Abstract
Background
High-altitude travel, for mountain climbing, trekking, or sightseeing, has become very popular. Therefore, the awareness of its dangers has increased, and many prospective travelers seek medical advice before setting forth on their trip.
Methods
We selectively searched the literature for relevant original articles and reviews about acclimatization to high altitude and about high-altitude-related illnesses, including acute mountain sickness (AMS), high-altitude cerebral edema (HACE), and high-altitude pulmonary edema (HAPE) (search in Medline for articles published from 1960–2010).
Results
High-altitude-related illnesses are caused by hypoxia and the resulting hypoxemia in otherwise healthy persons who travel too high too fast, with too little time to become acclimatized. The individual susceptibility to high-altitude-related illness is a further risk factor that can only be recognized in persons who have traveled to high altitudes in the past. In an unselected group of mountain climbers, 50% had AMS at 4500 meters, while 0.5–1% had HACE and 6% had HAPE at the same altitude. Persons with preexisting illnesses, particularly of the heart and lungs, can develop symptoms of their underlying disease at high altitudes because of hypoxia. Thus, medical advice is based on an assessment of the risk of illness in relation to the intended altitude profile of the trip, in consideration of the prospective traveler’s suitability for high altitudes (cardiopulmonary performance status, exercise capacity) and individual susceptibility to high-altitude-related illnesses, as judged from previous exposures. The symptoms and treatment of high-altitude-related illnesses should be thoroughly explained.
Conclusion
An understanding of the physiology of adaptation to high altitudes and of the pathophysiology and clinical manifestations of high-altitude-related illnesses provides a basis for the proper counseling of prospective travelers, through which life-threatening conditions can be prevented.
Trekking and culture-oriented vacations in Tibet and the Andes have become highly popular. Persons who have never journeyed to high altitudes before are now booking trips to mountains that can be climbed relatively easily despite altitudes of 5000 to almost 7000 meters, such as Kilimanjaro, volcanoes in Mexico and Ecuador, and Aconcagua. Meanwhile, skiing and hiking at altitudes of 2000 to 3000 meters have become more common as well. Patients now often ask their physicians about the risks of such ventures and how best to prepare for them. To advise competently, physicians need not just a basic knowledge of tropical and travel-related medicine, but also an understanding of altitude adaptation, altitude sicknesses, and the effects of hypoxia on pre-existing illnesses.
Learning objectives
The purpose of this article is to acquaint the reader with
the main risk factors for acute mountain sickness, high-altitude cerebral edema and pulmonary edema, and
the essential elements of competent medical advice before travel to high altitudes.
The main aspects of these topics are discussed in the light of a selective literature review.
Acute adaptation to high altitude.
With increasing altitude, the air pressure falls, and with it the PO2 in inhaled air, the arterial PO2, and the O2 saturation of the blood. Hypoxemia is registered by peripheral chemoreceptors, leading to hyperventilation.
The physiology of adaptation
Acute adaptation to high altitude
As a person ascends to higher altitudes, the air pressure falls, and with it the partial pressure of O2 (PO2) in inhaled air, the arterial PO2, and the O2 saturation of the blood. Hypoxemia is registered by peripheral chemoreceptors (1, 2), leading to hyperventilation, which raises the alveolar PO2 to some extent, and to activation of the sympathetic nervous system, with a resulting rise in the heart rate compensating for the lesser O2 content of the blood pumped by each heartbeat. This acute adaptation cannot fully counteract the altitude-induced limitation of maximal oxygen transport and the resulting limitation of aerobic capacity (VO2max). Untrained persons lose about 1% of VO2max for every 100 m of ascent above 1500 m; thus, aerobic capacity falls by about 10% at 2500 m, by 25% at 4000 m, and by 65% at 8000 m (3). At high altitudes, the performance of physical exercise that demands submaximal oxygen consumption is associated with higher ventilation and a higher heart rate than at sea level. The arterial blood pressure remains roughly constant: sympathetic activation would tend to raise it, but this effect is cancelled out by the peripheral vasodilatation that is directly induced by hypoxia (4).
The classification of altitude sicknesses.
Acute mountain sickness
High-altitude cerebral edema
High-altitude pulmonary edema
Acclimatization to high altitude
The oxygen supply in bodily tissues improves within a few days (3) for two reasons: there is a further rise in ventilation (“ventilatory acclimatization”) that continuously increases for 1–2 weeks and that is maintained thereafter throughout the stay at a particular altitude (e1) (for definitions of altitude see Table 1); also, the plasma volume is constricted (e2). After 2–3 weeks at altitudes above 2000–2500 m, increased erythropoiesis (e2) further raises the hemoglobin concentration. These mechanisms of acclimatization increase the amount of oxygen transported per unit volume of blood, thereby improving submaximal performance ability: they enable the individual to perform the same tasks with a slower heart rate, with less shortness of breath, and with a lesser feeling of exertion (e3). Nonetheless, acclimatization can no longer improve O2max at altitudes above 4000 m, because the altitude-induced redistribution of perfusion takes blood away from the musculature and does not raise the cardiac minute volume (e4). Longer stays at high altitudes are associated with rising blood pressure because of increased sympathetic activation: at 4500 m, this rise is on the order of 10 mm Hg (4, e5, e6).
Table 1. Classification of altitude levels (modified from [3]).
| Altitude level*1 | Remarks |
| Near sea level (0–500 m) | No altitude-related problems |
| Low altitude(>500–2000 m) |
|
| Moderate altitude(>2000–3000 m) |
|
| High altitude(>3000–5500 m) |
|
| Extreme altitude (>5500 m) |
|
*1 Terminology recommended by an international expert panel (3)
*2 Patients with cardiovascular and pulmonary diseases that may worsen under hypoxic conditions
Acclimatization to high altitude.
The oxygen supply in bodily tissues improves within a few days through a further rise in ventilation and plasma volume constriction.
Altitude sicknesses
The three main types of altitude sickness are acute mountain sickness (AMS), high-altitude cerebral edema (HACE), and high-altitude pulmonary edema (HAPE). Their characteristic symptoms and signs are listed in Table 2. The indicated references are recommended for further information.
Table 2. Overview of altitude sicknesses.
| Symptoms | Findings | Recommended reading | |
| Acute mountain sickness (AMS) |
|
|
{7} |
| High-altitude cerebral edema (HACE) |
|
|
(10) |
| High-altitude pulmonary edema (HAPE) |
|
|
(12) |
Risk factors that are common to all three of these conditions are
the absolute altitude,
the speed of ascent,
individual predisposition, and
lack of acclimatization (5).
