Abstract
Background
Diabetes is a major health problem in Korea. However, interest in the quality of life in patients with diabetes is low. We examined the effects of diabetes on health-related quality of life (HRQoL) and compared it with HRQoL in the general Korean population using the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV) (2007-2009).
Methods
Using KNHANES IV data, we compared EuroQol (EQ)-5D and EQ-visual analogue scale (VAS) scores after adjusting for sociodemographic and psychosocial factors as well as for comorbidities (hypertension, heart disease, stroke, arthritis, and chronic renal disease). Logistic regressions were used to explore determinants for the lowest quintile HRQoL scales in the diabetes group.
Results
The mean age of the 14,441 enrolled subjects (6,129 men and 8,312 women) was 52.5±14.5 years. The mean EQ-5D and EQ-VAS scores were significantly lower in the diabetes group (EQ-5D. 0.87; EQ-VAS, 71.94) than in the non-diabetes group (EQ-5D, 0.94; EQ-VAS, 77.40) (P<0.001). Self-reported depressive symptom had a significant effect on lowering the EQ-VAS (odds ratio [OR], 1.7; 95% confidence interval [CI], 1.1 to 2.6) in the diabetes group. Stress level had a significant effect in lowering both the EQ-5D (OR, 2.0; 95% CI, 1.3 to 2.9) and the EQ-VAS (OR, 1.9; 95% CI, 1.3 to 2.9). HbA1c, diabetes duration, and treatment modalities had no significant effect on lowering HRQoL.
Conclusion
Diabetes was clearly associated with impaired HRQoL compared with the non-diabetic population regardless of comorbidities. Therapeutic approaches should focus much more on the subjective perception of health in patients with diabetes.
Keywords: Diabetes, EQ-5D, Health-related quality of life, Korea National Health and Nutrition Examination Survey
INTRODUCTION
Diabetes is not yet a curable disease. Dietary restrictions, medications including insulin injections, and diabetes-associated morbidities seriously deteriorate the quality of life (QoL) of patients with diabetes [1]. The World Health Organization defines health as not only the absence of disease and infirmity, but also the presence of physical, mental, and social well-being [2]. If the purpose of medicine is to make patients healthy, the aim of diabetes treatment should not be limited to controlling glycemia, and more focus should be placed on improving QoL for patients with diabetes.
Many recent studies have reported on health-related quality of life (HRQoL) in diabetes patients. HRQoL is poorer in patients with diabetes than in the general population [2,3]. A recent multinational study showed that diabetes has a notable impact on general health [4], and poor HRQoL in patients with diabetes is associated with adverse outcomes, including increased mortality [5].
Diabetes is a major health problem in Korea. The prevalence of diabetes was estimated to be 9.1% in 2005 [6] with a diabetes-related mortality rate of 24.5 per 100,000 persons in 2005, which is double that of a decade earlier [7]. Although there is growing interest in diabetes, interest in the QoL of patients with diabetes is relatively low, and few studies have reported on HRQoL in Korean patients with diabetes. In the present study, we examined the effects of diabetes on HRQoL and compared it with HRQoL in the general Korean population using data from the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV) (2007-2009).
METHODS
The Ministry of Health and Welfare of Korea began conducting KNHANES in 1998 to examine the general health and nutritional status of Koreans [6,8]. KNHANES IV was conducted from July 2007 to December 2009. The survey used a stratified multistage probability sampling design for the South Korean population and a two-stage stratified systematic sampling method. Clusters of households were selected from each district, each including an average of 20 to 23 households. KNHANES consists of four different measures: a health interview, a health behavior survey, a health examination, and a nutrition survey. In KNHANES IV, 31,705 individuals aged >1 year were sampled by the health interview and examination (6,455 in 2007, 12,528 in 2008, and 12,722 in 2009); these individuals represented 9,421 households in 200 districts (1,739 in 2007, 3,707 in 2008, and 3,975 in 2009). From the initial 31,705 individuals sampled, 24,871 participated in the survey (4,594 in 2007, 9,744 in 2008, and 10,533 in 2009), for a response rate of 78.4% (71.2% in 2007, 77.8% in 2008, and 82.8% in 2009). In the present study, we analyzed data from 14,441 subjects aged ≥30 years (6,129 men and 8,312 women), after excluding 1,461 individuals (964 non-respondents on diabetes status and EuroQol [EQ]-5D, 497 participants who had a cancer history). We excluded subjects with a history of malignancy because malignancies have obvious deleterious effects on QoL.
