Summary
Aim
This pilot study evaluated patients’ experience of oral surgical and prosthetic procedures as well as their opinions regarding function, aesthetics, comfort, and satisfaction with treatment outcomes.
Materials and methods
Forty-nine subjects treated with oral implants completed questionnaires comprising 44 questions. Three questionnaires were used related to implant-supported single-tooth, fixed implant-supported prostheses and implant-retained overdentures. The questions related to demographic data (age, sex, employment, marital status and educational level), the source of information, the reason they underwent implant treatment, the discomfort related to all phases of treatment, and their functional and aesthetic satisfaction.
Results
Most of the patients (53.8%) were employed and had received a high school certificate or a university diploma. Patients heard about implants from various sources, including referring dentists (55.8%), relatives and friends (23.1%), and television, radio and the Internet (17.3%). The main reasons for choosing implant treatment were restoring lost teeth (35,5%), following dentist’s advice (33,3%), improving stability of the removable denture (15.4%), eating habits (13.5%) and aesthetics (1.9%). Most patients considered that the procedure took a long time (44.2%) but was not traumatic (62.5%). Pain was almost absent in most cases (64.5%) and swelling, when present, was generally moderate (48.1%) and seldom was marked (17.3%). Patients were very satisfied about the aesthetics (82.7%) and function (94.2%), and considered the implant prosthesis to be part of themselves (84.6%). Most of the patients considered the implant prostheses to be easy to clean (73.1%), and would repeat the treatment if necessary (86.5%) and recommend it to other people (94.2%).
Conclusions
Although the present study is limited by the small sample, the outcomes suggest that oral implant rehabilitation meets patients’ needs and aesthetic demands.
Keywords: patient opinion, oral implants, patient satisfaction, function, aesthetics
Introduction
Prosthetic rehabilitation of people with missing teeth is one of the most complex topics in dentistry due to its gnathological, psychosocial, aesthetic and functional implications. The loss of teeth can represent a severe handicap that directly impacts on the quality of life. Teeth serve both as part of the masticatory system and also greatly contribute to phonetics, functions and aesthetics (1).
In the past, the psychological reactions of people to tooth loss generated little concern, with most of them adapting to replacement prostheses such as crowns, bridges and dentures (2). Nowadays attitudes are different; for psychological and functional reasons, many patients prefer an implant restorative procedure. Implants improve retention and stability of the complete dentures, thereby providing functional, psychological and social advantages, and partial fixed reconstructions avoid the need to prepare intact adjacent teeth (3,4). Additional positive factors are preventing continuous alveolar bone resorption, preserving ridge heigh and width, and improving aesthetics, especially in anterior regions (5,6).
Most of the recent studies have focused on the clinical aspects of osseointegration (7,9,11) without considering patients’ attitudes toward implant treatment and their opinions about aesthetics, function, comfort and satisfaction. The present pilot study evaluated patients’ experiences of surgical and prosthetic procedures as well as their opinions regarding function, aesthetics, comfort, and satisfaction with treatment outcomes.
Materials and methods
At the Oral Surgery Unit of the Odontostomatological and Maxillofacial Department - “Sapienza” University of Rome from September 2008 to September 2009, 49 patients (with 128 implants) were selected for implants procedures; they underwent first stage surgery to insert one or more implants. After about 5 months they underwent second stage of surgery to insert abutments and to take impressions. Prosthesis took about one month to be completed. After about four mounths prosthetic treatment was completed, they were asked to fill in a questionnaires on their opinions about the effectiveness of the implant restorative procedure, overall satisfaction and oral function outcome.
Three questionnaires were used related to implant-supported single-tooth implants, fixed implant-supported prostheses and implant-retained overdentures. Three of the 49 patients completed two questionnaires (one for each type of treatment), giving a total of 52 completed questionnaires. The questions were formulated by the authors based on outcomes of related studies and on topics of relevance to clinicians. To assess parameters, questions had multiple choice as mode of answers. The patients filled the questionnaires at the recall examination under supervision of one of the authors not involved in the treatment so as to avoid bias and the effects of interpersonal reactions.
