Abstract
Object
Detailed costs to individuals with hydrocephalus and their families as well as to third-party payers have not been previously described. The purpose of this study was to determine the primary caregiver out-of-pocket expenses and the third-party payer reimbursement rate associated with a shunt failure episode.
Methods
A retrospective study of children born between 2000 and 2005 who underwent initial ventriculoperitoneal (VP) shunt placement and who subsequently experienced a shunt failure requiring surgical intervention within 2 years of their initial shunt placement was conducted. Institutional reimbursement and demographic data from Children’s Hospital of Alabama (CHA) were augmented with a caregiver survey of any out-of pocket expenses encountered during the shunt failure episode. Institutional reimbursements and caregiver out-of-pocket expenses were then combined to provide the cost for a shunt failure episode at CHA.
Results
For shunt failures, the median reimbursement total was $5008 (interquartile range [IQR] $2068–$17,984), the median caregiver out-of-pocket expenses was $419 (IQR $251–$1112), and the median total cost was $5411 (IQR $2428–$18,582). Private insurance reimbursed at a median rate of $5074 (IQR $2170–$14,852) compared with public insurance, which reimbursed at a median rate of $4800 (IQR $1876–$19,395). Caregivers with private insurance reported a median $963 (IQR $322–$1741) for out-of-pocket expenses, whereas caregivers with public insurance reported a median $391 (IQR $241–$554) for out-of-pocket expenses (p = 0.017).
Conclusions
This study confirmed that private insurance reimbursed at a higher rate, and that although patients had a shorter length of stay as compared with those with public insurance, their out-of-pocket expenses associated with a shunt failure episode were greater. However, it could not be determined if the significant difference in out-of-pocket expenses between those with private and those with public insurance was due directly to the cost of shunt failure. This model does not take into consideration community resources and services available to those with public insurance. These resources and services could offset the out-of-pocket burden, and therefore should be considered in future cost models.
Keywords: cost analysis, pediatric hydrocephalus, ventriculoperitoneal shunt
Understanding medical costs surrounding chronic illnesses is a priority among researchers, hospital administrators, and third-party payers. Equally, and potentially more importantly, there is a need to understand the short- and long-term costs experienced by families caring for children with chronic illnesses. Previous research has established that chronic childhood illnesses increase the financial burden to the family unit, as measured by wage and labor outcomes, maternal employment status, access to services and resources, transportation costs, and costs associated with the care of siblings.5,6,8,16 Compared with those without a chronically ill child, families with such a child report lower maternal and paternal employment rates, and lower wages when parents work.7 In addition, families with lower socioeconomic status are more likely to report financial problems.6 The financial burden to families increases over time as the severity of the condition and need for care for the child increase.
Medical costs associated with childhood hydrocephalus are poorly understood, but they appear to be increasing. Previous studies have assessed the treatment of hydrocephalus based on hospital charges alone.8,15 The management of hydrocephalus in children has seen a 34% increase in hospital utilization and LOS in the US over the last decade, 15,17 accounting for more than an estimated $100 million of national health care expenditures annually.2,18 In a recently published cross-sectional study, Simon et al.19 found that inpatient pediatric hydrocephalus accounted for approximately 38,000 admissions and 400,000 hospital days. Hydrocephalus accounted for 3.1% of all pediatric acute care hospital charges ($1.4–$2.0 billion for the year 2003), while cystic fibrosis accounted for 2.9% of hospital charges. This study concluded that children with hydrocephalus use a disproportionate share of hospital days and health care dollars. However, these studies have estimated charges to the overall health care system. Costs to individuals with hydrocephalus and their families as well as the costs to third-party payers have not been previously described.
As seen in previously conducted research, chronic childhood illnesses increase the financial burden to the family unit. Families caring for children with hydrocephalus incur out-of-pocket expenses each time their child has a shunt failure episode. This study is based on the hypothesis that hydrocephalus is no different from other chronic childhood illnesses, and its objectives were to determine the third-party payer reimbursement rate for a VP shunt failure episode, and out-of-pocket expenses associated with shunt failure episodes.
