Abstract
Background
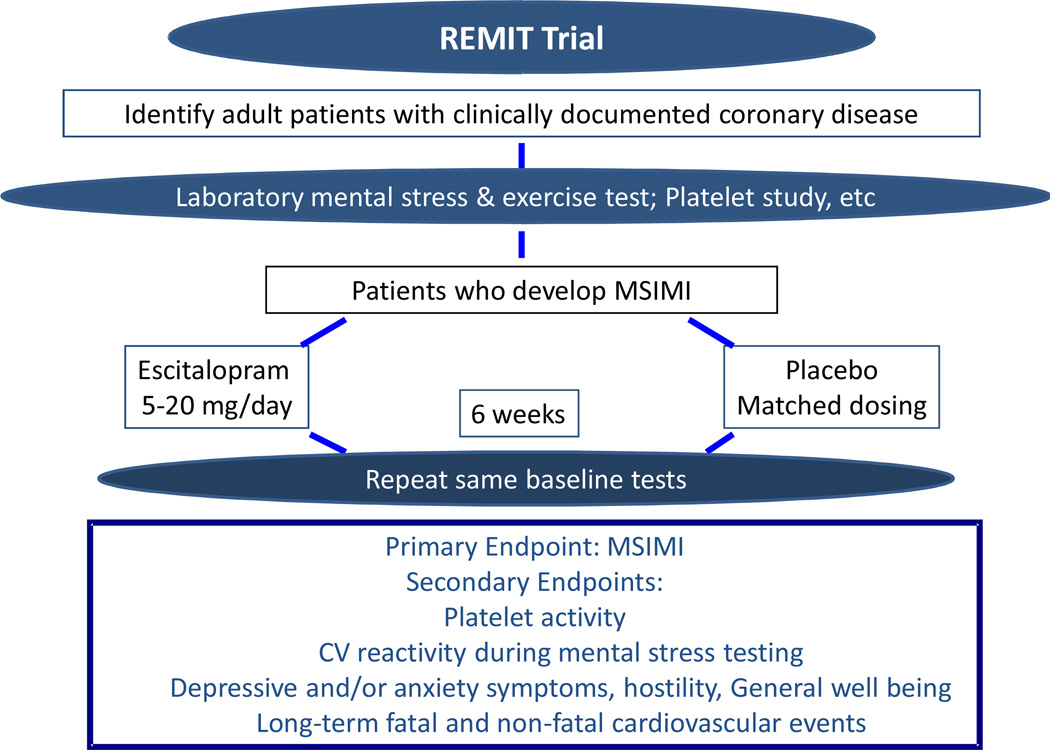
Mental stress induced myocardial ischemia (MSIMI) is common in patients with clinically stable coronary heart disease (CHD) and is associated with poor outcomes. Depression is a risk factor of MSIMI. The Responses of Mental Stress Induced Myocardial Ischemia to Escitalopram Treatment (REMIT) trial investigates whether selective serotonin reuptake inhibitor (SSRI) treatment can improve MSIMI. The rationale and outline of the study are described.
Method
In this single center randomized clinical trial, adult patients with clinically stable CHD are recruited for baseline mental and exercise stress testing assessed by echocardiography. Additionally, psychometric questionnaires are administered and blood samples are collected for platelet activity analysis. Patients who demonstrate MSIMI, defined by new abnormal wall motion, ejection fraction reduction ≥8%, and/or development of ischemic ST change in electrocardiogram during mental stress testing, are randomized at a 1:1 ratio to escitalopram or placebo for 6 weeks. Approximately 120 patients with MSIMI are enrolled in the trial. The stress testing, platelet activity assessment and psychometric questionnaires are repeated at the end of the 6-week intervention. The hypothesis of the study is that SSRI treatment improves MSIMI via mood regulation and modification of platelet activity.
Conclusion
The REMIT study examines the effect of SSRI on MSIMI in vulnerable CHD patients and probes some potential underlying mechanisms.
Introduction
Substantially accumulated evidence demonstrates that transient emotional distress or mental stress is strongly linked to coronary heart disease (CHD) 1. Over the last couple of decades, the association of mental activity and myocardial ischemia has been well studied. Mental stress induced myocardial ischemia (MSIMI) in the laboratory may occur in up to 70% in patients with clinically stable CHD2 and is associated with increased death and cardiovascular (CV) events3–4. Despite this, few studies have examined therapeutics that effectively modify MSIMI. We therefore are conducting a clinical trial, i.e. the Responses of Mental Stress Induced Myocardial Ischemia to Escitalopram Treatment (REMIT) trial, to investigate whether selective serotonin reuptake inhibitor (SSRI) treatment can improve MSIMI. The methods and rationale of the study are described.
