In the past 20 years, more information has become available about clinical outcomes in nursing homes. Since 1991, nursing homes have been mandated to collect and submit the Minimum Data Set (MDS) on Medicare and Medicaid recipients. The uniform data collection allowed the creation of 24 quality indicators (QIs), which reflect the quality of chronic care in individual nursing homes at the state and national levels. Since 1998, MDS records have been transmitted to a national repository to be used to assist in the survey process. MDS data gathering is completed on admission, quarterly, annually, and when a significant change in the resident’s condition occurs. It is also used to determine payment levels in some states for nursing homes certified for Medicare and Medicaid.
In 2002, the Centers for Medicare & Medicaid Services (CMS) released a set of quality measures (QM) on the Internet (http://medicare.gov/NHCompare) so that consumers and advocacy groups would have access to these measures. The revised QM system included post-acute care (PAC) measures and expanded the number of QMs to 31 chronic care and 3 PAC measures (Table 1). Nursing home care providers access their detailed facility QM/QI report on a secure Web site and receive 6 additional reports that provide them an in-depth review of the health status of their residents.
Table 1.
Domain/measure descriptions of the facility quality measure/indicator reporta
| Measure | QI/QM (measure ID) |
|---|---|
| Chronic care measures | |
| Incidence of new fractures | 1.1 |
| Prevalence of falls | 1.2 |
| Residents who have become more depressed or anxious | 2.1 |
| Prevalence of behavior symptoms affecting others | 2.2 |
| High risk | 2.2-HI |
| Low risk | 2.2-LO |
| Prevalence of symptoms of depression without antidepressant therapy | 2.3 |
| Use of 9 or more different medications | 3.1 |
| Incidence of cognitive impairment | 4.1 |
| Low-risk residents who lost control of their bowels or bladder | 5.1 |
| Residents who have/had a catheter inserted and left in their bladder | 5.2b |
| Prevalence of occasional or frequent bladder or bowel incontinence without a toileting plan | 5.3 |
| Prevalence of fecal impaction | 5.4c |
| Residents with a urinary tract infection | 6.1 |
| Residents who lose too much weight | 7.1 |
| Prevalence of tube feeding | 7.2 |
| Prevalence of dehydration | 7.3c |
| Residents who have moderate to severe pain | 8.1b |
| Residents whose need for help with daily activities has increased | 9.1 |
| Residents who spend most of their time in a bed or in a chair | 9.2 |
| Residents whose ability to move in and around their room got worse | 9.3b |
| Incidence of decline in ROM | 9.4 |
| Prevalence of antipsychotic use, in the absence of psychotic or related conditions | 10.1 |
| High risk | 10.1-HI |
| Low risk | 10.1-LO |
| Prevalence of antianxiety/hypnotic use | 10.2 |
| Prevalence of hypnotic use more than 2 times in last week | 10.3 |
| Residents who were physically restrained | 11.1 |
| Prevalence of little or no activity | 11.2 |
| High-risk residents with pressure ulcers | 12.1 |
| Low-risk residents with pressure ulcers | 12.2c |
| Post-acute care measures | |
| Short-stay residents with delirium | 13.1b |
| Short-stay residents who had moderate to severe pain | 13.2 |
| Short-stay residents with pressure ulcers | 13.3b |
The Centers for Medicare & Medicaid Services, which regulates nursing homes through a survey process via contracts with the states’ departments of health, adopted the practice of using the QM/QI performance measures to supplement and guide the inspection process after 2002. Because QM/QIs are problem-based measures, their goal is to score as low as possible; a score of 90% is considered poor, while a score of 20% is considered good. QM/QIs at the 90th percentile in the state ranking or a sentinel event are “flagged” for the nursing home and suggest that there is a concern that should be reviewed. For surveyor reports, they are “flagged” at the 75th percentile and are investigated or emphasized during the annual state survey visit.
After implementation of the MDS system, extensive education was provided to nursing homes and surveyors under the premise that the new data-gathering system needed to be accurate to reflect the resident’s condition. Ongoing education about the MDS process is offered regularly in states because of constant staff turnover.
The purpose of this article is to illustrate how one nursing home staff used its QM/QI reports to successfully improve during a National Institutes of Health (NIH)-funded multilevel intervention research project in a Midwestern state. The 5-year study used a bundled multilevel intervention approach to learn whether (1) the systematic clinical and management practices found in facilities with good resident outcomes could be adopted by nursing homes with resident outcomes needing improvement, (2) the processes of care delivery in poor-performing nursing homes could be improved, and (3) adopting better clinical and management practices would improve resident outcomes.