Each questionnaire comprised 44 questions, with questions 1 to 38 being the same in each questionnaire, and questions 39 to 44 varying with the specific treatment. The first five questions related to demographic data: age, sex, employment, marital status and educational level. In questions 6 and 7, patients explained where they had obtained information about the implant treatment and why they decided to undergo it. Questions 8 to 23 asked patients about the discomfort related to implant surgery and abutment surgery or associated with impression-taking and prosthetic procedures, as well as their overall experience of the treatment. Questions 24 to 38 evaluated functional and aesthetic satisfaction, oral hygiene, cost-effectiveness, acceptance of implant-supported prostheses, and willingness to repeat treatment or to recommend it to other people. Questions 39 to 43 were identical for the implant-supported single tooth and for the fixed prosthesis, while question 44 of the single-tooth-implant questionnaire assessed aesthetics in anterior segments and that of the fixed prosthesis assessed chewing function. Questions 39 to 44 of the implant-supported overdenture questionnaire assessed prosthesis stability and phonetics.
The relatively small sample made it impossible to validate the questionnaires. The standard statistical and data management package SPSS (version 16.0 for Windows XP) was used for descriptive statistical analysis. Mean and standard deviation (SD) values were calculated. The outcomes are represented here on pie charts and histograms produced with Microsoft Excel.
Results
The survival rate of 128 implants installed in 49 patients was 97,65%. Only three implants did not osseointegrate, all of which were successfully inserted again. The follow-up period after the prosthetic reconstruction ranged from 6 to 24 months with a mean of 14 months.
The 52 collected questionnaires were distributed as follows: 24 on single-tooth implants, 21 on implant-supported fixed prostheses and 7 on implant-retained overdenture. Percentages of questions from 1 to 7 are based on the number of patients (n.49) and from 8 to 44 on the number of questionnaires (n.52).
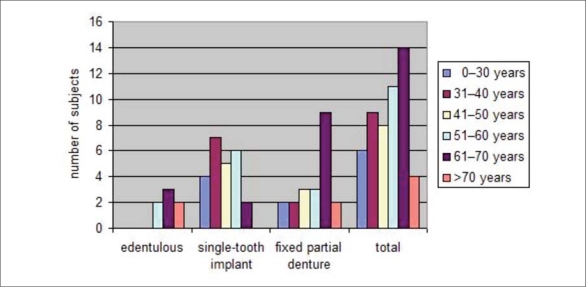
The 49 patients comprised 27 (55.1%) women and 22 (44.9%) men who ranged in age from 29 to 72 years, with a mean age of 51.16 years (SD=13.6 years). The decade between 61 and 70 years comprised the largest number of patients (26.9%) (Fig. 1).
Figure 1.
Distribution of patients by age.
Most of the patients were employed (53.8%) and retired (28,8%); 75% of them had received a high school certificate or a university diploma, 15,4% attended only medium school and 7,7% elementary school; patients had heard about implants from various sources, including referring dentists (55.8%), relatives and friends (23.1%), television, radio and the Internet (17.3%), newspapers (1.9%), and medical doctors (1.9%).
Patients who were partially or completely edentulous and who missed one anterior tooth considered it particularly necessary to restore lost teeth (34.6%). Other reasons for choosing implant treatment were the advice of a dentist (32.7%), improving the stability of the denture (15.4%), eating habits (13.5%) and aesthetics (1.9%).
The time to complete the treatment was consider enough long and long by 44.2% and 19.2% of our respondents, respectively. However, almost all (90,3%) of them considered that the procedures were not traumatic.
Implant insertion surgery was assessed negatively by only 3.8% of those who completed questionnaires. This finding could be attributable to the protocol used, because all the patients received diazepam per os before surgery to obtain conscious sedation, with consequent anterior amnesia of unpleasant remembrances.
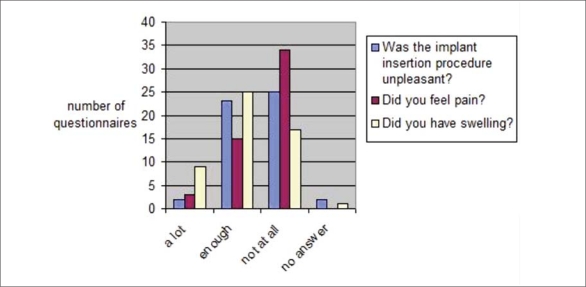
The post-operative period was free of complications in most cases. Pain was absent in 64.5% of the subjects, and only 5.8% experienced severe pain. Swelling was moderate and marked in 48.1% and 17.3% of the patients, respectively, with this often being correlated with the procedure complexity (Fig. 2).