Methods
Overall Trial Design
The REMIT study is a National Heart, Lung, and Blood Institute (NHLBI) sponsored, prospective, randomized, double-blind, placebo-controlled study that is designed to assess the efficacy of escitalopram on MSIMI in patients with CHD (Figure 1). The pharmaceutical company, Forest Laboratories, Inc. provides the study drug and the matched placebo only. The trial is registered at www.clinicaltrials.gov, registry number: NCT00574847.
Figure 1.
Study Design
This study also examines the effects of escitalopram on platelet activity, depression and anxiety symptoms, and CV response to stress in relationship to MSIMI. All assessments are conducted at baseline prior to study medication and at the end of 6-week intervention before the medication is tapered off (Figure 1).
Trial Population and Recruitment
The study population consists of approximate 120 adult patients (men or women) with clinically stable CHD and MSIMI. Patients with documented CHD, by angiographic finding of coronary artery stenosis ≥ 70%, history of myocardial infarction, or status post re-vascular procedures, such as coronary artery bypass graft surgery, or stenting are recruited for mental stress testing after consent. Only patients who develop MSIMI qualify for the trial, regardless of whether they are clinically depressed. The exclusion criteria of the study are listed in Table 1.
Table 1.
REMIT Inclusion/Exclusion Criteria
| Inclusion Criteria |
|
| Exclusion Criteria |
|
Mental Stress/Exercise Testing and Assessment of Stress Induced Myocardial Ischemia
Mental Stress and Exercise Testing
The stress testing is conducted at the Duke Cardiac Diagnostic Unit. Beta-blockers are withheld for 24–48 hours depending on the half life of these medications prior to the stress testing. Following a 20-minute rest period, participants are asked to complete a series of 3 mental stress tasks, i.e. 1) Mental arithmetic, 2) Public speaking with anger recall, and 3) Mirror trace. The use of multiple stressors allows for better identification of patients with MSIMI, as compared to the use of a single task. A rest period of 6 minutes follows every stress test. After the mental stress testing, patients undergo a treadmill exercise test using the standard Bruce protocol. The exercise testing is terminated according to the guidelines of the American College of Sports Medicine. The same testing is repeated at the 6-week endpoint visit, with one variation; an alternate mental arithmetic task is used to prevent habituation.
Myocardial Ischemia Assessment
Echocardiography5 and electrocardiography (ECG) are used to assess for an ischemic activity. Digital acquisition of echo imaging is obtained during the last 3 minutes of baseline resting period, during each mental stress test, and at the peak of exercise testing for 3 minutes. Images (parasternal long-axis and short-axis views and apical 4-chamber and 2-chamber views) are acquired with a 3 MHz transducer in the harmonic imaging mode with a Phillips iE33 system (Bothell, WA, USA). Doppler Tissue Imaging is used to measure the mitral annular movement and pulsed-Doppler imaging is used to measure transmitral flow. Left ventricular ejection fraction (LVEF) is calculated from a 3–5 beat loop and wall motion assessments are determined from 30–40 frames of systole from one cardiac cycle. Blood pressure, heart rate, and standard 12-lead ECG are measured simultaneously during the acquisition of the echo images.
REMIT Definition of Stress Induced Myocardial Ischemia
MSIMI is defined by the following: compared to rest, 1) any development or a worsening of wall motion; 2) reduction of LVEF ≥8%4 and/or; 3) deviation (depression or elevation) of ST-segment of ECG in 2 or more leads lasting for ≥3 consecutive beats, occurring during least one of the 3 mental stress tasks. If any of the above occurs during exercise testing, compared to rest, it is exercise induced myocardial ischemia.
Left ventricular wall motion is assessed using the American Society of Echocardiography recommended 16-segment model. Each segment is graded and scored based on either normal (normal or hyperdynamic, score = 0) or abnormal (hypokinetic, akinetic, or dyskinetic; scores = 1, 2, or 3, respectively) wall motion. Wall motion score index (WMSI), the sum of wall motion scores divided by the total number of segments scored, is calculated at rest, during each mental stress task and during the exercise test. This scoring system has been validated by other investigators with coefficients of correlation for intra-observer and inter-observer variability of 0.81 and 0.84, respectively5.
LVEF is calculated by measuring the images of the two apical windows (parasternal long axis, apical 4-chamber, and apical 2 chamber) via the biplane Simpson’s method6.
Randomization and Management of Study Drug
Patients who develop MSIMI during the laboratory testing are randomized to escitalopram or placebo at a 1:1 ratio for a 6-week period. The dose of the study medication begins at 5mg is titrated up to 10mg in one week, and then up to 20mg in two weeks. For patients who are not able to tolerate the titration, the dose may be reduced to the lowest dose of 5mg. If a patient is unable to tolerate the lowest dose, his or her participation in the study intervention is discontinued. For patients who have difficulty tolerating the study drug, and the side effects are not severe or life threatening, a brief medication taper and retry within one week may be conducted. Participants are assessed weekly via phone/and or clinic visit. Study medication compliance and pill counts are assessed as well. Following the end of 6-week intervention assessment, participants are instructed to taper the study medication to 10mg for the first week and 5 mg for the second week before terminating the medication completely.