Methods
Study Design
A retrospective observational study of patients who underwent initial VP shunt placement at the CHA and who subsequently experienced shunt failure was conducted. Patients meeting these eligibility criteria were identified, administrative data for their hospitalizations were obtained, and caregiver surveys were administered. The University of Alabama at Birmingham’s institutional review board approved the study (No. X070718006).
Patient Population
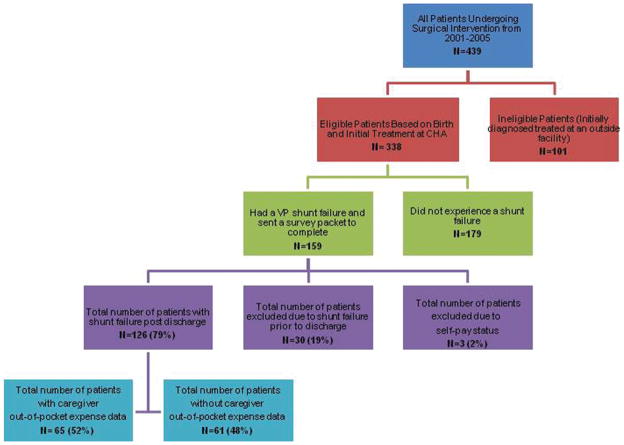
Among the 439 patients undergoing surgical intervention for CSF diversion at CHA, including initial shunt insertion and subsequent revisions with VP, ventriculoatrial, and ventriculopleural shunts between the years 2001 and 2005, 338 patients underwent initial VP shunt placement for hydrocephalus. One hundred fifty-nine (47%) experienced a shunt failure episode within 2 years after hospitalization for the initial VP shunt placement, and most failures occurred within the first 6 months (see Fig. 1). Thirty patients who experienced a shunt failure prior to discharge from initial hospitalization, and 3 patients who were considered self-paid and were not enrolled in a state insurance program during their initial admission were excluded, leaving 126 patients in the study cohort.
Fig. 1.
Flowchart showing patient and survey response breakdown. N = number of participants.
Data Collection
Administrative Data
Administrative datasets from CHA provided eligible patients as well as reimbursement and demographic data. For this study, shunt failure was defined as an episode of symptoms requiring hospitalization and surgical intervention for replacement of all or part of the VP shunt system.
Institutional reimbursement data incurred during a shunt failure episode from CHA and the Health Services Foundation of the University of Alabama at Birmingham were obtained. These included patient-level third-party payer reimbursement data for hospital, physician, and ED reimbursements, and the LOS. For our analysis, only reimbursement data were used and charges were avoided, since it is not possible to determine the percentage of the reimbursement assigned to each itemized charge. Additionally, any visits to the ED for evaluation of shunt failure (as determined by the ICD-9-CM diagnosis code V45.2 for postsurgical presence of a CSF drainage device), and up to 90 days of the patient’s required hospitalization for shunt failure, were included as part of the shunt failure episode. The ED reimbursements were only included if the visit was to evaluate the patient’s signs and symptoms related to shunt failure, and occurred within the 90-day period of the hospitalization for shunt failure. The 90-day period is consistent with the so-called global fee period used by third-party payers, which includes preoperative clinic visit, admission and stay for surgical intervention, and routine postoperative follow-up. Reimbursements for direct admission through the ED were included in the hospital reimbursement data, and therefore were not included as a separate category in the analysis.