Figure 2.
Did you experience pain and/or swelling after implant insertion procedure?
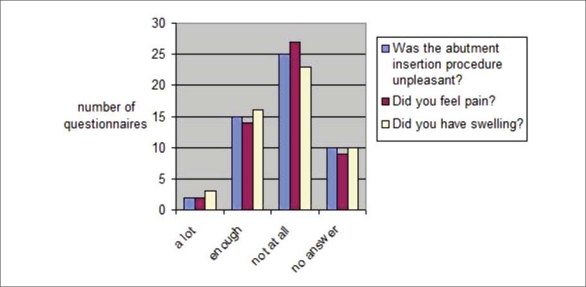
Abutment surgery was assessed positively by 76.9% of the subject: swelling and pain, which were often (Fig. 3).
Figure 3.
Did you experience pain and/or swelling in post-operative period after abutment insertion procedure?
The prosthetic procedure was evaluated as not unpleasant by 76.9% of the respondents in the present study, while 28.8% of them considered impression-taking to be the worst part of the procedure. Most of the patients in the present study (61.5%) considered the time between implant insertion and prosthesis rehabilitation to be acceptable, even when a temporary replacement was absent (63.5%). In remaining 36.5% of responders a removable provisional was used. The temporary removable replacement was viewed positively by the fully edentulous subjects and unpleasant by most of the subjects (63.5%) with implants restoring single crowns and fixed partial prosthesis. The temporary removable replacement was worn by 55% of subjects both day and night, and by 35% of them only during the day, while other subjects either did not wear it (5%) or only wore it when eating (5%). Almost half of the patients (47.4%) reported that the temporary rehabilitation functioned better after implant surgery. Almost all of the patients in the present study (94.2%) were satisfied with the chewing function (definitely in 44.2% of cases and adequate in 50% of cases) (Fig. 4).
Figure 4.
Are you satisfied of the implant-supported prosthesis functionally?
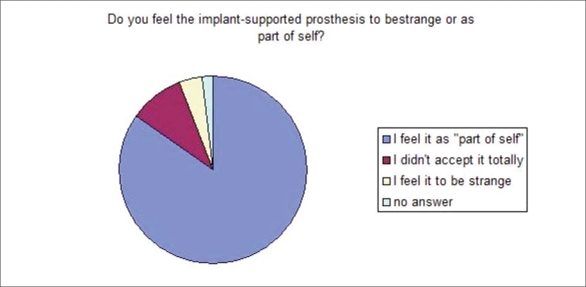
Chewing ability increased in 84.6% of our patients, with 82.7% being able to chew every kind of food and 84.6% considering that the prosthesis was comparable to their natural bite and that the construction was an integral part of their mouth (Fig. 5).
Figure 5.
Do you feel the implant-supported prosthesis to be strange or as part of yourself?
All the seven edentulous subjects in our study considered that the implant-supported overdenture provided improved stability and phonetics.
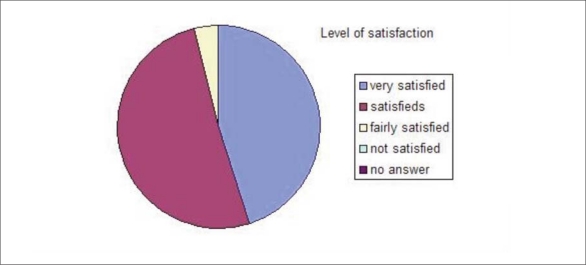
Most of our sample (82.8%) was completely satisfied with the aesthetic outcome, 15.4% were satisfied and only one person rated his implant-supported crown (upper lateral incisor) as not being very aesthetic.
Most of our respondents got used to the implant-supported prostheses either immediately (30.8%) or soon (65.4%) after the placement procedure; most of our patients (82.7%) were highly satisfied of the outcome of implant treatment, 86.5% were willing to have the same treatment performed again and 94.2% were willing to recommend the treatment to friends and relatives.
Most of our patients (69.2%) considered the cost of implant therapy to be reasonable.
