Summary
This study aims to critically summarize the literature about bisphenol A (BPA), indicate whether and how those risks are real and emphasize how it is eventually possible to prevent them. With this in mind, we should consider nature, risks and control of BPA, as well as its presence and its role in sealants and composites. It is important to note that we will focus on literature exclusively written about the possible estrogenic activity (and not about the general toxicology profile) of BPA or its possible derivatives released from composites and sealants (without mentioning, or covering just briefly, similar activities performed by their components).
Keywords: bisphenol A, composites, sealants
Introduction
Bisphenol A (BPA) is, by definition, a major component of Bis-GMA (bisphenol A glycidylmethacrylate or “Bowen’s resin”), a molecule known to be at the basis of composites and sealants used in dentistry. In the international dental literature articles regularly appear arguing that BPA and/or its derivatives might be released into the oral cavity from composites and sealants in doses which can produce estrogenic effects. This study aims to critically summarize the literature, indicate whether and how those risks are real and emphasize how it is eventually possible to prevent them. With this in mind, we should consider nature, risks and control of BPA, as well as its presence and its role in sealants and composites. It is important to note that we will focus on literature exclusively written about the possible estrogenic activity (and not about the general toxicology profile) of BPA or its possible derivatives released from composites and sealants (without mentioning, or covering just briefly, similar activities performed by their components).
Bisphenol A
Bisphenol A (BPA) is recorded in the CAS (Chemical Abstract Service), number 00080-05-7 and its chemical name as used in Europe is 2,2-Bis (4-hydroxyphenyl) propane. There are a large number of synonyms, such as the following most common: Bis(4-hydroxyphenyl)dimethyl methane; 4,4′-dihydroxydiphenyl propane; 4,4′-dihydroxy-2,2-diphenyl propane; Diphenylolpropane; 4,4′-isopropylidenediphenol (1).
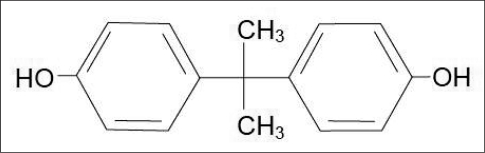
BPA is produced by the condensation of phenol and acetone in the presence of catalysts and catalyst promoters (2); its molecular formula is C15H16O2 and its structure is shown in Figure 1; the molecular mass is 228.29 g / mol and it exists at room temperature in the form of a white solid with a mild “phenolic” odour.
Figure 1.
Low level laser irradiation of tongue.
The main physico-chemical properties of BPA are shown in Table 1.
Table 1.
Ideal bone substitute features.
| PROPERTIES | VALUES |
|---|---|
| Boiling point | 220°C at 4 mmHg – 398°C at 760 mmHg |
| Melting point | 150–157°C |
| Specific gravity | 1.060–1.195 g/mL at 20–25°C |
| Solubility in water | 120–300 mg/L at 20–25°C |
| Vapour pressure | 8.7 x 10−10 – 3.96 x 10−7 mmHg at 20–25°C |
| LogKσw | 2.20 – 3.82 |
| Henry’s constant | 1.0 x 10−10 atm-m3/mol |
BPA is primarily used in the production of polycarbonate (PC), a plastic widely used to produce infant feeding bottles, tableware, microwave ovenware and storage containers.
It is also widely used in the production of epoxy resins, used as an internal, protective lining for cans and metal lids and the inner layer of water tanks and wine vats (1). Small amounts of BPA can migrate from containers into foods and beverages, therefore its use is regulated in the European Union under the Commission Directive 2002/72/EC of 6 August 2002 relating to plastic materials and articles intended to come into contact with foodstuffs.
In the United States and in Japan its use is also authorized in contact with food. The European Commission’s Scientific Committee on Food (SCF) published in 2002 an opinion on BPA, defining a temporary TDI (Tolerable Daily Intake = the amount of a substance, expressed on a body weight basis that can be ingested daily over a lifetime without appreciable risk) of 0.01 mg/kg bw (therefore, equal to 10 g/Kg pc), that derived from No-Observed-Adverse-Effect Level (NOAEL) of 5 mg/kg bw/day, applying a 500-fold uncertainty factor. In 2006, in the light of the vast number of scientific articles published in the meantime, the European Commission asked EFSA (European Food Safety Authority) to review the safety of BPA for use in materials in contact with food.
The Panel of EFSA has issued an opinion in which the re-evaluation of BPA focused particularly on effects of BPA on reproduction and on the endocrine (hormonal) system (1). A great scientific debate has taken place about the aforementioned effects.Therefore, the Panel concluded that the NOAEL of 5 mg/kg bw/day remains valid. The Panel also concluded that endocrine-system related effects of low-doses of BPA in rodents have not been demonstrated in a robust and reproducible way, as some studies indicated major species differences between rodents and humans in the way that BPA is handled in the body: humans more rapidly metabolise and eliminate BPA than rats do and, in addition, mice are particularly sensitive to estrogens. Given, however, that BPA is a weak oestrogen, absence of adverse effects at doses of BPA equal or below 0.5 mg/kg bw/day derived from an important study on mice and two generations of their offspring added further certainty for risk assessment. According to available scientific evidence and because of remaining doubts, the Panel applied a 100-fold uncertainty factor to establish TDI, that is usually used, and established for humans a full TDI of 0.05 mg / kg body weight equal to 50 μg/kg body weight.