Long-term Follow Up
All patients, irrespective of 6-week study treatment completion, are contacted yearly for long-term follow-up, CV outcome status, and medication use, until the last participant enrolled completes his or her 3-year follow up. At the end of the 6-week trial intervention, participants who request to continue on the study medication are provided a 30-day escitalopram prescription and are advised to follow-up with their primary care physician or cardiologist for further use of the medication.
Primary Endpoints
The primary study endpoint is the improvement, worsening, or no change in MSIMI at the end of 6 weeks of treatment compared to the baseline assessment between the two groups.
For the evaluation of the primary study endpoint, a side by side comparison of the echocardiographic images obtained at the baseline and at the 6-week endpoint to determine wall motion changes is first conducted by two experienced echocardiologists separately who are blinded to the treatment assignment and the order of mental stress tasks. In the event of disagreement of wall motion read, a consensual review/scoring is conducted by the two echocardiologists.
Difference of LVEF is compared between baseline and 6-week echocardiogram images. Definition of MSIMI Changes. Compared to MSIMI at baseline, reduction of total WMSI or frequency of LVEF reduction ≥ 8%, and/or disappearance of ischemic ST-segment deviation during mental stress tasks, compared to baseline, is considered an improvement of MSIMI; Increase in total WMSI or frequency of LVEF reduction ≥ 8%, and/or newly emerged ischemic ST-segment deviation during mental stress tasks is considered as worsening of MSIMI. In the event that there are no changes in WMSI total score, LVEF or ECG after the end of the 6-week intervention, it is considered as no change in MSIMI.
Other Study Endpoints
LVEF Changes
Change of actual LVEF between baseline and end of 6-week intervention is a secondary endpoint.
Platelet Activity Assessment
Blood samples are collected both at baseline and at the end of 6-week intervention. The first blood draw occurs prior to stress testing, after a 10 minute quiet and undisturbed resting period following catheter insertion to allow hormone levels to return to normal after venipuncture. Blood samples are also collected immediately after the third mental task. Blood is drawn into tube heparin and glutathione for anticoagulation and preservation of catecholamine and transferred immediately to the platelet assessment laboratory at room temperature. All tests are performed in mornings to eliminate circadian influence on stress responses and platelet aggregability.
Platelet aggregation
Platelet-rich plasma (PRP) is separated in the lab via centrifugation for 10 minutes at 160g. PRP is then adjusted to 250,000 platelets/µL with autologous platelet-poor plasma for use in a BIO-DATA 4-channel platelet aggregometer. One hundred percent aggregation is the optical density obtained with platelet-poor plasma. Aggregation triggered by epinephrine (1, 2, 5 and 10µM), serotonin (0.3–30 µM), collagen (1, 2, 5 and 10 µg/ml) and ADP (0.1, 0.5, 1 µM) as well as each agonist combined with serotonin (10 µg/ml) is evaluated.
Platelet Serotonin Uptake
Platelet serotonin uptake is conducted as described by Slotkin et al.7. Aliquots of platelet are diluted in modified Krebs-Henseleit buffer (calcium free containing 2mM EDTA and pargyline, 100uM) and indicated with 3H serotonin [1,2- 3H(N)] with or without imipramine. Samples are incubated for 10 min at 37°C with a range of serotonin concentrations (5nM-1uM) and Bmax and Km determined by nonlinear regression algorithm for sigmoid curves with Prism 3.0 (Graphpad, San Diego CA). Platelet is trapped on Whatman GF/C filters (Cardiff, UK) and 251 Q5 washed by vacuum filtration with ice-cold phosphate-buffered 252 saline and counted by liquid scintillation spectrum with a 253 non–toluene-based fluor.
Platelet Transporter Binding
Platelet serotonin transporter binding is quantitated with 3H paroxetine binding as described by Nemeroff8 and modified by Slotkin and colleagues7. The platelet-rich pellet is lysed by suspension into 5mmol Tris buffer (pH 7.5) containing 5mM EDTA, pH 7.5, sedimented at 39,000 X G suspended in 70mM Tris (pH 7.5), resedimented, and finally resuspended in the assay buffer (50mmol Tris [pH 7.5] containing 120 mmol NaCl and 5mmol KCl). Binding of 3H-paroxetine to platelet membranes is accomplished by incubating aliquots of platelet membranes in seven different concentrations of 3H-paroxetine (25, 50, 100, 250, 500, 1,000pM) in triplicate using 100ug of platelet protein/tube in a final volume of 250ul assay buffer. Tubes are incubated on ice for 60 minutes after which 5ml of ice-cold buffer are added and labeled membranes harvested by vacuum filtration on Whatman GF/C glass fiber papers, pre-soaked in 0.05% polyethyleneimine. Filters are washed three times with 5ml of ice-cold buffer, and filter papers counted by liquid scintillation spectrometry using a non-toluene based fluor (Safety Solve). Binding as analyzed by nonlinear regression algorithm for sigmoid curves with Prism 3.0 (Graphpad, San Diego CA) is used to determine the Kd and Bmax of binding. Non-specific binding was determined as the binding in the presence of 0.22 mM serotonin.
