Abstract
Introduction:
Individuals with alcohol, drug, or mental (ADM) disorders combined make up over 40% of all smokers in the U.S. Primary care providers (PCPs) play an important role in smoking cessation counseling, but their effectiveness with this population is unclear. This study evaluated the effectiveness of PCP smoking cessation counseling for smokers with ADM disorders.
Methods:
Probit regressions conducted in 2009–2010 examined the relationship between past year PCP smoking cessation counseling and successful quitting among 1,356 adults who reported smoking in the 1998–1999 Community Tracking Study survey and who reported seeing a PCP in the past year in the follow-up 2000–2001 Healthcare for Communities Survey. Past year PCP exercise counseling was used as an instrumental variable for past year PCP smoking cessation counseling to account for potential hidden bias between smoking status and receipt of smoking cessation counseling.
Results:
Smokers with and without ADM disorders were equally likely to receive smoking cessation counseling (72.9% vs. 69.9%). Using the instrumental variable approach, smoking cessation counseling by PCPs was significantly associated (p < .01) with quitting among both groups. Predicted probabilities of quitting without smoking cessation counseling were 6.0% for smokers with ADM disorders and 10.5% for smokers without ADM disorders. Predicted probabilities of quitting with smoking cessation counseling were 31.3% for smokers with ADM disorders and 34.9% for smokers without ADM disorders.
Conclusions:
This study shows that PCPs can help smokers with ADM disorders successfully quit. These smokers should be targeted for smoking cessation counseling to reduce the health burden of tobacco.
Introduction
Cigarette smoking continues to be the leading preventable cause of death in the United States (Adhikari, Kahende, Malarcher, Pechacek, & Tong, 2008; Mokdad, Marks, Stroup, & Gerberding, 2004, 2005). Individuals with alcohol, drug, or mental (ADM) disorders combined make up over 40% of all smokers in the United States (Lasser et al., 2000). Although individuals with ADM disorders comprise 22% of the U.S. population, as a group they account for 44% of all cigarettes consumed; this high consumption is due to their higher smoking prevalence (Breslau, 1995; Glassman et al., 1990; Goff, Henderson, & Amico, 1992; Gonzalez-Pinto et al., 1998; Kelly & McCreadie, 1999; Lasser et al., 2000) and their higher consumption of cigarettes (Lasser et al., 2000). Individuals with ADM disorders experience earlier mortality, particularly cardiovascular mortality, compared with those without ADM disorders; this earlier mortality is partially due to cigarette smoking (Harris & Barraclough, 1998; Kilbourne et al., 2009). Therefore, identification of approaches that reduce smoking among individuals with ADM disorders is important for reducing early mortality among these individuals and also the burden of smoking on the U.S. health care system (Ziedonis et al., 2008).
Primary care and other general medical providers play an important role in smoking cessation counseling. The provision of advice to quit by primary care providers (PCPs) by itself increases the odds of quitting by 1.3, and physician treatment for smoking increases the odds of quitting by 2.2 (Fiore et al., 2008). However, the relative effectiveness of smoking cessation advice by PCPs with smokers who have ADM disorders is not known (Fiore et al., 2008). As the care for many common ADM disorders are provided in the primary care setting (Unutzer, Schoenbaum, Druss, & Katon, 2006), identifying effective smoking cessation approaches in primary care settings for this population is critical (Ziedonis et al., 2008). The purpose of this study was to evaluate whether smoking cessation counseling by PCPs is associated with quitting behavior among smokers with ADM disorders.
Methods
Data
Our sampling frame consisted of the 7,909 adults who were respondents for two linked surveys, the second wave of the Healthcare for Communities Survey (HCC2), which was conducted in 2000–2001, and the second wave of the Community Tracking Survey (CTS2), which was conducted in 1998–1999. The HCC2 sampling method oversampled the CTS2 respondents who were poor, used mental health services, reported treatment for an alcohol problem from a doctor or other medical professional in the past 2 years, or reported psychological distress at the time of the CTS2 interview (Sturm et al., 1999). The HCC2 survey asked all respondents “Do you currently smoke or chew tobacco?” In addition, the HCC2 survey covered several broad areas: demographic characteristics; health and daily activities; mental health, alcohol and drug use that allow for identifying ADM disorders; general medical provider’s advice to change health behaviors; general health insurance and insurance coverage; and employment status, income, and wealth (Sturm et al., 1999). The CTS2 survey asked all respondents “Have you smoked at least 100 cigarettes in your entire life?” and “Do you now smoke cigarettes every day, some days, or not at all?” The CTS2 survey also covered areas including demographic characteristics, health status, health insurance, use of health services, and satisfaction with care; however, it did not include detailed questions that would identify the presence of ADM disorders (Center for Studying Health System Change, 2002). As a result, we used the HCC2 survey to identify ADM disorders and smoking status in 2000–2001 and used the CTS2 survey to identify “baseline” smoking status in 1998–1999.