Thus, a child of 36 kg weight can take, without risks, a daily dose of BPA of 1800 g and an adult of 70 kg a dose of 3500 g. It has been estimated that the human dietary level of BPA is below 50 mg/kg/day TDI, infants and children included (Table 2).
Table 2.
Ideal bone substitute features.
| Age of consumer | Food/Beverages consumed | Dietary exposure to BPA based on conservative migration value (microgram/kg bw/day) |
|---|---|---|
| 3 month-old infant | Breast milk only | 0.2 |
| 3 month-old infant | Infant formula fed with glass bottle | 2.3 |
| 3 month-old infant | Infant formula fed with PC bottle | 11 |
| 6 month-old infant | Infant formula fed with PC bottle and commercial foods/beverages | 13 |
| 1.5 year-old | 2 kg commercial foods/beverages | 5.3 |
| Adult | 3 kg commercial foods/beverages | 1.5 |
Furthermore, a recent publication of the American CERHR (Centre for the Evaluation of Risks to Human Reproduction, 2007) agrees with the reassuring general conclusions of the experts of the European Community.
Bisphenol A in composites and sealants
Bisphenol A plays an important role in almost all composites and sealants, as it is an integral part of the molecule of Bis-GMA. It must, however, be specified (as was clearly emphasized by ADI, 2008) that in reality BPA can become part of these dental materials in three ways: a) as a direct ingredient, b) as a product of the degradation of other ingredients, c) as trace material derived from the manufacture of other ingredients.
- As a direct ingredient, surprisingly, the BPA is rarely used as a formula ingredient in composites and sealants. In order to explain this apparent paradox, it is necessary to remember, together with Sodherolm and Mariotti, that Bowen described three methods for the synthesis of the monomer BIS-GMA (3,4):
- Reaction between two moles of glycidyl methacrylate with one mole of bisphenol A. A tertiary amine was added to catalyze the addition of the phenolic hydroxyl groups to the epoxide groups. This method (preferred by Bowen) is the simplest one and can lead to the maintenance of both glycidylmethacrylate and BPA as impurities in quantities instrumentally identified.
- Condensation of sodium salt of bisphenol A with an equivalent amount of the reaction product of glycidyl methacrylate and anhydrous hydrochloric acid. During this reaction, sodium chloride is formed as a by-product that could be washed away. Residuals of the bisphenol A salt are left in the final product if excess glycidylmethacrylate is used during the reaction and if the reaction is not allowed to be completed. These residuals may be in large quantities, which may reach several g/g of substance (able to induce estrogenic effects in vitro).
- Reaction of glacial methacrylic acid with the diglycidyl ether of a bisphenol and a tertiary amine was added to catalyze the above reaction. Therefore methacrylate groups were attached to hydroxy glyceryl groups, which, in turn, were linked to phenoxy groups. This synthetic method excludes the use of bisphenol A. Any molecule of bisphenol A possibly present in the final product comes from unreacted impurities from the synthesis of diglycidyl ether of bisphenol A. Good quality control measures in this reaction are sufficient to avoid the presence of these unreacted portions, and today the majority of manufacturers of dental composites prefer this synthetic method as it leaves the fewest parts per million of BPA free or released in the final product.
As a degradation product of other ingredients in the oral cavity conditions, the BPA may come, particularly but not exclusively, from products containing bisphenol A dimethacrylate (Bis-DMA), since the latter is exposed in the oral cavity to the BPA degradation, especially by salivary esterases.
As trace material, BPA can be used in the manufacture of other ingredients (bedsides Bis-GMA) in composites and sealants, therefore its residues may be present in final products in case of poorly controlled reactions.
Obviously it is necessary to note that the composites and sealants produced in Europe, Japan and in the U.S. must meet strict standards determining the maximum amount of BPA released under the conditions of the oral cavity; furthermore these standards are based on toxicological aspects and not on those of estrogens (which require lower doses to act). According to our point of view the problem has therefore to be focused on four questions, to which answers will be given at the end of the review of the literature:
- is BPA released from composites and sealants?
- If yes, how much of it is released?
- Might the released doses have estrogenic action?
- Is there a way to prevent the possible release?
Analysis of literature
Although it was known since the ‘30s that some diphenyl compounds containing two hydroxyl groups in para position could show estrogenicity, only since the mid-90s, the research has dealt with the possible estrogenic effects of BPA. This was generally due to the increased number of studies on this compound, which is, as already noted, widely used in the synthesis of substances forming the inner lining of many food containers and, in particular, to the increasing use of resin-based sealants and composites (both for their intrinsic improvement and for their use in adhesive systems) (3,5).
The first one addressing this issue in dentistry was a Spanish group of the University of Granada along with researchers at Tufts University of Boston: in this widely cited article the authors, studying the behaviour of three composites and a sealant, reported that the release and the estrogenic activity of BPA and BPA dimethacrylate was only due to the sealant(6). In particular, the authors concluded in a clinical trial on 18 subjects that the polymerized sealant (Delton) was able to release high doses into saliva (one hour period after treatment), ranging from 90 to 930 g of BPA and BPA dimethacrylate for 50 mg of compound. These doses were more than sufficient to induce estrogenic responses in a particular cell line. Authors concluded that “the use of bis-GMA-based resins in dentistry, and particularly the use of sealants in children, appears to contribute to human exposure to xenoestrogens”.
