Summary
The sirtuin (the mammalian homolog of silent information regulation 2 of yeast S.cerevisiae) 1 (SIRT1), a NAD-dependent histone deacetylase, has emerged as a critical regulator in response to oxidative stress. Through antagonism of oxidative stress-induced cell injury and through the maintenance of metabolic homeostasis in the body, SIRT1 can block vascular system injury. SIRT1 targets multiple cellular proteins, such as peroxisome proliferators-activated receptor-γ (PPAR-γ) and its coactivator-1α (PGC-1α), forkhead transcriptional factors, AMP-activated protein kinase (AMPK), nuclear factor-κB (NF-κB), and protein tyrosine phosphatase (PTP) to modulate intricate cellular pathways of multiple diseases. In the cardiovascular system, activation of SIRT1 can not only protect at the cellular level against oxidative stress, but also offer increased survival at the systemic level to limit coronary heart disease and cerebrovascular disease. Future knowledge of SIRT1 and its novel pathways can open new directions for the treatment of cardiovascular disease as well as offer the potential to limit disability from several related disorders.
Keywords: AMP-activated protein kinase (AMPK); cardiovascular disease; Forkhead transcription factor; nuclear factor-κB; oxidative stress, peroxisome proliferators-activated receptor-γ coactivator-1α (PGC-1α); protein tyrosine phosphatase; resveratrol, sirtuins
Introduction
SIRT1 is the closest homologue of the yeast (Saccharomyces cerevisiae) silent information regulator-2 (Sir2), a nicotinamide adenine dinucleotide (NAD+) -dependent protein deacetylase. In mammals, seven members of the Sir2 homologues have been found and identified as SIRT1-7. SIRT1 has been the most extensively investigated sirtuin [1]. Sirtuins are also named as class III histone deacetylases, which are NAD+ dependent protein deacetylases. In the deacetylase reaction, SIRT1 transfers the acetyl residue from the acetyllysine residue of histone to the ADP-ribose moiety of NAD+, resulting in the production of nicotinamide, 2′-O-acetyl ADP ribose, and deacetylated proteins. SIRT1 consumes one NAD+ to transfer one acetyl residue and activation of SIRT1 therefore decreases the ratio of NAD+/NADH. The decreased NAD+/NADH ratio as well as nicotinamide production can inhibit SIRT1 activity [2].
SIRT1 expressed in all organs of the body including the brain, heart, liver, pancreas, skeletal muscle, spleen, and adipose tissues and it exists in both the nucleus and cytoplasm with dominant expression in the nucleus. In cardiomyocytes, SIRT1 is primarily localized in the nucleus during embryonic period, but in myocytes of adult heart of rodents, SIRT1 is dominantly expressed in the cytoplasm [3]. Under pathological conditions, SIRT1 shuttles between the nucleus and the cytoplasm to modulate some cell signaling and the outcome of stress insults [4, 5].
SIRT1 mediated deaceylation has significant impact on the activity of many proteins, resulting in the regulation of a number of proteins and their translation which play important roles in the biological process including oxidative stress, metabolism, cell proliferation, and genomic stability. Recently, the role of SIRT1 under normal physiological conditions as well as during disease states have drawn great interest in the research community. SIRT1 has been linked to aging, metabolic diseases, neurodegenerative diseases, cancer, and cardiovascular dysfunction [6]. In this paper, we will discus the biological activity of SIRT1 and potential implications in cardiovascular disease.
SIRT1 cell signaling pathways
SIRT1 impacts upon the biological activity of a number of proteins through regulating their deacetylation or through non-deacetylating reactions. The targets of SIRT1 that have been identified include peroxisome proliferators-activated receptor-γ (PPAR-γ and its coactivator-1α (PGC-1α)), forkhead transcriptional factors, serine threonine liver kinase B1 (LKB1), nuclear factor-κB (NF-κB), and protein tyrosine phosphatase (PTP). Through regulating multiple cell signaling pathways, SIRT1 increases the resistance of cells to oxidative stress and thereby plays an important role in blocking the development of many disease entities.
SIRT1 and oxidative stress
When excessive generation of oxygen free radicals and other chemical species override the ability of the endogenous antioxidant system, oxidative stress ensues. Under physiological conditions, a low level of reactive oxygen species is produced and is scavenged by endogenous antioxidant systems that include superoxide dismutase (SOD), glutathione peroxidase, catalase, and small molecule substances such as vitamins C and E [7]. Oxygen free radicals, consisting of superoxide free radicals, hydrogen peroxide, singlet oxygen, nitric oxide, and peroxynitrite, can be generated in elevated quantities during the reduction of oxygen and lead to cell injury [8, 9].
Oxidative stress has been recognized as a significant contributor to cellular injury. Oxygen free radicals can result in the cellular membrane lipid peroxidation and protein oxidation leading to the disruption of cellular integrity [10, 11]. Oxidative stress plays a significant role in the pathology of numerous disease processes that can include metabolic disorders [12, 13], cognitive impairment [14, 15], cardiopulmonary and hepatic disease [16], degenerative disorders and psychiatric disorders [17, 18], and infertility [19, 20]. In addition, oxidative stress results in apoptosis that is an important mechanism that leads to the destruction of cells in many cell systems. Apoptosis consists of both the early exposure of membrane phosphatidylserine (PS) residues and the later destruction of genomic DNA [21, 22]. Apoptotic membrane PS exposure occurs in neurons, endothelial cells, and inflammatory microglia during conditions such as low oxygen levels [23] and β-amyloid (Aβ) exposure [24, 25]. In addition, membrane PS externalization also occurs on platelets and has been associated with clot formation in the vascular system [26]. Membrane PS exposure also can become a signal for the phagocytosis of cells. The loss of membrane phospholipid asymmetry leads to the exposure of membrane PS residues on the cell surface and attracts microglia to target cells for phagocytosis [27-29].
Oxidative stress has been closely implicated in cardiovascular diseases [30]. Disorders such as coronary heart disease, chronic heart failure [31], myocardial ischemia [32], atherosclerosis, and hypertension [33] are, at least in part, tied to oxidative stress. Since oxidative injury contributes also to the progressive development of many cardiovascular diseases, targeting oxidative stress may represent one of promising therapeutic strategies for their treatment.
SIRT1 activation has been found to protect cell survival against oxidative stress in diverse cell populations. In response to DNA damage, SIRT1 can negatively regulate p53-induced apoptosis [34]. Further work indicates that SIRT1 prevents oxidative stress induced apoptosis in mesangial cells and cardiomyocytes through p53 deacetylation and induction of manganese superoxide dismutase (MnSOD) [3, 35]. Increased activity of SIRT1 results in the cellular resistance to oxidative stress via modulation of FoxO transcription factors [36]. In renal tubular cells, SIRT1 protects cells against oxidative stress induced apoptosis via improving the activity of catalase [37]. SIRT1 overexpression enhances the tolerance against nitric oxide toxicity in neuronal cells [38, 39]. Resveratrol (trans-3,5,4′-trihydroxystibene), a naturally occurring phytoalexin, is the best-characterized compound that modulates SIRT1 activity. Application of the SIRT1 activator resveratrol prevents apoptotic injury in cerebral microvascular endothelial cells (ECs) during models of experimental diabetes with elevated glucose [4, 5]. These investigations suggest that SIRT1 activity may be a necessary component for cell protection during oxidative stress and that SIRT1 activity is a novel target for therapeutic strategies against diseases that are associated with oxidative stress [40].
SIRT1, PPAR-γ, and PGC-1α
PPAR-γ plays an important role in adipogenesis. PPAR-α increases free fatty acid uptake and decreases lipolysis. Under nutrient restriction, SIRT1 protein binds to and represses genes controlled by the fat regulator PPAR-γ. SIRT1 inhibits PPAR-γ by docking with its cofactors nuclear receptor co-repressor and silencing mediator of retinoid and thyroid hormone receptors, resulting in the mobilization of fatty acids from white adipocytes upon fasting [41]. Yet, PPAR-γ may directly interact with SIRT1 and form a negative feedback to regulate SIRT1 activity [42].
PGC-1α is a member of a family of transcriptional coactivators that includes PGC-1α, PGC-1β and PGC-1 related coactivator (PRC). PGC-1α interacts with transcription factors to activate transcription and increases the expression of genes that regulate mitochondrial functions and fatty acid oxidation [43]. As a result, enhanced PGC-1α activity may function to protect against some metabolic diseases and improve mitochondrial biogenesis. Interestingly, PGC-1α can prevent accumulation of reactive oxygen species in endothelial cells and protect cells against apoptotic injury [44]. Yet, increased expression of PGC-1α seems to increase the sensitivity of cardiomyocytes to anoxia/reoxygenation induced cell death through upregulation of adenine nucleotide translocase 1 [45]. Overexpression of PGC-1α in the hearts of adult mice also leads to cardiomyopathy [46], suggesting that PGC-1α levels in the heart need to be tightly regulated to prevent cardiovascular injury [47].