We then created an “all smokers” cohort, which consisted of 1,356 adults who reported that they were current smokers, both every day and some days, and had smoked at least 100 cigarettes as of the time of the CTS2 interview, and who responded in HCC2 that they had visited a general medical provider in the past year prior to their HCC2 interview, such as a primary care doctor or family physician, general internist, nurse or physician assistant, a chiropractor, or health clinic. Within this main cohort, we created two subcohorts. The first subcohort was an “ADM smokers” cohort, which was the subset of the all smokers cohort that consisted of 619 (45.6%) adults who reported any ADM disorder in the past year (except for psychotic disorder which was based on lifetime occurrence) in HCC2. The ADM disorders were defined by self-report of symptoms or behaviors, and included alcohol dependence, binge drinking, drug dependence, drug abuse, major depressive disorder, dysthymia, generalized anxiety disorder, panic disorder, and psychotic disorder. Alcohol dependence was identified using an AUDIT score ≥ 8 (Saunders, Aasland, Babor, Fuente, & Grant, 1993). Binge drinking was identified if ≥6 drinks were reported to be consumed per occasion. Drug dependence was identified by the presence of dependence symptoms or psychological/emotional problems with drug use. Drug abuse was identified by use of any substances or prescription drug use that did not follow prescribed directions. Depression, dysthymia, and generalized anxiety disorder were defined by classification of symptoms by Diagnostic and Statistical Manual of Mental Disorders, 3rd edition, revised. Panic attack was identified if associated symptoms occurred in past year. Psychosis was identified if there ever was a diagnosis of schizophrenia or hospitalization for psychotic symptoms. The second subcohort was a “non-ADM smokers” cohort, which consisted of 737 adults (54.4%) who were in the all smokers cohort but not in the ADM smokers cohort. Figure 1 shows the detailed process of sample selection and sample size for these three analytical cohorts.
Figure 1.
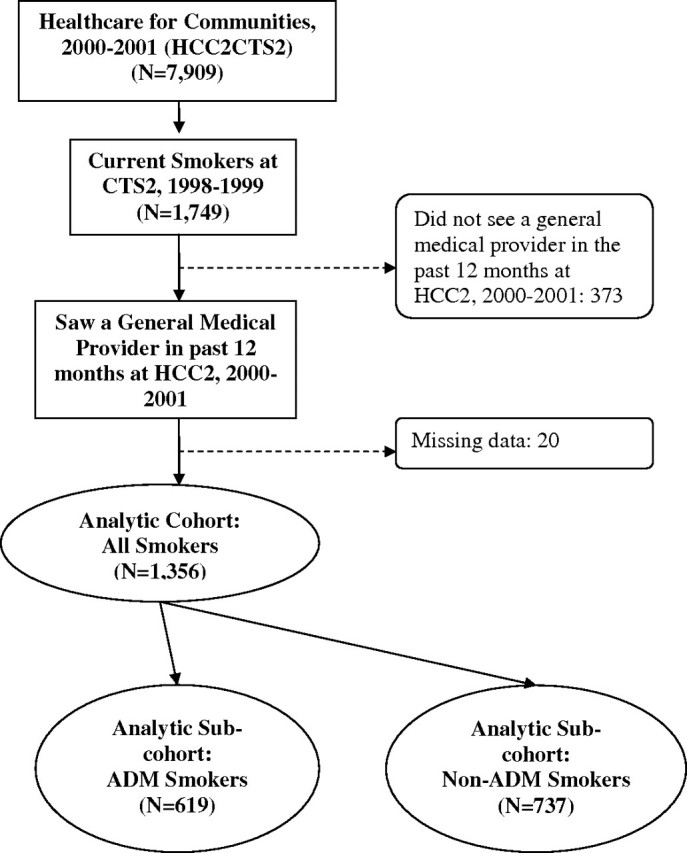
Flowchart of sample inclusion criteria and sample size. HCC2CTS2 = Healthcare for Communities Survey Wave 2 sample that previously responded to the Community Tracking Survey Wave 2; HCC2 = Healthcare for Communities Survey Wave 2; CTS2 = Community Tracking Survey Wave 2; ADM = alcohol, drug, or mental disorder.
Variables
From the HCC2 survey data, we constructed the following analytic variables. The dependent variable for quitting behavior was specified by the smoking status at the time of the HCC2 interview. If a respondent answered “no” to the question that asked “do you currently smoke or chew tobacco?” they were considered a quitter. The HCC2 survey, unlike the CTS2 survey, did not ask about amount of cigarette consumption or daily versus nondaily use. The main variable of interest, past year smoking cessation counseling, was defined by the survey question: “In the past 12 months, did any of the general medical providers talk to you about quitting or avoiding smoking?” Other covariates consisted of economic and sociodemographic factors including gender, age, race/ethnicity, U.S. Census region of residence, education level, nativity status, household income in the past year, marital status, employment status, body mass index (BMI), health insurance coverage, and physical activity. The main variable of interest and other covariates were categorical variables using the following reference groups: no cessation counseling, male, age 18–24 years, non-Hispanic White, Northeast region, less than a high school degree, not born in the United States, annual household income less than $25,000, married, not unemployed, BMI < 25, private health insurance coverage, and no physical activity.
Potential Hidden Bias Affecting Analysis of Smoking Cessation Counseling by PCPs
Studies of the relationship between receipt of smoking cessation counseling and quitting are potentially affected by a hidden bias. Rather than a unidirectional relationship, there may be a bidirectional relationship, also known as endogeneity in the econometrics literature. Receipt of smoking cessation counseling has a positive effect on quitting (Fiore et al., 2008). However, many individuals who receive smoking cessation counseling do not successfully quit; even with intensive counseling, abstinence rates are around 22% (Fiore et al., 2008). As a result, a simple examination of the association between receipt of smoking cessation counseling and quitting may appear negative as the effect of the greater number of smokers who do not quit outweighs the effect of the fewer number of successful quitters. One method of dealing with this hidden bias problem is to use the instrumental variable approach, an approach which has been increasingly used in studies of health care outcomes (Bao, Duan, & Fox, 2006; McClellan, McNeil, & Newhouse, 1994; Stukel et al., 2007). This approach identifies “instrumental variables” that are associated with the characteristics of interest for the predictor variable potentially affected by hidden bias (e.g., smoking cessation counseling), but ideally have no direct correlation with the outcome variable (i.e., quitting).