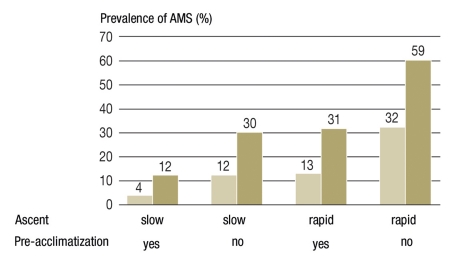
The Figure shows how these factors interact to produce AMS at an altitude of 4559 m.
Figure.
The prevalence of acute mountain sickness (AMS) in 827 mountain-climbers at 4559 m as a function of the rate of ascent, pre-acclimatization, and susceptibility to AMS. Definitions: slow ascent, an ascent from 2000 m to 4559 m over more than 3 days; pre-acclimatization, more than 4 days spent above 3000 m in the preceding 2 months; non-suceptibility to AMS, prior experience of altitudes above 3000 m with no more than rare headache and a history score below 4 points. Darker columns indicate susceptible, lighter columns non-susceptible, mountaineers (modified from [5])
Thus, the main elements to be considered in assessing the risk of altitude sickness are the intended profile of ascent, particularly the altitude of overnight stays, and the individual predisposition, which can only be assessed on the basis of earlier trips to high altitudes, if there have been any.
Acute mountain sickness
The main symptom of acute mountain sickness (6, 7) is headache. There may also be nonspecific symptoms such as malaise, dizziness, anorexia, nausea, and sleep disturbance.
AMS arises after at least 4–6 hours spent at an altitude above 2000–2500 m. Its reported prevalence ranges from 8% to 25% at 2500–3000 m and from 40% to 60% at 4500 m, depending on the definition of AMS and on the subjects under study (mountain climbers or tourists) (e7– e9).
Acute mountain sickness is usually most severe after the first night at a new, higher altitude. It is promoted and exacerbated by intense physical exercise (e10). The symptoms usually resolve in 24 to 48 hours if the sufferer does not ascend any further and avoids strenuous exercise. Further ascent in the presence of symptoms of AMS is dangerous, because high-altitude cerebral edema (HACE) may ensue. The pathophysiology is currently unclear.
Acute mountain sickness is usually associated with marked hypoxemia; the cause may be interstitial pulmonary edema, leading to a mild increase in respiratory rate and to reduced gas exchange (e11). The migraine-like nature of AMS symptoms has prompted speculation that they may be mediated by activation of the trigeminovascular system (e12, e13).
A number of magnetic resonance imaging (MRI) studies have shown that acute mountain sickness is not associated with any appreciable degree of cerebral edema (8, e14, e15).
Risk factors for all three altitude sicknesses.
Absolute altitude
Speed of ascent
Individual predisposition
Lack of acclimatization
Acute mountain sickness.
The main symptom of acute mountain sickness is headache. There may also be nonspecific symptoms such as malaise, dizziness, anorexia, nausea, and sleep disturbance.
High-altitude cerebral edema
High-altitude cerebral edema (HACE) (9) is usually preceded by symptoms of acute mountain sickness, such as intractable headache and vomiting. Nonetheless, the absence of AMS symptoms does not rule out HACE. In practically all cases, HACE arises after at least 48 hours spent at altitudes above 4000 m. Its prevalence at 4000–5000 m is estimated at 0.5% to 1%. Its main symptoms are truncal ataxia with inability to walk and/or impaired consciousness, with possible worsening to coma within hours (10). The arterial oxygen saturation is very low in relation to the altitude (at least 20% lower than the altitude-specific normal value). Fever is usually present. If not adequately treated, HACE is usually fatal. Cerebral edema can cause brain herniation with brainstem compression leading to death within 24 hours of the onset of illness. Cerebral MRI of HACE survivors reveals microhemorrhages in the corpus callosum (11).
High-altitude pulmonary edema
An early symptom of high-altitude pulmonary edema (HAPE) is a marked loss of exercise capacity during ascent, often accompanied by dyspnea and an initially dry cough (12).
High-altitude cerebral edema.
High-altitude cerebral edema (HACE) is usually preceded by symptoms of acute mountain sickness, such as intractable headache and vomiting. Nonetheless, the absence of these symptoms does not rule out HACE.
Persons with the initial symptoms of HAPE who remain at a high altitude or continue to ascend develop dyspnea at rest, orthopnea, bloody sputum, cyanosis, and pulmonary rales. Severe hypoxemia, if present, leads to concomitant cerebral edema. HAPE usually develops within 48 to 72 hours of a very rapid ascent above 4000 m (e16). HAPE generally does not arise after five days at an altitude to which one has become acclimatized.
The risk of high-altitude pulmonary edema essentially depends on the speed of ascent, the altitude reached, and the individual predisposition (e17), as shown in Table 3. The decisive pathogenetic factor is an excessive and inhomogeneous pulmonary arterial vasoconstriction in response to hypoxia, which probably arises on a genetic basis (13).
Table 3. The prevalence of high-altitude pulmonary edema (HAPE) by location, type of climber, and speed of ascent.
| Altitude | Time for ascent | Rate of HAPE | |
| Alps (mountain climbers) | 4559 m | 2–4 days | <0.8% |
| Himalayas (trekkers) | 5450 m | 6 days | 2.3% |
| Alps (persons without known ‧susceptibility to HAPE) | 4559 m | 22 hours | 6% |
| Himalayas (soldiers) | 5400 m | <10 hours | 15.5% |
| Alps (persons with known ‧susceptibility to HAPE) | 4559 m | 22 hours | 62% |
If pulmonary edema arises at altitudes below 3000 m, a preexisting illness should be sought, e.g., (latent) left heart failure, pulmonary embolism, or an absent pulmonary artery on one side (e18).
High-altitude pulmonary edema.
An early symptom of high-altitude pulmonary edema (HAPE) is a marked loss of exercise capacity during ascent, often accompanied by dyspnea and an initially dry cough.
The prevention of altitude sicknesses
Non-pharmacological prevention
The best way to prevent altitude sicknesses is to ascend slowly. Persons with a predisposition to high-altitude cerebral edema and high-altitude pulmonary edema who ascend to altitudes higher than 2500 m should not spend the night at an altitude any more than 300–350 m higher than the previous night (e17). Persons with a predisposition to acute mountain sickness can tolerate ascents of 400–500 m daily above 2500 m when trekking to destinations no higher than 5000 m. In the Alps, ascents are now generally made rapidly, and often passively, for overnight stays at altitudes up to 3500 m (e.g., by mountain railway or other modes of transport). At such altitudes, the symptoms of acute mountain sickness are usually mild; nonetheless, persons predisposed to acute mountain sickness, HACE and/or HAPE should avoid such rapid ascents. If the destination lies above 4000 m, an ascent over several days is recommended. Alternatively, tours can be made at intermediate heights for pre-acclimatization: For example, before trekking in the Himalayas with a rapid ascent from 3500 m to 5000 m, it may be helpful to visit the Alpine region beforehand, with overnight stays at altitudes that are as high as possible. Briefer exposures to hypoxia—e.g., daily training under hypoxic conditions, usually normobaric (created by mixing nitrogen gas with inhaled air), as offered in specialized fitness studios—do not afford adequate protection against altitude sicknesses with rapid ascent above 4000 m (14).