SIRT1 regulates the activity of PGC-1α via deacetylation and it can interact with PGC-1α in the liver to induce gluconeogenic genes and hepatic glucose output. SIRT1 also can modulate the PGC-1α repressing effect on glycolytic genes in response to fasting and pyruvate [48]. Hepatic SIRT1 interacts with peroxisome proliferators-activator-α (PPARα) through activating PGC-1α to mediate lipid homeostasis and an adaptive response to fasting. SIRT1 deletion in the liver results in the loss of PGC-1α activity and the impairment of fatty acid oxidation, predisposing to develop hepatic steatosis when fed with a high-fat diet [49].
SIRT1 and forkhead transcriptional factors
SIRT1 regulates cellular stress through modulating FoxO nuclear shuttling and transcriptional activity. Mammalian forkhead transcription factors of the O class (FoxO1, FoxO3, FoxO4, and FoxO6) are involved in cell metabolism, insulin sensitivity, aging, and oxidative stress [50, 51]. Phosphorylation of FoxOs results in their retention in the cytoplasm and inhibition of their transcription activity [52, 53]. Acetylation of FoxOs can also modulate their transcriptional activity through facilitating their phosphorylation and nuclear translocation [25, 29, 54]. Nuclear localization of FOXO is induced by deacetylation [55] and is inhibited by phosphorylation.
In response to oxidative stress, FoxOs translocate to the nucleus, interact with SIRT1, and result in the deacetylation of FoxOs. SIRT1 can deacetylate FoxO3 and form a complex with FoxO3 in cells in response to oxidative stress. Interestingly, SIRT1 has a dual effect on FoxO3 function: SIRT1 enhances the ability of FoxO3 to induce cell cycle arrest and to increase resistance to oxidative stress, but impairs the ability of FoxO3 to induce cell death [56, 57]. SIRT1 also can bind to and deacetylate FoxO4 in an NAD-dependent manner, and thereby increase its transcription activity in response to oxidative stress [58]. In contrast, loss of SIRT1 results in the impairment of FoxO4 nuclear translocation and the growth arrest and DNA damage (GADD45) expression [59], suggesting that SIRT1 modulates FoxO function via NAD-dependent deacetylation in response to oxidative stress. SIRT1 can target FOXO1 to bind and deacetylate FOXO1 at residues that are acetylated by cAMP-response element-binding protein [60]. In addition, overexpression of SIRT1 protects cardiomyocytes from oxidative stress through a FoxO1-dependent pathway [61]. It should be noted that SIRT1 enhances expression of FoxO targets that is involved in stress resistance (MnSOD, GADD45) but diminishes the expression of pro-apoptotic FoxO targets (Fas ligand and Bim), suggesting that SIRT1 may modulate the balance between stress resistance and cell death within cells [51, 57].
Deacetylation of FoxOs by SIRT1 also can regulate autophagy. SIRT1 mediated deacetylation of FoxO1 has been associated with increases in autophagic flux which may be required to maintain cardiac function during glucose deprivation and starvation [62]. FoxO1 also increases the expression of Rab7, a small GTP-binding protein that mediates late autophagosome-lysosome fusion, which is both necessary and sufficient for mediating FoxO1-induced increases in autophagic process [62].
Given that SIRT1 deacetylates and activates FoxO transcriptional activity, in turn, FoxOs exert a positive feedback mechanism regulating SIRT1 expression. FoxO1 can directly bind to SIRT1 promoter region containing a cluster of five putative FoxO1 core binding repeat motifs (IRS-1) and a forkhead-like consensus-binding site (FKHD-L). This results in FoxO1 dependent SIRT1 transcription and leads to an increase in the expression of SIRT1 [63]. FoxO3a can also regulate the expression of SIRT1 through binding to two p53 binding sites within the SIRT1 promoter to induce SIRT1 transcription during acute nutrient withdrawal [64].
SIRT1 and AMPK
AMPK is another target for SIRT1 to regulate insulin sensitivity and metabolism. Low energy states with an increase in the AMP/ATP ratio result in the activation of AMPK. Activation of AMPK by phosphorylation functions to promote insulin sensitivity, fatty acid oxidation, and mitochondrial biogenesis, resulting in the generation of ATP and elimination of oxidative stress. Activation of AMPK has been associated with cardioprotection. Increased AMPK activation reduces myocardial infarct size in both non-diabetic and diabetic rat hearts following ischemia/reperfusion, which may be mediated through the inhibition of mitochondrial permeability transition pore opening in cardiomyocytes [65]. Mice expressing dominant negative AMPK or loss of AMPK have glucose uptake inhibition and increased infarct volume following cardiac ischemia [66].
SIRT1 regulates AMPK through the AMPK kinase, serine-threonine liver kinase B1 (LKB1). Overexpression of SIRT1 results in the deacetylation of LKB1, leading to its translocation from the nucleus to the cytoplasm, where LKB1 activates AMPK [67]. AMPK, in turn, can mediate the activation of SIRT1. AMPK mediated impairment of muscle differentiation during glucose restriction and PGC-1α-mediated gene expression is SIRT1 dependent, yet, AMPK can’t directly activate SIRT1, but may enhance SIRT1 activity though two indirect ways. AMPK activation enhances SIRT1 activity either by increasing cellular NAD+/NADH ratio, resulting in the deacetylation and modulation of the activity of downstream SIRT1 targets that include the PGC-1α, FoxO1, and FoxO3a [68] or by up-regulating nicotinamide phosphoribosyltransferase (Nampt) during glucose restriction, leading to increased NAD+ and decreased nicotinamide, an inhibitor of SIRT1 [69]. The SIRT1 activator resveratrol also has been demonstrated to activate AMPK through SIRT1 dependent or independent mechanisms [68, 70]. Resveratrol increases AMPK phosphorylation to protect cells against elevated glucose concentration, improve insulin sensitivity, and stimulate glucose transport.
SIRT1 and NF-κB
NF-κB has been identified as one of transcription factors that play an important role in the protection against oxidative stress [29, 71-73]. Once activated, NF-κB is translocated to the nucleus and activates several anti-apoptotic genes, such as the inhibitors of apoptotic protein (IAPs), Gadd45β, and Bcl-xL to prevent apoptosis against oxidative stress [74]. On the other hand, NF-κB nuclear translocation at times also can lead to pro-inflammatory genes that promote inflammation, cell death, and tumorigenesis [75, 76]. Treatment of cells with resveratrol potentiates chromatin-associated SIRT1 protein on the cIAP-2 promoter region and inhibits NF-κB regulated gene expression, leading to an increase in the sensitization of cells to tumor necrosis factor-α-induced apoptosis [77]. In contrast, activation of SIRT1 reduces amyloid-beta induced toxicity and decreases NF-κB transcriptional activity, suggesting that SIRT1 promotes cell protection through inhibiting NF-κB transcriptional activity [78]. Additional work suggests that SIRT1 can physically interact with and deacetylate the RelA/p65 subunit of NF-κB and inhibit its transcriptional activity [77].
In cardiac cells, nuclear factor NF-κB has been implicated in the regulation of cell survival in cardiac myocytes and can protect cardiomyocytes against hypoxia and reperfusion injury [79]. Activation of NF-κB has also been associated with cardiac ischemia preconditioning [80]. NF-κB inhibition also blocks left ventricle hypertrophy in IκB mutant male mice but not in female mice following low-gradient trans-aortic constriction. NF-κB inhibition dose not affect left ventricle remodeling, suggesting that NF-κB regulates stress induced cardiac hypertrophy in a gender specific manner [81].
SIRT1 and PTP
SIRT1 may regulate insulin sensitivity through targeting protein tyrosine phosphatase (PTP). Among PTPs, inhibition of PTP1B results in phosphorylation of endothelial nitric oxide synthase and Akt (protein kinase B), improving endothelial function during heart failure [82]. In addition, PTP1B has been identified to negatively regulate insulin signal transduction via targeting the insulin receptor. PTP1B deficiency or inhibition leads to improved insulin sensitivity and glycemic control. Lowering the PTP1B level in the liver decreases blood glucose in diabetic mice. SIRT1 overexpression or SIRT1 activation was found to reduce both the PTP1B mRNA and protein levels during insulin-resistance. In contrast, an increase in PTP1B expression prevented SIRT1 mediated glucose uptake and insulin receptor phosphorylation in response to insulin stimulation, suggesting that SIRT1 improves insulin sensitivity at least in part through repressing PTP1B [83].