Instrumental Variable
A prior study of smoking cessation counseling in a general population sample used exercise and diet/nutrition counseling as instrumental variables to correct for the hidden bias (Bao et al., 2006). The theoretical basis for these two instrumental variables is based on the behavioral pattern of providers in providing preventive care. Providers who counsel on one type of health behavior of the patient (e.g., diet or physical activity) tend to counsel on other types (e.g., smoking cessation) as well. As a result, counseling on exercise and diet/nutrition should be associated with smoking cessation counseling (Bao et al., 2006). The HCC2 survey contained two potential instrumental variables: exercise counseling and weight counseling. Past year exercise counseling was defined by the question: “In the past 12 months, did any of the general medical providers talk to you about starting or increasing regular exercise?” Past year weight counseling question asked: “In the past 12 months, did any of the general medical providers talk to you about losing or gaining weight?”
The prior study using counseling measures as instrumental variables for smoking cessation counseling makes the assumption that provider counseling for diet/nutrition and for physical activity is not directly correlated with the patient's likelihood of success in smoking cessation (except through increased likelihood of provider advice for smoking cessation; Bao et al., 2006). However, weight counseling has several characteristics that make it a less appealing instrumental variable for smoking cessation counseling. First, it is generally targeted to overweight or obese individuals; exercise counseling is a more applicable to a broader range of individuals since few meet the recommendations for exercise levels (U.S. Department of Health and Human Services, 2008). Second, smoking cessation has been associated with weight gain (Eisenberg & Quinn, 2006; Klesges, Meyers, Klesges, & La Vasque, 1989; Klesges et al., 1997; Williamson et al., 1991), which raises issues of additional hidden bias between weight counseling and smoking cessation status. As a result, we only considered exercise counseling as the potential instrumental variable for smoking cessation advice in this study.
Analysis
We conducted probit regressions in 2009 and 2010 separately for all smokers, ADM smokers, and non-ADM smokers cohorts to estimate quitting as a function of past year PCP smoking cessation counseling and other covariates. These covariates included gender, age, race/ethnicity, region of residence, education, nativity, household income, marital status, employment, BMI, health insurance, and physical activity. We then checked for hidden bias between past year PCP smoking cessation and quitting by conducting the Durbin–Wu–Hausman specification test (Durbin, 1954; Hausman, 1978; Wu, 1973). To correct for the hidden bias, we used the instrumental variable approach in a two-stage model. In the first-stage model of the instrumental variable approach, smoking cessation counseling was specified as a function of past year PCP exercise counseling and all the other covariates specified above. We tested the validity of using exercise counseling as the instrumental variables based on the partial R2, and the χ2 test from the first-stage model, which is similar to the F test from the first stage regression (Staiger & Stock, 1997); the Sargan test was not performed since we only used one instrument (Greene, 2008). In the second-stage model, quitting behavior was estimated as a function of the predicted smoking cessation counseling from the first-stage model and all the other covariates specified above. The probit model without using the instrumental variable and the probit model with the instrumental variable were estimated by using the probit and ivprobit functions in Stata 10 (StataCorp, 2007). Statistical significance was defined by a p value < .05. We also conducted sensitivity analyses that controlled for logarithmically transformed changes in cigarette price between the time of the CTS2 survey and the time of the HCC2 survey and the addition of variables for presence of the specific ADM disorders. Cigarette prices were measured by the published state-specific average annual retail price (including generics; Orzechowski & Walker, 2007) and assigned to individual respondents by state of residence and year of survey response. This study was approved by the institutional review board at University of California Los Angeles with a waiver of informed consent.
Results
The all smokers cohort smoked an average of 15.9 cigarettes per day in the CTS2 survey. Among these, those who had quit smoking at the time of the HCC2 survey had smoked significantly less at the time of the CTS2 survey (p < .01, 10.7 vs. 17.1 cigarettes per day) than those who had not quit smoking. The ADM smokers cohort smoked significantly more at the time of the CTS2 survey (p < . 01, 17.0 vs. 14.9 cigarettes per day) than the non-ADM smokers cohort. Table 1 shows the ADM smokers cohort and non-ADM smokers cohort were equally likely to receive smoking cessation counseling (p not significant, 72.9% vs. 69.9%). However, the ADM smokers were less likely than non-ADM smokers to be successful quitters (p < .05, 17.1% vs. 22.0%). The two cohorts also significantly differed in several other characteristics, with ADM smokers more likely to receive exercise counseling (p < .01, 44.3% vs. 34.9%), to be younger, to live in the West, to have lower levels of education, to have lower levels of income, to be not married, to be unemployed, to be uninsured, and to be less physically active.
Table 1.