Demographic variables obtained included sex, race, insurance status, and address for primary residence. Race was categorized according to National Institutes of Health guidelines.11 Electronic medical records were reviewed to obtain the source of hydrocephalus, patient age, and all clinical data collected during the care of the patient. The source of hydrocephalus was categorized as acquired (including intraventricular hemorrhage, meningitis, tumor, and posttraumatic brain injury) or congenital (including spina bifida, genetic disorder, Dandy-Walker syndrome, hydranencephaly, arachnoid cyst, and aqueductal stenosis). Primary insurance status was categorized at the time of shunt failure as private (including BlueCross BlueShield, commercial, military, and HMO [health maintenance organization]) or public (including Medicaid, AlKids, and SCHIP [State Children’s Health Insurance Program]); no secondary insurance provider was included.
Caregiver Surveys
A survey asking for details of out-of-pocket expenses encountered during their child’s first shunt failure episode (transportation cost, food and lodging, sibling child care expenses, and copayments) was mailed out to 126 caregivers.
Data Analysis
Univariate analyses were performed to describe study enrollment and patient characteristics by using nonparametric statistics. Bivariate analyses were performed using the Mann-Whitney test to compare survey responders to nonresponders, and to compare the cost of shunt failure by insurance status and failure type. The Wilcoxon rank-sum test and the Kruskal-Wallis test were used to compare population medians. Testing for normality was not conducted in this cohort, and whether the survey responders represent the target population could not be determined. Medians and interquartile ranges were used throughout the analysis. Due to the small sample size, multivariate analysis was not conducted. All analyses were conducted using SAS version 9.2 software.
Adjustment for inflation over the study period was performed using the Bureau of Labor Statistics Consumer Price Index inflation calculator, and 2009 was used as the comparison year, so all costs are reported in 2009 dollars. The reimbursement total represents the sum of the total third-party payer reimbursements for hospital, physician, and ED charges related to the initial shunt failure episode. Caregiver out-of-pocket expenses were composed of the total self-reported expenses incurred by the primary caregiver during the shunt failure episode, and included transportation, mileage, food and lodging, child care costs for siblings, and copayments. Total cost was therefore the sum of any reimbursement or out-of-pocket expenses related to the initial shunt failure episode.
Distance in miles and time from the primary household to CHA was determined using an online tool in which a geocoding algorithm was used to estimate the latitude and longitude of the address of interest by US post office data (MapQuest). Determination of mileage cost associated with caregiver out-of-pocket expenses was accomplished by multiplying the mileage estimate by $0.55, which was the current National Institutes of Health governmental rate for mileage reimbursement.
The LOS was defined as the total number of in-patient hospital days associated with the shunt failure episode.
Results
Characteristics of the Study Population
We identified 126 patients with a shunt failure episode. Sixty-five caregivers (52%) returned the survey with out-of-pocket expenses noted. The remaining 61 (48%) did not return the survey, and therefore out-of-pocket expenses were not captured for these caregivers (Fig. 1). We are not able to conclude whether the caregiver was unable to recall this information or if no out-of-pocket expenses were incurred by the caregiver during the shunt failure episode. Of the combined cohort, 62% were male, and non-Hispanic white patients were the majority (60%) of our study population, followed by African American (37%), and the remaining 3% were either Hispanic or “other.” Insurance mix coverage was divided, with 46% private and 54% public insurance. Of the 126 patients included in the study, 67 (53%) of them had acquired, 57 (45%) had congenital, and 2 (2%) had hydrocephalus of unknown origin. The majority of shunt failures were categorized as due to shunt obstruction (69%) or shunt infection (17%). The median gestational age was 35.5 weeks, and the median age at initial VP shunt placement was 2.41 months (Table 1).
TABLE 1.