SIRT1 and oncogenes
SIRT1 has been found to negatively regulate the tumor suppressor gene p53 through an NAD dependent deacetylating mechanism and therefore, SIRT1 has been considered as a tumorigenic factor [84]. However, some of the tumor suppressing functions of SIRT1 may override its tumor promoting effects.
SIRT1 also can interact with apoptotic transcriptional regulator E2F1 during cell cycle regulation and apoptosis [85]. E2F1 has recently been associated with cardiomyopathy [86] and, as a result, cardiomyocyte hypertrophy may be tied to SIRT1. As an important regulator in response to DNA damage induced stress, E2F1 can positively regulate SIRT1 expression at the transcriptional level. SIRT1 binds to E2F1 and deacetylates E2F1, resulting in the inhibition of E2F1 transcriptional activity.
In breast cancer, SIRT1 activation inhibits the expression of survivin, an apoptosis inhibitor. In human BRCA1 (breast cancer associated gene 1)-associated breast cancers, the level of SIRT1 is low. The decreased level of SIRT1 and high level of survivin also was observed in mammary tumors from BRCA1 mutant mice. Work has shown that BRCA1 binds to the SIRT1 promoter and increases SIRT1 expression. SIRT1 in turn negatively regulates survivin expression by changing the epigenetic modification of histone H3 [87].
Regulation of SIRT1 activation
Although the regulation of SIRT1 activation is not yet completely known, several cellular pathways have been identified under a variety of conditions. Calorie restriction, starvation, exercise, and oxidative stress have been identified as significant factors to increase SIRT1 expression. NAD+ serves as substrate of SIRT1. The level of NAD+ can also control the deacetylating activity of SIRT1. In the salvage pathway of NAD+ synthesis, nicotinamide phosphoribosyltransferase (NAMPT) catalyzes the conversion of nicotinamide to nicotinamide mononucleotide, which is then converted to NAD+ by nicotinamide/nicotinic acid mononucleotide adenylyltransferase (NMNAT). NAMPT is the rate-limiting enzyme in mammalian NAD+ biosynthesis pathway. Enhanced NAMPT activity increases the total cellular NAD level and subsequent transcriptional regulatory activity of SIRT1 in mouse fibroblasts [88]. NMNAT also can regulate the deacetylating activity SIRT1 at its target gene promoters [89].
As described in previous sections, there exist several feedback mechanisms that lead to the activation of SIRT1, such as SIRT1-FoxOs and SIRT1-AMPK interacting systems. In addition, HuR, a RNA binding protein, regulates the stability of many target mRNAs and can bind the 3′ non-translated region of the mRNA of SIRT1, leading to the stabilization of the SIRT1 mRNA and up-regulation of SIRT1 expression [90]. During oxidative stress, HuR is phosphorylated, resulting the dissociation of the HuR-SIRT1 mRNA complex and subsequent SIRT1 mRNA decay. A nuclear protein active regulator of SIRT1 (AROS) has been identified to directly enhance SIRT1-mediated deacetylation of p53 both in vitro and in vivo models and prevents p53-mediated transcriptional activity [34].
Hypermethylated in Cancer 1 (HIC1) and deleted in breast cancer 1 (DBC1) have emerged as negative regulators of SIRT1 [91]. HIC1, a transcriptional repressor, binds to the SIRT1 promoter and represses its transcription. Loss of HIC1 up-regulates SIRT1 expression in normal or cancer cells, resulting in the deacetylation and inactivation of p53 and enhanced tumorigenesis [92]. Another negative regulator of SIRT1, Deleted in Breast Cancer 1 (DBC1), directly interacts with SIRT1 to inhibit SIRT1 activity. Down-regulation of DBC1 expression potentiates SIRT1-dependent inhibition of apoptosis induced by genotoxic stress [92].
SIRT1 and cardiovascular diseases
Cytoprotection of SIRT1
Activation of SIRT1 confers cytoprotection in cardiomyocytes. The cytoprotection of SIRT1 activator resveratrol was initially suggested following the association between the reduced risk of coronary heart disease and the consumption of red wine that contains resveratrol [93]. Direct application of resveratrol has been shown to protect H9c2 cells, a cardiomyocyte cell line, against H2O2 and hypoxia induced apoptosis [94, 95]. The antioxidant and protective ability of resveratrol is SIRT1 dependent since knockdown of SIRT1 results in the loss of resveratrol mediated reduction of reactive oxygen species and cell protection [3-5]. Resveratrol has been shown also to prevent cardiotoxicity by the chemotherapeutic agent doxorubicin. Cardiotoxicity is in part mediated by increased production of reactive oxygen species and the protection is lost by SIRT1 inhibition [93].
Although SIRT1 is expressed in both the cytoplasm and the nucleus, nuclear SIRT1 serves to regulate anti-apoptotic or anti-oxidant function. During apoptotic injury, SIRT1 is sequestered in the cytoplasm of vascular endothelial cells and resveratrol treatment induces its translocation to the nucleus leading to an increase in cell survival [4, 5]. In cardiomyocytes, nuclear SIRT1 increases the resistance of myoblast to oxidative stress by enhancing the MnSOD expression. RNA interference of MnSOD abolishes the cell protective effect of nuclear SIRT1 and resveratrol, suggesting that nuclear SIRT1 translocation reduces oxidative stress and protect cardiomyocytes via its antioxidant activity [3].
SIRT1 and coronary heart disease
Endothelial SIRT1 also may serve as an anti-atherosclerosis factor. High fat diets with the resulting elevation of fatty acid anion and lipoprotein lipase products can activate vascular endothelial cells and impair the integrity of endothelium providing the foundation for atherosclerotic plaque [96, 97]. Dysfunctional endothelial cells also lead to platelet activation and form vessel thrombi. SIRT1 can protect endothelial cells from oxidative stress and oxidized low-density lipoprotein induced apoptosis [4, 5, 98]. Overexpression of SIRT1 in human umbilical vein endothelial cells (HUVECs) prevents oxidized low-density lipoprotein (LDL) induced apoptosis. In endothelial cell-specific SIRT1 transgenic mice, high fat-induced impairment in endothelium-dependent vasorelaxation is improved accompanied by less atherosclerotic lesion [98], suggesting that SIRT1 improves endothelial function to prevent atherosclerosis. Activation of SIRT1 also improves endothelium relaxation through up-regulating endothelial nitric oxide synthase (eNOS) expression and production of nitric oxide [99]. In addition, anti-platelet properties of resveratrol may also contribute to its ability to prevent atherosclerosis.
SIRT1 activation can inhibit vascular smooth muscle cell (VSMC) hypertrophy, which has been considered one of the critical contributors to atherosclerosis. Over-expression of SIRT1 prevents angiotensin II induced VSMC hypertrophy. Application of resveratrol prevents oxidative stress induced human coronary smooth muscle cell proliferation through inhibiting ERK activation [100]. In VSMCs, the matrix foundation may function to stabilize atherosclerotic plaque. Tissue inhibitor of metalloproteinase 3 (TIMP3) is responsible for preventing metalloproteinase 3 to digest intracellular matrix [101]. Down-regulation of TIMP3 has been tied to atherosclerosis in diabetic patients, since TIMP3 is significantly reduced in human carotid atherosclerotic plaques with decreased levels of SIRT1 [102]. In contrast, SIRT1 over-expression in VSMCs promotes TIMP3 expression while inhibition of SIRT1 reduces TIMP3 levels. This work suggests that SIRT1 in VSMCs regulates atherosclerosis through enhancing the activity of TIMP3 [101, 102].
In addition, SIRT1 appears to exert a direct protection against ischemia/reperfusion injury in cardiac tissue. Resveratrol treatment during myocardial ischemia/reperfusion in rats can reduce rhythm disturbances, cardiac infarct size, and plasma levels of lactate dehydrogenase and creatine kinase [103]. The protection of resveratrol on the heart against ischemia/reperfusion injury may be dependent on its anti-oxidant, and subsequent anti-apoptotic and anti-inflammatory activities [4, 5]. SIRT1 has been demonstrated to promote the transcriptional activity of FoxO1 to upregulate MnSOD, suppress oxidative stress in cardiac myocytes, and thereby reduce cardiac infarct volume and improve functional recovery after ischemia/reperfusion in mice [104]. In addition, application of resveratrol provides increased myocardial functional recovery after global ischemia and this may be associated with its angiogenic effect [105]. In rat myocardial infarction models, resveratrol significant increases the expression of vascular endothelial growth factor (VEGF) and its tyrosine kinase receptor Flk-1 3 weeks after myocardial infarction. Knockdown of SIRT1 in endothelial cells leads to impairment of new blood vessel formation in ischemic tissues. Resveratrol mediated angiogenesis of the infracted heart may function through nuclear factor-κB (NF-κB) and induction of nitric oxide synthase in endothelial cells [106].