Successful Quit Status and Sociodemographic Characteristics for All Smokers, ADM Disorder Smokers, and Non-ADM Disorder Smokers
| All smokers cohort |
ADM disorder smokers cohort |
Non-ADM disorder smokers cohort |
p Value | ||||
| N | % | N | % | N | % | ||
| Total | 1,356 | 619 | 737 | ||||
| Successful quitter | 268 | 19.8 | 106 | 17.1 | 162 | 22.0 | <.05 |
| Smoking cessation counseling | 966 | 71.2 | 451 | 72.9 | 515 | 69.9 | NS |
| Exercise counseling | 531 | 39.2 | 274 | 44.3 | 257 | 34.9 | <.01 |
| Male gender | 504 | 37.2 | 246 | 39.7 | 258 | 35.0 | <.10 |
| Age | |||||||
| 18–24 | 83 | 6.1 | 50 | 8.1 | 33 | 4.5 | <.01 |
| 25–34 | 220 | 16.2 | 113 | 18.3 | 107 | 14.5 | |
| 35–44 | 350 | 25.8 | 180 | 29.1 | 170 | 23.1 | |
| 45–54 | 313 | 23.1 | 142 | 22.9 | 171 | 23.2 | |
| 55–64 | 240 | 17.7 | 97 | 15.7 | 143 | 19.4 | |
| 65+ | 150 | 11.1 | 37 | 6.0 | 113 | 15.3 | |
| Race/ethnicity | |||||||
| White | 1143 | 84.3 | 512 | 82.7 | 631 | 85.6 | NS |
| Black | 138 | 10.2 | 69 | 11.1 | 69 | 9.4 | |
| Other | 18 | 1.3 | 11 | 1.8 | 7 | 0.9 | |
| Hispanic | 57 | 4.2 | 27 | 4.4 | 30 | 4.1 | |
| Region of residence | |||||||
| Northeast | 333 | 24.6 | 139 | 22.5 | 194 | 26.3 | <.05 |
| Midwest | 325 | 24.0 | 143 | 23.1 | 182 | 24.7 | |
| South | 479 | 35.3 | 219 | 35.4 | 260 | 35.3 | |
| West | 219 | 16.2 | 118 | 19.1 | 101 | 13.7 | |
| Education | |||||||
| Less than high school | 191 | 14.1 | 105 | 17.0 | 86 | 11.7 | <.01 |
| High school | 957 | 70.6 | 435 | 70.3 | 522 | 70.8 | |
| College or higher | 208 | 15.3 | 79 | 12.8 | 129 | 17.5 | |
| US born | 1294 | 95.4 | 587 | 94.8 | 707 | 95.9 | NS |
| Household income | |||||||
| <$25,000 | 606 | 44.7 | 300 | 48.5 | 306 | 41.5 | <.01 |
| $25,000–$49,999 | 362 | 26.7 | 174 | 28.1 | 188 | 25.5 | |
| $50,000–$74,999 | 206 | 15.2 | 77 | 12.4 | 129 | 17.5 | |
| >$75,000 | 182 | 13.4 | 68 | 11.0 | 114 | 15.5 | |
| Marital status | |||||||
| Married | 693 | 51.1 | 267 | 43.1 | 426 | 57.8 | <.01 |
| Single | 548 | 40.4 | 293 | 47.3 | 255 | 34.6 | |
| Partner | 115 | 8.5 | 59 | 9.5 | 56 | 7.6 | |
| Unemployed | 131 | 9.7 | 88 | 14.2 | 43 | 5.8 | <.01 |
| Body mass index | |||||||
| <25.0 | 580 | 42.8 | 265 | 42.8 | 315 | 42.7 | <.10 |
| 25.0–30.0 | 443 | 32.7 | 186 | 30.0 | 257 | 34.9 | |
| >30.0 | 333 | 24.6 | 168 | 27.1 | 165 | 22.4 | |
| Health insurance | |||||||
| Private insurance | 859 | 63.3 | 346 | 55.9 | 513 | 69.6 | <.01 |
| Not insured | 178 | 13.1 | 107 | 17.3 | 71 | 9.6 | |
| Medicare | 196 | 14.5 | 94 | 15.2 | 102 | 13.8 | |
| Medicaid | 82 | 6.0 | 55 | 8.9 | 27 | 3.7 | |
| Other | 41 | 3.0 | 17 | 2.7 | 24 | 3.3 | |
| Physical activity | |||||||
| Not at all active | 59 | 4.4 | 36 | 5.8 | 23 | 3.1 | <.01 |
| A little/fairly | 703 | 51.8 | 375 | 60.6 | 328 | 44.5 | |
| Quite | 319 | 23.5 | 119 | 19.2 | 200 | 27.1 | |
| Very/extremely | 275 | 20.3 | 89 | 14.4 | 186 | 25.2 | |
Note. ADM disorder = alcohol, drug, or mental disorder. The p values are for differences between the ADM and non-ADM cohorts. “NS” stands for p > .10.
Table 2 shows the results from probit regression analyses of successful quitting for the all smokers cohort and the separate ADM smokers and non-ADM smokers cohorts. In the analyses without using the instrumental variable, there was a negative significant association between receipt of smoking cessation counseling in the past year with successful quitting (coefficient = −1.04, p < .01 for all smokers; coefficient = −0.93, p < .01 for ADM smokers, coefficient = −1.16, p < .01 for non-ADM smokers). The Durbin–Wu–Hausman specification test could not reject hidden bias in the analysis for all smokers (χ2 = 76.68, p < .01), for ADM smokers (χ2 = 54.04, p < .01), or for non-ADM smokers (χ2 = 52.59, p < .01), which suggests that using an instrumental variable approach to address hidden bias is appropriate.
Table 2.