Presence of diabetes and measurement of QoL
The presence of diabetes was based on a self-reported questionnaire asking if the participants had ever been diagnosed with diabetes; undiagnosed patients who reported diabetes on the health examination survey were not included in this study because we assumed that self-perceived diabetes itself could affect HRQoL. Participants with diabetes were asked what year they were diagnosed and what treatment modalities they had experienced (no care, lifestyle modifications, oral hypoglycemic agents, and insulin). We calculated the duration of diabetes using the year of diabetes diagnosis and divided participants into groups based on that number: ≤10 years, 10 to 20 years, and ≥20 years.
The EuroQol was used evaluate HRQoL. The EuroQol consists of two parts, the health-status descriptive system (EQ-5D) and a visual analogue scale (EQ-VAS). The EQ-5D records the level of self-reported problems according to five dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) [9,10]. Each of the dimensions is assessed based on a single question with three response levels (no problems, some problems, and extreme problems). Using a combination of these items, a single health index score was calculated using the Korea valuation set developed by the Korean Centers for Disease Control and Prevention [11]. Scores on the EQ-5D index range from -0.171 to 1, where 1 indicates no problems in any of the five dimensions, zero indicates death, and negative values indicate a health status worse than death. Next, respondents described their own health status using a VAS ranging from 0 (worst imaginable health) to 100 (best imaginable health) [10].
Covariates
Participants were requested to provide information on household income (divided into quartiles), education level, current job status (employed or not), marital status (single, married, divorced, widow, or widower), current smoker (yes or no), frequency of alcohol consumption per week (more than or less than twice per week), level of psychological stress (none, low, moderate, extreme), continuous depressive symptoms during the past 2 weeks (yes or no). Participants also reported whether they had ever had comorbidities including malignancies, hypertension, heart diseases (acute myocardial infarction or angina), stroke, arthritis, and/or chronic renal disease.
Glycated hemoglobin (HbA1c) measurements
Subjects were instructed to fast after 7 PM on the day before blood sampling and to drink only bottled water after 7 PM The next morning, blood (2 mL) was collected from each participant into a NaF container. Samples were properly processed, refrigerated, and transported in cold storage to the Central Testing Institute at Seoul, Korea on the same day. HbA1c was measured using high-performance liquid chromatography. We divided HbA1c results into three categories (≤6.5%, 6.5% to 8.0%, and ≥8.0%).
Statistical analysis
All sample and weight variables were stratified, and the PASW complex-samples procedure was used for all statistical analyses. We used the stratification variables and sampling weights designated by the Korean Centers for Disease Control and Prevention for prevalence calculations, which were based on the sample design for each survey year. Sampling weights were adjusted for non-response according to demographic factors after the surveys were completed. The frequencies procedure was performed with cluster as a sampling-district variable, and prevalence was reported with a 95% confidential interval (CI). The descriptive procedure was used to evaluate the distribution of sociodemographic and clinical variables and QoL measurements. The crosstabs procedure was used to compare categorical or ordinal variables in participants with and without diabetes. The general linear model was used to compare continuous variables. Additionally, a sensitivity analysis was used to determine whether including undiagnosed patients with diabetes in the non-diabetes group would significantly alter the HRQoL score. We excluded undiagnosed patients with diabetes using the health examination survey in the non-diabetes