By return mail, Habib and Kugel, in a letter to the editor of the magazine which had published the article by Olea et al., criticized it, underlining in particular the need to undertake scientific studies in order to define the presence of risks and their possible gravity as well as the need to avoid “emotional aspects and hysteria”(7).
In the following years, the problem posed by Spanish authors does not seem to have raised, in fact, the said “hysteria” in dentistry, and even the dental scientific analyses are rather reduced in number.
Hamid and Hume in a study in vitro by HPLC did not identify the presence of BPA in the eluate of seven dental sealants (Concise, Ultraseal, P & FS, Prisma Shield Compules, Helioseal F, Dentsply Delton and Delton J & J), but stressed the release of TEGDME from Concise and Helioseal(8).
Carrying out an in vitro analysis using high-performance liquid chromatography (HPLC) for seven sealants (Delton, Concise, Helioseal, PrismaShield, Seal-Rite I, Rite II and Defender Seal), Nathanson et al. found that none of them had released BPA, even if the BPA dimethacrylate was detected in the eluate of two commercial products (Delton and Defender) as well as the presence of various other molecules (TEGDME, Bis-GMA, UDMA) (9).
In 1999 some important contributions worth being taken more carefully into consideration appear almost simultaneously.
Schafer et al., in an experimental work in vitro, confirm the potential estrogenicity of BPA and BPA dimethacrylate in micromolar concentrations in vitro (at doses that are, however, 1,000 times higher than the estrogen reference, represented by 17β-estradiol), both repeating the experiences of Olea et al. and with the use of flow cytometry. They very clearly stress that their conclusions are valid only “in vitro” and that “in vivo” is necessary to investigate various controversial aspects and, in particular:
- how much the xenoestrogens are accumulated and metabolized;
- what is the level of exposure of people to these compounds;
- what exactly are the levels sufficient to cause adverse reactions;
- how much the xenoestrogens have additive effects (10).
Soderholm and Mariotti (3), in a comprehensive and precise review of the literature (already mentioned in this introduction), not only present the synthesis of experimental work that had appeared up until then on the release and possible estrogenic action of BPA from dental products, but also explore for explanatory purposes three main areas: chemistry and clinical use of Bis-GMA, steroids’ action in the body and in the oral cavity, the various theories about how bisphenol A–based resins may affect estrogen-sensitive tissues in the body. These authors concluded that “based on existing research, we must accept that certain impurities may be present in some Bis-GMA–based resins, and these impurities, when released from restorations, are potentially estrogenic” but added that “the amounts of bisphenol A that may be present as an impurity or produced as a degradation product from dental restorations, including sealants, are quite small and far below the doses needed to affect the reproductive tract.
Lewis et al., in a study in vitro carried out to identify the release of BPA and BPA dimethacrylate from 28 commercial dental products (20 composites and 8 sealants, see Table 1) using HPLC, found no measurable released quantities of these compounds; the only exception was represented by a sealant (Delton II) able to release amounts of bisphenol capable of producing estrogenic responses in vitro. The authors concluded, however, that “dental resins in general do not represent a significant source of BPA or BAD exposure” (11).
Schmalz et al., in a trial in vitro conducted by HPLC on the release of BPA from sealant monomers under different hydrolytic conditions (variable pH values, esterase action, pooled saliva for up to 24 hours) stress the importance of the conversion under these conditions of BPA into BPA dimethacrylate as well as how the majority of commercial products did not contain any compounds (12). Authors concluded that the results reported by Olea et al. (6) may be attributed to the BPA-dimethacrylate content of Delton, but, on the other hand, no BPA release is expected under physiological conditions from fissure sealants based on Bis-GMA if pure-base monomers are used.
The same research group, Arenholt-Bindslev et al., then conducted an in vivo analysis, placing two different types of fissure sealants (Delton and Visioseal) in 8 volunteers. 5 ml of saliva were collected immediately, 1 hour and 24 hours after placement of the fissure sealant. The saliva samples analysis by HPLC found that small quantities of BPA (0.3–2.8 ppm i.e. 0.3 to 2.8 mg/L, as the sample collected of 5 ml, the total quantity was 1.5–14 g) were detected in saliva samples collected only immediately after placement of Delton sealant; furthermore, in a recombinant yeast cell assay, significantly increased estrogenic activity was found in saliva samples collected immediately after placement of Delton. The authors concluded that “BPA can be found in saliva samples collected immediately after placement of Delton”, however, it is “considerably lower than the amount reported by other sealants. No detectable amounts of BPA nor estrogenic activity were detected 1 hour after Delton treatment (13).
In 2000, the Olea group revived interest in research in this field, showing that, despite the reassuring findings of previous literature, BPA was released not only from the “usual” Delton, but also from 7 others commercial composites currently used in dentistry (Pekalux, Charisma, SILUX plus, Z100, Tetric, Brilliant, Polofil). Using HPLC and gas chromatography/mass spectrometry, the authors studied biphenolic molecules eluted from in vitro polymerized commercial composites, with particular reference to BPA, and found values of up to 1.8 g/g of polymerized materials. Such concentrations, underlined the authors, may have “biological effects, as have been demonstrated in in vivo experimental models (14).