Estimated Probit Regression Models of Successful Quitting
| Variable | Category | All smokers cohort |
ADM disorder smokers cohort |
Non-ADM disorder smokers cohort |
|||
| Analysis without instrumental variable | Exercise counseling as an instrumental variable | Analysis without instrumental variable | Exercise counseling as an instrumental variable | Analysis without instrumental variable | Exercise counseling as an instrumental variable | ||
| Smoking cessation counseling | Yes | −1.036*** | 0.879** | −0.925*** | 1.063** | −1.160*** | 0.863** |
| Gender | Female | 0.191* | 0.052 | −0.050 | −0.178 | 0.378** | 0.254* |
| Age | 25–34 | −0.184 | −0.185 | −0.102 | −0.257 | −0.271 | −0.107 |
| 35–44 | −0.480* | −0.595*** | −0.418 | −0.633** | −0.618* | −0.575* | |
| 45–54 | −0.382 | −0.526** | −0.485 | −0.648** | −0.373 | −0.470 | |
| 55–64 | −0.189 | −0.387* | −0.306 | −0.628* | −0.246 | −0.325 | |
| 65+ | 0.095 | −0.070 | 0.033 | −0.306 | 0.151 | 0.074 | |
| Race/ethnicity | Black | 0.372** | 0.461*** | 0.258 | 0.451* | 0.483* | 0.478** |
| Other | 0.183 | 0.270 | 0.239 | 0.346 | 0.195 | 0.207 | |
| Hispanic | 0.243 | 0.504** | −0.096 | 0.214 | 0.546 | 0.704** | |
| Region of residence | Midwest | −0.294* | −0.168 | −0.359 | −0.244 | −0.291 | −0.158 |
| South | −0.337** | −0.109 | −0.524** | −0.346* | −0.243 | 0.048 | |
| West | 0.066 | 0.167 | −0.012 | −0.026 | 0.076 | 0.272 | |
| Education | High school | 0.081 | 0.072 | −0.026 | 0.078 | 0.236 | 0.059 |
| College or higher | 0.384* | 0.291* | 0.624* | 0.574* | 0.393 | 0.154 | |
| US born | Yes | −0.201 | −0.107 | −0.284 | −0.273 | −0.277 | −0.061 |
| Household income | $25,000–$49,999 | 0.036 | −0.035 | −0.110 | −0.181 | 0.158 | 0.086 |
| $50,000–$75,000 | −0.130 | −0.080 | −0.403 | −0.377 | 0.035 | 0.090 | |
| >$75,000 | 0.014 | 0.066 | −0.419 | −0.355 | 0.296 | 0.307 | |
| Marital status | Single | −0.205* | −0.126 | −0.335* | −0.157 | −0.086 | −0.093 |
| Partner | 0.153 | 0.001 | 0.435 | 0.297 | −0.219 | −0.345 | |
| Unemployed | Yes | −0.248 | −0.256 | −0.228 | −0.243 | −0.340 | −0.320 |
| Body mass index | 25.0–30.0 | 0.109 | 0.067 | −0.128 | −0.043 | 0.294* | 0.174 |
| >30.0 | 0.177 | 0.092 | 0.016 | −0.050 | 0.329* | 0.252 | |
| Health insurance | Not insured | −0.209 | −0.034 | −0.401 | −0.052 | −0.034 | −0.020 |
| Medicare | −0.198 | −0.247 | −0.049 | −0.070 | −0.370 | −0.389 | |
| Medicaid | −0.405 | −0.324 | −0.313 | −0.244 | −0.697 | −0.530 | |
| Other | 0.400 | 0.380 | 0.677 | 0.611 | 0.222 | 0.180 | |
| Physical activity | A little/fairly | −0.458* | −0.357* | −0.100 | −0.201 | −1.089** | −0.596* |
| Quite | −0.574** | −0.431* | −0.237 | −0.234 | −1.194*** | −0.727* | |
| Very/extremely | −0.520* | −0.329 | −0.388 | −0.148 | −1.037** | −0.612* | |
Note. ADM disorder = alcohol, drug, or mental disorder. Reference categories are no counseling, male, age 18–24 years, non-Hispanic White, Northeast region, less than a high school degree, not born in the United States, annual household income less than $25,000, married, not unemployed, body mass index < 25, private health insurance coverage, and no physical activity. The coefficients and p-values in bold are for statistical significance.
*p < .05. **p < .01. ***p < .001.
When exercise counseling was included as an explanatory variable instead of smoking cessation counseling in the regression analyses of quitting, exercise counseling had a positive association with smoking cessation status for all smokers (coefficient = 0.19, p < .05), for ADM smokers (coefficient = 0.25, p < .10), and for non-ADM smokers (coefficient = 0.19, p < .10). In the first-stage regression model of the instrumental variable analyses in which smoking cessation counseling was as a function of past year PCP exercise counseling and other covariates, the χ2 test was 34.16 for all smokers, 13.35 for ADM smokers, and 24.26 for non-ADM smokers, suggesting that exercise counseling was a valid instrument. In the second-stage regression model, when exercise counseling was used as an instrumental variable for smoking cessation counseling, the predicted smoking cessation counseling by PCPs had a positive significant association with quitting for all smokers (coefficient = 0.88, p < .01), for ADM smokers (coefficient = 1.06, p < .01), and for non-ADM smokers (coefficient = 0.86, p < .01).