Further consequences of HAPE.
Persons with the initial symptoms of HAPE who remain at a high altitude or continue to ascend develop dyspnea at rest, orthopnea, bloody sputum, cyanosis, and pulmonary rales.
Pharmacological prevention
Prophylactic medication should be considered if a person with known susceptibility will be making an ascent without any opportunity for a slow ascent or preliminary acclimatization.
Numerous prospective, placebo-controlled studies have documented the efficacy of pharmacological prevention of acute mountain sickness and high-altitude pulmonary edema, but not of high-altitude cerebral edema. No Cochrane reviews have yet been published on this topic.
Indications for prophylactic medication.
Prophylactic medication should be considered if a person with known susceptibility will be making an ascent without any opportunity for a slow ascent or preliminary acclimatization.
The efficacy of acetazolamide 250 mg p.o. b.i.d. for the prevention of acute mountain sickness has been documented in a large mumber of placebo-controlled double-blind studies (15, 16, e19); a meta-analysis that has been the target of much criticism (e20) came to the conclusion that 750 mg/day would be a more effective dose. By increasing the renal excretion of bicarbonate, acetazolamide leads to acidosis-triggered hyperventilation and thereby to a rise in oxygen saturation (e21, e22). Its side effects are paresthesiae and an altered perceived taste of carbonated drinks. Dexamethasone 4 mg p.o. b.i.d. or t.i.d. (or the equivalent dose of another steroid) can be used to prevent acute mountain sickness as well (e23, e24), but should only be given in case of intolerance of acetazolamide, in view of the known side effects of high-dose steroids. If treatment is given for more than five days, the steroid dose must be tapered off. As high-altitude cerebral edema generally arises by the progression of acute mountain sickness, the preventive strategies for HACE are the same as those for AMS. On the other hand, medications that lower the pulmonary-arterial blood pressure are effective in the prevention of high-altitude pulmonary edema. Nifedipine is the the best established drug for this indication (17) (60 mg of a timed-release preparation daily, in 2 or 3 divided doses). PDE-5-esterase inhibitors such as tadalafil (18) (10 mg p.o. b.i.d.) can also be used. Dexamethasone 8 mg p.o. b.i.d. can also prevent high-altitude pulmonary edema if begun at least 24 hours before the ascent to a high altitude (18).
The treatment of altitude sicknesses.
Improving the oxygen supply to the body’s tissues is the main consideration. This can be achieved by descent, by supplemental oxygen administration, or by raising the pressure of inhaled air with portable pressure bags.
The treatment of altitude sicknesses
Improving the oxygen supply to the body’s tissues is the main consideration. This can be achieved by descent, by supplemental oxygen administration, or by raising the pressure of inhaled air with portable pressure bags (19). At the first sign of high-altitude cerebral or pulmonary edema, the affected individual must descend immediately. If the symptoms are too severe for descent, medications should be used to bring about enough symptomatic improvement for the patient to descend. In this situation, a descent of at least 1000 m is usually required. Mild symptoms of acute mountain sickness generally resolve in 24 to 48 hours with rest and symptomatic treatment. Any further ascent should be deferred until the symptoms have nearly totally resolved; otherwise, there is the danger that AMS may undergo a transition to high-altitude cerebral edema. An overview of the pharmacotherapy of altitude sicknesses is given in Table 4. Steroids are indicated for the treatment of severe acute mountain sickness (20) and high-altitude cerebral edema; they are ineffective for the acute treatment of high-altitude pulmonary edema (e25, e26). If a journey to high altitudes is planned where there is inadequate infrastructure for immediate descent, the authors recommend that a mountain guide with training in high-altitude medicine take along dexamethasone and nifedipine in his or her backpack in case of emergency.
Table 4. The pharmacotherapy of altitude sicknesses.
| Type of altitude sickness | Drug | Dose | Administration | Remarks |
| Mild acute mountain ‧sickness (AMS) | IbuprofenParacetamol Metoclopramide Domperidone | 400 mg500–1000 mg 10 mg 10 mg | p.o.p.o. p.o. p.o., s.l. | Up to 4 x / 24 hr as neededUp to 4 g / 24 hr as needed Up to 4 x / 24 hr as needed Up to 8 x / 24 hr as needed |
| Severe AMS | Dexamethasone | 4–8 mg | p.o., i.m., i.v. | Every 6 hr |
| High-altitude cerebral ‧edema (HACE) | Dexamethasone | 4 mg | i.m., i.v. | Every 6 hr |
| High-altitude pulmonary ‧edema (HAPE) | Nifedipine (1st choice)Tadalafil* | 20–30 mg10 mg | p.o.p.o. | Every 8 hr, timed-release Every 12 hr (not tested) |
| Simultaneous high-altitude pulmonary & cerebral ‧edema | Like HAPE, plus dexa‧methasone | 4–8 mg | i.m., i.v. | Every 6 hr |
p.o.: per os; s.l.: sublingual; i.m.: intramuscular; i.v.: intravenous.* Unlike nifedipine (25), there are no prospective studies for the use of tadalafil (or other phosphodiesterase inhibitors) in the treatment of HAPE—listed as an alternative to nifedipine because of the authors’ own (unpublished) observations in a small number of cases
Counseling
The elements of a consultation in high-altitude medicine are the following:
assessment of the risk of altitude sicknesses,
recognition of any preexisting cardiopulmonary diseases and assessment of their relevance to high-altitude exposures,
assessment of exercise capacity in view of the intended activities and altitude,
patient education about the symptoms of altitude sicknesses and their treatment.
Risk profiles that demand attention are listed in the Box.
Box. Altitude tolerance among patients with common cardiovascular and pulmonary diseases.