group and compared the mean EQ-5D and EQ-VAS scores. General linear model analyses were also performed using the results of the EQ-5D and EQ-VAS for each chronic disease (diabetes, hypertension, heart diseases, stroke, arthritis, chronic renal disease) as dependent variables after controlling for age, gender, survey year, household income, educational level, current job, marital status, current smoking status, frequency of alcohol consumption, level of stress, self-reported depressive symptom, and other comorbidities. The survey year was also included as a controlled variable because the EQ-5D and EQ-VAS scores were significantly different according to survey year (data not shown). The EQ-5D and EQ-VAS scales were divided into quintiles, and the odd ratios (ORs) of the lowest quintile of these scales in the diabetes group were compared with those in the non-diabetic group after adjusting for age, gender, survey year, household income, educational level, current job, marital status, current smoking status, frequency of alcohol consumption, stress level, self-reported depressive symptoms, and other comorbidities (such as hypertension, heart diseases, stroke, arthritis, and chronic renal disease) using the logistic regression procedure. Four models were constructed. The ORs in model 1 were analyzed without adjustment. The ORs in model 2 were adjusted for age and gender. In model 3, ORs were further adjusted for survey year, household income, education level, marital status, percentage of current smokers, frequency of drinking, and level of stress and self-reported depressive symptom. In model 4, ORs were further adjusted for chronic diseases. Subsequently, we also performed subgroup analyses for participants with diabetes. Using the logistic regression procedure, the ORs of the lowest quintile of the EQ-5D and EQ-VAS scales for the level of HbA1c (≤6.5%, 6.5% to 8.0%, ≥8.0%), diabetes duration (≤10 years, 10 to 20 years, ≥20 years), treatment modalities (no care, lifestyle modification, oral hypoglycemic agents, insulin), self-reported depressive symptom, the level of stress, and other comorbidities were obtained after adjusting for age, gender, survey year, household income, educational level, current job, marital status, current smoking, and the frequency of alcohol consumption. All statistical analyses were conducted using PASW Statistics version 18.0 (SPSS Inc., Chicago, IL, USA). P values of less than 0.05 were considered statistically significant.
RESULTS
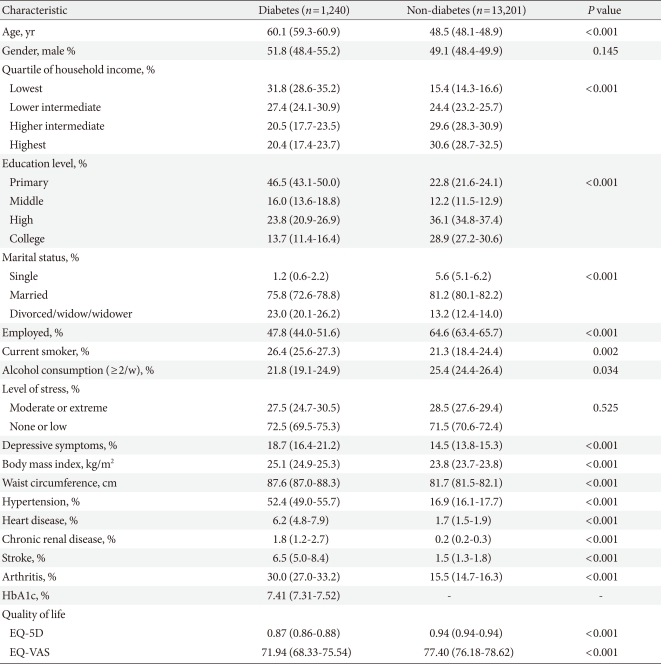
Of the 14,441 respondents, 1,240 (8.6%) reported that they had been diagnosed with diabetes. Characteristics of participants with and without diabetes are shown in Table 1.
Table 1.
Subject characteristics and EQ-5D and EQ-visual analogue scale (VAS) index scores
Values are presented as mean (95% confidence intervals).
The mean age for patients with diabetes was significantly higher than that of subjects without diabetes. Household income, education level, marital status, employment state, percentage of current smokers, and drinking frequency were also significantly different between the two groups. The level of psychological stress was similar between the two groups; however, self-reported depressive symptoms were significantly higher in the diabetes group than that in the non-diabetes group. The prevalence of chronic diseases such as hypertension, stroke, heart diseases, chronic renal disease, and arthritis was also significantly higher in the diabetes group than in the non-diabetic group. The mean EQ-5D index score was 0.87 (95% CI, 0.86 to 0.88) for those with diabetes and 0.94 (95% CI, 0.94 to 0.94) for those without diabetes (P<0.001). The mean EQ-VAS score was 71.94 (95% CI, 68.33 to 75.54) for those with diabetes and 77.40 (95% CI, 76.18 to 78.62) for those without diabetes (P<0.001). In the sensitivity analysis to determine whether the inclusion of undiagnosed patients with diabetes in the non-diabetes group would significantly alter the HRQoL score, no significant change was observed (0.87 vs. 0.94 for EQ-5D, 71.94 vs. 76.95 for EQ-VAS, P<0.01).