We used the probit regression results estimated by the instrumental variable approach to generate the predicted probabilities of quitting for two hypothetical situations: (a) if no study individuals received past year PCP smoking cessation counseling or (b) if study individuals all received past year PCP smoking cessation counseling. The predicted probabilities of quitting without smoking cessation counseling were 9.2% (95% CI: 6.1%–13.4%) for all smokers, 6.0% (95% CI: 2.9%–11.3%) for smokers with ADM disorders, and 10.5% (95% CI: 6.4%–16.3%) for smokers without ADM disorders. The predicted probabilities of quitting with smoking cessation counseling were 32.7% (95% CI: 22.6%–44.2%) for all smokers, 31.3% (95% CI: 16.1%–50.5%) for smokers with ADM disorders, and 34.9% (95% CI: 22.1%–49.6%) for smokers without ADM disorders.
Sensitivity analyses that included the changes in cigarette price between the time of the two surveys showed no change in the results for the association between smoking cessation counseling and successful quitting (all smokers coefficient = 0.87, p < .01; ADM smokers coefficient = 1.06, p < .01; non-ADM smokers coefficient = 0.85, p < .01). Sensitivity analyses that included specific ADM disorders also showed no change in the results for the association between smoking cessation counseling and successful quitting (all smokers coefficient = 0.98, p < .01; ADM smokers coefficient = 1.17, p < .01).
Discussion
It has been suggested that as many as 200,000 of the 435,000 deaths from smoking in the United States occur among individuals with ADM disorders (Schroeder, 2009). Although instrumental variable analyses have been previously used with cross-sectional data to demonstrate the effectiveness of PCP smoking cessation counseling on successful quitting among smokers in the general population (Bao et al., 2006), this is the first study to demonstrate that past year PCP smoking cessation counseling is positively associated with successful quitting among smokers with ADM disorders. Previous studies on smoking cessation for individuals with ADM disorders have not focused on primary care settings (El-Guebaly, Cathcart, Currie, Brown, & Gloster, 2002); this study provides evidence for the effectiveness of for PCPs counseling on smoking cessation among all smokers, including those with ADM disorders.
Findings from an instrumental variable analysis are not generalizable to the entire study population. Instead, the findings indicate the effect among the subset of population (the “marginal patients”) who received different treatments based on the randomization from the instrumental variables (Bao et al., 2006; Buntin, Colla, Deb, Sood, & Escarce, 2010). In our study, as in the prior study using similar instrumental variables, the ‘‘marginal patients’’ are those who were counseled on smoking cessation because their providers counseled them on exercise and carried the pattern to smoking cessation. Additional studies are needed to determine whether these findings also apply to those individuals who are “nonmarginal” (Bao et al., 2006).
The generalizability of our findings to all smokers with ADM disorders is also limited by the study sample. Our analyses were restricted to those individuals who visited a general medical provider in the year prior to the HCC2 interview and individuals needed to be dwelling in the community with a telephone to be in the survey sampling frame. As a result, our findings may not extend to the full spectrum of smokers with ADM disorders, particularly those who do not access primary care, nor to those who are institutionally housed or homeless. Additional studies are needed to explore the effectiveness of primary care smoking cessation interventions among smokers with ADM disorders those who do not routinely use primary care and among those who are institutionally housed or homeless.
The predicted probability of successful quitting in this analysis is higher than what might be expected from smoking cessation counseling alone since most studies suggest a baseline 4%–7% annual quit rate without assistance (Fiore et al., 2008), and physician counseling alone in studies is only 1.3 times as likely to result in smoking cessation as no advice to quit or 10.2% versus 7.9% (Fiore et al., 2008). However, we are not able to identify whether individuals used other smoking cessation aids as a result of physician counseling, such as nicotine replacement therapy or bupropion. Use of these aids would increase the likelihood of smoking cessation; the combination of counseling (not just brief physician counseling) and medication is 1.7 times as likely to result in smoking cessation as counseling alone or 22.1% versus 14.6% (Fiore et al., 2008). In addition, the time interval between the CTS2 and HCC2 surveys, essentially 2 years, may also result in higher predicted probabilities of smoking cessation than what would be seen with a 1-year interval due to repeated quit attempts. Further studies using shorter time intervals are needed to confirm the relationship between smoking cessation counseling and subsequent quitting among individuals with ADM disorders.
As our data are from a survey of individuals from 2000 to 2001, it is possible that this relationship between smoking cessation counseling and quitting behavior may have changed over time. The past decade has seen many states increase their cigarette taxes to even greater levels than during the 1990s; (Orzechowski & Walker, 2007) since ADM smokers in this survey have been shown to be sensitive to cigarette prices (Ong, Zhou, & Sung, 2010). ADM smokers who are both price sensitive and see PCPs on a regular basis may have been induced to quit smoking. Additional studies using more recent data will be needed to confirm that individuals with ADM disorders are still likely to quit smoking after receiving smoking cessation counseling by PCPs.
Our measures of smoking status were obtained by self-report which is not as accurate as biological markers such as cotinine (Burling & Burling, 2003; Perez-Stable, Benowitz, & Marin, 1995). However, prior studies have shown that self-report is a reasonable measure of smoking behavior when compared with biologic markers (Patrick et al., 1994). Since the HCC2 survey did not ask amount of cigarette consumption, we cannot ascertain whether individuals reduced their cigarette use. However, complete cessation is a reasonable outcome since even low levels of smoking engender health risks (Pechacek & Babb, 2004). Our measure of smoking cessation intervention only measures receipt of a discussion on quitting smoking and should not be considered equivalent to receipt of a full smoking cessation intervention such as the 5 A’s (Fiore et al., 2008) or even “Ask, Advise, Refer” (Schroeder, 2005). However, it is encouraging to see a positive association with smoking cessation even with this lower level of intervention.