Most of our respondents (65.4%) experienced a major change in their oral hygiene habits after implant insertion, and 73.1% found it easy to clean the implant reconstructions. In spite of this, only one-third of the patients increased their frequency of visiting a dentist for hygiene reasons and follow-up.
In the comparison between conventional and implant-supported prostheses, 42.2% of the subjects found the two procedures to be similar in time and quality, 76.2% did not find any difference between implants and teeth, and 70% could chew similarly with implants and teeth. Implants were perceived as a part of oneself, which constituted a very important advantage for the respondents.
Discussion
Our results show that people who undergo implant terapy can be male or female, of every age, especially after 50. Most of the patients were employed (53.8%) and 75% of them had received a high school certificate or a university diploma. In accordance with other studies (9,10,11), patients had heard about implants from various sources, especially referring dentists (55.8%) and relatives and friends (23.1%); television, radio and the Internet (17.3%), newspapers (1.9%) and medical doctors (1.9%) seem less important. Our outcomes were comparable with those of de Bruyn et al. (12). Those authors used a questionnaire to evaluate patients’ opinions on oral rehabilitation using implants, and found that only 27% of patients considered using additional types of information (brochures, slides or models) important to supporting an oral explanation. For 60% of those who completed questionnaires, an oral explanation had the greatest influence on the decision to undergo treatment. This might be due to too much information being difficult to handle and even leading to confusion or fear, because, as non-professionals, the patients might have difficulties in extrapolating information concerning their own oral condition. In contrast, a more client-centred approach appears to increase confidence in the procedure.
Patients who were partially or completely edentulous and who missed one anterior tooth considered it particularly necessary to restore lost teeth (34.6%). The main reasons for choosing implant treatment were the advice of a dentist (32.7%), improving the stability of the denture (15.4%), eating habits (13.5%) and aesthetics (1.9%). Analogous outcomes were reported by Grogono et al. (2), who assessed the attitudes of edentulous patients towards implant treatment, and by de Bruyn et al. (15).
Implant and abutment surgery were assessed positively by most of the subject: infact they were in most of the case painless and without swelling. Similar results were found in previous studies, such as by Schropp et al. (16) who used VAS scores to assess implant surgery. Their survey paper reported that patients rated implant insertion significantly worse than the abutment operation, and considered swelling but not pain to be a problem.
The prosthetic procedure was evaluated as not unpleasant by 76.9% of the respondents in the present study, while 28.8% of them considered impression-taking to be the worst part of the procedure. In contrast, Schropp et al. (16) found that approximately one-fourth of their respondents considered the prosthetic procedures unpleasant: namely, impression-taking, try-in and mounting of the crown. The temporary removable replacement was viewed positively by the fully edentulous subjects and unpleasant by most of the subjects (63.5%) with implants restoring single crowns and fixed partial prosthesis; infact the temporary removable replacement was worn by 55% of subjects both day and night, and by 35% of them only during the day, while other subjects either did not wear it (5%) or only wore it when eating (5%). Almost half of the patients (47.4%) reported that the temporary rehabilitation functioned better after implant surgery. These data did not support the outcome of Schropp et al. (16), who in approximately 60% of the cases of implant rehabilitation of incisors and canines decided—in concert with the patient—to make a removable partial denture as a temporary solution in the edentulous period. They found that most of their patients either did not wear their denture or only used it during the day. None of their patients considered that the denture function was influenced by insertion of the implant, and in only a few cases was the function impaired after the abutment operation.
Almost all of the patients in the present study (94.2%) were satisfied with the chewing, chewing ability increased in 84.6% of our patients, with 82.7% being able to chew every kind of food and 84.6% considering that the prosthesis was comparable to their natural bite and that the construction was an integral part of their mouth. These data are in accordance with Pjetursson et al. (17) finding that more than 90% of patients treated with crowns or implant-supported fixed partial denture were completely satisfied. Those authors compared the chewing function between natural teeth and implants, and found that 72.1% of their patients perceived no difference, and 7.7% of them preferred implants due to the adaptive capacity of the stomatognathic system following implant therapy (18).
This finding contrasted those of some other studies. Hämmerle et al. (19) showed that patient tactile perception differed significantly between implant abutments and natural abutments, and Keller et al. (20) demonstrated that the threshold for tactile perception in implants was increased after 1 week of healing and remained unchanged thereafter.