SIRT1 and cardiac hypertrophy
SIRT1 can function to protect the heart from hypertrophy and prevent progressive cardiac failure. Over-expression of SIRT1 by 2.5 to 7.5 fold in transgenic mouse hearts attenuated age-related cardiac hypertrophy, apoptosis, cardiac dysfunction, and expression of senescence markers [61]. However, increased expression of SIRT1 may be detrimental. Expression of SIRT1 by 12.5 fold resulted in oxidative stress, apoptosis, and increased cardiac hypertrophy possibly as a result of mitochondrial dysfunction and depletion of NAD+ [61]. Over-expression of SIRT1 also has been demonstrated to promote recruitment of Akt and PDK1 to phosphatidylinositol 3,4,5-trisphosphate (PIP3) and increase their activation, which may be one mechanism for SIRT1 to enhance cardiac hypertrophy. Impairment of Akt activation in the hearts of SIRT1-deficient mice results in reduced cardiac hypertrophy in response to physical exercise and angiotensin II [107]. However, application of the SIRT1 activator resveratrol prevents concentric hypertrophy and cardiac cell dysfunction in animal and cell models partially through the reduction of oxidative stress without lowering the blood pressure [108], suppresses pressure overload induced cardiac hypertrophy in rats [109], and inhibits angiotensin II induced cardiomyocyte hypertrophy [110]. A recent study indicates that both SIRT1 over-expression as well as resveratrol application to activate SIRT1 prevent phenylephrine induced neonatal cardiomyocyte hypertrophy and inhibit phenylephrine induced down-regulation of fatty acid oxidation genes [111]. In H9c2 cardiac myoblasts, treatment with phenylephrine significantly increases SIRT1 expression and its deacetylase activity which is blocked by AMPK inhibitors or by AMPK knockdown. Inhibition of SIRT1 with sirtinol or siRNA gene knockdown of SIRT1 decreases H9c2 cell viability following phenylephrine treatment [112], similar to the detrimental effects observed with the loss of SIRT1 during oxidative stress in other cell systems [113]. SIRT1 also inhibits phenylephrine-induced increase in mRNA levels of the pro-inflammatory cytokine monocyte chemoattractant protein-1 in neonatal cardiomyocytes and blocks increased NF-κB activity in response to phenylephrine. Activation of SIRT1 during cardiac hypertrophy may be an adaptive response since SIRT1 expression increases with progressive cardiac hypertrophy [114]. The underlying mechanism of SIRT1 on cardiac hypertrophy has been associated with the activation of PPARα [111]. Inhibition of PPARα suppresses the beneficial effects of SIRT1 on cardiac hypertrophy, fatty acid metabolism, and inflammation. The anti-hypertrophic effects of resveratrol also may function via activation of AMPK and the inhibition of Akt [115]. Akt can be a central pathway for cell growth and protection [21, 96, 116]. In some cell pathways, Akt activation in conjunction with SIRT1 may be necessary to foster cell survival [117, 118].
SIRT1 protection in related neuro-cardiovascular disease
Activation of SIRT1 has been demonstrated to protect neurovascular tissue against ischemia. For example, resveratrol prevents hydrogen peroxide induced neuronal cell injury. Protection is dependent on SIRT1 activation since neuronal protection is lost with SIRT1 inhibition during sirtinol application or during SIRT1 gene knockdown [119]. SIRT1 also may be responsible for ischemic preconditioning since inactivation of SIRT1 by sirtinol abolishes neuroprotection [120]. In addition, treatment with resveratrol reduces brain infarct volume, decreases neurological deficits, and increases regional brain blood flow after cerebral ischemia [121]. Neurovascular protection in the brain may result from a reduction in oxygen free radical generation and subsequent inhibition of lipid peroxidation [122].
Future perspectives
Activation of SIRT1 provides cellular protection against oxidative stress, a key mechanism in the progression of many diseases, including cardiovascular disorders. Multiple cell signaling targets of SIRT1 have recently been identified that can potentially alleviate disability from cardiovascular injury. Yet, it is clear that SIRT1 modulates a complex array of downstream pathways that can be critical in determining both cell survival and cell longevity. Furthermore, SIRT1 appears to functions as a tightly regulated pathway that depending upon the level of expression may be beneficial or detrimental to cardiac cells during exposure to oxidative stress. For example, resveratrol is a well-known agent that modulates SIRT1 activity. Although resveratrol has been extensively employed as SIRT1 activator, it has broad cellular signaling targets that extend far beyond SIRT1. As a result, the effects of resveratrol and SIRT1 are tied closely to concentration and expression levels. Low concentrations of resveratrol may provide protection against oxidative stress while higher concentrations down-regulate PI 3-K/Akt/mTOR (mammalian target of rapamycin) and produce toxic effects in cells [123]. Therefore, future work in the field over the next 5-10 years has important challenges to overcome. It will be vital to understand the fine interplay between SIRT1 and its associated pathways in the cardiovascular system to identify potential therapeutic targets for the cardiovascular and related systems that offer precise disease targeting and at the same time eliminate, or at the very least, limit harmful toxic outcomes that may ensue with modulation of SIRT1 pathways.
Executive summary.
SIRT1
SIRT1 is one of the seven homologues of the yeast (Saccharomyces cerevisiae) silent information regulator-2 (Sir2) in mammals. SIRT1 is a NAD+-dependent protein deacetylase.
SIRT1 mediated deacetylase reaction
The reaction is NAD dependent (class III). In the reaction, SIRT1 transfer the acetyl residue of histone to the ADP-ribose moiety of NAD+, resulting in the production of nicotinamide, 2′-O-acetyl ADP ribose, and deacetylated proteins. SIRT1 consumes one NAD+ to transfer one acetyl residue, resulting in the decrease of the NAD+/NADH ratio.
Resveratrol
Resveratrol (trans-3,5,4′-trihydroxystibene) is a naturally occurring phytoalexin and the best-characterized compound that activates SIRT1. Resveratrol may have more broad targets in cell signaling far beyond SIRT1.
Targets of SIRT1
SIRT1 mediates many important functional proteins include PPAR-γ and its coactivator PGC-1α, forkhead transcriptional factors, AMPK, NF-κB, PTP, eNOS, p53 to regulate metabolism and cell survival.
SIRT1 and cardiovascular diseases
SIRT1 activation protects cardiomyocytes and endothelial cells against stresses.
SIRT1 inhibits VSMC hypertrophy and increases the TIMP3 activity in VSMCs to stabilize the atherosclerotic plague.
SIRT1 prevents cardiac ischemia/reperfusion induced injury.
SIRT1 activation prevents age-related and pressure overload induced cardiac hypertrophy.
Conclusions
SIRT1 and its downstream pathways are critical in the cardiovascular system during normal homeostasis and during injury
For the future development of novel strategies for cardiovascular disease, SIRT1 and its biological pathways hold great promise but further understanding of the pathways of SIRT1 is critical to foster safe and effective strategies
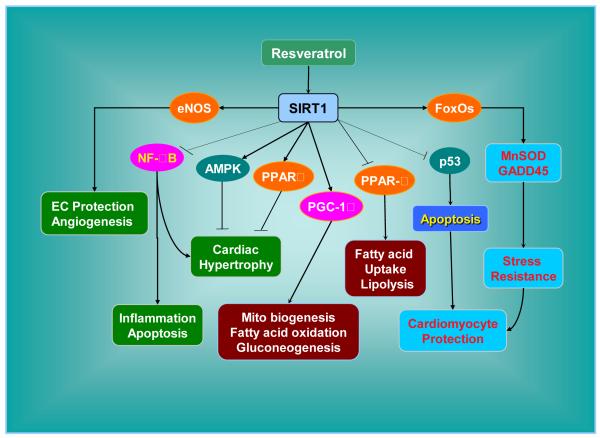
Figure 1. Cell signaling of SIRT1 leads to cardiovascular protection.
SIRT1 targets forkhead family member (FoxOs) to result in manganese superoxide dismutase (MnSOD) and the growth arrest and DNA damage (GADD45) expression to resist oxidative stress. Other SIRT1 substrates include peroxisome proliferators-activated receptor-γ (PPAR-γ) and its coactivator-1α (PGC-1α), peroxisome proliferators-activated receptor-α (PPARα), AMP activated protein kinase (AMPK), p53, nuclear factor-κB (NF-κB), and endothelial nitric oxide synthase (eNOS). The outcomes of regulating these signaling pathways by SIRT1 include protection of cardiomyocyte and endothelial cells, balance of lipid metabolism, inhibition of inflammation and atherosclerotic formation, and inhibition of cardiac hypertrophy.
Acknowledgments
This research was supported by the following grants to Kenneth Maiese: American Diabetes Association, American Heart Association (National), Bugher Foundation Award, Janssen Neuroscience Award, LEARN Foundation Award, MI Life Sciences Challenge Award, Nelson Foundation Award, NIH NIEHS (P30 ES06639), NIH NIA, NIH NINDS, and NIH ARRA.