Tarumi et al., by means of the Reporter Gene Assay, investigated the endocrine response to three sealants (Delton, Defender and Teethmate) and 4 adhesive resins (Linerbond, Scotchbond, Optibond Solo and AllBond). Two of these sealants (Delton and Defender) were confirmed to have estrogenic activity, although none of the tested materials contained BPA. They concluded that “endocrine-like action is probably linked to BPA dimethacrylate” and that “the possibilities of the BPA eluted from dental resin-based materials mimicking natural steroid hormones are negligible” (15).
Fung et al. have carried out an in vivo test on 40 adult volunteers collecting saliva and blood samples at various intervals (1h, 3h, 1 day, 3 days and 5 days) after sealant (Delton) placement and using HPLC to determine BPA concentration; 18 patients constituted the low-dose group, receiving a single 8-mg dental sealant dose on one surface, while 22 patients constituted the high-dose group, receiving a total dosage of 32 mg of sealant on four surfaces. This experience frankly seemed rather questionable in some respects, from a dental point of view, because the authors did not used a dental dam (as most of the other authors cited did), did not immediately make a collection of fluid, touched up the areas of sealant with rotary instruments, and collected fluids in plastic containers (which can react with BPA). However, the authors, despite detected low concentrations of BPA in saliva specimens collected at both one and three hours immediately after sealant placement in saliva (from 5.8 to 105.6 parts per billion, i.e. g/L), and relying on the continued absence of measurements in blood and saliva samples after 24 hours, state that “that BPA released orally from a dental sealant may not be absorbed or may be present in non-detectable amounts in systemic circulation, therefore, “the concern about potential estrogenicity of a sealant may be unfounded” (16).
Manabe et al., using in vitro an original method of selective extraction in combination with gas chromatography-mass spectrometry, revealed that the composites and sealants examined released up to 91.4 ng of bisphenol-A/g material into a buffered saline solution, when polymerized, during a 24-hour incubation. The authors concluded that bisphenol-A can be released from dental materials, however the leachable amount would be less than 1/1000 of the reported dose (2 g/kg body weight/day) required for xenoestrogenisity in vivo (17).
Al-Hiyasat et al., in an in vivo study, investigated the effect of leached substances from dental composites on the fertility of male mice. Using Z 100, the authors prepared 50 polymerized discs (for a weight of 3.9 g), immersed them in ethanol for 24 hours and sonicated them for 30 minutes. The eluate evaporated the at 80°C. The obtained sediment was dissolved in distilled water and intragastrically administered to 20 male mice. The procedure was repeated for 28 days (while keeping the same 50 discs). The study of these various fertility tests enabled the authors to conclude that the components released from the composite under the above-mentioned conditions “have an adverse effect on the fertility and reproductive system of male mice” (18).
Atkinson et al. conducted an in vitro investigation into the stability of compounds usually found in dental sealants, using gas chromatography/mass spectrophotometry and HPLC. Subsequently, standard BPA molecules BPA dimethacrylate and TEGDMA (triethylene-glycol dimethacrylate) were added to saliva. The authors found that free BPA in saliva is stable while the BPA dimethacrylate is rapidly converted to BPA which can slow this process. This process is significantly influenced by decreasing salivary pH and temperature (19).
In an interesting article, Kostoryz et al. studied in vitro the cytotoxic, mutagenic and estrogenic effects of hydroxylated metabolites of BisGMA and BFDGE (bisphenol F diglycidyl ether, a molecule found in many oxirane composites), respectively represented by Bisphenol A bis (2,3-dihydroxypropyl) ether and bisphenol F bis (2,3-dihydroxypropyl) ether. The study showed that they neither have estrogenic effects nor are mutagenic, and presented a lower cytotoxicity. They were non-mutagenic, non-estrogenic, and presented minor cytotoxicity (20).
Using a reporter gene assay, Nomura et al. tested in vitro for estrogenic activity three monomers (Bis-GMA, UDMA and TEGDME) and five polymerization initiators (camphorquinone (CQ), benzoyl peroxide (BPO), dimethyl-para-toluidine (DMPT), 2-dimethylamino-ethyl-methacrylate (DMAEMA), and 1-allyl-2-thiourea (ATU)). Two of the products (BPO and DMPT) even showed reduced estrogenic activity in vitro (21).
Al-Hiyasat et al., in a similar article to the one already mentioned (Al-Hiyasat et al., 2002) (18), suggested that leached components from a resin-based dental composite (Z-100) “have adverse effects on the fertility and reproductive system of female mice”(22). The same Jordanian group made up by Darmani et al., no longer studying the composite eluate but directly the BPA dimethacrylate administered intragastrically in doses ranging from 5 to 100 μg /μg body weight, showed significant adverse effects on the fertility and reproductive systems of male and female mice (23).