The multilevel intervention involved all levels of nursing home staff, that is, owners, administrators, and direct care staff. The research team measured select resident outcomes, using QM/QIs from MDS information. Based on prior research outcomes,2 4 QM/QIs that were found to be amenable to nursing interventions and sensitive to quality of care were used to evaluate changes in the processes of care of study homes. The QM/QIs domains were bladder and bowel incontinence (5.1–5.4), weight loss (7.1–7.3), decline in activities of daily living (9.1–9.4), and pressure ulcers (12.1–12.2) (Table 1). There are a total of 13 items measured within the 4 domains (4 in bladder and bowel incontinence, 3 in weight loss, 4 in decline in activities of daily living, and 2 in pressure ulcers). The 4 domains served as resident outcome measures for effectiveness of nursing practices and processes. Although there have been challenges to the validity of the MDS process since its inception, ongoing research has provided evidence supporting its validity and reliability.2–8
COMPLEXITY SCIENCE IN HEALTHCARE SETTINGS
The research study was guided by complexity science.9,10 Complexity theory underpins the direction provided by the 2001 Institute of Medicine report, Crossing the Quality Chasm.11 Researchers have studied complexity theory in hospitals,12,13 primary care practices,14,15, and nursing facilities.10,16 Using the lens of complexity science, nursing homes are viewed as complex adaptive systems consisting of agents, such as nurses and residents, that learn and relate to each other and the environment in nonlinear ways.17 Change in nursing homes, under complexity science, emerges through self-organization, as a result of mutual adjustment of behaviors from the interactions among the staff to meet the needs of residents. Anderson et al have studied the nursing management practices of nursing homes, using complexity science methods.11,16–19 Their research has revealed 3 system parameters that have a strong influence on self-organization: the rate of new information flow through the system, nature of connections among people, and diversity of cognitive schema (mental models people use to make sense of information).17 The 3 system parameters were used by the authors while reviewing field notes of the 29 intervention nursing homes. Research nurses wrote extensive field notes following each site visit or other contact with facility staff as they worked with them over the 2-year intervention.
The NIH-funded study used a 3-pronged approach: (1) a baseline educational program about quality improvement and the basics of care processes, (2) on-site monthly quality-improvement consultations by a gerontological nurse expert, and (3) monthly telephone support of the nursing leader and administrator by the nurse expert. The intervention was based on the assumption that basic QM/QI knowledge was present in the leadership staff of the recruited homes because the MDS data-gathering process was in place since 1991.
Early in the monthly quality improvement consultations, it became obvious to the research nurses that a basic understanding of the MDS process was lacking in the majority of the nursing homes. The Director of Nurses (DON) at the intervention homes claimed to understand the MDS process and use the QM/QI report in quality improvement processes, but when questions arose by the research nurses about the QM/QI scores that were elevated (indicating poor clinical outcomes), the DONs would admit their lack of understanding and use of the QM/QI information and reports.
On the basis of those initial qualitative observations, the research team developed a QM/QI Mentor program to educate leadership and nursing home staff on the MDS process. The Program consisted of 3 50-minute classes. Class 1 covered the basics of data entry into MDS, the MDS reports and their definitions, and the impact of the nursing assistant’s role on QM/QI scores. Class 2 addressed Kitwood’s Psychosocial Needs20 and their use with the MDS Process. Class 3 consisted of applications of the QM/QI and Psychosocial Needs knowledge. A QM/QI quiz was used to assist participants to evaluate their knowledge base throughout the classes, and certificates of completion were awarded to the staff completing all 3 classes.
Graduates of the classes were asked to be mentors about the MDS process with their peers, and QM/QI reports were placed on all nursing units for access by all nursing staff. The QM/QI Mentor Program was offered repeatedly at intervention homes, willing to commit their staff’s time to learn about the process over the years of the consultation visits. An exemplar case study follows revealing dramatic improvement in QM/QI scores following QM/QI teaching, the use of a process improvement team (PIT), and application of the knowledge by nursing home staff.