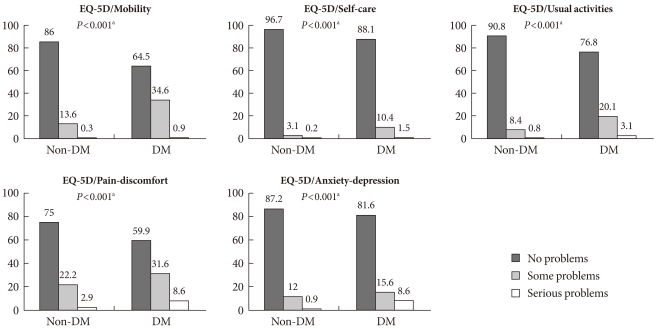
The percentages of subjects who had problems in each scale of the EQ-5D index are shown in Fig. 1. In total, 35.5% of those with diabetes had problems with mobility, 11.9% with self-care, 23.2% with usual activities, 40.2% with pain/discomfort, and 18.4% with anxiety/depression. For subjects without diabetes, the percentages were 13.9%, 3.3%, 9.2%, 25.1%, and 13.1%, respectively.
Fig. 1.
Distribution of perceived problem levels in each of the dimensions of the EQ-5D descriptive system for the diabetes (DM) and non-DM groups.
aSignificance level between with and without diabetes by chi-square test.
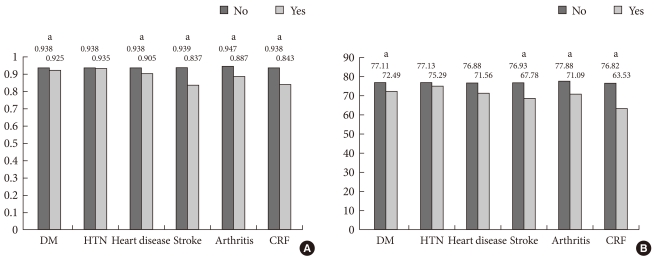
The mean EQ-5D index and EQ-VAS score were significantly lower in the diabetes group than in the group without diabetes. When we compared the mean EQ-5D index and EQ-VAS scores after adjusting for socio-demographic and psychosocial factors and for the presence of chronic diseases using a general linear model (Fig. 2), diabetes was still associated with deficits in HRQoL, with decreases of 0.013 units on the EQ-5D index and 4.62 units on the EQ-VAS compared with subjects without diabetes (P<0.05). However, the decreases in HRQoL were smaller than those for other chronic diseases (heart diseases, stroke, arthritis, and chronic renal disease), except hypertension, when controlling for other comorbidities.
Fig. 2.
Multi-variables adjusted means of (A) EQ-5D scores and (B) EQ-visual analogue scale (VAS) according to chronic diseases; diabetes (DM), hypertension (HTN), heart diseases, stroke, and chronic renal failure (CRF). aSignificant difference between those with and without the chronic disease (P<0.05).
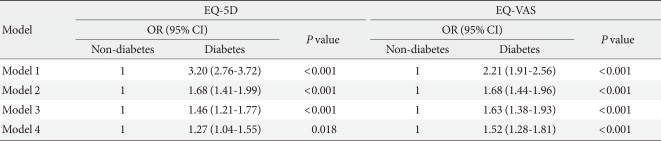
The ORs for the lowest quintile of the EQ-5D index and EQ-VAS score for the diabetes group compared with the non-diabetes group are shown in Table 2. In model 1, the OR for the lowest quintile of the EQ-5D index was 3.20 (95% CI, 2.76 to 3.72). Even in model 4, after adjusting for other factors including comorbidities, the significance did not change (OR, 1.27; 95% CI, 1.04 to 1.55). Similarly, the OR for the lowest quintile of the EQ-VAS score in model 1 was 2.21. In model 4, the OR for the lowest quintile of the EQ-VAS score was 1.52 (95% CI, 1.28 to 1.81).
Table 2.