Other Measurements
Cardiovascular (CV) Reactivity
The difference of blood pressure and heart rate obtained between rest and during stress are used as the CV reactivity.
Beck Depression Inventory (BDI)
The 21-item BDI was developed to assess the presence and severity of symptoms of depression in CHD population and prognostic associations.
Center for Epidemiologic Studies Depression Scale (CES-D)
The CES-D is a 20-item, self-administered questionnaire to assess the presence and severity of depressive symptoms. It is used to validate the previous findings that depression is associated with increased likelihood of MSIMI9 and to further explore the association of MSIMI and severe depression.
State-Trait Anxiety Inventory (STAI)
The STAI is one of the most commonly used self-administered scales for anxiety assessment in medically ill patients.
Cook-Medley Hostility Scale (Ho scale)
The Ho scale10 has been used to evaluate potential health consequences of hostility11 and is correlated with anger proneness, cynicism, and mistrust of others12. The adverse association of depression and MSIMI may be mediated by hostility.
Perceived Stress Scale (PSS)
The PSS is the most widely used psychological instrument to measure the degree to which situations in one’s life are appraised as stressful during the last month. Items were designed to determine how unpredictable, uncontrollable, and overloaded respondents find their lives.
General Well Being Scale (GWBS)
The GWBS is commonly used in health research and contains 6 subscales (depressed mood, anxiety, general health, vitality, emotional self control, and a sense of positive well-being). These items have been demonstrated to be highly stable over time. This scale has been validated by several studies in the general population as well as among CHD patients to particularly measure vitality and positive emotions13.
Statistical Analysis
Sample Size Consideration
The primary outcome is to compare a trichotomized variable, i.e., the rates of the improvement vs. worsening vs. no change of MSIMI at the end of 6-week treatment from baseline assessment between the escitalopram and the placebo groups. Based on an estimate of a 30% reduction in MSIMI in the placebo group and over 60% reduction in the group randomized to escitalopram, with alpha = 0.05, the targeted enrollment of 120 participants who all have MSIMI at baseline will provide a power of over 80%, with up to 10 drop-outs, for the estimated between group differences (2-sided statistical test). The total enrollment will increase if drop-out is greater than 10 to guarantee 110 participants who complete both baseline and 6-week assessments.
Analysis of Primary Endpoint
The initial analysis aims at the treatment effects on the primary endpoint: MSIMI change following 6-week intervention between two groups compared to baseline. The primary analysis of the study is conducted on the intent-to-treat (ITT) involving all randomized patients, with per-protocol analyses planned for the “treated” cases (who complete the 6-week intervention and 6-week assessment). The chi-square test is primarily used to compare the difference in the proportion of presence or absence of MSIMI improvement (binary outcome), followed by a multinomial logistic regression model with worsening outcome as the reference group. One caveat is that the main analysis may require the use of Mantel-Haenszel chi-square tests or multinomial logistic regression models instead of chi-square tests in the event that the randomization procedures failed to balance the two treatment groups with regard to baseline characteristics, such as age, sex, and baseline LVEF. All significance of the test will be assessed at level 0.05.
Analysis of Mediators
Once the main analysis is completed, supplemental analyses will be used to further examine the influence of other explanatory variables or mediators on the outcome. We will evaluate 1) the associations or extent to which the measures, such as platelet activity, depression, anxiety, and hostility, etc., mediate the occurrence of MSIMI; 2) the alteration of these variables by the trial intervention; 3) the role that the changes in these variables mediate the change of MSIMI; and 4) the mediator and treatment indicator simultaneously as predictors of the long term outcome of interest.
Treatment Effect on Long-term Clinical Outcomes
The Cox proportional hazards model is used to evaluate the effect of treatment on the composite endpoint of death or first cardiac-related hospitalization. Patients who have not experienced an event by the end of the follow-up period will be coded as censored at the time of last contact.
Discussion
The REMIT trial is the first clinical trial to examine the effects of an SSRI on MSIMI in patients with clinically stable CHD. The rationale for use of an SSRI to reduce MSIMI include 1) depressive symptoms are associated with MSIMI, 2) negative emotions are associated with daily ischemic activity, 3) stress management but not conventional anti-angina medications improves MSIMI, and 4) while mental stress enhances platelet activity, SSRI reduces platelet activity.