Descriptive characteristics of survey responders versus nonresponders on behalf of 126 patients with a shunt failure episode
| Characteristic | No. of Responders (%) | No. of Nonresponders (%) | p Value |
|---|---|---|---|
| no. of patients | 65 | 61 | |
| sex of patient | 0.65 | ||
| F | 24 (35) | 24 (39) | |
| M | 41 (63) | 37 (61) | |
| race of patient | 0.83 | ||
| non-Hispanic white | 42 (65) | 34 (56) | |
| African American | 21 (32) | 25 (41) | |
| Hispanic | 1 (2) | 2 (3) | |
| other | 1 (1) | 0 | |
| insurance status | 0.46 | ||
| private | 32 (49) | 26 (43) | |
| public | 33 (51) | 35 (57) | |
| origin of hydrocephalus | 0.26 | ||
| acquired | 30 (46) | 37 (61) | |
| congenital | 34 (52) | 23 (38) | |
| unknown | 1 (2) | 1 (1) | |
| type of initial shunt failure | 0.14 | ||
| obstruction | 42 (63) | 46 (75) | |
| infection | 14 (22) | 7 (11) | |
| other | 9 (15) | 8 (12) | |
| median gestational age of patient | 37 wks | 34 wks | 0.005 |
| median patient age at time of initial shunt insertion | 3.1 mos | 2 mos | 0.44 |
Treatment Costs
For shunt failures at our institution, the median reimbursement total for this study cohort was $5008 (IQR $2068–$17,984), the median caregiver out-of-pocket expenses was $419 (IQR $251–$1112), and the median total cost was $5411 (IQR $2428–$18,582).
Cost was further examined by insurance status and by type of shunt failure (Tables 2 and 3). The median reimbursement for private third-party payers was $5074, versus $4800 for public third-party payers, which was not statistically significant. Caregivers with private insurance experienced a median exposure of $963 for out-of-pocket expenses, while caregivers with public insurance had a median $391 for out-of-pocket expenses, which was significant (p = 0.017). Third-party payer reimbursement totals were found to be significant (p = 0.002) when comparing failure type. The median reimbursement totals for obstructions and infections were $3710 (IQR $1767–$7795) and $23,728 (IQR $20,806–$37,809), respectively. Caregiver out-of-pocket expenses differed between types of shunt failure: $361 for obstruction and $472 for infection (p = 0.027). Distance from the primary household to CHA was found to be statistically significant, with patients who had private insurers living 103.6 miles from CHA, compared with the 52.7 miles that patients who had public insurers had to travel to CHA (p < 0.0005). The LOS and distance to CHA were found to be inversely correlated (Pearson coefficient −0.27). For every additional mile traveled to CHA there was a reduction in LOS of 0.05 days.
TABLE 2.
The median cost of a shunt failure episode by insurance status (private vs public)*
| Category | No. of Patients | Private (58 patients)
|
Public (68 patients)
|
p Value | ||
|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | |||
| reimbursement total | 126 | $5074 | $2170–14,852 | $4800 | $1876–19,395 | 0.677 |
| caregiver out-of-pocket expenses† | 65 | $963 | $322–1741 | $391 | $241–554 | 0.017 |
| total cost of episode | 126 | $5828 | $2445–14,852 | $4800 | $1979–20,039 | 0.508 |
| distance in miles from primary household to CHA† | 65 | 103.64 | 46.4–146.4 | 52.7 | 30.9–98.2 | <0.0005 |
| LOS in days | 126 | 2 | 1–4 | 3 | 1–10.5 | 0.038 |
For this table, 32 responders had private insurance and 33 had public insurance.
Caregiver out-of-pocket expenses and distance from CHA were only captured if the primary caregiver responded to the survey.
TABLE 3.
The median cost of a shunt failure episode comparing obstruction versus infection*
| Category | No. of Patients | Obstruction (87 patients)
|
Infection (21 patients)
|
p Value | ||
|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | |||
| reimbursement total | 126 | $3710 | $1767–7795 | $23,728 | $20,806–37,809 | <0.0001 |
| caregiver out-of-pocket expenses† | 55 | $361 | $234–1000 | $472 | $397–1017 | 0.027 |
| total cost of episode | 126 | $3964 | $2029–8951 | $23,541 | $20,806–39,561 | <0.0001 |
| distance in miles from primary household to CHA† | 55 | 69.09 | 32–112 | 71.03 | 40–178 | 0.825 |
| LOS in days | 126 | 2 | 1–3 | 12 | 9–15 | <0.0001 |
For this table, 44 responders’ children were noted to have a shunt obstruction and 14 were noted to have a shunt infection.