Bibliography
- 1.Kelly GS. A review of the sirtuin system, its clinical implications, and the potential role of dietary activators like resveratrol: part 2. Altern Med Rev. 2010;15(4):313–328. [PubMed] [Google Scholar]
- 2.Bitterman KJ, Anderson RM, Cohen HY, Latorre-Esteves M, Sinclair DA. Inhibition of silencing and accelerated aging by nicotinamide, a putative negative regulator of yeast sir2 and human SIRT1. J Biol Chem. 2002;277(47):45099–45107. doi: 10.1074/jbc.M205670200. [DOI] [PubMed] [Google Scholar]
- 3.Tanno M, Kuno A, Yano T, et al. Induction of manganese superoxide dismutase by nuclear translocation and activation of SIRT1 promotes cell survival in chronic heart failure. J Biol Chem. 2010;285(11):8375–8382. doi: 10.1074/jbc.M109.090266. * Demonstrates that nuclear translocation of SIRT1 increases its activity and induces MnSOD to protect cardiomyocytes during heart failure.
- 4.Hou J, Chong ZZ, Shang YC, Maiese K. Early apoptotic vascular signaling is determined by Sirt1 through nuclear shuttling, forkhead trafficking, bad, and mitochondrial caspase activation. Curr Neurovasc Res. 2010;7(2):95–112. doi: 10.2174/156720210791184899. * Demonstrates that nuclear translocation of SIRT1 protects endothelial cells against oxidative stress.
- 5.Hou J, Wang S, Shang YC, Chong ZZ, Maiese K. Erythropoietin Employs Cell Longevity Pathways of SIRT1 to Foster Endothelial Vascular Integrity During Oxidant Stress. Curr Neurovasc Res. 2011;8(3):220–235. doi: 10.2174/156720211796558069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schemies J, Uciechowska U, Sippl W, Jung M. NAD(+) -dependent histone deacetylases (sirtuins) as novel therapeutic targets. Med Res Rev. 2010;30(6):861–889. doi: 10.1002/med.20178. [DOI] [PubMed] [Google Scholar]
- 7.Chong ZZ, Li F, Maiese K. Stress in the brain: novel cellular mechanisms of injury linked to Alzheimer’s disease. Brain Res Brain Res Rev. 2005;49(1):1–21. doi: 10.1016/j.brainresrev.2004.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chong ZZ, Li F, Maiese K. Oxidative stress in the brain: Novel cellular targets that govern survival during neurodegenerative disease. Prog Neurobiol. 2005;75(3):207–246. doi: 10.1016/j.pneurobio.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 9.Maiese K, Chong ZZ, Hou J, Shang YC. Oxidative stress: Biomarkers and novel therapeutic pathways. Exp Gerontol. 2010;45(3):217–234. doi: 10.1016/j.exger.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Maiese K, Chong ZZ, Shang YC. Raves and risks for erythropoietin. Cytokine Growth Factor Rev. 2008;19(2):145–155. doi: 10.1016/j.cytogfr.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maiese K, Li F, Chong ZZ. New avenues of exploration for erythropoietin. Jama. 2005;293(1):90–95. doi: 10.1001/jama.293.1.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maiese K, Chong ZZ, Shang YC, Hou J. Novel Avenues of Drug Discovery and Biomarkers for Diabetes Mellitus. Journal of clinical pharmacology. 2010 doi: 10.1177/0091270010362904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Szabo C. Role of nitrosative stress in the pathogenesis of diabetic vascular dysfunction. Br J Pharmacol. 2009;156(5):713–727. doi: 10.1111/j.1476-5381.2008.00086.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Erol A. Unraveling the Molecular Mechanisms Behind the Metabolic Basis of Sporadic Alzheimer’s Disease. J Alzheimers Dis. 2009 doi: 10.3233/JAD-2009-1047. [DOI] [PubMed] [Google Scholar]
- 15.Maiese K, Hou J, Chong ZZ, Shang YC. Erythropoietin, forkhead proteins, and oxidative injury: biomarkers and biology. ScientificWorldJournal. 2009;9:1072–1104. doi: 10.1100/tsw.2009.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fisher-Wellman K, Bell H, Bloomer R. Oxidative stress and antioxidant defense mechanisms linked to exercise during cardiopulmonary and metabolic disorders. Oxid Med Cell Longev. 2009;2(1):43–51. doi: 10.4161/oxim.2.1.7732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouayed J, Rammal H, Soulimani R. Oxidative stress and anxiety: Relationship and cellular pathways. Oxid Med Cell Longev. 2009;2(2):63–67. doi: 10.4161/oxim.2.2.7944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Maiese K, Chong ZZ, Shang YC, Hou J. FoxO proteins: cunning concepts and considerations for the cardiovascular system. Clin Sci (Lond) 2009;116(3):191–203. doi: 10.1042/CS20080113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cheema RS, Bansal AK, Bilaspuri GS. Manganese provides antioxidant protection for sperm cryopreservation that may offer new consideration for clinical fertility. Oxid Med Cell Longev. 2009;2(3):33–40. doi: 10.4161/oxim.2.3.8804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maiese K, Chong ZZ, Hou J, Shang YC. The “O” class: crafting clinical care with FoxO transcription factors. Adv Exp Med Biol. 2009;665:242–260. doi: 10.1007/978-1-4419-1599-3_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chong ZZ, Maiese K. The Src homology 2 domain tyrosine phosphatases SHP-1 and SHP-2: diversified control of cell growth, inflammation, and injury. Histol Histopathol. 2007;22(11):1251–1267. doi: 10.14670/hh-22.1251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Maiese K, Chong ZZ, Li F, Shang YC. Erythropoietin: elucidating new cellular targets that broaden therapeutic strategies. Prog Neurobiol. 2008;85(2):194–213. doi: 10.1016/j.pneurobio.2008.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Maiese K, Chong ZZ, Shang YC. Mechanistic insights into diabetes mellitus and oxidative stress. Curr Med Chem. 2007;14(16):1729–1738. doi: 10.2174/092986707781058968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chong ZZ, Li F, Maiese K. Cellular demise and inflammatory microglial activation during beta-amyloid toxicity are governed by Wnt1 and canonical signaling pathways. Cell Signal. 2007;19(6):1150–1162. doi: 10.1016/j.cellsig.2006.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shang YC, Chong ZZ, Hou J, Maiese K. The forkhead transcription factor FoxO3a controls microglial inflammatory activation and eventual apoptotic injury through caspase 3. Curr Neurovasc Res. 2009;6(1):20–31. doi: 10.2174/156720209787466064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leytin V, Allen DJ, Mykhaylov S, Lyubimov E, Freedman J. Thrombin-triggered platelet apoptosis. J Thromb Haemost. 2006;4(12):2656–2663. doi: 10.1111/j.1538-7836.2006.02200.x. [DOI] [PubMed] [Google Scholar]
- 27.Maiese K, Chong ZZ, Hou J, Shang YC. New strategies for Alzheimer’s disease and cognitive impairment. Oxid Med Cell Longev. 2009;2(5):279–289. doi: 10.4161/oxim.2.5.9990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mallat M, Marin-Teva JL, Cheret C. Phagocytosis in the developing CNS: more than clearing the corpses. Curr Opin Neurobiol. 2005;15(1):101–107. doi: 10.1016/j.conb.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 29.Shang YC, Chong ZZ, Hou J, Maiese K. Wnt1, FoxO3a, and NF-kappaB oversee microglial integrity and activation during oxidant stress. Cell Signal. 2010;22(9):1317–1329. doi: 10.1016/j.cellsig.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elahi MM, Kong YX, Matata BM. Oxidative stress as a mediator of cardiovascular disease. Oxid Med Cell Longev. 2009;2(5):259–269. doi: 10.4161/oxim.2.5.9441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wolfram R, Oguogho A, Palumbo B, Sinzinger H. Evidence for enhanced oxidative stress in coronary heart disease and chronic heart failure. Adv Exp Med Biol. 2003;525:197–200. doi: 10.1007/978-1-4419-9194-2_42. [DOI] [PubMed] [Google Scholar]