In accordance with other studies (21,22,23,24,25), the seven edentulous subjects in our study considered that the implant-supported overdenture provided improved stability and phonetics. In an investigation of the differences in patients’ psychological and psychosocial attitudes after receiving implant prostheses, Grogono et al. (2) found that many respondents improved their speaking ability. In addition, most of the patients smiled more often and felt more comfortable in their social contacts and in relationships with the opposite sex. Only a few respondents reported negative changes in attitude, and even when the responses were not totally positive, patients perceived that their implant prostheses were at least as satisfactory as their removable ones.
These outcomes were similar to those found in the survey of Zitmann et al. (5) of patients treated with fixed implant-supported prostheses in the maxilla. Those authors found significant improvements in aesthetics, eating comfort, phonetics and overall satisfaction. Equally, subjects interviewed by Blomberg and Lindquist (11) perceived their prosthesis to be part of themselves, and provided improvements in aesthetics, self-esteem and interpersonal relationships.
Most of our sample (82.8%) was completely satisfied with the aesthetic outcome, 15.4% were satisfied and only one person rated his implant-supported crown (upper lateral incisor) as not being very aesthetic. This is in agreement with high satisfaction levels found in other studies that have investigated patients’ opinions on implant-supported single-tooth replacements (6,16,17,26).
Most of our respondents got used to the implant-supported prostheses either immediately (30.8%) or soon (65.4%) after the placement procedure, as also reported by Pjetursson et al. (17). Those authors reported that some patients needed 2–3 months to get used to an implant reconstruction and for the implant to feel like natural teeth. In accordance with the studies of Grogono et al. (2) and de Bruyn et al. (15), most of our patients (82.7%) were highly satisfied of the outcome of implant treatment, 86.5% were willing to have the same treatment performed again and 94.2% were willing recommend the treatment to friends and relatives.
Most our patients (69.2%) considered the cost of implant therapy to be reasonable. This is probably due to our implant-supported prosthesis procedures being performed in a public hospital, with the patients paying only for the materials (prosthesis and implant). This resulted in the total cost of the treatment being considerably lower than in private practices. Therefore, our outcomes cannot be compared with all other studies (13,14), although they are in accordance with Pjetursson et al. (17) finding that 71% of patients considered the implant costs justified in private practice.
Most of our respondents (65.4%) experienced a major change in their oral hygiene habits after implant insertion, and 73.1% found it easy to clean the implant reconstructions. In spite of this, only one-third of the patients increased their frequency of visiting a dentist for hygiene reasons and follow-up. These data are in accordance with Pjetursson et al. (17) finding that the feasibility of and the time needed to clean the teeth after implant reconstruction did not differ for 50% and 70% of their patients, respectively. In contrast, Yi et al. (27,28) found that patients with implant-supported prostheses considered oral hygiene procedures to be more difficult than those for natural teeth.
Conclusions
The outcomes of the present study should be interpreted with caution because they are based on a relatively small sample and a relatively short observation time, although previous studies have found that the adaptation to masticatory function with implant reconstructions tends to improve with time after insertion. Furthermore, assessment of the treatment procedures and experience of the edentulous period can be influenced by memory and by the time and money spent.
In spite of these limitations, the present study shows that oral implant rehabilitation meets patients’ needs and demands. This is because oral function, aesthetics and well-being improve significantly with implant-supported prostheses, while surgical and prosthetic procedures are not considered traumatic, even though they are long and complex.