NURSING HOME EXEMPLAR
The nursing home had more than 100 beds and was privately owned and operated as a for-profit facility but was not part of a chain. Before entering the research, the home had undergone a complete transition of leadership and the interim DON had been on the job less than 6 months, while the home was recruiting a permanent replacement. An initial structured observation of the home revealed a vague and unclear leadership structure that contributed to role confusion and uncertainty experienced by both staff and administrators. A review of the processes of care of the 4 select QM/QI domains of interest (bladder and bowel incontinence, weight loss, decline in activities of daily living, and pressure ulcers) revealed a lack of clear standards of care and processes in use at the home. The QM/QI scores for the majority of the 4 domains were over the 60th percentile, meaning that 60% of the nursing homes in the state had better QM/QI outcomes than the nursing home.
As part of the multilevel intervention, the nursing homes’ leaders were encouraged to select a clinical domain to be the focus of a PIT. The acting DON selected QM/QI 5.3, Prevalence of occasional or frequent bladder and bowel incontinence without a toileting plan, as a clinical area needing improvement. The home’s state percentile score for this QM/QI prior to the research project was over the 90th percentile, which means that the score was “flagged” as a potential problem on their facility report. The interim DON was unfamiliar with QM/QI reports and how to interpret the scores.
Recruitment of a PIT to address the QM/QI 5.3 was accomplished by the fourth visit, with the interim DON choosing to lead the team. All nursing staff levels were represented on the team. The PIT members were not intimidated by the interim DON as leader as observed by the nurse researcher, and they met weekly for 30 minutes. The PIT shared information about its efforts with all nursing home staff via posters about the topic and posting of the PIT minutes. Education of staff about incontinence care standards and assessment methods were identified by PIT as topics that needed addressing first. External and internal resources and teachers were used to meet the knowledge gap, and the DON assigned homework to PIT members to complete and discuss at the weekly meetings. Challenges to involve nursing assistants in decision making about resident care processes were expressed by nurses during the education process.
The PIT also recognized in their initial meetings the need for an admission incontinent assessment process with toileting diaries so that individualized toileting plans could be developed. The PIT members expressed that a goal of their efforts was to improve the quality of life of residents through improved continence and explained to the research nurse how they would know if they were accomplishing that goal. By the fifth consultation visit, the PIT had agreed on an incontinence assessment form to use, and the staff were completing diaries on 2 residents.
An interruption in the progress of the PIT occurred during month 6 when a new DON was recruited, the annual state survey visit occurred, and the new DON voiced doubts about continuing the efforts of PIT during the weekly meeting. Team members were vocal about the value of their efforts and discussed the number of residents whose quality of life could be improved with a toileting plan, and the new DON agreed to continue the work of the PIT. “Survey paralysis” occurred during month 7 as all the energies of nursing management were focused on drafting their responses to the state citations. However, during the month 7 visit, the research nurse reinforced QM/QI teaching for PIT members, who were quick to understand that the flagged QM/QIs and sentinel events on their report need improvement. During month 8, the DON was receptive to QM/QI teaching, as the PIT had not met because of the numerous educational in-services held in response to state citations.
Staff turnover led to recruitment of new PIT members during month 9, and a noticeable decline in toileting practices was noticed by the research nurse during tours of the facility. The PIT was revitalized in month 10 with new members, and QM/QI teaching was offered again: PIT members were shocked at the score of QM/QI 5.3, which rose to the 95th percentile. The PIT selected a different assessment form to use and agreed to complete toileting diaries initially on 3 residents. When the research nurse returned for the month 11 visit, the DON and team were frustrated with their efforts. Against the advice of the research nurse, the DON increased the number of residents to obtain toileting diaries on and then left on vacation. Upon return, the toileting diaries were found to be incomplete, and PIT members shared that the licensed nurses were not supportive of the new toileting efforts and would not participate in the documentation requests. PIT members were convinced by the research nurse to restart the data-gathering process with a small number of residents, and the DON committed to follow-up with licensed nurses about the effort.
In month 13 the PIT was still frustrated with the obstructionist responses of some nursing staff, and the DON shared that nursing employees who were uncooperative in the effort to change the toileting practices were terminated. This was done with the support of the nursing home administrator who wanted the efforts to improve care to succeed. A decline in the QM/QI 5.3 score was observed in the quarterly scores submitted to the research team, with the score decreasing to the 81st percentile during month 13. Contact with the DON during month 14 was met with the comment that the efforts of the PIT were starting to influence positive behavioral changes among the nursing staff about toileting. During months 14 and 15 visits, the PIT analyzed procedural steps, scheduling practices, and their impact on their toileting efforts. They revised steps and practices to improve access to the flow of information for all staff and revised scheduling routines to free up staff to assist with toileting. The nursing assistants on the PIT volunteered to help with writing toileting plans for residents who had an assessment and diary completed.