Takahashi et al. demonstrated that the release of BPA from polycarbonate crowns also demonstrated that the hTERT (human telomerase catalytic subunit mRNA) is a possible target test to evaluate the estrogenicity of the PBA (24). Also of great interest is the article by Wada et al., published in the well known Journal of Dental Research in which the Japanese authors tested the hypothesis that commercial composites, which contain various monomers and additives, may exhibit estrogenic activity in vitro. The estrogenic activity of eluates obtained from 24 resin composites placed into a steel mould (5 mm diameter and 1.5 mm high), and 18 chemicals with concentration equal to 100 nmol/L identified from the composites tested, were examined with the use of the reporter gene assay (25).
They revealed estrogenic activity in vitro for six of the 24 composites (Table 4, active composites are shown with X), and three of the 18 constituents: a photostabilizer (HMBP), a photoinitiator (DMPA) and an inhibitor (BHT) (Table 5). The authors wisely concluded that “the clinical relevance of the results of the present in vitro study remains unclear“ and that “further investigation into the in vivo estrogenic effects of composites is necessary, although the release of estrogenic compounds from composites is basically undesirable”.
Table 4.
Ideal bone substitute features.
| Composites | Manufacturer | Estrogenic activity in vitro |
|---|---|---|
| Charisma | Heraeus Kulzer | X |
| Flowline* | Heraeus Kulzer | X |
| Esthet X | Dentsply/Caulk | X |
| Surefil | Dentsply/Caulk | X |
| Spectrum | Dentsply/DeTrey | X |
| Herculite | Kerr | |
| Prodigy | Kerr | |
| Revolution* | Kerr | X |
| Clearfil APX | Kuraray | |
| Clearfil ST | Kuraray | |
| Palfique Estelite | Tokuyama | |
| Palfique Toughwell | Tokuyama | |
| Palfique Estelite LV* | Tokuyama | |
| Litefil IIA | SHOFU | |
| Beautifil | SHOFU | |
| Unifil F | GC | |
| Z250 | 3M | |
| Filtek Flow* | 3M | |
| Glacier | SDI | |
| Wave* | SDI | |
| Heliomolar | Vivadent | |
| Tetric Ceram | Vivadent | |
| Tetric Flow* | Vivadent | |
| Progress | Kanebo |
Flowable composites.
Table 5.
Ideal bone substitute features.
| Formula | Abbreviations | Estrogenicity |
|---|---|---|
| Monomers | ||
| 2,2-bis[4-(3-methacryloxy-2-hydroxypropoxy)-phenyl]-propane | Bis-GMA | |
| Urethane dimethacrylate | UDMA | |
| Triethyleneglycol dimethacrylate | TEGDMA | |
| Diethyleneglycol dimethacrylate | DEGDMA | |
| Ethyleneglycol dimethacrylate | EGDMA | |
| Initiators | ||
| Camphorquinone | CQ | |
| 2,2-dimethoxy-2-phenylacetophenone | DMPA | X |
| Photostabilizers | ||
| 2-hydroxy-4-methoxybenzophenone | HMBP | X |
| 2-(2-benzotriazolyl)-p-cresol | TIN-P | |
| 2-(2′-hydroxy-5′-tert-octylphenyl) benzotriazole | TIN 320 | |
| Inhibitors | ||
| 2,6-di-tert-butyl-p-cresol | BHT | X |
| 4-methoxyphenol | HQME | |
| Co-initiators | ||
| 4-dimethylaminobenzoic acid ethyl ester | DMABEE | |
| 4-dimethylaminobenzoic acid 2-n-butoxyethyl ester | DMABBEE | |
| 4-dimethylaminobenzoic acid 2-ethylhexyl ester | DMABEHE | |
| 2-(dimethylamino) ethyl methacrylate | DMAEMA | |
| N,N-dimethyl-p-toluidine | DMPT | |
| N-(2-cyanoethyl)-N-methylaniline | CEMA | |
Sasaki et al., in an in vivo study using the ELISA system, investigated the changes in the BPA concentration in the saliva of 21 volunteers after restoration with composite resins (of constant weight of 0.1 grams). Nine commercially available products were used in this study: (Z100, Progress, Palfique, Metafile Flo, UNIFIL S, Beautifil, Xeno CFII, Prodigy, Clearfil ST). Thanks to this method, the authors found BPA concentrations ranging from 15 to 100 ng/ml of saliva (in other words in 1 ml of saliva, a released amount equal to 0.15–1 g/g of substance was present). It is interesting to find that sufficient gargling, if carried out immediately after polymerization, can quickly remove BPA completely from the oral cavity (26).
Joskow et al. conducted a study in vivo on the release of BPA from two sealants (Delton and Helioseal): after sealant placement in 14 volunteers they measured BPA in saliva and urine samples collected at prescribed intervals immediately after, after an hour and after 24 hours. The sealants were tested using a gas chromatograph-high resolution mass spectrometer. The authors detected differences between the salivary BPA concentrations of Delton (large amounts, also present one hour later in the urine) and Helioseal-treated patients one hour after sealant placement. This conclusion of this article is particularly interesting as the authors (hosted by the ADA official journal) stated that “Dental sealants may be a point source for low-level BPA exposure at levels that show health effects in rodents. Further research is required to determine whether human exposure to BPA at these levels causes adverse effects” (27). Eliades et al. did not discover release of BPA by HPLC from two types of composite (Rely-a-bond and Reliance) intended for the fitting of an orthodontic bracket. (28,29)
In a selective review of the literature, Azarpazhooh and Main, working on the assumption that the “release of dental sealant components such as BPA has the potential to bind the estrogen receptors of relevant cells at sub-toxic concentrations”, instead investigated whether the placement of pit- and fissure-sealant materials causes toxicity, and thus harms patients (30).