Caregiver out-of-pocket expenses and distance from CHA were only captured if the primary caregiver responded to the survey.
Length of Stay
A statistically significant difference was seen in LOS between those with private insurance and those with public insurance: 2 days versus 3 days, respectively. The median hospital LOS for a shunt failure episode ranged from 2 days for obstruction to 12 days for infection (p < 0.0001). Several outliers existed in our cohort, with a maximum LOS for obstruction and infection of 71 and 47 days, respectively. The difference in LOS between patients in each of the insurance groups could be associated with the number of shunt infections seen: 7 for private insurance versus 14 for public insurance. However, based on standard practice at our institution, a shunt infection requires a 10- to 14-day stay, with administration of antibiotics, and 3 consecutive CSF cultures with negative results prior to a new shunt placement. Only 6 patients in our cohort experienced extensive hospital LOSs, and only 1 of those had a shunt failure episode due to shunt infection. Additionally, LOS was correlated with both out-of-pocket expenses and reimbursement totals, at p = 0.0005 and < 0.0001, respectively.
Discussion
As with other chronic childhood illnesses, shunted hydrocephalus requires a lifetime of management, often requiring multiple surgical interventions for manipulation or replacement of a child’s implanted shunt system. This study examined the costs associated with initial VP shunt failure, including third-party payer reimbursement and the out-of-pocket expenses caregivers incurred during a shunt failure episode. Length of stay, third-party payer reimbursement rate, and caregiver out-of-pocket expenses incurred during a shunt failure episode were all found to be associated with the type of shunt failure (that is, obstruction or infection). Although all shunt failure types lead to a surgical intervention requiring new implants for either part or all of the shunt system, these 2 particular failure types are dissimilar with regard to management. Shunt obstruction is often treated with a single surgical intervention (revision of the obstructed catheter or valve only), whereas shunt infections require at least 2 surgical interventions (removal of the entire existing shunt system and insertion of a new one after 3 confirmed negative results for CSF cultures) and a course of antibiotics for 7–14 days, making this particular type of failure more costly. The increased LOS required to treat a shunt infection not only puts a patient at higher risk for additional infection, but also increases out-of-pocket expenses incurred by the caregiver.1,3,18 Shunts that are poorly placed or those with malfunctions such as a CSF leak or loculated ventricles are often more difficult to treat and lead to additional procedures, including diagnostic scans, and longer hospitalizations. Given the recent pressure from state governments for hospitals to implement patient safety guidelines and quality improvement programs to improve overall outcomes for patients,4,9–13,20,21 it is important to maximize the reduction in the frequency of shunt failure episodes (especially as a result of shunt infections) experienced by this patient population.
Insurance status was associated with caregiver out-of-pocket expenses incurred in this study. Those patients with private insurance had a greater amount of out-of-pocket expenses than those with public insurance. There are several reasons that could explain these findings. We cannot dismiss the fact that in general those with private insurance often have more disposable income to use when making food, lodging, and travel choices. Therefore it could be possible that the association is not due to any significant factors other than household income. However, within the study population, the median distance from the primary household to CHA for those with private insurance was 103.6 miles, compared with the 52.7 miles for those with public insurance. Increased distance could impact gasoline expenses, as well as the number of days that food and lodging expenses accumulated. Second, private insurance usually carries with it a copayment for hospitalization and prescriptions, compared with the much lower or even nonexistent copayment requirements and prescription costs for those with public insurance. These expenses can greatly impact out-of-pocket expenses. Additionally, caregivers who receive public insurance usually also qualify for other governmental or public health services such as transportation vouchers, food vouchers, and reduced prescription costs. Although out-of-pocket expenses would be a direct reflection on household income and disposable income, other factors, including distance between home and hospital and eligibility for governmental programs, also impact the expenses that families incur per hospitalization.