During the month 16 visit, the DON was feeling positive about the changes made in the toileting processes at the home, the team work evidenced by staff, and the use of the QM/QI report to monitor progress in the home. The QM/QI 5.3 score decreased to the 58th percentile and the DON shared that the home is no longer using crisis management to respond to issues. By month 17, the home had their annual state survey visit and received no citations on toileting. At the weekly PIT meeting, members shared numerous examples of residents who had regained their urinary continence after being put on an individualized toileting plan. Staff who made significant contributions were recognized by nursing leaders and the home celebrated its progress with a party.
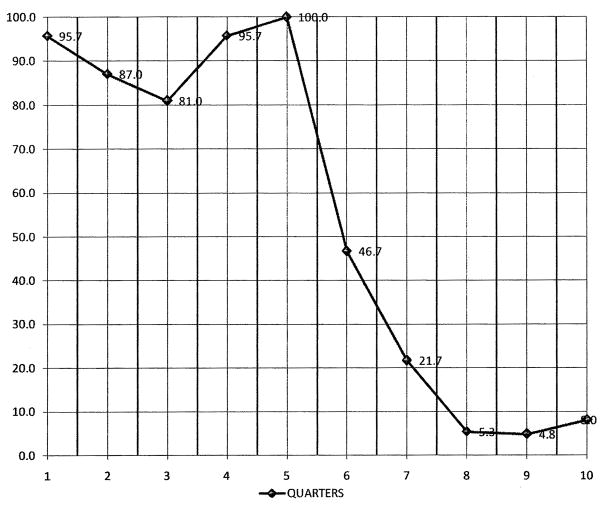
By month 19, the QM/QI 5.3 score decreased to the 26th percentile, a dramatic decline from the home’s preadmission score, which was at the 92nd percentile (Fig 1). Nursing leadership reported using the knowledge gained with the PIT that focused on improving incontinence to address other clinical issues. Leadership was using the successful management practices and the QM/QI reports to set priorities for change and focus for process improvement. At the completion of the 2-year study, the nursing home had implemented PITs to work on clinical issues and was involving other departments in the team.
Figure 1.
QM/QI 5.3 incontinence observed percentile score.
CONCLUSION
The challenge of disseminating knowledge in a systematic way in nursing homes that is sustainable is difficult. The system parameters identified by Anderson et al10 are present in the above case study. Information exchange occurred in the home as the efforts and work of the PIT were shared with staff on a regular basis. Cognitive diversity was promoted by having all levels of nursing staff on the team and replacing them as turnover occurred. All members of the PIT were free to offer their diverse opinions while working to design and redesign the systems of care related to toileting. Making changes in the process did not mean that an error had happened, but that a better way to manage the steps of the process had been discovered. Connections were developed through the weekly meetings of PIT, leading to a capacity for new behaviors. The nurse members of PIT came to appreciate the valuable knowledge that the nursing assistants could offer when planning individualized care, and improved working relationships between the members were observed by the nursing leaders.
As the months progressed, PIT members came to understand that resistance to change was a normal response and that their persistence would win the battle. Education about the QM/QI process and clinical standards provided PIT members with a common language to share with their coworkers when promoting the changes in the toileting practices of the home. PIT had a measurable goal using the QM/QI reports, and management was able to celebrate progress as QM/QI 5.3 (incontinence) declined over the 19 months. The progress made in the above case study validates that nursing management practices, using complexity science as their guide, can lead to self-organization within a nursing home resulting in new behaviors for quality improvement.
Acknowledgments
This research was supported by the National Institute of Nursing Research grant 5R01NR009040-05 (Rantz, PI).
The authors acknowledge the work of the research nurses and other team members: De Minner, Margie Diekemper, Jessica Mueller, David Mehr, Lenis Hicks, Greg Petroski, Richard Madsen, and Jill Scott-Cawiezell.
References
- 1.Centers for Medicare & Medicaid Services. [Accessed August 20, 2009];MDS Quality Measure/Indicator Report. http://www.cms.hhs.gOV/MDSPubQIandResRep/02_qmreport.asp#TopOfPage.