-
Travel to altitudes above 2000 m inadvisable:
1.1 Cardiovascular diseases
Within 3 months of myocardial infarction, stroke, ICD implantation, thromboembolic event
Unstable angina pectoris
Before planned coronary interventions
Heart failure, NYHA class >II
Congenital cyanotic or severe acyanotic heart defect
1.2 Pulmonary diseases
Pulmonary arterial hypertension
Severe or exacerbated COPD (GOLD stage III–IV)
FEV1 <1 liter
CO2 retention
Poorly controlled asthma
-
Travel to altitudes of 2000–3000 m permissible:
2.1 Cardiac diseases
asymptomatic or stable CHD (CCS I–II)
Stress ECG normal up to 6 METs
Normal performance capacity for age
Blood pressure under good control
No high-grade cardiac arrhythmia
No concomitant illnesses affecting gas exchange
2.2 Pulmonary diseases
Stable COPD or asthma under medical treatment, with adequate reserve function for the planned activity
-
For travel to altitudes above 3000 m:
Evaluation by a specialist in altitude medicine and physiology
ICD, implantable cardiac defribrillator; NYHA, New York Heart Association; COPD, chronic obstructive pulmonary disease; GOLD, Global Initiative for Chronic Obstructive Lung Disease; FEV1, forced expiratory volume in 1 second; CHD, coronary heart disease; CCS, Canadian Cardiovascular Society; MET, metabolic equivalent of task
Altitude profile
Risk stratification is best performed on the basis of an altitude profile showing the average and the daily difference in altitude (in relation to the altitude at which the patient will be spending the night) as well as the altitude of the destination. Other considerations include the degree of physical effort required (the duration of each climb in relation to altitude), specific topographical features (plateaus, mountain passes) that may affect the possibility of descent, and the local medical infrastructure. The segmentation of altitudes in Table 1 has been performed in such a way as to yield a practical indication of the risk at each altitude level (3).
Determination of baseline conditions
One must consider the following issues to determine whether the patient meets the prerequisite conditions for undertaking the intended expedition.
Preexisting illnesses—In particular, any cardiopulmonary diseases that might decompensate at high altitude must be recognized beforehand. Recommendations for patients with common cardiopulmonary diseases are summarized in the Box These are taken from recent publications (4, 21–23) that interested readers may consult for further information. There have been no more than a few prospective studies (e27– e49) on the ability of patients with preexisting illnesses to tolerate high altitudes; thus, these recommendations are largely based on expert opinion.
Acute treatment.
For trips to high altitudes without the option of immediate descent, the authors recommend that a mountain guide trained in high-altitude medicine take along dexamethasone and nifedipine in his or her backpack in case of emergency.
As a rule, persons with cardiopulmonary diseases who are oligo- or asymptomatic, in stable condition, and under adequate treatment, can tolerate moderately high altitudes well and generally do not have any more medical difficulties than at lower altitudes at unchanged levels of physical activity and with adequate reserve capacity. Such persons should avoid exertion until some acclimatization has occurred, leading to an improvement of their tissue oxygen supply; this takes no more than 2 to 3 days at moderately high altitudes. This also applies to skiers who are exposed to altitudes of 2000 to 3000 m only in the daytime while skiing. At altitudes above 2000 m, each overnight stay should be no more than 300 or 400 m higher than that of the previous night.
As hardly any clinical studies have been performed on altitude exposures above 3000 m in persons with preexisting conditions, and because many different factors relating to the patient’s illness and altitude physiology have to be considered in such situations, the authors recommend referring such patients for a consultation with a physician with special expertise in high-altitude medicine.
Assessment of performance status—The question whether an individual’s physical performance will be up to the proposed trip can be answered in the light of his or her sport history, making allowance for the expected reduction of performance capacity at high altitudes (the altitude-related reduction of VO2max was already mentioned above). In general, anyone who can hike for several hours at a normal pace in the Alps without symptoms at 2500 to 3000 m should be able to tolerate similar exercise one altitude level higher while trekking, though perhaps at reduced speed. If inadequate performance ability is suspected, particularly in persons with heart or lung disease, spiroergometry should be performed to measure performance ability directly and judge whether performance is limited by illness.
Assessment of performance status.
In general, anyone who can hike for several hours at a normal pace in the Alps without symptoms at 2500 to 3000 m should be able to tolerate similar exercise one level higher while trekking, though perhaps at reduced speed.
Assessment of the risk of altitude sicknesses.
The best predictor is the individual’s condition during a previous expedition that was comparable in terms of preparation, speed of ascent, and terminal altitude.
Assessment of the risk of altitude sicknesses
As individuals vary greatly in their susceptibility to altitude sicknesses, many attempts have been made to detect susceptible persons by testing under conditions of acute hypoxia (e50– e52). Unfortunately, however, the measurement of ventilation, heart rate, blood gases, and pulmonary arterial pressure in acute hypoxia is an inadequate means of identifying susceptible persons with the requisite sensitivity and specificity (24). None of the tests that are occasionally recommended has been validated in a prospective study, with the single exception of pulmonary arterial pressure measurement—which has been found to be inadequately sensitive for the identification of persons susceptible to high-altitude pulmonary edema (authors’ own unpublished data). Thus, the best predictor is still the individual’s condition during a previous expedition that was comparable in terms of preparation, speed of ascent, and terminal altitude. If such information is not available, the individual should climb slowly to avoid inducing any symptoms of altitude sickness, and should have the option of resting for a day or two in case symptoms do arise. It has been shown that even persons who are susceptible to high-altitude pulmonary edema remain asymptomatic if they climb an average of 300 to 350 m per day at altitudes above 2000 m (e16), while non-susceptible persons can tolerate 400 to 500 m per day (e53). If the destination lies above 5000–6000 m, the ascent should be slower; preacclimatization, however, enables a much more rapid ascent.
Prophylactic medication against altitude sickness can be considered if acute mountain sickness or high-altitude pulmonary edema seems likely to arise, e.g., when persons of unknown susceptibility plan to ascend rapidly (for example, climbing Kilimanjaro in 4–5 days) or when a person who is known to be susceptible has no way of avoiding a relatively rapid ascent. Pulmonary vasodilators should only be prescribed for the prevention of high-altitude pulmonary edema if the patient has had an episode of HAPE in the past.
Information about altitude sicknesses
Travelers to high altitudes should be well acquainted with altitude sicknesses and with the proper measures to be taken in case symptoms arise. This information is found in books on the subject and on the Internet home pages of a number of societies for high-altitude medicine, e.g., the Mountain Medicine Information Center (www.ismmed.or). Physicians can obtain further training in high-altitude medicine in special courses offered by the German Society for Sports Medicine and Prevention (Deutsche Gesellschaft für Sportmedizin und Prävention, DGSP) in collaboration with the Department of Sports Medicine of the University of Heidelberg (http://ams-die-akademie.de), or by the German Society for Mountain and Expedition Medicine (Deutsche Gesellschaft für Berg- und Expeditionsmedizin, www.bexmed.de). These courses lead to a diploma that is recognized by the International Society for Mountain Medicine (ISMM).
Patient education is essential.
Travelers to high altitudes should be well acquainted with altitude sicknesses and the proper measures to be taken in case symptoms arise.
Key Messages.
At high altitudes, oxygen transport to the body’s tissues improves in the first few days and weeks through the process of acclimatization.
The main risk factors for acute mountain sickness, high-altitude cerebral edema, and high-altitude pulmonary edema are a lack of acclimatization, individual susceptibility, rapid ascent, and high altitude.