Having identified 377 articles in the literature related to this topic, the authors chose 11 of them, under strict exclusion criteria, to be investigated (though 15 studies have been assessed). From the comparison of these studies, the authors concluded that “that patients are not at risk for exposure to BPA from the use of dental sealants”, however, “to reduce the potential for BPA toxicity from sealants, dental providers should use simple clinical procedures.
Gioka et al. examined the structure, composition and estrogenic effects in vitro of particles obtained from the drilling of two types of orthodontic composite (System 1 + and Blugloo). In particular, they investigated the estrogenicity of the eluate obtained after one months’ immersion, carried out by grinding in saline solution in contact with an estrogen-responsive cell line (MCF-7). Both the adhesives showed estrogenic effects in vitro, and proliferation rates of MCF-7 cells increased by 160% and 128%, compared to the control. The authors concluded that, apart from the potentially hazardous action of adhesive aerosol particulate produced by grinding, composite resin particulates may act as “endocrinological disruptors” (31).
The last bibliographic consideration is the limited number of articles that dealt with the preventive activities that can be performed in dentistry in order to avoid the absorption by the patient of the monomers and, in particular, the release of BPA from sealants and composites.
Rueggeberg et al. conducted research to examine the effectiveness of 5 treatments (carried out for 20 seconds) in eliminating the residual monomer amount of the surface of freshly polymerized sealants. They found that the use of pumice in cup eliminates on average 95%, while pumice on cotton ball 93%, dry cotton 89%, wet cotton 86%, and an air/water spray removed 68%. The authors concluded that it appears that the most effective method of removing the air-inhibited layer from sealants after their placement is to apply a mild abrasive (pumice) in combination with some sort of mechanical energy (a hand scrub with a cotton roll or an air-driven prophylaxis cup) (32). Schafer et al. emphasize the possibility of treating the surface of freshly polymerized sealants with mild abrasive and by means of a prophylaxis cup to remove residual free monomer (33).
Sasaki et al., as we mentioned before, noticed in their experiments that 30 seconds’ gargling with warm water was sufficient to almost completely remove the BPA released from tested composites (26).
At the end of their review of the literature, Azarpazhooh and Main recommended that dental providers avoid the potential for BPA toxicity from the dental sealants by treating their polymerized surface layer using one of the following procedures:
using a mild abrasive, such as pumice, either on a cotton applicator or with a prophylaxis cup
having older children and adolescents gargle with tepid water for 30 seconds
washing the surface of the sealant for 30 seconds with an air-water syringe while using suction to remove fluids and debris from a child’s mouth (30).
Conclusion
Regarding the four initial questions, the conclusions that we can draw from analysis of the literature are the following:
- BPA can be effectively released from composites and sealants.
- In the literature, released doses vary greatly between composites (very low releases of between 0 and 1–2 g) and sealants. In the first investigation on this subject, the amount released reached a maximum of 930 g per dose of 50 mg sealant. This amount was never reached in subsequent researches which never revealed releases or, if there were any, the doses were from 10 to 100 times lower (1–10 g).
- The maximum doses that may be released may actually have estrogenic action in vitro (i.e., on “sensitized” cells), but it is necessary to note that, compared to a maximum release of 930 micrograms of BPA from the “worst” sealant, under the European regulations a child of 36 kg can tolerate a daily dose of over 1800 g BPA without any risks, while a teenager of 50 kg can tolerate a dose of 2500 g. It should be emphasized that any acute dose of sealant is usually single or distributed, up to a maximum of four times.
- It is impossible to prevent release, but it is possible to prevent the absorption of BPA by the patient. In this regard, we would suggest not only employing one or more of the mechanical methods proposed by different authors, but especially (and perhaps these authors implied this) the use of a dental dam.
Finally, here below is a statement from the ADA (2008):
“There is also evidence that some dental sealants, and to a lesser extent dental composites, may contribute to very low-level BPA exposure. The ADA fully supports continued research into the safety of BPA but, based on current evidence, the ADA does not believe there is a basis for health concerns relative to BPA exposure from any dental material”.
Table 3.
Commercial dental products (from ref. 11).