Although our measure of psychosis is a lifetime and not a past year measure as the other ADM measures, neither this did result in a high proportion of individuals with psychosis in our study sample nor did this group strongly influence our findings. Our inclusion of binge drinking and substance use in our definition of ADM disorder includes some individuals who have episodes of heavy drinking or who use drugs illicitly but without any evidence of experiencing problems resulting from such use, which defines a disorder. Unfortunately, the limits of the survey do not allow us to differentiate between individuals with these problems who do or do not have problems from such use. Future studies are needed to more definitively evaluate effects among individuals with these alcohol and substance use disorders. Our measure of binge drinking does not match the current definitions of binge drinking (five or more drinks for men, four or more drinks for women), as its threshold is at a higher level of drinks (six or more drinks regardless of gender). As a result, our measure includes those who drink more on a given occasion but may miss individuals who would currently be considered binge drinkers. Additional studies with data based on the current definition of binge drinking may be helpful in determining whether the relationship also exists for these additional binge drinkers not identified in our data.
Using the instrumental variable approach, our study results show that past year PCP counseling is associated with successful quitting among smokers with ADM disorders. Most smokers with ADM disorders want to quit smoking (Schroeder, 2009). Smokers with ADM disorders should continue to be targeted for smoking cessation counseling, particularly by PCPs. Future prospective studies should be conducted to verify a causal relationship between smoking cessation counseling and actual smoking cessation in this population, which is critical to the successful reduction of the health burden of tobacco.
Funding
Robert Wood Johnson Foundation’s Substance Abuse Policy Research Program (#61104); a Jonsson Cancer Center Foundation at the University of California, Los Angeles research seed grant; the University of California, Los Angeles National Institute of Mental Health Partnered Research Center for Quality Care (P30 MH082760).
Declaration of Interests
None declared.
Acknowledgments
We also appreciate the assistance of Lily Zhang, M.S., for assisting us with the matching of respondents between the two surveys.
References
- Adhikari B, Kahende J, Malarcher A, Pechacek T, Tong V. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. Morbidity and Mortality Weekly Report. 2008;57:1226–1228. doi:mm5745a3. [PubMed] [Google Scholar]
- Bao Y, Duan N, Fox SA. Is some provider advice on smoking cessation better than no advice? An instrumental variable analysis of the 2001 National Health Interview Survey. Health Services Research. 2006;41:2114–2135. doi: 10.1111/j.1475-6773.2006.00592.x. doi:10.1111/j.1475-6773.2006.00592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N. Psychiatric comorbidity of smoking and nicotine dependence. Behavior Genetics. 1995;25:95–101. doi: 10.1007/BF02196920. doi:10.1007/BF02196920. [DOI] [PubMed] [Google Scholar]
- Buntin MB, Colla CH, Deb P, Sood N, Escarce JJ. Medicare spending and outcomes after postacute care for stroke and hip fracture. Medical Care. 2010;48:776–784. doi: 10.1097/MLR.0b013e3181e359df. doi:10.1097/MLR.0b013e3181e359df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burling AS, Burling TA. A comparison of self-report measures of nicotine dependence among male drug/alcohol-dependent cigarette smokers. Nicotine & Tobacco Research. 2003;5:625–633. doi: 10.1080/1462220031000158708. doi:T4TK07BD0NVH8MG9. [DOI] [PubMed] [Google Scholar]
- Center for Studying Health System Change. Community Tracking Study Household Survey, 1998–1999 and Followback Survey, 1998–2000. 2nd Inter-university Consortium for Political and Social Research version ed. Washington, DC: 2002. [Google Scholar]
- Durbin J. Errors in variables. Review of the International Statistical Institute. 1954;22:23–32. [Google Scholar]
- Eisenberg D, Quinn BC. Estimating the effect of smoking cessation on weight gain: An instrumental variable approach. Health Services Research. 2006;41:2255–2266. doi: 10.1111/j.1475-6773.2006.00594.x. doi:10.1111/j.1475-6773.2006.00594.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Guebaly N, Cathcart J, Currie S, Brown D, Gloster S. Smoking cessation approaches for persons with mental illness or addictive disorders. Psychiatric Services. 2002;53:1166–1170. doi: 10.1176/appi.ps.53.9.1166. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaén CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: Public Health Service; 2008. [Google Scholar]
- Glassman AH, Helzer JE, Covey LS, Cottler LB, Stetner F, Tipp JE, et al. Smoking, smoking cessation, and major depression. Journal of the American Medical Association. 1990;264:1546–1549. doi:10.1001/jama.1990.03450120058029. [PubMed] [Google Scholar]
- Goff DC, Henderson DC, Amico E. Cigarette smoking in schizophrenia: Relationship to psychopathology and medication side effects. American Journal of Psychiatry. 1992;149:1189–1194. doi: 10.1176/ajp.149.9.1189. [DOI] [PubMed] [Google Scholar]
- Gonzalez-Pinto A, Gutierrez M, Ezcurra J, Aizpuru F, Mosquera F, Lopez P, et al. Tobacco smoking and bipolar disorder. Journal of Clinical Psychiatry. 1998;59:225–228. doi: 10.4088/jcp.v59n0503. [DOI] [PubMed] [Google Scholar]
- Greene WH. Econometric analysis. 6th ed. Upper Saddle River, NJ: Pearson Prentice Hall; 2008. [Google Scholar]