- 32.Venditti P, Masullo P, Di Meo S. Effects of myocardial ischemia and reperfusion on mitochondrial function and susceptibility to oxidative stress. Cell Mol Life Sci. 2001;58(10):1528–1537. doi: 10.1007/PL00000793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vasdev S, Gill VD, Singal PK. Modulation of oxidative stress-induced changes in hypertension and atherosclerosis by antioxidants. Exp Clin Cardiol. 2006;11(3):206–216. [PMC free article] [PubMed] [Google Scholar]
- 34.Kim EJ, Kho JH, Kang MR, Um SJ. Active regulator of SIRT1 cooperates with SIRT1 and facilitates suppression of p53 activity. Mol Cell. 2007;28(2):277–290. doi: 10.1016/j.molcel.2007.08.030. [DOI] [PubMed] [Google Scholar]
- 35.Kume S, Haneda M, Kanasaki K, et al. Silent information regulator 2 (SIRT1) attenuates oxidative stress-induced mesangial cell apoptosis via p53 deacetylation. Free Radic Biol Med. 2006;40(12):2175–2182. doi: 10.1016/j.freeradbiomed.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 36.Brunet A, Sweeney LB, Sturgill JF, et al. Stress-dependent regulation of FOXO transcription factors by the SIRT1 deacetylase. Science. 2004;303(5666):2011–2015. doi: 10.1126/science.1094637. [DOI] [PubMed] [Google Scholar]
- 37.Hasegawa K, Wakino S, Yoshioka K, et al. Sirt1 protects against oxidative stress-induced renal tubular cell apoptosis by the bidirectional regulation of catalase expression. Biochem Biophys Res Commun. 2008;372(1):51–56. doi: 10.1016/j.bbrc.2008.04.176. [DOI] [PubMed] [Google Scholar]
- 38.Chong ZZ, Lin SH, Li F, Maiese K. The sirtuin inhibitor nicotinamide enhances neuronal cell survival during acute anoxic injury through Akt, Bad, PARP, and mitochondrial associated “anti-apoptotic” pathways. Curr Neurovasc Res. 2005;2(4):271–285. doi: 10.2174/156720205774322584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chong ZZ, Maiese K. Enhanced Tolerance against Early and Late Apoptotic Oxidative Stress in Mammalian Neurons through Nicotinamidase and Sirtuin Mediated Pathways. Curr Neurovasc Res. 2008;5(3):159–170. doi: 10.2174/156720208785425666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Maiese K, Shang YC, Chong ZZ, Hou J. Diabetes mellitus: channeling care through cellular discovery. Curr Neurovasc Res. 2010;7(1):59–64. doi: 10.2174/156720210790820217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Picard F, Kurtev M, Chung N, et al. Sirt1 promotes fat mobilization in white adipocytes by repressing PPAR-gamma. Nature. 2004;429(6993):771–776. doi: 10.1038/nature02583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Han L, Zhou R, Niu J, Mcnutt MA, Wang P, Tong T. SIRT1 is regulated by a PPAR{gamma}-SIRT1 negative feedback loop associated with senescence. Nucleic Acids Res. 2010;38(21):7458–7471. doi: 10.1093/nar/gkq609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sugden MC, Caton PW, Holness MJ. PPAR control: it’s SIRTainly as easy as PGC. J Endocrinol. 2010;204(2):93–104. doi: 10.1677/JOE-09-0359. [DOI] [PubMed] [Google Scholar]
- 44.Valle I, Alvarez-Barrientos A, Arza E, Lamas S, Monsalve M. PGC-1alpha regulates the mitochondrial antioxidant defense system in vascular endothelial cells. Cardiovasc Res. 2005;66(3):562–573. doi: 10.1016/j.cardiores.2005.01.026. [DOI] [PubMed] [Google Scholar]
- 45.Lynn EG, Stevens MV, Wong RP, et al. Transient upregulation of PGC-1alpha diminishes cardiac ischemia tolerance via upregulation of ANT1. J Mol Cell Cardiol. 2010;49(4):693–698. doi: 10.1016/j.yjmcc.2010.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Russell LK, Mansfield CM, Lehman JJ, et al. Cardiac-specific induction of the transcriptional coactivator peroxisome proliferator-activated receptor gamma coactivator-1alpha promotes mitochondrial biogenesis and reversible cardiomyopathy in a developmental stage-dependent manner. Circ Res. 2004;94(4):525–533. doi: 10.1161/01.RES.0000117088.36577.EB. [DOI] [PubMed] [Google Scholar]
- 47.Wenz T. Mitochondria and PGC-1alpha in Aging and Age-Associated Diseases. J Aging Res. 2011;2011:810619. doi: 10.4061/2011/810619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rodgers JT, Lerin C, Haas W, Gygi SP, Spiegelman BM, Puigserver P. Nutrient control of glucose homeostasis through a complex of PGC-1alpha and SIRT1. Nature. 2005;434(7029):113–118. doi: 10.1038/nature03354. [DOI] [PubMed] [Google Scholar]
- 49.Purushotham A, Schug TT, Xu Q, Surapureddi S, Guo X, Li X. Hepatocyte-specific deletion of SIRT1 alters fatty acid metabolism and results in hepatic steatosis and inflammation. Cell Metab. 2009;9(4):327–338. doi: 10.1016/j.cmet.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maiese K, Chong ZZ, Shang YC. “Sly as a FOXO”: New paths with Forkhead signaling in the brain. Curr Neurovasc Res. 2007;4(4):295–302. doi: 10.2174/156720207782446306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Maiese K, Chong ZZ, Shang YC. OutFOXOing disease and disability: the therapeutic potential of targeting FoxO proteins. Trends Mol Med. 2008;14(5):219–227. doi: 10.1016/j.molmed.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Maiese K, Chong ZZ, Shang YC, Hou J. Clever cancer strategies with FoxO transcription factors. Cell Cycle. 2008;7(24):3829–3839. doi: 10.4161/cc.7.24.7231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Maiese K, Chong ZZ, Shang YC, Hou J. A “FOXO” in sight: targeting Foxo proteins from conception to cancer. Med Res Rev. 2009;29(3):395–418. doi: 10.1002/med.20139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lei H, Quelle FW. FOXO transcription factors enforce cell cycle checkpoints and promote survival of hematopoietic cells after DNA damage. Mol Cancer Res. 2009;7(8):1294–1303. doi: 10.1158/1541-7786.MCR-08-0531. [DOI] [PubMed] [Google Scholar]
- 55.Frescas D, Valenti L, Accili D. Nuclear trapping of the forkhead transcription factor FoxO1 via Sirt-dependent deacetylation promotes expression of glucogenetic genes. J Biol Chem. 2005;280(21):20589–20595. doi: 10.1074/jbc.M412357200. [DOI] [PubMed] [Google Scholar]
- 56.Maiese K, Chong ZZ, Shang YC, Hou J. Rogue proliferation versus restorative protection: where do we draw the line for Wnt and forkhead signaling? Expert opinion on therapeutic targets. 2008;12(7):905–916. doi: 10.1517/14728222.12.7.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Storz P. Forkhead homeobox type O transcription factors in the responses to oxidative stress. Antioxid Redox Signal. 2011;14(4):593–605. doi: 10.1089/ars.2010.3405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Van Der Horst A, Tertoolen LG, De Vries-Smits LM, Frye RA, Medema RH, Burgering BM. FOXO4 is acetylated upon peroxide stress and deacetylated by the longevity protein hSir2(SIRT1) J Biol Chem. 2004;279(28):28873–28879. doi: 10.1074/jbc.M401138200. [DOI] [PubMed] [Google Scholar]
- 59.Kobayashi Y, Furukawa-Hibi Y, Chen C, et al. SIRT1 is critical regulator of FOXO-mediated transcription in response to oxidative stress. Int J Mol Med. 2005;16(2):237–243. [PubMed] [Google Scholar]
- 60.Daitoku H, Hatta M, Matsuzaki H, et al. Silent information regulator 2 potentiates Foxo1-mediated transcription through its deacetylase activity. Proc Natl Acad Sci U S A. 2004;101(27):10042–10047. doi: 10.1073/pnas.0400593101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Alcendor RR, Gao S, Zhai P, et al. Sirt1 regulates aging and resistance to oxidative stress in the heart. Circ Res. 2007;100(10):1512–1521. doi: 10.1161/01.RES.0000267723.65696.4a. * Demonstrates that the moderate increase in SIRT1 activity prevents age-related cardiac hypertrophy.