References
- 1.Albrektsson T, Blomberg S, Brånemark A, Carlsson GE. Edentulousness—an oral handicap. Patient reactions to treatment with jawbone-anchored prostheses. Journal of Oral Rehabilitation. 1987;14(6):503–511. doi: 10.1111/j.1365-2842.1987.tb00746.x. [DOI] [PubMed] [Google Scholar]
- 2.Grogono AL, Lancaster DM, Finger IM. Dental implants: a survey of patients’ attitudes. The Journal of Prosthetic Dentistry. 1989;62(5):573–576. doi: 10.1016/0022-3913(89)90082-6. [DOI] [PubMed] [Google Scholar]
- 3.Palmer RM, Smith BJ, Palmer PJ, Floyd PD. A prospective study of Astra single tooth implants. Clinical Oral Implants Research. 1997;8(3):173–9. doi: 10.1034/j.1600-0501.1997.080303.x. [DOI] [PubMed] [Google Scholar]
- 4.Lekholm U, Gröndahl K, Jemt T. Outcome of oral implant treatment in partially edentulous jaws followed 20 years in clinical function. Clin Implant Dent Relat Res. 2006;8(4):178–86. doi: 10.1111/j.1708-8208.2006.00019.x. [DOI] [PubMed] [Google Scholar]
- 5.Zitmann NU, Marinello CP. Treatment outcomes of fixed or removable implant-supported prostheses in the edentulous maxilla. Part I: patients’ assessments. The Journal of Prosthetic Dentistry. 2000;83(4):424–433. doi: 10.1016/s0022-3913(00)70037-0. [DOI] [PubMed] [Google Scholar]
- 6.Chang M, Odman PA, Wennström JL, Andersson B. Esthetic outcome of implant-supported single-tooth replacements assessed by the patient and by prosthodontists. The International Journal of Prosthodontics. 1999;12(4):335–341. [PubMed] [Google Scholar]
- 7.Adell R, Eriksson B, Lekholm U, Branemark PI, Jemt T. Long term follow up study of osseointergrated implants in the treatment of totally edentulous jaws. International Journal of Oral and Maxillofacial Implants. 1990;5(4):347–359. [PubMed] [Google Scholar]
- 8.Astrand P, Ahlqvist J, Gunne J, Nilson H. Implant treatment of patients with edentulous jaws: a 20-year follow-up. Clin Implant Dent Relat Res. 2008 Dec;10(4):207–17. doi: 10.1111/j.1708-8208.2007.00081.x. Epub 2008 Apr 1. [DOI] [PubMed] [Google Scholar]
- 9.Bergendal T, Engquist B. Implant-supported overdentures a longitudinal prospective study. International Journal of Oral and Maxillofacial Implants. 1998;13(2):253–62. [PubMed] [Google Scholar]
- 10.Gualini F, Gualini G, Cominelli R, Lekholm U. Outcome of Brånemark Novum implant treatment in edentulous mandibles: a retrospective 5-year follow-up study. Clin Implant Dent Relat Res. 2009 Dec;11(4):330–7. doi: 10.1111/j.1708-8208.2008.00118.x. Epub 2008 Sep 9. [DOI] [PubMed] [Google Scholar]
- 11.Blomberg S, Lindquist LW. Psychological reactions to edentulousness and treatment with jawbone-anchored bridges. Acta Psychiatrica Scandinavica. 1983;68(4):251–262. doi: 10.1111/j.1600-0447.1983.tb07005.x. [DOI] [PubMed] [Google Scholar]
- 12.Berge TI. Public awareness, information sources and evaluation of oral implant treatment in Norway. Clinical Oral Implants Research. 2000;11(5):401–408. doi: 10.1034/j.1600-0501.2000.011005401.x. [DOI] [PubMed] [Google Scholar]
- 13.Tepper G, Haas R, Mailath G, Teller C, Bernhart T, Monov G, Watzek G. Representative marketing-oriented study on implants in the Austrian population. II. Implant acceptance, patient-perceived cost and patient satisfaction. Clinical Oral Implants Research. 2003;14(5):634–642. doi: 10.1034/j.1600-0501.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 14.Tepper G, Haas R, Mailath G, Teller C, Zechner W, Watzak G, Watzek G. Representative marketing-oriented study on implants in the Austrian population. I. Level of information, sources of information and need for patient information. Clinical Oral Implants Research. 2003;14(5):621–633. doi: 10.1034/j.1600-0501.2003.00916.x. [DOI] [PubMed] [Google Scholar]