- 2.Rantz MJ, Mehr D, Conn V, et al. Assessing the quality of nursing home care: the foundation for improving resident outcomes. J Nurs Care Qual. 1996;10(4):1–9. doi: 10.1097/00001786-199607000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Hawes C, Phillips CD, Mor V, Fries B, Morris JN. MDS data set should be used for research. Gerontologist. 1992;32(4):563–564. doi: 10.1093/geront/32.4.563b. [DOI] [PubMed] [Google Scholar]
- 4.Hawes C, Morris JN, Phillips CD, Mor V, Fries BE, Nonemaker S. Reliability estimates for the Minimum Data Set for nursing home assessment and care screening (MDS) Gerontologist. 1995;35(2):172–178. doi: 10.1093/geront/35.2.172. [DOI] [PubMed] [Google Scholar]
- 5.Karon S, Sainfort F, Zimmerman DR. Stability of nursing home quality indicators over time. Med Care. 1999;37(6):570–579. doi: 10.1097/00005650-199906000-00006. [DOI] [PubMed] [Google Scholar]
- 6.Phillips CD, Chu CW, Morris JN, Hawes C. Effects of cognitive impairment on the reliability of geriatric assessments in nursing homes. J Am Geriatr Soc. 1993;41:136–142. doi: 10.1111/j.1532-5415.1993.tb02047.x. [DOI] [PubMed] [Google Scholar]
- 7.Rantz MJ, Mehr DR. A quest to understand and measure nursing quality of care. Long-Term Care Interface. 2001;2(7):34–38. [Google Scholar]
- 8.Rantz MJ, Hicks L, Petroski GF, et al. Stability and sensitivity of nursing home quality indicators. J Gerontol A Biol Set Med Sc. 2004;59A(1):79–82. doi: 10.1093/gerona/59.1.m79. [DOI] [PubMed] [Google Scholar]
- 9.Aita V, McIlvain H, Susman J, Crabtree B. Using metaphor as a qualitative analytic approach to understand complexity in primary care research. Qual Health Res. 2003;13(10):1419–1431. doi: 10.1177/1049732303255999. [DOI] [PubMed] [Google Scholar]
- 10.Anderson RA, Issel LM, McDaniel RR. Nursing homes as complex adaptive systems: relationship between management practice and resident outcomes. Nurs Res. 2003;52(1):12–21. doi: 10.1097/00006199-200301000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Committee on Quality of Health Care in America, Institute of Medicine. Crossing the Quality Chasm. Washington, DC: National Academies Press; 2001. [Google Scholar]
- 12.Ashmos D, Duchon D, Hauge F, McDaniel R. Internal complexity and environmental sensitivity in hospitals. Hosp Health Serv Adm. 1996;41(4):535–555. [PubMed] [Google Scholar]
- 13.Ashmos D, Duchon D, McDaniel R. Physicians and decisions: a simple rule for increasing connections in hospitals. Health Care Manag Rev. 2000;25(1):109–115. doi: 10.1097/00004010-200001000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Miller W, Crabtree B, McDaniel R, Stange K. Understanding change in primary care practice using complexity theory. J Fam Pract. 1998;46(5):369–376. [PubMed] [Google Scholar]
- 15.Miller W, McDaniel R, Crabtree B, Stange K. Practice jazz: understanding variation in family practices using complexity science. J Fam Pract. 2001;50(10):872–878. [PubMed] [Google Scholar]
- 16.Anderson RA, McDaniel R. The implication of environmental turbulence for nursing-unit design in effective nursing homes. Nurs Econ. 1992;10(2):117–125. [PubMed] [Google Scholar]
- 17.Anderson RA, McDaniel R. Taking complexity science seriously: New research, new methods. In: Lindberg C, Nash S, Lindberg C, editors. On the Edge: Nursing in the Age of Complexity. Bordentown, NJ: PlexusPress; 2008. pp. 73–95. [Google Scholar]
- 18.Anderson RA, McDaniel R. RN participation in organizational decision making and improvements in resident outcomes. HealthCare Manag Rev. 1999;24(1):7–16. doi: 10.1097/00004010-199901000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Anderson RA, Corazzini KN, McDaniel R. Complexity science and the dynamics of climate and communication: reducing nursing home turnover. Gerontologist. 2004;44(3):378–388. doi: 10.1093/geront/44.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kitwood T. Dementia Reconsidered: The Person Comes First. New York: Open University Press; 1997. [Google Scholar]