| 1. Bisfil P Bisco, A |
| 2. Brilliant Dentin Coltene/Whaledent A |
| 3. Charisma Kulzer, A |
| 4. Clearfil PhotoPosterior Kuraray A |
| 5. Heliomolar Vivadent A |
| 6. Herculite XRV Kerr/Sybron A |
| 7. Lite-Fil II Shofu Dental A |
| 8. Occlusin GC-America A |
| 9. P-50 3 M Dental Products A |
| 10. Palfique Estilite Paste Tokuyama A |
| 11. Pekafil NF Bayer Dental, Germany A |
| 12. Pekalux Bayer Dental, Germany A |
| 13. Pertac-Hybrid ESPE A |
| 14. PhotoClearfil Kuraray A |
| 15. Prisma APH Caulk/Dentsply A |
| 16. Prisma TPH Caulk/Dentsply A |
| 17. Prodigy Kerr A |
| 18. Silux Plus 3 M Dental Prod. A |
| 19. Tetric Vivadent, A |
| 20. Z100 3 M Dental Products A |
| 21. Delton Base Dentsply/Ash, B |
| 22. Delton Catalyst Dentsply/Ash, B |
| 23. Delton LC Ash/Dentsply, B |
| 24. FluoroShield Caulk/Dentsply B |
| 25. PermaSeal Ultradent Products B |
| 26. Prisma•Shield Caulk/Dentsply B |
| 27. Concise Opaque 3 M Dental Prod. B |
| 28. UltraSeal XT Ultradent Products B |
References
- 1.EFSA (European Food Safety Authority) Bisphenol A for use in food contact materials EFSA Journal. 2006;428:10–75. [Google Scholar]
- 2.Staples CA, Dorn PB, Klecka GM, O’Block ST, Harris LR. A review of the environmental fate, effects and exposures of bisfenol A Chemosphere. 1998;36(10):2149–2173. doi: 10.1016/s0045-6535(97)10133-3. [DOI] [PubMed] [Google Scholar]
- 3.Soderholm KJ, Mariotti A. BisGMA based resins in dentistry: Are they safe? J Am Dent Assoc. 1999;130:201–209. doi: 10.14219/jada.archive.1999.0169. [DOI] [PubMed] [Google Scholar]
- 4.Bowen RL. Method of preparing a monomer having phenoxy and methacrylate groups linked by hydroxy glycerol groups. Apr, inventor. U.S. patent 1965 3179623.
- 5.Dodds EC, Lawson W. Synthetic estrogenic agents without the phenanthrene nucleus. Nature. 1936;137:996. [Google Scholar]
- 6.Olea N, Pulgar R, Perez P, Olea-Serrano F, Rivas A, Novillo-Fertrell A, Padranza V, Soto AM, Sonnenschein C. Estrogenicity of resin-based composites and sealants used in dentistry. Environ Health Perspect. 1996;104:298–305. doi: 10.1289/ehp.96104298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Habib CM, Kugel G. Estrogenicity of Resin-based Composites and Sealants in Dentistry. Environ Health Perspect. 1996;104:808. doi: 10.1289/ehp.104-1469430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hamid A, Hume WR. A study of component release from resin pit and fissure sealants in vitro. Dent Mater. 1997;13(2):98–102. doi: 10.1016/s0109-5641(97)80018-8. [DOI] [PubMed] [Google Scholar]
- 9.Nathanson D, Lertpitayakun P, Lamkin MS, Edalatpour M, Chou LL. In vitro elution of leachable components from dental sealants. J Am Dent Assoc. 1997;128:1517–1523. doi: 10.14219/jada.archive.1997.0091. [DOI] [PubMed] [Google Scholar]
- 10.Schafer TE, Lapp CA, Hanes CM, Lewis JB, Wataha JC, Schuster GS. Estrogenicity of bisphenol A and bisphenol A dimethacrylate in vitro. J Biomed Mater Res. 1999;45:192–197. doi: 10.1002/(sici)1097-4636(19990605)45:3<192::aid-jbm5>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 11.Lewis JB, Rueggeberg FA, Lapp CA, Ergle JW, Schuster GS. Identification and characterization of estrogen-like components in commercial resin-based dental restorative materials. Clin Oral Invest. 1999;3:107–113. doi: 10.1007/s007840050087. [DOI] [PubMed] [Google Scholar]
- 12.Schmalz G, Preiss A, Arenholt-Bindslev D. Bisphenol-A content of resin monomers and related degradation products. Clin Oral Invest. 1999;3:114–9. doi: 10.1007/s007840050088. [DOI] [PubMed] [Google Scholar]
- 13.Arenholt-Bindslev D, Breinholt V, Preiss A, Schmalz G. Time-related bisphenol-A content and estrogenic activity in saliva samples collected in relation to placement of fissure sealants. Clin Oral Invest. 1999;3:120–125. doi: 10.1007/s007840050089. [DOI] [PubMed] [Google Scholar]
- 14.Pulgar R, Olea-Serrano MF, Novillo-Fertrell A, Rivas A, Pazos P, Pedraza V, Navajas JM, Olea N. Determination of Bisphenol A and Related Aromatic Compounds Released from Bis-GMA-Based Composites and Sealants by High Performance Liquid Chromatography. Environ Health Perspect. 2000;108:21–27. doi: 10.1289/ehp.0010821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tarumi H, Imazato S, Narimatsu M, Matsuo M, Ebisu S. Estrogenicity of fissure sealants and adhesive resins determined by reporter gene assay. J Dent Res. 2000;79:1838–1843. doi: 10.1177/00220345000790110401. [DOI] [PubMed] [Google Scholar]