- 62.Hariharan N, Maejima Y, Nakae J, Paik J, Depinho RA, Sadoshima J. Deacetylation of FoxO by Sirt1 Plays an Essential Role in Mediating Starvation-Induced Autophagy in Cardiac Myocytes. Circ Res. 2010;107(12):1470–1482. doi: 10.1161/CIRCRESAHA.110.227371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xiong S, Salazar G, Patrushev N, Alexander RW. FoxO1 Mediates an Autofeedback Loop Regulating SIRT1 Expression. J Biol Chem. 2011;286(7):5289–5299. doi: 10.1074/jbc.M110.163667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Nemoto S, Fergusson MM, Finkel T. Nutrient availability regulates SIRT1 through a forkhead-dependent pathway. Science. 2004;306(5704):2105–2108. doi: 10.1126/science.1101731. [DOI] [PubMed] [Google Scholar]
- 65.Paiva MA, Rutter-Locher Z, Goncalves LM, et al. Enhancing AMPK activation during ischemia protects the diabetic heart against reperfusion injury. Am J Physiol Heart Circ Physiol. 2011;300(6):H2123–2134. doi: 10.1152/ajpheart.00707.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Carvajal K, Zarrinpashneh E, Szarszoi O, et al. Dual cardiac contractile effects of the alpha2-AMPK deletion in low-flow ischemia and reperfusion. Am J Physiol Heart Circ Physiol. 2007;292(6):H3136–3147. doi: 10.1152/ajpheart.00683.2006. [DOI] [PubMed] [Google Scholar]
- 67.Lan F, Cacicedo JM, Ruderman N, Ido Y. SIRT1 modulation of the acetylation status, cytosolic localization, and activity of LKB1. Possible role in AMP-activated protein kinase activation. J Biol Chem. 2008;283(41):27628–27635. doi: 10.1074/jbc.M805711200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Canto C, Auwerx J. Caloric restriction, SIRT1 and longevity. Trends Endocrinol Metab. 2009;20(7):325–331. doi: 10.1016/j.tem.2009.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fulco M, Cen Y, Zhao P, et al. Glucose restriction inhibits skeletal myoblast differentiation by activating SIRT1 through AMPK-mediated regulation of Nampt. Dev Cell. 2008;14(5):661–673. doi: 10.1016/j.devcel.2008.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Herranz D, Serrano M. SIRT1: recent lessons from mouse models. Nat Rev Cancer. 2010;10(12):819–823. doi: 10.1038/nrc2962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Aoshiba K, Onizawa S, Tsuji T, Nagai A. Therapeutic effects of erythropoietin in murine models of endotoxin shock. Crit Care Med. 2009;37(3):889–898. doi: 10.1097/CCM.0b013e31819b8371. [DOI] [PubMed] [Google Scholar]
- 72.Chong ZZ, Li F, Maiese K. Erythropoietin requires NF-kappaB and its nuclear translocation to prevent early and late apoptotic neuronal injury during beta-amyloid toxicity. Curr Neurovasc Res. 2005;2(5):387–399. doi: 10.2174/156720205774962683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Pappo O, Ben-Ari Z, Shevtsov E, et al. The role of excessive versus acute administration of erythropoietin in attenuating hepatic ischemia-reperfusion injury. Can J Physiol Pharmacol. 2010;88(12):1130–1137. doi: 10.1139/Y10-091. [DOI] [PubMed] [Google Scholar]
- 74.Chong ZZ, Li F, Maiese K. The pro-survival pathways of mTOR and protein kinase B target glycogen synthase kinase-3beta and nuclear factor-kappaB to foster endogenous microglial cell protection. Int J Mol Med. 2007;19(2):263–272. [PMC free article] [PubMed] [Google Scholar]
- 75.Kaushal V, Schlichter LC. Mechanisms of microglia-mediated neurotoxicity in a new model of the stroke penumbra. J Neurosci. 2008;28(9):2221–2230. doi: 10.1523/JNEUROSCI.5643-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Maiese K, Chong ZZ, Hou J, Shang YC. Erythropoietin and oxidative stress. Curr Neurovasc Res. 2008;5(2):125–142. doi: 10.2174/156720208784310231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yeung F, Hoberg JE, Ramsey CS, et al. Modulation of NF-kappaB-dependent transcription and cell survival by the SIRT1 deacetylase. Embo J. 2004;23(12):2369–2380. doi: 10.1038/sj.emboj.7600244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Teng FY, Tang BL. NF-kappaB signaling in neurite growth and neuronal survival. Reviews in the neurosciences. 2010;21(4):299–313. doi: 10.1515/revneuro.2010.21.4.299. [DOI] [PubMed] [Google Scholar]
- 79.Regula KM, Baetz D, Kirshenbaum LA. Nuclear factor-kappaB represses hypoxia-induced mitochondrial defects and cell death of ventricular myocytes. Circulation. 2004;110(25):3795–3802. doi: 10.1161/01.CIR.0000150537.59754.55. [DOI] [PubMed] [Google Scholar]
- 80.Boyle EM, Jr., Canty TG, Jr., Morgan EN, Yun W, Pohlman TH, Verrier ED. Treating myocardial ischemia-reperfusion injury by targeting endothelial cell transcription. Ann Thorac Surg. 1999;68(5):1949–1953. doi: 10.1016/s0003-4975(99)01033-4. [DOI] [PubMed] [Google Scholar]
- 81.Zelarayan L, Renger A, Noack C, et al. NF-kappaB activation is required for adaptive cardiac hypertrophy. Cardiovasc Res. 2009;84(3):416–424. doi: 10.1093/cvr/cvp237. [DOI] [PubMed] [Google Scholar]
- 82.Vercauteren M, Remy E, Devaux C, et al. Improvement of peripheral endothelial dysfunction by protein tyrosine phosphatase inhibitors in heart failure. Circulation. 2006;114(23):2498–2507. doi: 10.1161/CIRCULATIONAHA.106.630129. [DOI] [PubMed] [Google Scholar]
- 83.Sun C, Zhang F, Ge X, et al. SIRT1 improves insulin sensitivity under insulin-resistant conditions by repressing PTP1B. Cell Metab. 2007;6(4):307–319. doi: 10.1016/j.cmet.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 84.Vaziri H, Dessain SK, Ng Eaton E, et al. hSIR2(SIRT1) functions as an NAD-dependent p53 deacetylase. Cell. 2001;107(2):149–159. doi: 10.1016/s0092-8674(01)00527-x. [DOI] [PubMed] [Google Scholar]
- 85.Wang C, Chen L, Hou X, et al. Interactions between E2F1 and SirT1 regulate apoptotic response to DNA damage. Nat Cell Biol. 2006;8(9):1025–1031. doi: 10.1038/ncb1468. [DOI] [PubMed] [Google Scholar]
- 86.Wohlschlaeger J, Schmitz KJ, Takeda A, et al. Reversible regulation of the retinoblastoma protein/E2F-1 pathway during “reverse cardiac remodelling” after ventricular unloading. J Heart Lung Transplant. 2010;29(1):117–124. doi: 10.1016/j.healun.2009.09.017. [DOI] [PubMed] [Google Scholar]
- 87.Wang RH, Zheng Y, Kim HS, et al. Interplay among BRCA1, SIRT1, and Survivin during BRCA1-associated tumorigenesis. Mol Cell. 2008;32(1):11–20. doi: 10.1016/j.molcel.2008.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Revollo JR, Grimm AA, Imai S. The NAD biosynthesis pathway mediated by nicotinamide phosphoribosyltransferase regulates Sir2 activity in mammalian cells. J Biol Chem. 2004;279(49):50754–50763. doi: 10.1074/jbc.M408388200. [DOI] [PubMed] [Google Scholar]
- 89.Zhang T, Berrocal JG, Frizzell KM, et al. Enzymes in the NAD+ salvage pathway regulate SIRT1 activity at target gene promoters. J Biol Chem. 2009;284(30):20408–20417. doi: 10.1074/jbc.M109.016469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Abdelmohsen K, Pullmann R, Jr., Lal A, et al. Phosphorylation of HuR by Chk2 regulates SIRT1 expression. Mol Cell. 2007;25(4):543–557. doi: 10.1016/j.molcel.2007.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen WY, Wang DH, Yen RC, Luo J, Gu W, Baylin SB. Tumor suppressor HIC1 directly regulates SIRT1 to modulate p53-dependent DNA-damage responses. Cell. 2005;123(3):437–448. doi: 10.1016/j.cell.2005.08.011. [DOI] [PubMed] [Google Scholar]
- 92.Kim JE, Chen J, Lou Z. DBC1 is a negative regulator of SIRT1. Nature. 2008;451(7178):583–586. doi: 10.1038/nature06500. [DOI] [PubMed] [Google Scholar]
- 93.Renaud S, De Lorgeril M. Wine, alcohol, platelets, and the French paradox for coronary heart disease. Lancet. 1992;339(8808):1523–1526. doi: 10.1016/0140-6736(92)91277-f. [DOI] [PubMed] [Google Scholar]
- 94.Yu W, Fu YC, Zhou XH, et al. Effects of resveratrol on H(2)O(2)-induced apoptosis and expression of SIRTs in H9c2 cells. J Cell Biochem. 2009;107(4):741–747. doi: 10.1002/jcb.22169. [DOI] [PubMed] [Google Scholar]
- 95.Chen CJ, Yu W, Fu YC, Wang X, Li JL, Wang W. Resveratrol protects cardiomyocytes from hypoxia-induced apoptosis through the SIRT1-FoxO1 pathway. Biochem Biophys Res Commun. 2009;378(3):389–393. doi: 10.1016/j.bbrc.2008.11.110. [DOI] [PubMed] [Google Scholar]
- 96.Maiese K, Chong ZZ, Hou J, Shang YC. The vitamin nicotinamide: translating nutrition into clinical care. Molecules. 2009;14(9):3446–3485. doi: 10.3390/molecules14093446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Melnik BC, John SM, Schmitz G. Over-stimulation of insulin/IGF-1 signaling by western diet may promote diseases of civilization: lessons learnt from laron syndrome. Nutr Metab (Lond) 2011;8:41. doi: 10.1186/1743-7075-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Zhang QJ, Wang Z, Chen HZ, et al. Endothelium-specific overexpression of class III deacetylase SIRT1 decreases atherosclerosis in apolipoprotein E-deficient mice. Cardiovasc Res. 2008;80(2):191–199. doi: 10.1093/cvr/cvn224. * Demonstrates that endothelial SIRT1 functions to prevent atherosclerosis.