The essential elements of medical counseling for trips to high altitudes are an assessment of the risk of altitude sicknesses, the recognition of preexisting cardiopulmonary illnesses, an evaluation of physical performance reserve in view of the planned activities and altitude, and patient education about the symptoms of altitude sicknesses and their treatment.
Persons with coronary heart disease, chronic obstructive pulmonary disease, or bronchial asthma who have good performance ability for their age, are medically stable, and have few or no symptoms can generally tolerate altitudes up to 3000 m without difficulty. Such persons who plan to ascend above 3000 m should be referred for consultation with a physician with special expertise in high-altitude physiology and medicine.
Proper specialized counseling in high-altitude medicine can prevent life-threatening altitude-related diseases.
Further Information On Cme. This article has been certified by the North Rhine Academy for Postgraduate and Continuing Medical Education.
Deutsches Ärzteblatt provides certified continuing medical education (CME) in accordance with the requirements of the Medical Associations of the German federal states (Länder). CME points of the Medical Associations can be acquired only through the Internet, not by mail or fax, by the use of the German version of the CME questionnaire within 6 weeks of publication of the article. See the following website: cme.aerzteblatt.de
Participants in the CME program can manage their CME points with their 15-digit “uniform CME number” (einheitliche Fortbildungsnummer, EFN). The EFN must be entered in the appropriate field in the cme.aerzteblatt.de website under “meine Daten” (“my data”), or upon registration. The EFN appears on each participant’s CME certificate.
The solutions to the following questions will be published in issue 5/2012.
The CME unit “Vaccination Recommendations for Germany” (issue 45/2011) can be accessed until 23 December 2011.
For issue 1–2/2012, we plan to offer the topic “The Differential Diagnosis and Treatment of Normal-Pressure Hydrocephalus.”
Solutions to the CME questionnaire in issue 41/2011:
Meye, H-J, Wilke H: Treatment Strategies in Gastric Cancer.
Solutions: 1a, 2b, 3c, 4a, 5b, 6c, 7e, 8e, 9c, 10c
Please answer the following questions to participate in our certified Continuing Medical Education program. Only one answer is possible per question. Please select the answer that is most appropriate.
Question 1
At high altitudes, what reaction is induced by peripheral chemoreceptors?
Syncope
Fall in blood pressure
Increased ventilation
Hypoperfusion syndrome
Bronchiectasis
Question 2
As recommended by an expert committee, how is the expression “high altitude” defined in the classification of altitude levels?
Between 0 and 500 m
Above 500 m, below 2000 m
Above 2000 m, below 3000 m
Above 3000 m, below 5500 m
Above 5500 m
Question 3
Which of the following is a characteristic symptom of high-altitude pulmonary edema?
Dyspnea
Anorexia
Peripheral edema
Chronic obstructive bronchitis
Somnolence
Question 4
What is the characteristic symptom of acute mountain sickness?
Cardiovascular disturbances
Hypotension
Diarrhea
Vomiting
Headache
Question 5
You are the physician accompanying a trekking expedition in the Himalayas. You have been at an altitude of 5300 m for the last 48 hours. After a resting period at this altitude, a trained mountain-climber in your group who had symptoms of acute mountain sickness on earlier expeditions in the Alps is unable to walk or even to sit up straight; when he tries, his upper body sways to and fro. What do you consider the most likely diagnosis?
Acute exhaustion
Advanced dehydration
High-altitude cerebral edema
High-altitude pulmonary edema
Lumbago
Question 6
What is the best way to prevent altitude sicknesses on expeditions with planned ascents above 4000 m?
Training in a low-pressure chamber
Hypoxia training in a specialized fitness studio
Sprint training on the side of a cliff
Ascent over several days
A week-long hiking tour in the mountains of the Black Forest
Question 7
What medication should be given to prevent acute mountain sickness if the patient cannot tolerate acetazolamide?
Dexamethasone
Ibuprofen
Acetylsalicylic acid
Diphenhydramine
Betahistine
Question 8
Your patient, an active and athletic skier who sustained a myocardial infarction 2 months ago, would like to go skiing next week in a winter resort that is situated above 2300 m. What do you advise him to do?
Undertake this trip under medical supervision.
Pack prophylactic medications against acute mountain sickness in his suitcase.
Take a vacation in a warm area instead, because the risk of infection is higher in the cold.
Go there but do not ski, because the danger of injury is too great.
Go skiing at a different resort below 2000 m instead.
Question 9
Which of the following steps should be taken urgently at the first sign of high-altitude pulmonary or cerebral edema?
A day of rest
Administration of nifedipine
Administration of sildenafil
Immediate descent
Administration of acetazolamide
Question 10
Which of the following is often found in survivors of high-altitude cerebral edema?
Microhemorrhages in the corpus callosum
Lesions in the hypothalamus
Microaneurysms in the frontal cortex
Hyperintense periventricular white-matter lesions, mainly in the temporal, occipital, and parietal lobes
Symmetrical parietal lesions
Acknowledgments
Translated from the original German by Ethan Taub, MD.
Footnotes
Dr. Schommer states that he has no conflict of interest.
Prof. Bärtsch has received lecture honoraria from the Boehringer Ingelheim and MSD companies, as well as financial support for research projects from Geratherm, Actelion, Lilly, Boehringer Ingelheim, and Viasys.