Mental Stress Testing and MSIMI in CHD Patients
Investigators have demonstrated consistently that mental stress elicits myocardial ischemia in patients with documented CHD3–4, 14–16. Approximately 20% to 70% CHD patients exhibit ischemia during mental stress testing2. This wide variation in the prevalence of ischemia is attributed to the measurement technique used to detect ischemia, the number and type of mental stress tasks, whether patients received anti-ischemic medication prior to testing, and when the study was conducted. A patient who develops MSIMI does not necessarily demonstrate exercise-induced ischemia, and vice versa3.
Unique Features and Clinical Significance of MSIMI
In contrast to exercise-induced ischemia, MSIMI occurs at lower heart rates, higher diastolic blood pressure, and much lower double products; the result of systolic pressure multiplied by heart rate. MSIMI is silent most of the time and rarely results in ischemic ECG changes 16. Systemic vascular resistance increases significantly during mental stress17, but declines during exercise testing.
MSIMI has been found to consistently predict increased adverse cardiac events3–4, 18–19. In a sample of 126 CHD patients with a positive exercise test, we found MSIMI was associated with increased cardiac events during a 5-year follow-up (odds ratio [OR] 2.8; 95% confidence interval [CI] 1.0–7.7; p<0.05), independent of conventional risks3. However, exercise-induced ischemia did not predict for adverse cardiac events (OR, 1.5; 95% CI, 0.6–3.9; p=.39) in this study. Sheps et al. demonstrated that mental stress-induced ischemia was associated with an almost 3-fold increase in mortality in CHD patients4.
Underlying Mechanisms of MSIMI
Mental stressors provoke constriction of coronaries that have a stenotic lesion or endothelial injury. Yeung et al.20 assessed the change of coronary blood flow during mental stress testing and endothelium-dependent vasodilatation by means of intra-coronary Doppler in a group of CHD patients. Responses of the coronary arteries varied from 38% constriction to 29% dilation, with coronary blood flow ranging from a decrease of 48% to an increase of 42% under mental stress compared to baseline 20. Compared to individuals without CHD, the coronary microcirculation of CHD patients did not dilate during mental stress testing21
Activation of certain regions of the brain and neuro-hormones released during emotional arousals are thought to be the mediators of this pathological process22–23. Accelerated platelet aggregation triggered by mental stress is a key element in the underlying pathological process, especially in individuals who are under chronic stress24–28. Heightened platelet activation in acute coronary syndrome (ACS) has been well supported in literature and is the reason that Aspirin and other anti-platelet activity agents are used in patients with acute coronary syndrome and other forms of CHD. While depression is evidently a significant risk factor for CHD development and for poor prognosis of CHD29, occurrence of MSIMI and myocardial ischemic activity during daily life are found to be related to negative emotions30. Patients with greater depressive symptoms had higher likelihood of developing MSIMI but not exercise-induced ischemia9. In addition, depression has been associated with heightened platelet activity25.
Therapeutic Modalities Treating MSIMI
Despite the clinical significance of MSIMI, investigation of therapeutic modalities to improve MSIMI is limited. There have been only two pharmacological studies that have explored the effects of beta-blockers and calcium channel blockers on MSIMI31–32. However, both studies failed to demonstrate the effectiveness of these interventions in MSIMI treatment. In a study31 with 19 CHD patients who received metoprolol or placebo in a cross-over design for 4 weeks, the beta-blocker was found to effectively reduce exercise-induced wall motion abnormalities but not mental stress induced wall motion abnormalities. Andrews et al.32 tested the effects of nifedipine gastrointestinal therapeutic system (GITS) or atenolol on MSIMI in 15 CHD patients, also using a cross-over design with a placebo control. These two medications did not change the LVEF response to mental stress tests compared to placebo (p=0.94). In a further examination among 5 subjects who had greater LVEF reduction to mental stress during placebo, the authors reported both nifedipine GITS and atenolol prevented the mental stress induced wall motion abnormalities. The biggest limitation of these studies is the small sample size which might have led to type II errors for some of the findings.
Effects of psycho-behavioral intervention on MSIMI have been examined by two studies, conducted by the same laboratory33–34. In studying approximately 250 patients with clinically stable CHD, the investigators demonstrated both exercise and stress management significantly lowered the intensity of LVEF reduction and wall motion abnormalities induced by mental stress testing34. The authors also found that stress management was associated with a significantly lower risk of adverse cardiac outcome compared with the patients in the control group (relative risk = 0.26; p=.04), which was independent of conventional CV risks35. These findings suggest that improving negative emotions may be the key therapeutic approach to improve MSIMI.