- 16.Fung EY, Ewoldsen NO, St Germain HA, Marx DB, Miaw CL, Siew C, Chou HN, Gruninger SE, Meyer DM. Pharmacokinetics of bisphenol A released from a dental sealant. J Am Dent Assoc. 2000;131(1):51–8. doi: 10.14219/jada.archive.2000.0019. [DOI] [PubMed] [Google Scholar]
- 17.Manabe A, Kaneko S, Numazawa S, Itoh K, Inoue M, Hisamitsu H, Sasa R, Yoshida T. Detection of bisphenol-A in dental materials by gas chromatography-mass spectrometry. Dent Mater J. 2000;19(1):75–86. doi: 10.4012/dmj.19.75. [DOI] [PubMed] [Google Scholar]
- 18.Al-Hiyasat AS, Darmani H, Elbetieha AM. Effects of resin based dental composites on fertility of male mice. Eur J Oral Sci. 2002;110(1):44–7. doi: 10.1034/j.1600-0722.2002.00163.x. [DOI] [PubMed] [Google Scholar]
- 19.Atkinson JC, Diamond F, Eichmiller F, Selwitz R, Jones G. Stability of bisphenolA, triethylene-glycol dimethacrylate, and bisphenol A dimethacrylate in whole saliva. Dent Mater. 2002;18(2):128–35. doi: 10.1016/s0109-5641(01)00031-8. [DOI] [PubMed] [Google Scholar]
- 20.Kostoryz EL, Eick JD, Glaros AG, Judy BM, Welshons WV, Burmaster S, Yourtee DM. Biocompatibility of Hydroxylated Metabolites of BISGMA and BFDGE. J Dent Res. 2003;82(5):367–371. doi: 10.1177/154405910308200508. [DOI] [PubMed] [Google Scholar]
- 21.Nomura Y, Ishibashi H, Miyahara M, Shinohara R, Shiraishi F, Arizono K. Effects of dental resin metabolites on estrogenic activity in vitro. J Mater Sci Mater Med. 2003;14(4):307–10. doi: 10.1023/a:1022923713892. [DOI] [PubMed] [Google Scholar]
- 22.Al-Hiyasat AS, Darmani H, Elbetieha AM. Leached components from dental composites and their effects on fertility of female mice. Eur J Oral Sci. 2004;112(3):267–72. doi: 10.1111/j.1600-0722.2004.00136.x. [DOI] [PubMed] [Google Scholar]
- 23.Darmani H, Al-Hiyasat AS. Reproductive toxic effect of bisphenol A dimethacrylate in Mice. J Biomed Mater Res. 2004;69A:637–643. doi: 10.1002/jbm.a.30029. [DOI] [PubMed] [Google Scholar]
- 24.Takahashi A, Higashino F, Aoyagi M, Kyo S, Nakata T, Noda M, Shindoh M, Kohgo T, Sano H. Bisphenol A from Dental Polycarbonate Crown Upregulates the Expression of hTERT. J Biomed Mater Res. 2004;71B:214–221. doi: 10.1002/jbm.b.30085. [DOI] [PubMed] [Google Scholar]
- 25.Wada H, Tarumi H, Imazato S, Narimatsu M, Ebisu S. In vitro Estrogenicity of Resin Composites. J Dent Res. 2004;83:222–226. doi: 10.1177/154405910408300307. [DOI] [PubMed] [Google Scholar]
- 26.Sasaki N, Okuda K, Kato T, Kakishima H, Okuma H, Abe K. Salivary bisphenol-A levels detected by ELISA after restoration with composite resin. J Mater Sci Mater Med. 2005;16(4):297–300. doi: 10.1007/s10856-005-0627-8. [DOI] [PubMed] [Google Scholar]
- 27.Joskow R, Barr DB, Barr JR, Calafat AM, Needham LL, Rubin C. Exposure to bisphenol A from bis-glycidyl dimethacrylate-based dental sealants. J Am Dent Assoc. 2006;137(3):353–62. doi: 10.14219/jada.archive.2006.0185. [DOI] [PubMed] [Google Scholar]
- 28.Eliades T, Hiskia A, Eliades G, Athanasiou AE. Assessment of bisphenol-A release from orthodontic adhesives. Am J Orthod Dentofacial Orthop. 2007a;131:72–5. doi: 10.1016/j.ajodo.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 29.Eliades T, Gioni V, Kletsas D, Athanasiou AE, Eliades G. Oestrogenicity of orthodontic adhesive resins. Eur J Orthod. 2007b;29:404–7. doi: 10.1093/ejo/cjm040. [DOI] [PubMed] [Google Scholar]
- 30.Azarpazhooh A, Main PA. Is There a Risk of Harm or Toxicity in the Placement of Pit and Fissure Sealant Materials? A Systematic Review. J Can Dent Assoc. 2008;74(2):179–183. [PubMed] [Google Scholar]
- 31.Gioka C, Eliades T, Zinelis S, Pratsinis H, Athanasiou AE, Eliades G, Kletsas D. Characterization and in vitro estrogenicity of orthodontic adhesive particulates produced by simulated debonding. Dent Mater. 2009;25:376–382. doi: 10.1016/j.dental.2008.08.010. [DOI] [PubMed] [Google Scholar]
- 32.Rueggeberg FA, Dlugokinski M, Ergle JW. Minimizing patients’ exposure to uncured components in a dental sealant. J Am Dent Assoc. 1999;130(12):1751–7. doi: 10.14219/jada.archive.1999.0132. [DOI] [PubMed] [Google Scholar]
- 33.Schafer TE, Lapp CA, Hanes CM, Lewis JB. What parents should know about estrogen-like compounds in dental materials. Pediatr Dent. 2000;22(1):75–6. [PubMed] [Google Scholar]