References
- 1.Smith CA, Bisgard GE, Nielsen AM, Daristotle L, Kressin NA, Forster HV, et al. Carotid bodies are required for ventilatory acclimatization to chronic hypoxia. J Appl Physiol. 1986;60:1003–1010. doi: 10.1152/jappl.1986.60.3.1003. [DOI] [PubMed] [Google Scholar]
- 2.Heistad DD, Abboud FM. Dickinson W. Richards Lecture: Circulatory adjustments to hypoxia. Circulation. 1980;61:463–470. doi: 10.1161/01.cir.61.3.463. [DOI] [PubMed] [Google Scholar]
- 3.Bartsch P, Saltin B. General introduction to altitude adaptation and mountain sickness. Scand J Med Sci Sports. 2008;18(Suppl 1):1–10. doi: 10.1111/j.1600-0838.2008.00827.x. [DOI] [PubMed] [Google Scholar]
- 4.Bartsch P, Gibbs JS. Effect of altitude on the heart and the lungs. Circulation. 2007;116:2191–2202. doi: 10.1161/CIRCULATIONAHA.106.650796. [DOI] [PubMed] [Google Scholar]
- 5.Schneider M, Bernasch D, Weymann J, Holle R, Bartsch P. Acute mountain sickness: influence of susceptibility, preexposure, and ascent rate. Med Sci Sports Exerc. 2002;34:1886–1891. doi: 10.1097/00005768-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Hackett PH, Roach RC. High-altitude illness. N Engl J Med. 2001;345:107–114. doi: 10.1056/NEJM200107123450206. [DOI] [PubMed] [Google Scholar]
- 7.Bartsch P, Bailey DM, Berger MM, Knauth M, Baumgartner RW. Acute mountain sickness: controversies and advances. High Alt Med Biol. 2004;5:110–124. doi: 10.1089/1527029041352108. [DOI] [PubMed] [Google Scholar]
- 8.Kallenberg K, Bailey DM, Christ S, Mohr A, Roukens R, Menold E, et al. Magnetic resonance imaging evidence of cytotoxic cerebral edema in acute mountain sickness. J Cereb Blood Flow Metab. 2007;27:1064–1071. doi: 10.1038/sj.jcbfm.9600404. [DOI] [PubMed] [Google Scholar]
- 9.Hackett PH, Roach RC. High altitude cerebral edema. High Alt Med Biol. 2004;5:136–146. doi: 10.1089/1527029041352054. [DOI] [PubMed] [Google Scholar]
- 10.Wilson MH, Newman S, Imray CH. The cerebral effects of ascent to high altitudes. Lancet Neurol. 2009;8:175–191. doi: 10.1016/S1474-4422(09)70014-6. [DOI] [PubMed] [Google Scholar]
- 11.Kallenberg K, Dehnert C, Dorfler A, Schellinger PD, Bailey DM, Knauth M, et al. Microhemorrhages in nonfatal high-altitude cerebral edema. J Cereb Blood Flow Metab. 2008;28:1635–1642. doi: 10.1038/jcbfm.2008.55. [DOI] [PubMed] [Google Scholar]
- 12.Bartsch P, Mairbaurl H, Maggiorini M, Swenson ER. Physiological aspects of high-altitude pulmonary edema. J Appl Physiol. 2005;98:1101–1110. doi: 10.1152/japplphysiol.01167.2004. [DOI] [PubMed] [Google Scholar]
- 13.Dehnert C, Berger MM, Mairbaurl H, Bartsch P. High altitude pulmonary edema: a pressure-induced leak. Respir Physiol Neurobiol. 2007;158:266–273. doi: 10.1016/j.resp.2007.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Schommer K, Wiesegart N, Menold E, Haas U, Lahr K, Buhl H, et al. Training in normobaric hypoxia and its effects on acute mountain sickness after rapid ascent to 4559 m. High Alt Med Biol. 2010;11:19–25. doi: 10.1089/ham.2009.1019. [DOI] [PubMed] [Google Scholar]
- 15.Hackett PH, Rennie D, Levine HD. The incidence, importance, and prophylaxis of acute mountain sickness. Lancet. 1976;2:1149–1155. doi: 10.1016/s0140-6736(76)91677-9. [DOI] [PubMed] [Google Scholar]
- 16.Forwand SA, Landowne M, Follansbee JN, Hansen JE. Effect of acetazolamide on acute mountain sickness. N Engl J Med. 1968;279:839–845. doi: 10.1056/NEJM196810172791601. [DOI] [PubMed] [Google Scholar]
- 17.Bartsch P, Maggiorini M, Ritter M, Noti C, Vock P, Oelz O. Prevention of high-altitude pulmonary edema by nifedipine. N Engl J Med. 1991;325:1284–1289. doi: 10.1056/NEJM199110313251805. [DOI] [PubMed] [Google Scholar]
- 18.Maggiorini M, Brunner-La Rocca HP, Peth S, Fischler M, Bohm T, Bernheim A, et al. Both tadalafil and dexamethasone may re-duce the incidence of high-altitude pulmonary edema: a randomized trial. Ann Intern Med. 2006;145:497–506. doi: 10.7326/0003-4819-145-7-200610030-00007. [DOI] [PubMed] [Google Scholar]
- 19.Bartsch P, Merki B, Hofstetter D, Maggiorini M, Kayser B, Oelz O. Treatment of acute mountain sickness by simulated descent: a randomised controlled trial. BMJ. 1993;306:1098–1101. doi: 10.1136/bmj.306.6885.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ferrazzini G, Maggiorini M, Kriemler S, Bartsch P, Oelz O. Successful treatment of acute mountain sickness with dexamethasone. Br Med J (Clin Res Ed) 1987;294:1380–1382. doi: 10.1136/bmj.294.6584.1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Luks AM, Swenson ER. Travel to high altitude with pre-existing lung disease. Eur Respir J. 2007;29:770–792. doi: 10.1183/09031936.00052606. [DOI] [PubMed] [Google Scholar]
- 22.Rimoldi SF, Sartori C, Seiler C, Delacretaz E, Mattle HP, Scherrer U, et al. High-altitude exposure in patients with cardiovascular disease: risk assessment and practical recommendations. Prog Cardiovasc Dis. 2010;52:512–524. doi: 10.1016/j.pcad.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 23.Dehnert C, Bartsch P. Can patients with coronary heart disease go to high altitude? High Alt Med Biol. 2010;11:183–188. doi: 10.1089/ham.2010.1024. [DOI] [PubMed] [Google Scholar]
- 24.Bärtsch P, Grünig E, Hohenhaus E, Dehnert C. Beurteilung der Höhentauglichkeit beim Gesunden. Deutsche Zeitschrift für Sportmedizin. 2000;50:401–406. [Google Scholar]
- 25.Oelz O, Maggiorini M, Ritter M, Waber U, Jenni R, Vock P, et al. Nifedipine for high altitude pulmonary oedema. Lancet. 1989;2:1241–1244. doi: 10.1016/s0140-6736(89)91851-5. [DOI] [PubMed] [Google Scholar]
- e1.Bender PR, McCullough RE, McCullough RG, Huang SY, Wagner PD, Cymerman A, et al. Increased exercise SaO2 independent of ventilatory acclimatization at 4,300 m. J Appl Physiol. 1989;66:2733–2738. doi: 10.1152/jappl.1989.66.6.2733. [DOI] [PubMed] [Google Scholar]