This study allowed the assessment of the cost of shunt failure in a single institution with a large patient population. To achieve a more homogeneous patient population, patients who were previously treated at another facility and/ or experienced their initial shunt failure prior to discharge from their initial VP shunt hospitalization were excluded; however, these are also potentially more costly hospitalizations. Hospital-level reimbursement data were used that provided a more accurate picture of the financial impact associated with a shunt failure episode at the individual patient level. A patient caregiver component was added to this analysis, which has not received a great deal of attention in the literature. One limitation of this study was the average survey response rate of 52%. Had the study timeline permitted, follow-up phone calls might have increased the response rate, thereby adding additional power to our analysis. However, our results showed that there were no differences in participant characteristics among those who responded and those who did not respond to the survey. Therefore, we can assume a representative sample. Another limitation of this study was the lack of information about the caregiver’s indirect costs associated with a shunt failure episode. Capturing information regarding type of employment (salaried vs hourly), time off from work due to their child’s shunt failure episode, and lost wages would allow us to understand the financial burden on the family unit and the potential barrier to health care access these caregivers face.
Conclusions
The purpose of this study was to evaluate the costs associated with initial VP shunt failure. The cost of shunt failure has been previously reviewed in the literature by using CPT codes and ICD-9 codes, and these studies looked specifically at overall costs. This study took a different approach, as follows: 1) we used patient-level reimbursements; and 2) indirect costs incurred by caregivers during their child’s hospitalization. Type of shunt failure and insurance status were 2 factors found to be associated with total reimbursement, out-of-pocket expenses, and LOS. The financial effects that distance from CHA and eligibility for additional resources and services have on the cost of shunt failure are not elucidated by this study. A case-control study looking at patients treated for a shunt failure compared with those who did not experience a shunt failure is currently being developed for further estimation of the financial impact and “real world” costs associated with a shunt failure episode.
Acknowledgments
The authors gratefully acknowledge the editorial assistance of Amelia Boehme and Dr. Beverly Walters in the preparation of this manuscript.
Abbreviations used in this paper
- CHA
Children’s Hospital of Alabama
- CPT
Current Procedural Terminology
- ED
emergency department
- IQR
interquartile range
- LOS
length of stay
- VP
ventriculoperitoneal
Footnotes
Disclosure
None of the authors have potential financial or personal conflicts of interest to disclose.
Author contributions to the study and manuscript preparation include the following. Conception and design: Shannon. Acquisition of data: Shannon, Reed. Analysis and interpretation of data: Shannon. Drafting the article: Shannon. Critically revising the article: all authors. Reviewed submitted version of manuscript: all authors. Approved the final version of the manuscript on behalf of all authors: Shannon. Statistical analysis: Shannon, Kilgore. Administrative/technical/material support: Reed. Study supervision: Shannon, Franklin, Kirby, Kilgore. Clinical mentor: Wellons.