SSRI and Platelet Activities
Several studies have indicated that SSRIs reduce elevated platelet activities, which may or may not occur in treatment with other kinds of antidepressants8, 36–38. Alvarez et al. studied the effects of therapy with fluoxetine and clomipramine for 12 weeks. They found both drugs had no difference in effect on the platelet inositol phosphate but the platelet activity was normalized among patients who responded to the antidepressant treatment36. In a study of depressed patients with CHD, reduced platelet activity occurred in patients treated with paroxetine for 6 weeks but not in patients treated with nortriptyline. Other studies showed, compared to placebo, treatment with sertraline37 and paroxetine8 resulted in decrease of platelet activity in patients who were depressed but had no CHD. Platelet activity in patients who participated in the Sertraline against Depression and Heart Disease (SADHART) trial was evaluated and treatment with sertraline was associated with substantially less release of platelet/endothelial biomarkers compared to placebo39.
Conclusion
Compelling evidence supports the need to seek effective intervention for MSIMI. The REMIT study hypothesizes that SSRI treatment improves MSIMI via mood regulation and improvement of platelet activity. This study is unique in that it evaluates the effects of SSRI on MSIMI and simultaneously examines certain mechanisms and/or mediators of MSIMI.
The study began patient recruitment in July 2007 and is scheduled to conclude enrollment in fall of 2011.
Acknowledgement
The study is funded by NHLBI, grant No. RHL085704. Forest Laboratory Inc. provides the study drug and the matched placebo only, and has no role in trial design, data collection and analysis. The authors are solely responsible for the design and conduct of this study including all study analyses, the drafting and editing of the paper and its final contents.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Dimsdale JE. Psychological stress and cardiovascular disease. J Am Coll Cardiol. 2008;51(13):1237–1246. doi: 10.1016/j.jacc.2007.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Strike PC, Steptoe A. Systematic review of mental stress-induced myocardial ischaemia. European Heart Journal. 2003;24(8):690–703. doi: 10.1016/s0195-668x(02)00615-2. [DOI] [PubMed] [Google Scholar]
- 3.Jiang W, Babyak M, Krantz DS, Waugh RA, Coleman RE, Hanson MM, et al. Mental stress-induced myocardial ischemia and cardiac events. Jama-Journal of the American Medical Association. 1996;275(21):1651–1656. doi: 10.1001/jama.275.21.1651. [DOI] [PubMed] [Google Scholar]
- 4.Sheps DS, McMahon RP, Becker L, Carney RM, Freedland KE, Cohen JD, et al. Mental stress-induced ischemia and all-cause mortality in patients with coronary artery disease - Results from the psychophysiological investigations of myocardial ischemia study. Circulation. 2002;105(15):1780–1784. doi: 10.1161/01.cir.0000014491.90666.06. [DOI] [PubMed] [Google Scholar]
- 5.Gottdiener JS, Livengood SV, Meyer PS, Chase GA. Should echocardiography be performed to assess effects of antihypertensive therapy? Test-retest reliability of echocardiography for measurement of left ventricular mass and function. Journal of the American College of Cardiology. 1995;25(2):424–430. doi: 10.1016/0735-1097(94)00375-z. [DOI] [PubMed] [Google Scholar]
- 6.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: A report from the American Society of Echocardiography's guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. Journal of the American Society of Echocardiography. 2005;18(12):1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 7.Slotkin TA, McCook EC, Ritchie JC, Carroll BJ, Seidler FJ. Serotonin transporter expression in rat brain regions and blood platelets: Aging and glucocorticoid effects. Biological Psychiatry. 1997;41(2):172–183. doi: 10.1016/S0006-3223(96)00215-6. [DOI] [PubMed] [Google Scholar]
- 8.Musselman DL, Marzec UM, Manatunga A, Penna S, Reemsnyder A, Knight BT, et al. Platelet reactivity in depressed patients treated with paroxetine - Preliminary findings. Archives of General Psychiatry. 2000;57(9):875–882. doi: 10.1001/archpsyc.57.9.875. [DOI] [PubMed] [Google Scholar]