- e2.Grover RF, Bärtsch P. Blood: High altitude - an exploration of human adaptation. In: Hornbein TF, Schoene RB, editors. New York: Marcel Dekker Inc.; 2001. pp. 493–523. [Google Scholar]
- e3.Lundby C, Calbet JA, van Hall G, Saltin B, Sander M. Pulmonary gas exchange at maximal exercise in Danish lowlanders during 8 wk of acclimatization to 4,100 m and in high-altitude Aymara natives. Am J Physiol Regul Integr Comp Physiol. 2004;287:R1202–R1208. doi: 10.1152/ajpregu.00725.2003. [DOI] [PubMed] [Google Scholar]
- e4.Calbet JA, Boushel R, Radegran G, Sondergaard H, Wagner PD, Saltin B. Why is VO2 max after altitude acclimatization still reduced despite normalization of arterial O2 content? Am J Physiol Regul Integr Comp Physiol. 2003;284:R304–R316. doi: 10.1152/ajpregu.00156.2002. [DOI] [PubMed] [Google Scholar]
- e5.Hansen J, Sander M. Sympathetic neural overactivity in healthy humans after prolonged exposure to hypobaric hypoxia. J Physiol. 2003;546:921–929. doi: 10.1113/jphysiol.2002.031765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e6.Reeves JT, Mazzeo RS, Wolfel EE, Young AJ. Increased arterial pressure after acclimatization to 4300 m: possible role of norepinephrine. Int J Sports Med. 1992;13(Suppl 1):S18–821. doi: 10.1055/s-2007-1024581. [DOI] [PubMed] [Google Scholar]
- e7.Maggiorini M, Buhler B, Walter M, Oelz O. Prevalence of acute mountain sickness in the Swiss Alps. BMJ. 1990;301:853–855. doi: 10.1136/bmj.301.6756.853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e8.Honigman B, Theis MK, Koziol-McLain J, Roach R, Yip R, Houston C, et al. Acute mountain sickness in a general tourist population at moderate altitudes. Ann Intern Med. 1993;118:587–592. doi: 10.7326/0003-4819-118-8-199304150-00003. [DOI] [PubMed] [Google Scholar]
- e9.Montgomery AB, Mills J, Luce JM. Incidence of acute mountain sickness at intermediate altitude. JAMA. 1989;261:732–734. [PubMed] [Google Scholar]
- e10.Roach RC, Maes D, Sandoval D, Robergs RA, Icenogle M, Hinghofer-Szalkay H, et al. Exercise exacerbates acute mountain sickness at simulated high altitude. J Appl Physiol. 2000;88:581–585. doi: 10.1152/jappl.2000.88.2.581. [DOI] [PubMed] [Google Scholar]
- e11.Bartsch P, Swenson ER, Paul A, Julg B, Hohenhaus E. Hypoxic ventilatory response, ventilation, gas exchange, and fluid balance in acute mountain sickness. High Alt Med Biol. 2002;3:361–376. doi: 10.1089/15270290260512846. [DOI] [PubMed] [Google Scholar]
- e12.Sanchez del Rio M, Moskowitz MA. High altitude headache - Lessons from headaches at sea level. In: Roach RC, Wagner PD, Hackett PH, editors. Hypoxia: Into the Next Millenium. New York: Kluwer Academic/Plenum Publishers; 1999. pp. 145–153. [PubMed] [Google Scholar]
- e13.Bailey DM, Bartsch P, Knauth M, Baumgartner RW. Emerging concepts in acute mountain sickness and high-altitude cerebral edema: from the molecular to the morphological. Cell Mol Life Sci. 2009;66:3583–3594. doi: 10.1007/s00018-009-0145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e14.Fischer R, Vollmar C, Thiere M, Born C, Leitl M, Pfluger T, et al. No evidence of cerebral oedema in severe acute mountain sickness. Cephalalgia. 2004;24:66–71. doi: 10.1111/j.1468-2982.2004.00619.x. [DOI] [PubMed] [Google Scholar]
- e15.Schoonman GG, Sandor PS, Nirkko AC, Lange T, Jaermann T, Dydak U, et al. Hypoxia-induced acute mountain sickness is associated with intracellular cerebral edema: a 3 T magnetic reso-nance imaging study. J Cereb Blood Flow Metab. 2008;28:198–206. doi: 10.1038/sj.jcbfm.9600513. [DOI] [PubMed] [Google Scholar]
- e16.Bartsch P. High altitude pulmonary edema. Med Sci Sports Exerc. 1999;31:S23–S27. doi: 10.1097/00005768-199901001-00004. [DOI] [PubMed] [Google Scholar]
- e17.Bartsch P, Maggiorini M, Mairbaurl H, Vock P, Swenson ER. Pulmonary extravascular fluid accumulation in climbers. Lancet. 2002;360:571–572. doi: 10.1016/S0140-6736(02)09723-4. 571; author reply. [DOI] [PubMed] [Google Scholar]
- e18.Hackett PH, Creagh CE, Grover RF, Honigman B, Houston CS, Reeves JT, et al. High-altitude pulmonary edema in persons without the right pulmonary artery. N Engl J Med. 1980;302:1070–1073. doi: 10.1056/NEJM198005083021907. [DOI] [PubMed] [Google Scholar]
- e19.Larson EB, Roach RC, Schoene RB, Hornbein TF. Acute mountain sickness and acetazolamide. Clinical efficacy and effect on ventilation. JAMA. 1982;248:328–332. [PubMed] [Google Scholar]
- e20.Dumont L, Mardirosoff C, Tramer MR. Efficacy and harm of pharmacological prevention of acute mountain sickness: quantitative systematic review. BMJ. 2000;321:267–272. doi: 10.1136/bmj.321.7256.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e21.Sutton JR, Houston CS, Mansell AL, McFadden MD, Hackett PM, Rigg JR, et al. Effect of acetazolamide on hypoxemia during sleep at high altitude. N Engl J Med. 1979;301:1329–1331. doi: 10.1056/NEJM197912133012406. [DOI] [PubMed] [Google Scholar]
- e22.Birmingham Medical Research Expeditionary Society Mountain Sickness Study Group. Acetazolamide in control of acute mountain sickness. Lancet. 1981;1:180–183. [PubMed] [Google Scholar]
- e23.Johnson TS, Rock PB, Fulco CS, Trad LA, Spark RF, Maher JT. Prevention of acute mountain sickness by dexamethasone. N Engl J Med. 1984;310:683–686. doi: 10.1056/NEJM198403153101103. [DOI] [PubMed] [Google Scholar]
- e24.Montgomery AB, Luce JM, Michael P, Mills J. Effects of dexamethasone on the incidence of acute mountain sickness at two intermediate altitudes. JAMA. 1989;261:734–736. [PubMed] [Google Scholar]
- e25.Bärtsch P, Vock P, Franciolli M. High altitude pulmonary edema after successful treatment of acute mountain sickness with dexamthasone. J Wild Med. 1990;1:162–164. [Google Scholar]
- e26.Naeije R, Melot C. Acute pulmonary oedema on the Ruwenzori mountain range. Br Heart J. 1990;64:400–402. doi: 10.1136/hrt.64.6.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e27.Okin JT. Response of patients with coronary heart disease to exercise at varying altitudes. Adv Cardiology. 1970;5:92–96. [Google Scholar]