References
- 1.Arthur AS, Whitehead WE, Kestle JR. Duration of antibiotic therapy for the treatment of shunt infection: a surgeon and patient survey. Pediatr Neurosurg. 2002;36:256–259. doi: 10.1159/000058429. [DOI] [PubMed] [Google Scholar]
- 2.Bondurant CP, Jimenez DF. Epidemiology of cerebrospinal fluid shunting. Pediatr Neurosurg. 1995;23:254–259. doi: 10.1159/000120968. [DOI] [PubMed] [Google Scholar]
- 3.Cochrane D, Kestle J, Steinbok P, Evans D, Heron N. Model for the cost analysis of shunted hydrocephalic children. Pediatr Neurosurg. 1995;23:14–19. doi: 10.1159/000120930. [DOI] [PubMed] [Google Scholar]
- 4.Fla Stat. Hospital licensing and regulation: internal risk management program. Title XXIX, ch 395, §0197, 2003
- 5.Hwang W, Weller W, Ireys H, Anderson G. Out-of-pocket medical spending for care of chronic conditions. Health Aff (Millwood) 2001;20:267–278. doi: 10.1377/hlthaff.20.6.267. [DOI] [PubMed] [Google Scholar]
- 6.Kuhlthau K, Hill KS, Yucel R, Perrin JM. Financial burden for families of children with special health care needs. Matern Child Health J. 2005;9:207–218. doi: 10.1007/s10995-005-4870-x. [DOI] [PubMed] [Google Scholar]
- 7.Kuhlthau KA, Perrin JM. Child health status and parental employment. Arch Pediatr Adolesc Med. 2001;155:1346–1350. doi: 10.1001/archpedi.155.12.1346. [DOI] [PubMed] [Google Scholar]
- 8.McCallum JE, Turbeville D. Cost and outcome in a series of shunted premature infants with intraventricular hemorrhage. Pediatr Neurosurg. 1994;20:63–67. doi: 10.1159/000120766. [DOI] [PubMed] [Google Scholar]
- 9.Me Stat. Facilities for children and adults: sentinel event reporting. Title 22, ch 1684, §8753, 2002
- 10.Mo. Patient safety and quality improvements act. S720 and HR663, 2004
- 11.National Institutes of Health, US Department of Health and Human Services. NIH Policy on Reporting Race and Ethnicity Data: Subjects in Clinical Research. Bethesda, MD: National Institutes of Health; 2001. [Google Scholar]
- 12.Nev Rev Stat. Mandatory reporting of sentinel events and patient safety committee. 2002 Special Session 13–15 ed, 2003
- 13.New York Hospital Infection Disclosure Act. S7766, §2805- q, 2004
- 14.NJ Administrative Code. Hospital Licensing Standards. Title 8, ch 43G, 2000
- 15.Patwardhan RV, Nanda A. Implanted ventricular shunts in the United States: the billion-dollar-a-year cost of hydrocephalus treatment. Neurosurgery. 2005;56:139–145. doi: 10.1227/01.neu.0000146206.40375.41. [DOI] [PubMed] [Google Scholar]
- 16.Pikus HJ, Levy ML, Gans W, Mendel E, McComb JG. Outcome, cost analysis, and long-term follow-up in preterm infants with massive grade IV germinal matrix hemorrhage and progressive hydrocephalus. Neurosurgery. 1997;40:983–989. doi: 10.1097/00006123-199705000-00021. [DOI] [PubMed] [Google Scholar]
- 17.PricewaterhouseCoopers. Cost of caring: key drivers of growth in spending on hospital care. Executive summary; Presented to: The American Hospital Association and The Federation of American Hospitals; February 19, 2003; Washington, DC. [Accessed September 27, 2011]. ( http://www.aha.org/content/00-10/CostsReportSummary.ppt) [Google Scholar]
- 18.Sciubba DM, Lin LM, Woodworth GF, McGirt MJ, Carson B, Jallo GI. Factors contributing to the medical costs of cerebrospinal fluid shunt infection treatment in pediatric patients with standard shunt components compared with those in patients with antibiotic impregnated components. Neurosurg Focus. 2007;22(4):E9. doi: 10.3171/foc.2007.22.4.11. [DOI] [PubMed] [Google Scholar]
- 19.Simon TD, Riva-Cambrin J, Srivastava R, Bratton SL, Dean JM, Kestle JR. Hospital care for children with hydrocephalus in the United States: utilization, charges, comorbidities, and deaths. J Neurosurg Pediatr. 2008;1:131–137. doi: 10.3171/PED/2008/1/2/131. [DOI] [PubMed] [Google Scholar]
- 20.Tenn Senate Bill SB1855, Title 68, ch 11, §201, 2005
- 21.Wash Administrative Code. Hospital licensing regulations: hospital leadership. WAC 246-320-145, 2004