- Harris EC, Barraclough B. Excess mortality of mental disorder. British Journal of Psychiatry. 1998;173:11–53. doi: 10.1192/bjp.173.1.11. doi:10.1192/bjp.173.1.11. [DOI] [PubMed] [Google Scholar]
- Hausman J. Specification tests in econometrics. Econometrica. 1978;46:1251–1271. [Google Scholar]
- Kelly C, McCreadie RG. Smoking habits, current symptoms, and premorbid characteristics of schizophrenic patients in Nithsdale, Scotland. American Journal of Psychiatry. 1999;156:1751–1757. doi: 10.1176/ajp.156.11.1751. [DOI] [PubMed] [Google Scholar]
- Kilbourne AM, Morden NE, Austin K, Ilgen M, McCarthy JF, Dalack G, et al. Excess heart-disease-related mortality in a national study of patients with mental disorders: Identifying modifiable risk factors. General Hospital Psychiatry. 2009;31:555–563. doi: 10.1016/j.genhosppsych.2009.07.008. doi:10.1016/j.genhosppsych.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klesges RC, Meyers AW, Klesges LM, La Vasque ME. Smoking, body weight, and their effects on smoking behavior: A comprehensive review of the literature. Psychological Bulletin. 1989;106:204–230. doi: 10.1037/0033-2909.106.2.204. doi:10.1037/0033-2909.106.2.204. [DOI] [PubMed] [Google Scholar]
- Klesges RC, Winders SE, Meyers AW, Eck LH, Ward KD, Hultquist CM, et al. How much weight gain occurs following smoking cessation? A comparison of weight gain using both continuous and point prevalence abstinence. Journal of Consulting and Clinical Psychology. 1997;65:286–291. doi: 10.1037//0022-006x.65.2.286. doi:10.1037/0022-006X.65.2.286. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. doi:10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- McClellan M, McNeil BJ, Newhouse JP. Does more intensive treatment of acute myocardial infarction in the elderly reduce mortality? Analysis using instrumental variables. Journal of the American Medical Association. 1994;272:859–866. doi:10.1001/jama.1994.03520110039026. [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. doi:10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: Actual causes of death in the United States, 2000. Journal of the American Medical Association. 2005;293:293–294. doi: 10.1001/jama.293.3.293. doi:10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- Ong MK, Zhou Q, Sung H-Y. Cigarette price sensitivity of individuals with alcohol, drug, or mental disorders. American Journal of Public Health. 2010;100:1243–1245. doi: 10.2105/AJPH.2009.159962. doi:10.2105/AJPH.2009.159962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orzechowski W, Walker RC. The tax burden on tobacco. Vol. 42. Arlington, VA: Author; 2007. [Google Scholar]
- Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: A review and meta-analysis. American Journal of Public Health. 1994;84:1086–1093. doi: 10.2105/ajph.84.7.1086. doi:10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pechacek TF, Babb S. How acute and reversible are the cardiovascular risks of secondhand smoke? British Medical Journal. 2004;328:980–983. doi: 10.1136/bmj.328.7446.980. doi:10.1136/bmj.328.7446.980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Stable EJ, Benowitz NL, Marin G. Is serum cotinine a better measure of cigarette smoking than self-report? Preventive Medicine. 1995;24:171–179. doi: 10.1006/pmed.1995.1031. doi:S0091743585710316. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. doi:10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schroeder SA. What to do with a patient who smokes. Journal of the American Medical Association. 2005;294:482–487. doi: 10.1001/jama.294.4.482. doi:10.1001/jama.294.4.482. [DOI] [PubMed] [Google Scholar]
- Schroeder SA. A 51-year-old woman with bipolar disorder who wants to quit smoking. Journal of the American Medical Association. 2009;301:522–531. doi: 10.1001/jama.2008.982. doi:10.1001/jama.2008.982. [DOI] [PubMed] [Google Scholar]
- Staiger D, Stock JH. Instrumental variables regression with weak instruments. Econometrica. 1997;65:557–586. [Google Scholar]
- StataCorp. Stata statistical software: Release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- Stukel TA, Fisher ES, Wennberg DE, Alter DA, Gottlieb DJ, Vermeulen MJ. Analysis of observational studies in the presence of treatment selection bias: Effects of invasive cardiac management on AMI survival using propensity score and instrumental variable methods. Journal of the American Medical Association. 2007;297:278–285. doi: 10.1001/jama.297.3.278. doi:10.1001/jama.297.3.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturm R, Gresenz C, Sherbourne C, Minnium K, Klap R, Bhattacharya J, et al. The design of Healthcare for Communities: A study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry. 1999;36:221–233. [PubMed] [Google Scholar]
- Unutzer J, Schoenbaum M, Druss BG, Katon WJ. Transforming mental health care at the interface with general medicine: Report for the presidents commission. Psychiatric Services. 2006;57:37–47. doi: 10.1176/appi.ps.57.1.37. doi:10.1176/appi.ps.57.1.37. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2008 Physical activity guidelines for Americans. Rockville, MD: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. New England Journal of Medicine. 1991;324:739–745. doi: 10.1056/NEJM199103143241106. [DOI] [PubMed] [Google Scholar]
- Wu DM. Alternative tests of independence between stochastic regressors and disturbances. Econometrica. 1973;41:733–750. [Google Scholar]
- Ziedonis D, Hitsman B, Beckham JC, Zvolensky M, Adler LE, Audrain-McGovern J, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine & Tobacco Research. 2008;10:1691–1715. doi: 10.1080/14622200802443569. doi:10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]