Multivariate-adjusted odd ratios for the lowest quintile of the EQ-5D and EQ-visual analogue scale (VAS) scores for the diabetes group compared with the non-diabetes group
Model 1, no adjustments; Model 2, adjusted for age and gender; Model 3, adjusted for age, gender, year, household income, education level, marital status, occupational status, smoking, alcohol, stress, and presence of depression; Model 4, adjusted for age, gender, year, household income, education level, marital status, occupational status, smoking, alcohol, stress, presence of depression, and other chronic diseases (hypertension, heart diseases, stroke, arthritis, and chronic renal disease).
OR, odds ratio; CI, confidence interval.
We performed a subgroup analysis for patients with diabetes to examine the impacts of the HbA1c level, diabetes duration, treatment modalities, presence of depressive symptom, stress level, and comorbidities on impaired HRQoL (data not shown). The results indicated that HbA1c level, diabetes duration, and treatment modalities did not have significant effects on the HRQoL. Self-reported depressive symptom had a significant effect only on lower EQ-VAS (OR, 1.7; 95% CI, 1.1 to 2.6; P<0.05). However, the level of stress significantly lowered both EQ-5D (OR, 2.0; 95% CI, 1.3 to 2.9, P<0.01) and EQ-VAS (OR, 1.9; 95% CI, 1.3 to 2.9; P<0.01). Among the comorbidities tested, only stroke and heart diseases had significant effects on both EQ-5D and EQ-VAS.
DISCUSSION
Our results demonstrated that patients with diabetes had significantly lower HRQoL than those without diabetes. Our data are consistent with previous population-based studies that have demonstrated the considerable impact of diabetes on lower HRQoL [4,12,13]. Numerous demographic and psychosocial factors such as age, gender, depressive symptom, and psychological stress influence QoL. Diabetic complications are among the most important disease-specific determinants of QoL [1]. Actually, OR was largely attenuated in models 2, 3, and 4 (from 3.20 to 1.27) indicating that differences in age, income, education and diabetes complications play a large role in the observed difference in HRQoL. However, we also found that HRQoL scores remained low in patients with diabetes even after adjusting for many socio-demographic and psychosocial factors and comorbidities. Therefore, diabetes itself might lower HRQoL compared with that in the general population regardless of complications and other related factors.
In this study, patients with diabetes reported better HRQoL than did people with a variety of other chronic diseases (such as heart disease, stroke, arthritis, and chronic renal disease). Previous studies [14-16] have reported that patients suffering from stroke or heart disease had lower HRQoL than those with diabetes, and HRQoL in those with hypertension was higher than that for patients with diabetes [15]. Our finding that the HRQoL in Korean patients with diabetes was better than that in patients with other diseases was also consistent with previous studies.
QoL in patients with diabetes could be affected by various factors. Of these factors, we examined diabetes duration, HbA1c level, treatment modalities, depressive symptom, psychological stress, and comorbidities in a subgroup analysis of patients with diabetes. Our results demonstrated that subjective factors such as depressive symptom and psychological stress affected HRQoL. In contrast, objective factors related to diabetic status did not appear to affect HRQoL. In particular, HbA1c, an indicator of glycemic control, was not associated with impaired HRQoL. Thus, glycemic control itself may not necessarily translate to better QoL [17], and a subjective perception of well-being could be more important for the HRQoL of patients with diabetes than objective diabetic status.
There are some preference-based instruments, such as the Rosser Index, the 15D, the Quality of Well-Being scale, the Health Utility Index (HUI) versions II and III, the EQ-5D, and the SF-6D, which are based on the generic SF-36 health survey [18]. It has been suggested in some reports that the SF-36-based SF6D is more sensitive than the EQ5D in healthy people and for detecting small health changes, particularly at the extremes of the scale [19,20]. However, in the ADVANCE trial, algorithms based on survey instruments including more comprehensive aspects of HRQoL did not appear to measure greater variations in utility than those based on simpler instruments such as the EQ-5D. Moreover, the EQ-5D is easier to use and less time-consuming [21]. Therefore, the EQ-5D has some advantages, particularly for large population studies such as the KNHANES.