- e28.Khanna PK, Dham SK, Hoon RS. Exercise in an hypoxic environment as a screening test for ischaemic heart disease. Aviat Space Environ Med. 1976;47:1114–1117. [PubMed] [Google Scholar]
- e29.Grover RF, Tucker CE, McGroarty SR, Travis RR. The coronary stress of skiing at high altitude. Arch Intern Med. 1990;150:1205–1208. [PubMed] [Google Scholar]
- e30.Morgan BJ, Alexander JK, Nicoli SA, Brammell HL. The patient with coronary heart disease at altitude: observations during acute exposure to 3100 meters. J Wild Med. 1990;1:147–153. [Google Scholar]
- e31.Roach RC, Houston CS, Honigman B, Nicholas RA, Yaron M, Grissom CK, et al. How well do older persons tolerate moderate altitude? West J Med. 1995;162:32–36. [PMC free article] [PubMed] [Google Scholar]
- e32.Levine BD, Zuckerman JH, deFilippi CR. Effect of high-altitude exposure in the elderly: the Tenth Mountain Division study. Circulation. 1997;96:1224–1232. doi: 10.1161/01.cir.96.4.1224. [DOI] [PubMed] [Google Scholar]
- e33.Erdmann J, Sun KT, Masar P, Niederhauser H. Effects of exposure to altitude on men with coronary artery disease and impaired left ventricular function. Am J Cardiol. 1998;81:266–270. doi: 10.1016/s0002-9149(97)00901-6. [DOI] [PubMed] [Google Scholar]
- e34.Agostoni P, Cattadori G, Guazzi M, Bussotti M, Conca C, Lomanto M, et al. Effects of simulated altitude-induced hypoxia on exercise capacity in patients with chronic heart failure. Am J Med. 2000;109:450–455. doi: 10.1016/s0002-9343(00)00532-5. [DOI] [PubMed] [Google Scholar]
- e35.Wyss CA, Koepfli P, Fretz G, Seebauer M, Schirlo C, Kaufmann PA. Influence of altitude exposure on coronary flow reserve. Circulation. 2003;108:1202–1207. doi: 10.1161/01.CIR.0000087432.63671.2E. [DOI] [PubMed] [Google Scholar]
- e36.Schmid JP, Noveanu M, Gaillet R, Hellige G, Wahl A, Saner H. Safety and exercise tolerance of acute high altitude exposure (3454 m) among patients with coronary artery disease. Heart. 2006;92:921–925. doi: 10.1136/hrt.2005.072520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e37.Burtscher M, Mittleman MA. Time-dependent SCD risk during mountain sports changes with age. Circulation. 1995;92:3151–3152. [PubMed] [Google Scholar]
- e38.Burtscher M, Philadelphy M, Nachbauer W, Likar R. The risk of death to trekkers and hikers in the mountains. JAMA. 1995;273 doi: 10.1001/jama.1995.03520300030031. [DOI] [PubMed] [Google Scholar]
- e39.Burtscher M, Pachinger O, Mittleman MA, Ulmer H. Prior myocardial infarction is the major risk factor associated with sudden cardiac death during downhill skiing. Int J Sports Med. 2000;21:613–615. doi: 10.1055/s-2000-8481. [DOI] [PubMed] [Google Scholar]
- e40.Arbab-Zadeh A, Levine BD, Trost JC, Lange RA, Keeley EC, Hillis LD, et al. The effect of acute hypoxemia on coronary arterial dimensions in patients with coronary artery disease. Cardiology. 2009;113:149–154. doi: 10.1159/000186695. [DOI] [PubMed] [Google Scholar]
- e41.Burtscher M, Philadelphy M, Likar R. Sudden cardiac death during mountain hiking and downhill skiing. N Engl J Med. 1993;329:1738–1739. doi: 10.1056/NEJM199312023292315. [DOI] [PubMed] [Google Scholar]
- e42.Huismans HK, Douma WR, Kerstjens HA, Renkema TE. Asthma in patients climbing to high and extreme altitudes in the Tibetan Everest region. J Asthma. 2010;47:614–619. doi: 10.3109/02770900903573277. [DOI] [PubMed] [Google Scholar]
- e43.Graham WG, Houston CS. Short-term adaptation to moderate altitude. Patients with chronic obstructive pulmonary disease. JAMA. 1978;240:1491–1494. [PubMed] [Google Scholar]
- e44.Dillard TA, Beninati WA, Berg BW. Air travel in patients with chronic obstructive pulmonary disease. Arch Intern Med. 1991;151:1793–1795. [PubMed] [Google Scholar]
- e45.Golan Y, Onn A, Villa Y, Avidor Y, Kivity S, Berger SA, et al. Asthma in adventure travelers: a prospective study evaluating the occurrence and risk factors for acute exacerbations. Arch Intern Med. 2002;162:2421–2426. doi: 10.1001/archinte.162.21.2421. [DOI] [PubMed] [Google Scholar]
- e46.Louie D, Pare PD. Physiological changes at altitude in nonasthmatic and asthmatic subjects. Can Respir J. 2004;11:197–199. doi: 10.1155/2004/734760. [DOI] [PubMed] [Google Scholar]
- e47.Cogo A, Basnyat B, Legnani D, Allegra L. Bronchial asthma and airway hyperresponsiveness at high altitude. Respiration. 1997;64:444–449. doi: 10.1159/000196721. [DOI] [PubMed] [Google Scholar]
- e48.Allegra L, Cogo A, Legnani D, Diano PL, Fasano V, Negretto GG. High altitude exposure reduces bronchial responsiveness to hypo-osmolar aerosol in lowland asthmatics. Eur Respir J. 1995;8:1842–1846. doi: 10.1183/09031936.95.08111842. [DOI] [PubMed] [Google Scholar]
- e49.Matthys H, Ernst HH, Volz E, Konietzko N. Hemodynamic and ventilatory changes in patients with obstructive airway disease ex-posed to a simulated altitude of 2,500 m. Prog Resp Res. 1975;9:187–194. [Google Scholar]
- e50.Richalet JP, Keromes A, Dersch B, Corizzi F, Mehdioui H, Pophillat B. Caractéristiques physiologiques des alpinistes de haute altitude. Sci Sports. 1988;3:89–108. [Google Scholar]
- e51.Pesce C, Leal C, Pinto H, Gonzalez G, Maggiorini M, Schneider M, et al. Determinants of acute mountain sickness and success on Mount Aconcagua (6962 m) High Alt Med Biol. 2005;6:158–166. doi: 10.1089/ham.2005.6.158. [DOI] [PubMed] [Google Scholar]
- e52.Burtscher M, Flatz M, Faulhaber M. Prediction of susceptibility to acute mountain sickness by SaO2 values during short-term exposure to hypoxia. High Alt Med Biol. 2004;5:335–340. doi: 10.1089/ham.2004.5.335. [DOI] [PubMed] [Google Scholar]
- e53.Hohenhaus E, Paul A, McCullough RE, Kucherer H, Bartsch P. Ventilatory and pulmonary vascular response to hypoxia and susceptibility to high altitude pulmonary oedema. Eur Respir J. 1995;8:1825–1833. doi: 10.1183/09031936.95.08111825. [DOI] [PubMed] [Google Scholar]