- 9.Jiang W, Babyak MA, Rozanski A, Sherwood A, O'Connor CM, Waugh RA, et al. Depression and increased myocardial ischemic activity in patients with ischemic heart disease. American Heart Journal. 2003;146(1):55–61. doi: 10.1016/S0002-8703(03)00152-2. [DOI] [PubMed] [Google Scholar]
- 10.Cook WW, Medley DM. Proposed hostility and pharisaic-virtue scales for the MMPI. Journal of Applied Psychology. 1954;38:414–418. [Google Scholar]
- 11.Barefoot JC, Dodge KA, Peterson BL, Dahlstrom WG, Williams RB., Jr The Cook-Medley hostility scale: item content and ability to predict survival. Psychosom Med. 1989;51(1):46–57. doi: 10.1097/00006842-198901000-00005. [DOI] [PubMed] [Google Scholar]
- 12.Hardy JD, Smith TW. Cynical hostility and vulnerability to disease: social support, life stress, and physiological response to conflict. Health Psychol. 1988;7(5):447–459. doi: 10.1037//0278-6133.7.5.447. [DOI] [PubMed] [Google Scholar]
- 13.Revicki DA, Allen H, Bungay K, Williams GH, Weinstein MC. Responsiveness and Calibration of the General Well-Being Adjustment Scale in Patients with Hypertension. Journal of Clinical Epidemiology. 1994;47(12):1333–1342. doi: 10.1016/0895-4356(94)90077-9. [DOI] [PubMed] [Google Scholar]
- 14.Blumenthal JA, Jiang W, Waugh RA, Frid DJ, Morris JJ, Coleman RE, et al. Mental Stress-Induced Ischemia in the Laboratory and Ambulatory Ischemia during Daily-Life - Association and Hemodynamic Features. Circulation. 1995;92(8):2102–2108. doi: 10.1161/01.cir.92.8.2102. [DOI] [PubMed] [Google Scholar]
- 15.Deanfield JE, Shea M, Ribiero P, Delandsheere CM, Wilson RA, Horlock P, et al. Transient St-Segment Depression as a Marker of Myocardial Ischemia during Daily Life. American Journal of Cardiology. 1984;54(10):1195–1200. doi: 10.1016/s0002-9149(84)80066-1. [DOI] [PubMed] [Google Scholar]
- 16.Rozanski A, Bairey CN, Krantz DS, Friedman J, Resser KJ, Morell M, et al. Mental Stress and the Induction of Silent Myocardial Ischemia in Patients with Coronary-Artery Disease. New England Journal of Medicine. 1988;318(16):1005–1012. doi: 10.1056/NEJM198804213181601. [DOI] [PubMed] [Google Scholar]
- 17.Goldberg AD, Becker LC, Bonsall R, Cohen JD, Ketterer MW, Kaufman PG, et al. Ischemic, hemodynamic, and neurohormonal responses to mental and exercise stress - Experience from the psychophysiological investigations of Myocardial Ischemia Study (PIMI) Circulation. 1996;94(10):2402–2409. doi: 10.1161/01.cir.94.10.2402. [DOI] [PubMed] [Google Scholar]
- 18.Krantz DS, Santiago HT, Kop WJ, Merz CNB, Rozanski A, Gottdiener JS. Prognostic value of mental stress testing in coronary artery disease. American Journal of Cardiology. 1999;84(11):1292–1297. doi: 10.1016/s0002-9149(99)00560-3. [DOI] [PubMed] [Google Scholar]
- 19.Specchia G, Falcone C, Traversi E, Larovere MT, Guasti L, Demicheli G, et al. Mental Stress as a Provocative Test in Patients with Various Clinical Syndromes of Coronary Heart-Disease. Circulation. 1991;83(4):108–114. [PubMed] [Google Scholar]
- 20.Yeung AC, Vekshtein VI, Krantz DS, Vita JA, Ryan TJ, Ganz P, et al. The Effect of Atherosclerosis on the Vasomotor Response of Coronary-Arteries to Mental Stress. New England Journal of Medicine. 1991;325(22):1551–1556. doi: 10.1056/NEJM199111283252205. [DOI] [PubMed] [Google Scholar]
- 21.Dakak N, Quyyumi AA, Eisenhofer G, Goldstein DS, Cannon RO. Sympathetically Mediated Effects of Mental Stress on the Cardiac Microcirculation at Patients with Coronary-Artery Disease. American Journal of Cardiology. 1995;76(3):125–130. doi: 10.1016/s0002-9149(99)80043-5. [DOI] [PubMed] [Google Scholar]
- 22.Waldstein SR, Kop WJ, Schmidt LA, Haufler AJ, Krantz DS, Fox NA. Frontal electrocortical and cardiovascular reactivity during happiness and anger. Biological Psychology. 2000;55(1):3–23. doi: 10.1016/s0301-0511(00)00065-x. [DOI] [PubMed] [Google Scholar]
- 23.Soufer R, Arrighi JA, Burg MM. Brain, behavior, mental stress, and the neurocardiac interaction. Journal of Nuclear Cardiology. 2002;9(6):650–662. doi: 10.1067/mnc.2002.129884. [DOI] [PubMed] [Google Scholar]
- 24.Shimbo D, Child J, Davidson K, Geer E, Osende JI, Reddy S, et al. Exaggerated serotonin-mediated platelet reactivity as a possible link in depression and acute coronary syndromes. American Journal of Cardiology. 2002;89(3):331-+. doi: 10.1016/s0002-9149(01)02236-6. [DOI] [PubMed] [Google Scholar]