In this study, the presence of diabetes was based on a self-reported questionnaire, so the reliability of the diagnosis may be arguable. However, the mean HbA1c level for self-reported diabetes was 7.41% and showed clear differences between patients with diabetes and healthy subjects. Moreover, we originally thought that a subjective perception of disease could be more important for HRQoL than an objective diagnosis, and the results were not significantly different in the sensitivity analysis.
The strength of our study was that these data were obtained from a nationwide population with a high response rate and therefore provided representative information on the Korean population. Nevertheless, several study limitations should be considered. First, although diabetes complications were closely related to individual HRQoL level [1], we did not assess all diabetic complications because KNHANES is not a survey only for diabetes and does not provide all data related to diabetes complications. We did control for other comorbidities, including heart diseases (acute myocardial infarction and angina) and stroke, which are macrovascular complications, and for chronic renal disease, which is a microvascular complication. Although it is possible that uncontrolled diabetic complications could have affected the lower HRQoL observed in the diabetic group, the possibility that diabetes itself affects QoL still exists regardless of diabetes complications. To examine this possibility, further studies on HRQoL in patients with diabetes are needed, including a complete investigation of diabetic complications. Second, we did not determine whether the patients with diabetes had type 1 or type 2 diabetes. However, only 35 patients may have had type 1 diabetes (about 3% among all diabetes diagnoses) based on a diagnosis before the age of 30 years in this survey. Therefore, we considered that most patients in the study population had type 2 diabetes. Third, we could not measure HRQoL using a diabetes-specific quality of life tool [22-24] as none have been validated in Korea, and only EQ-5D was measured in KNHANES. Studies are needed that use disease-specific QoL tools to assess the association between diseases and HRQoL [25].
In conclusion, we found that diabetes was clearly associated with impaired HRQoL compared with a population without diabetes. This association may be independent of other comorbidities. In patients with diabetes, subjective factors such as depression and psychological stress, rather than objective factors such as glycemic control, were related to impaired HRQoL, suggesting that objectively well-controlled diabetes does not necessarily translate to a better QoL. Therapeutic approaches should focus more on the subjective perception of health by patients with diabetes, and further studies on HRQoL are needed for Korean patients with diabetes.
ACKNOWLEDGMENTS
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry of Health and Welfare, Republic of Korea (A102065).
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15:205–218. doi: 10.1002/(sici)1520-7560(199905/06)15:3<205::aid-dmrr29>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 2.Constitution of the World Health Organization. Handbook of basic documents. 5th ed. Geneva: Palais des Nation; 1952. pp. 3–20. [Google Scholar]
- 3.Saito I, Inami F, Ikebe T, Moriwaki C, Tsubakimoto A, Yonemasu K, Ozawa H. Impact of diabetes on health-related quality of life in a population study in Japan. Diabetes Res Clin Pract. 2006;73:51–57. doi: 10.1016/j.diabres.2005.11.015. [DOI] [PubMed] [Google Scholar]
- 4.Alonso J, Ferrer M, Gandek B, Ware JE, Jr, Aaronson NK, Mosconi P, Rasmussen NK, Bullinger M, Fukuhara S, Kaasa S, Leplege A IQOLA Project Group. Health-related quality of life associated with chronic conditions in eight countries: results from the International Quality of Life Assessment (IQOLA) Project. Qual Life Res. 2004;13:283–298. doi: 10.1023/b:qure.0000018472.46236.05. [DOI] [PubMed] [Google Scholar]
- 5.Kleefstra N, Landman GW, Houweling ST, Ubink-Veltmaat LJ, Logtenberg SJ, Meyboom-de Jong B, Coyne JC, Groenier KH, Bilo HJ. Prediction of mortality in type 2 diabetes from health-related quality of life (ZODIAC-4) Diabetes Care. 2008;31:932–933. doi: 10.2337/dc07-2072. [DOI] [PubMed] [Google Scholar]