- 99.Mattagajasingh I, Kim CS, Naqvi A, et al. SIRT1 promotes endothelium-dependent vascular relaxation by activating endothelial nitric oxide synthase. Proc Natl Acad Sci U S A. 2007;104(37):14855–14860. doi: 10.1073/pnas.0704329104. * Demonstrates that SIRT1 regulates vascular tone through deacetylation of eNOS.
- 100.El-Mowafy AM, Alkhalaf M, El-Kashef HA. Resveratrol reverses hydrogen peroxide-induced proliferative effects in human coronary smooth muscle cells: a novel signaling mechanism. Archives of medical research. 2008;39(2):155–161. doi: 10.1016/j.arcmed.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 101.Stein S, Matter CM. Protective roles of SIRT1 in atherosclerosis. Cell Cycle. 2011;10(4):640–647. doi: 10.4161/cc.10.4.14863. [DOI] [PubMed] [Google Scholar]
- 102.Cardellini M, Menghini R, Martelli E, et al. TIMP3 is reduced in atherosclerotic plaques from subjects with type 2 diabetes and increased by SirT1. Diabetes. 2009;58(10):2396–2401. doi: 10.2337/db09-0280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hung LM, Su MJ, Chen JK. Resveratrol protects myocardial ischemia-reperfusion injury through both NO-dependent and NO-independent mechanisms. Free Radic Biol Med. 2004;36(6):774–781. doi: 10.1016/j.freeradbiomed.2003.12.016. [DOI] [PubMed] [Google Scholar]
- 104.Hsu CP, Zhai P, Yamamoto T, et al. Silent information regulator 1 protects the heart from ischemia/reperfusion. Circulation. 2010;122(21):2170–2182. doi: 10.1161/CIRCULATIONAHA.110.958033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Dernek S, Ikizler M, Erkasap N, et al. Cardioprotection with resveratrol pretreatment: improved beneficial effects over standard treatment in rat hearts after global ischemia. Scand Cardiovasc J. 2004;38(4):245–254. doi: 10.1080/14017430410035476. [DOI] [PubMed] [Google Scholar]
- 106.Fukuda S, Kaga S, Zhan L, et al. Resveratrol ameliorates myocardial damage by inducing vascular endothelial growth factor-angiogenesis and tyrosine kinase receptor Flk-1. Cell Biochem Biophys. 2006;44(1):43–49. doi: 10.1385/CBB:44:1:043. [DOI] [PubMed] [Google Scholar]
- 107.Sundaresan NR, Pillai VB, Wolfgeher D, et al. The deacetylase SIRT1 promotes membrane localization and activation of Akt and PDK1 during tumorigenesis and cardiac hypertrophy. Science signaling. 2011;4(182):ra46. doi: 10.1126/scisignal.2001465. [DOI] [PubMed] [Google Scholar]
- 108.Thandapilly SJ, Wojciechowski P, Behbahani J, et al. Resveratrol prevents the development of pathological cardiac hypertrophy and contractile dysfunction in the SHR without lowering blood pressure. Am J Hypertens. 2010;23(2):192–196. doi: 10.1038/ajh.2009.228. [DOI] [PubMed] [Google Scholar]
- 109.Wojciechowski P, Juric D, Louis XL, et al. Resveratrol arrests and regresses the development of pressure overload-but not volume overload-induced cardiac hypertrophy in rats. J Nutr. 2010;140(5):962–968. doi: 10.3945/jn.109.115006. [DOI] [PubMed] [Google Scholar]
- 110.Cheng TH, Liu JC, Lin H, et al. Inhibitory effect of resveratrol on angiotensin II-induced cardiomyocyte hypertrophy. Naunyn Schmiedebergs Arch Pharmacol. 2004;369(2):239–244. doi: 10.1007/s00210-003-0849-6. * Shows for the first time that SIRT1 activator resveratrol prevents angiotensin II induced cardiomyocyte hypertrophy.
- 111.Planavila A, Iglesias R, Giralt M, Villarroya F. Sirt1 acts in association with PPAR{alpha} to protect the heart from hypertrophy, metabolic dysregulation, and inflammation. Cardiovasc Res. 2010 doi: 10.1093/cvr/cvq376. [DOI] [PubMed] [Google Scholar]
- 112.Passariello CL, Zini M, Nassi PA, Pignatti C, Stefanelli C. Upregulation of SIRT1 deacetylase in phenylephrine-treated cardiomyoblasts. Biochem Biophys Res Commun. 2011;407(3):512–516. doi: 10.1016/j.bbrc.2011.03.049. [DOI] [PubMed] [Google Scholar]
- 113.Balan V, Miller GS, Kaplun L, et al. Life span extension and neuronal cell protection by Drosophila nicotinamidase. J Biol Chem. 2008;283(41):27810–27819. doi: 10.1074/jbc.M804681200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Li L, Zhao L, Yi-Ming W, et al. Sirt1 hyperexpression in SHR heart related to left ventricular hypertrophy. Can J Physiol Pharmacol. 2009;87(1):56–62. doi: 10.1139/Y08-099. [DOI] [PubMed] [Google Scholar]
- 115.Chan AY, Dolinsky VW, Soltys CL, et al. Resveratrol inhibits cardiac hypertrophy via AMP-activated protein kinase and Akt. J Biol Chem. 2008;283(35):24194–24201. doi: 10.1074/jbc.M802869200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Chong ZZ, Kang JQ, Maiese K. Erythropoietin is a novel vascular protectant through activation of Akt1 and mitochondrial modulation of cysteine proteases. Circulation. 2002;106(23):2973–2979. doi: 10.1161/01.cir.0000039103.58920.1f. [DOI] [PubMed] [Google Scholar]
- 117.Chong ZZ, Li F, Maiese K. Activating Akt and the brain’s resources to drive cellular survival and prevent inflammatory injury. Histol Histopathol. 2005;20(1):299–315. doi: 10.14670/hh-20.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Maiese K, Morhan SD, Chong ZZ. Oxidative stress biology and cell injury during type 1 and type 2 diabetes mellitus. Curr Neurovasc Res. 2007;4(1):63–71. doi: 10.2174/156720207779940653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Albani D, Polito L, Batelli S, et al. The SIRT1 activator resveratrol protects SK N-BE cells from oxidative stress and against toxicity caused by alpha-synuclein or amyloid-beta (1-42) peptide. J Neurochem. 2009;110(5):1445–1456. doi: 10.1111/j.1471-4159.2009.06228.x. [DOI] [PubMed] [Google Scholar]
- 120.Raval AP, Dave KR, Perez-Pinzon MA. Resveratrol mimics ischemic preconditioning in the brain. J Cereb Blood Flow Metab. 2006;26(9):1141–1147. doi: 10.1038/sj.jcbfm.9600262. [DOI] [PubMed] [Google Scholar]
- 121.Lu KT, Chiou RY, Chen LG, et al. Neuroprotective effects of resveratrol on cerebral ischemia-induced neuron loss mediated by free radical scavenging and cerebral blood flow elevation. Journal of agricultural and food chemistry. 2006;54(8):3126–3131. doi: 10.1021/jf053011q. [DOI] [PubMed] [Google Scholar]
- 122.Simao F, Matte A, Matte C, et al. Resveratrol prevents oxidative stress and inhibition of Na(+)K(+)-ATPase activity induced by transient global cerebral ischemia in rats. The Journal of nutritional biochemistry. 2011 doi: 10.1016/j.jnutbio.2010.07.013. [DOI] [PubMed] [Google Scholar]
- 123.Jiang H, Shang X, Wu H, et al. Resveratrol downregulates PI3K/Akt/mTOR signaling pathways in human U251 glioma cells. Journal of experimental therapeutics & oncology. 2009;8(1):25–33. [PMC free article] [PubMed] [Google Scholar]