- 25.Musselman DL, Tomer A, Manatunga AK, Knight BT, Porter MR, Kasey S, et al. Exaggerated platelet reactivity in major depression. American Journal of Psychiatry. 1996;153(10):1313–1317. doi: 10.1176/ajp.153.10.1313. [DOI] [PubMed] [Google Scholar]
- 26.Markovitz JH. Hostility is associated with increased platelet activation in coronary heart disease. Psychosomatic Medicine. 1998;60(5):586–591. doi: 10.1097/00006842-199809000-00013. [DOI] [PubMed] [Google Scholar]
- 27.LaghrissiThode F, Wagner WR, Pollock BG, Johnson PC, Finkel MS. Elevated platelet factor 4 and beta-thromboglobulin plasma levels in depressed patients with ischemic heart disease. Biological Psychiatry. 1997;42(4):290–295. doi: 10.1016/S0006-3223(96)00345-9. [DOI] [PubMed] [Google Scholar]
- 28.Zupancic ML. Acute psychological stress as a precipitant of acute coronary syndromes in patients with undiagnosed ischemic heart disease: a case report and literature review. Prim Care Companion J Clin Psychiatry. 2009;11(1):21–24. doi: 10.4088/pcc.08r00623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jiang W, Krishnan RRK, O'Connor CM. Depression and heart disease - Evidence of a link, and its therapeutic implications. Cns Drugs. 2002;16(2):111–127. doi: 10.2165/00023210-200216020-00004. [DOI] [PubMed] [Google Scholar]
- 30.Gullette ECD, Blumenthal JA, Babyak M, Jiang W, Waugh RA, Frid DJ, et al. Effects of mental stress on myocardial ischemia during daily life. Jama-Journal of the American Medical Association. 1997;277(19):1521–1526. [PubMed] [Google Scholar]
- 31.Bairey CN, Krantz DS, Dequattro V, Berman DS, Rozanski A. Effect of Beta-Blockade on Low Heart Rate-Related Ischemia during Mental Stress. Journal of the American College of Cardiology. 1991;17(6):1388–1395. doi: 10.1016/s0735-1097(10)80152-4. [DOI] [PubMed] [Google Scholar]
- 32.Andrews TC, Parker JD, Jacobs S, Friedman R, Cummings N, MacCallum G, et al. Effects of therapy with nifedipine GITS or atenolol on mental stress-induced ischemic left ventricular dysfunction. Journal of the American College of Cardiology. 1998;32(6):1680–1686. doi: 10.1016/s0735-1097(98)00445-8. [DOI] [PubMed] [Google Scholar]
- 33.Blumenthal JA, Babyak M, Wei J, O'Connor C, Waugh R, Eisenstein E, et al. Usefulness of psychosocial treatment of mental stress-induced myocardial ischemia in men. American Journal of Cardiology. 2002;89(2):164–168. doi: 10.1016/s0002-9149(01)02194-4. [DOI] [PubMed] [Google Scholar]
- 34.Blumenthal JA, Sherwood A, Babyak MA, Watkins LL, Waugh R, Georgiades A, et al. Effects of exercise and stress management training on markers of cardiovascular risk in patients with ischemic heart disease - A randomized controlled trial. Jama-Journal of the American Medical Association. 2005;293(13):1626–1634. doi: 10.1001/jama.293.13.1626. [DOI] [PubMed] [Google Scholar]
- 35.Blumenthal JA, Jiang W, Babyak MA, Krantz DS, Frid DJ, Coleman RE, et al. Stress management and exercise training in cardiac patients with myocardial ischemia - Effects on prognosis and evaluation of mechanisms. Archives of Internal Medicine. 1997;157(19):2213–2223. [PubMed] [Google Scholar]
- 36.Alvarez JC, Gluck N, Fallet A, Gregoire A, Chevalier JF, Advenier C, et al. Plasma serotonin level after 1 day of fluoxetine treatment: a biological predictor for antidepressant response? Psychopharmacology. 1999;143(1):97–101. doi: 10.1007/s002130050924. [DOI] [PubMed] [Google Scholar]
- 37.Markovitz JH, Shuster JL, Chitwood WS, May RS, Tolbert LC. Platelet activation in depression and effects of sertraline treatment: An open-label study. American Journal of Psychiatry. 2000;157(6):1006–1008. doi: 10.1176/appi.ajp.157.6.1006. [DOI] [PubMed] [Google Scholar]
- 38.Pollock BG, Laghrissi-Thode F, Wagner WR. Evaluation of platelet activation in depressed patients with ischemic heart disease after paroxetine or nortriptyline treatment. Journal of Clinical Psychopharmacology. 2000;20(2):137–140. doi: 10.1097/00004714-200004000-00004. [DOI] [PubMed] [Google Scholar]
- 39.Serebruany VL, Glassman AH, Malinin AI, Nemeroff CB, Musselman DL, van Zyl LT, et al. Platelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events - The Sertraline AntiDepressant Heart Attack Randomized Trial (SADHART) platelet substudy. Circulation. 2003;108(8):939–944. doi: 10.1161/01.CIR.0000085163.21752.0A. [DOI] [PubMed] [Google Scholar]