- 6.Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care. 2009;32:2016–2020. doi: 10.2337/dc08-2228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Korea National Statistical Office. 2005 statistical results about cause of death. Daejeon: Korea National Statistical Office; 2006. [Google Scholar]
- 8.Kim SM, Lee JS, Lee J, Na JK, Han JH, Yoon DK, Baik SH, Choi DS, Choi KM. Prevalence of diabetes and impaired fasting glucose in Korea: Korean National Health and Nutrition Survey 2001. Diabetes Care. 2006;29:226–231. doi: 10.2337/diacare.29.02.06.dc05-0481. [DOI] [PubMed] [Google Scholar]
- 9.The EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 10.Brooks R. EuroQol: the current state of play. Health Policy. 1996;37:53–72. doi: 10.1016/0168-8510(96)00822-6. [DOI] [PubMed] [Google Scholar]
- 11.Nam HS, Kim KY, Kwon SS, Koh KW, Poul K. EQ-5D Korean valuation study using time trade of method. Seoul: Centers for Disease Control and Prevention; 2007. [Google Scholar]
- 12.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 13.Smith DW. The population perspective on quality of life among Americans with diabetes. Qual Life Res. 2004;13:1391–1400. doi: 10.1023/B:QURE.0000040785.59444.7c. [DOI] [PubMed] [Google Scholar]
- 14.Stewart AL, Greenfield S, Hays RD, Wells K, Rogers WH, Berry SD, McGlynn EA, Ware JE., Jr Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. JAMA. 1989;262:907–913. [PubMed] [Google Scholar]
- 15.Vickrey BG, Hays RD, Rausch R, Sutherling WW, Engel J, Jr, Brook RH. Quality of life of epilepsy surgery patients as compared with outpatients with hypertension, diabetes, heart disease, and/or depressive symptoms. Epilepsia. 1994;35:597–607. doi: 10.1111/j.1528-1157.1994.tb02480.x. [DOI] [PubMed] [Google Scholar]
- 16.Naess S, Midthjell K, Moum T, Sorensen T, Tambs K. Diabetes mellitus and psychological well-being. Results of the Nord-Trondelag health survey. Scand J Soc Med. 1995;23:179–188. doi: 10.1177/140349489502300308. [DOI] [PubMed] [Google Scholar]
- 17.Ali S, Stone M, Skinner TC, Robertson N, Davies M, Khunti K. The association between depression and health-related quality of life in people with type 2 diabetes: a systematic literature review. Diabetes Metab Res Rev. 2010;26:75–89. doi: 10.1002/dmrr.1065. [DOI] [PubMed] [Google Scholar]
- 18.Kontodimopoulos N, Pappa E, Papadopoulos AA, Tountas Y, Niakas D. Comparing SF-6D and EQ-5D utilities across groups differing in health status. Qual Life Res. 2009;18:87–97. doi: 10.1007/s11136-008-9420-8. [DOI] [PubMed] [Google Scholar]
- 19.Kopec JA, Willison KD. A comparative review of four preference-weighted measures of health-related quality of life. J Clin Epidemiol. 2003;56:317–325. doi: 10.1016/s0895-4356(02)00609-1. [DOI] [PubMed] [Google Scholar]
- 20.Longworth L, Bryan S. An empirical comparison of EQ-5D and SF-6D in liver transplant patients. Health Econ. 2003;12:1061–1067. doi: 10.1002/hec.787. [DOI] [PubMed] [Google Scholar]
- 21.Glasziou P, Alexander J, Beller E, Clarke P ADVANCE Collaborative Group. Which health-related quality of life score? A comparison of alternative utility measures in patients with type 2 diabetes in the ADVANCE trial. Health Qual Life Outcomes. 2007;5:21. doi: 10.1186/1477-7525-5-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Influence of intensive diabetes treatment on quality-of-life outcomes in the diabetes control and complications trial. Diabetes Care. 1996;19:195–203. doi: 10.2337/diacare.19.3.195. [DOI] [PubMed] [Google Scholar]
- 23.Boyer JG, Earp JA. The development of an instrument for assessing the quality of life of people with diabetes. Diabetes-39. Med Care. 1997;35:440–453. doi: 10.1097/00005650-199705000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, Schwartz CE. Assessment of diabetes-related distress. Diabetes Care. 1995;18:754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- 25.El Achhab Y, Nejjari C, Chikri M, Lyoussi B. Disease-specific health-related quality of life instruments among adults diabetic: a systematic review. Diabetes Res Clin Pract. 2008;80:171–184. doi: 10.1016/j.diabres.2007.12.020. [DOI] [PubMed] [Google Scholar]