- 15.de Bruyn H, Collaert B, Lindén U, Björn AL. Patient’s opinion and treatment outcome of fixed rehabilitation on Brånemark implants. A 3-year follow-up study in private dental practices. Clinical Oral Implants Research. 1997;8(4):265–271. doi: 10.1034/j.1600-0501.1997.080403.x. [DOI] [PubMed] [Google Scholar]
- 16.Schropp L, Isidor F, Kostopoulos L, Wenzel A. Patient experience of, and satisfaction with, delayed-immediate vs delayed single-tooth implant placement. Clinical Oral Implants Research. 2004;15(4):498–503. doi: 10.1111/j.1600-0501.2004.01033.x. [DOI] [PubMed] [Google Scholar]
- 17.Pjetursson BE, Karoussis I, Bürgin W, Brägger U, Lang NP. Patients’ satisfaction following implant therapy. A 10-year prospective cohort study. Clinical Oral Implants Research. 2005;16(2):185–193. doi: 10.1111/j.1600-0501.2004.01094.x. [DOI] [PubMed] [Google Scholar]
- 18.Jakobs R, van Steenberghe D. Comparative evaluation of the oral tactile function by means of teeth or implant-supported prostheses. Clinical Oral Implants Research. 1991;2(2):75–80. doi: 10.1034/j.1600-0501.1991.020205.x. [DOI] [PubMed] [Google Scholar]
- 19.Hämmerle CH, Wagner D, Brägger U, Lussi A, Karayiannis A, Joss A, Lang NP. Threshold of tactile sensitivity perceived with dental endosseous implants and natural teeth. Clinical Oral Implants Research. 1995;6(2):83–90. doi: 10.1034/j.1600-0501.1995.060203.x. [DOI] [PubMed] [Google Scholar]
- 20.Keller D, Hämmerle CH, Lang ND. Threshold for tactile sensitivity perceived with dental implants remain unchanged during a healing phase of 3 months. Clinical Oral Implants Research. 1996;7(1):48–54. doi: 10.1034/j.1600-0501.1996.070106.x. [DOI] [PubMed] [Google Scholar]
- 21.Cibirka RM, Razzoog M, Lang BR. Critical evaluation of patient responses to dental implant therapy. The Journal of Prosthetic Dentistry. 1997;78(6):574–581. doi: 10.1016/s0022-3913(97)70008-8. [DOI] [PubMed] [Google Scholar]
- 22.Boerrigter EM, Stegenga B, Raghoebar GM, Boering G. Patient satisfaction and chewing ability with implant-retained mandibular overdentures: a comparison with new complete dentures with or without preprosthetic surgery. Journal of Oral and Maxillofacial Surgery. 1995;53(10):1167–1173. doi: 10.1016/0278-2391(95)90627-4. [DOI] [PubMed] [Google Scholar]
- 23.Boerrigter EM, Geertman ME, Van Oort RP, Bouma J, Raghoebar GM, van Waas MA, Van’t Hof MA, Boering G, Kalk W. Patient satisfaction with implant-retained mandibular overdentures. A comparison with new complete dentures not retained by implants—a multicentre randomized clinical trial. British Journal of Oral and Maxillofacial Surgery. 1995;33(5):282–288. doi: 10.1016/0266-4356(95)90038-1. [DOI] [PubMed] [Google Scholar]
- 24.Wismeijer D, Vermeeren JI, van Waas MA. Patient satisfaction with overdentures supported by one-stage TPS implants. The International Journal of Oral and Maxillofacial Implants. 1992;7(1):51–55. [PubMed] [Google Scholar]
- 25.Bakke M, Holm N, Gotfredsen K. Masticatory function and patient satisfaction with implant-supported mandibular over-dentures: a prospective 5-year study. The International Journal of Prosthodontics. 2002;15(6):575–581. [PubMed] [Google Scholar]
- 26.Vermylen K, Collaert B, Lindén U, Björn AL, De Bruyn H. Patient satisfaction and quality of single-tooth restorations. Clinical Oral Implants Research. 2003;14(1):119–124. doi: 10.1034/j.1600-0501.2003.140116.x. [DOI] [PubMed] [Google Scholar]
- 27.Yi S-W, Carlsson GE, Ericsson I, Kim CK. Patient evaluation of treatment with fixed implant-supported partial dentures. Journal of Oral Rehabilitation. 2001;28(11):998–1002. doi: 10.1046/j.1365-2842.2001.00819.x. [DOI] [PubMed] [Google Scholar]
- 28.Yi S-W, Carlsson GE, Ericsson I, Wennström JL. Long-term follow up of cross-arch fixed partial dentures in patients with advanced periodontal destruction: evaluation of occlusion and subjective function. Journal of Oral Rehabilitation. 1996;23(3):186–196. doi: 10.1111/j.1365-2842.1996.tb01232.x. [DOI] [PubMed] [Google Scholar]