11.1273. [DOI] [PubMed] [Google Scholar]
- 4.Sherbourne CD, Weiss R, Duan N, Bird CE, Wells KB. Do the effects of quality improvement for depression care differ for men and women? Results of a group-level randomized controlled trial. Med Care. 2004;42:1186–1193. doi: 10.1097/00005650-200412000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Miranda J, Duan N, Sherbourne C, et al. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health Serv Res. 2003;38:613–630. doi: 10.1111/1475-6773.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Areán PA, Ayalon L, Hunkeler E, et al. Improving depression care for older, minority patients in primary care. Med Care. 2005;43:381–390. doi: 10.1097/01.mlr.0000156852.09920.b1. [DOI] [PubMed] [Google Scholar]
- 7.Flores G. The impact of medical interpreter services on the quality of health care: A systematic review. Med Care Res Rev. 2005;62:255–299. doi: 10.1177/1077558705275416. [DOI] [PubMed] [Google Scholar]
- 8.Karliner L, Jacobs E, Chen A, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42:727–754. doi: 10.1111/j.1475-6773.2006.00629.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bauer A, Alegría M. The impact of patient language proficiency and interpreter service use on the quality of psychiatric care: A systematic review. Psychiatr Serv. 2010;61:765–773. doi: 10.1176/appi.ps.61.8.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alegria M, Mulvaney-Day N, Woo M, et al. Correlates of past-year mental health service use among Latinos: Results from the National Latino and Asian American Study. Am J Public Health. 2006;97:76–83. doi: 10.2105/AJPH.2006.087197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sentell T, Shumway M, Snowden L. Access to mental health treatment by English language proficiency and race/ethnicity. J Gen Intern Med. 2007;22:289–293. doi: 10.1007/s11606-007-0345-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bauer A, Chen CN, Alegría M. English language proficiency and mental health service use among Latino and Asian Americans with mental disorders. Med Care. 2010;48:1097–1104. doi: 10.1097/MLR.0b013e3181f80749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. JAMA. 2010;303:47–53. doi: 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wells K, Sherbourne C, Duan N, et al. Quality improvement for depression in primary care: Do patients with subthreshold depression benefit in the long run? Am J Psychiatry. 2005;162:1149–1157. doi: 10.1176/appi.ajp.162.6.1149. [DOI] [PubMed] [Google Scholar]
- 15.Wells KB, Schoenbaum M, Duan N, et al. Cost-effectiveness of quality improvement programs for patients with subthreshold depression or depressive disorder. Psychiatr Serv. 2007;58:1269–1278. doi: 10.1176/ps.2007.58.10.1269. [DOI] [PubMed] [Google Scholar]
- 16.Katon W, Unützer J, Russo J. Major depression: The importance of clinical characteristics and treatment response to prognosis. Depress Anxiety. 2010;27:19–26. doi: 10.1002/da.20613. [DOI] [PubMed] [Google Scholar]
- 17.Katon W, Von Korff M, Lin E, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: A randomized trial. Arch Gen Psychiatry. 1999;56:1109–1115. doi: 10.1001/archpsyc.56.12.1109. [DOI] [PubMed] [Google Scholar]
- 18.Unützer J, Katon W, Callahan C, et al. Collaborative Care Management of Late-Life Depression in the Primary Care Setting: A Randomized Controlled Trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 19.Bauer A, Azzone V, Goldman HH, et al. Implementation of Collaborative Depression Management at Community-Based Primary Care Clinics: An Evaluation. Psychiatr Serv. doi: 10.1176/appi.ps.62.9.1047. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Unützer J, Choi Y, Cook IA, Oishi S. A web-based data management system to improve care for depression in a multicenter clinical trial. Psychiatr Serv. 2002;53:671–673. doi: 10.1176/ps.53.6.671. 678. [DOI] [PubMed] [Google Scholar]
- 21.American Psychiatric Association. Practice Guideline for the Treatment of Patients with Major Depressive Disorder. 2nd Edition. Washington DC: American Psychiatric Association; 2000. [PubMed] [Google Scholar]
- 22.Suehs B, Argo TR, Bendele SD, et al. Texas Medication Algorithm Project Procedural Manual. Major Depressive Disorder Algorithms. Texas Department of State Health Services; 2008. [Google Scholar]
- 23. [Accessed 5/10/2010];MacArthur Initiative on Depression and Primary Care: Depression Management Tool Kit. 2009 Available at http://www.depression-primarycare.org/images/pdf/macarthur_toolkit.pdf.
- 24.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Löwe B, Unützer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Med Care. 2004;42:1194–1201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Gilbody S, Richards D, Brealey S, Hewitt C. Screening for Depression in Medical Settings with the Patient Health Questionnaire (PHQ): A Diagnostic Meta-Analysis. J Gen Intern Med. 2007;22:1596–1602. doi: 10.1007/s11606-007-0333-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer RL. Validation and utility of the Patient Health Questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med. 2001;63:679–686. doi: 10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- 28.Wulsin L, Somoza E, Heck J. The feasibility of using the Spanish PHQ-9 to screen for depression in primary care in Honduras. Prim Care Companion J Clin Psychiatry. 2002;4:191–195. doi: 10.4088/pcc.v04n0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Campbellsills L, Norman S, Craske M, et al. Validation of a brief measure of anxiety-related severity and impairment: The Overall Anxiety Severity and Impairment Scale (OASIS) J Affect Disord. 2009;112:92–101. doi: 10.1016/j.jad.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roy-Byrne P, Craske MG, Sullivan G, et al. Delivery of evidence-based treatment for multiple anxiety disorders in primary care: a randomized controlled trial. JAMA. 2010;303:1921–1928. doi: 10.1001/jama.2010.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alexopoulos GS, Katz IR, Bruce ML, et al. Remission in depressed geriatric primary care patients: a report from the PROSPECT study. Am J Psychiatry. 2005;162:718–724. doi: 10.1176/appi.ajp.162.4.718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Institute of Medicine (U.S.) Committee on Crossing the Quality Chasm: Adaptation to Mental Health and Addictive Disorders. Improving the quality of health care for mental and substance-use conditions. Washington, DC: National Academies Press; 2006. [PubMed] [Google Scholar]
- 33.Hinton L, Zweifach M, Oishi S, Tang L, Unützer J. Gender disparities in the treatment of late-life depression: qualitative and quantitative findings from the IMPACT trial. Am J Geriatr Psychiatry. 2006;14:884–992. doi: 10.1097/01.JGP.0000219282.32915.a4. [DOI] [PubMed] [Google Scholar]
- 34.Alegría M, Canino G, Shrout PE, et al. Prevalence of mental illness in immigrant and non-immigrant U.S. Latino groups. Am J Psychiatry. 2008;165:359–369. doi: 10.1176/appi.ajp.2007.07040704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Van Voorhees B, Walters A, Prochaska M, Quinn M. Reducing health disparities in depressive disorders outcomes between non-Hispanic whites and ethnic minorities: A call for pragmatic strategies over the life course. Med Care Res Rev. 2007;64:157S–194S. doi: 10.1177/1077558707305424. [DOI] [PubMed] [Google Scholar]
- 36.Miranda J, McGuire TG, Williams DR, Wang P. Mental health in the context of health disparities. Am J Psychiatry. 2008;165:1102–1108. doi: 10.1176/appi.ajp.2008.08030333. [DOI] [PubMed] [Google Scholar]