Abstract
When performing reconstruction of the ACL, the major complications that can arise include missed concomitant injuries, tunnel malposition, patellar fracture, knee stiffness, and infection. We review the complications that can occur as a result of errors made before, during, and after surgery.
Avoidance of Major Complications
To ensure functional ROM and ultimate knee stability, the surgeon must carefully examine the injured knee and correlate findings to preoperative imaging; use anatomic landmarks and imaging as necessary to ensure adequate tunnel placement; harvest grafts in a meticulous fashion; tension grafts appropriately; and use sterile technique and trusted donor graft sources to minimize infection.
Detection and Treatment of Major Complications
Concomitant injuries must be recognized and surgically treated if necessary (eg, reconstruction of the posterolateral corner, meniscus repair, etc). Misplaced femoral and tibial tunnels should be revised to their anatomic position, fractures should be anatomically reduced and early ROM begun, knee stiffness should be treated with aggressive rehabilitation or lysis of adhesions when necessary, and infection should be treated with irrigation and debridement with or without preservation of the graft.
Summary
Rupture of the ACL, once a devastating and career-ending injury for athletes, is now amenable to surgical reconstruction so refined that the injured athlete often returns to high-level performance. Nonetheless, there are many pitfalls and potential problems associated with ACL reconstruction. In this article, the problems associated with diagnosis and judgment (Table 1; Fig. 1); graft harvest (Table 2), graft sizing (Table 3), graft placement and fixation (Table 4; Figs. 2 and 3); and postoperative care are presented (Table 5). The goal of ACL reconstruction is to offer the patient a functional, pain-free, and stable joint. With attention to the issues presented here, the surgeon is more apt to deliver on that promise.
Table 1.
Complications related to errors in diagnosis and judgment
| Complication | Clinical effect | Prevention | Detection | Remedy |
|---|---|---|---|---|
| Performing surgery too soon after injury [20, 26] | Postoperative stiffness | Postpone surgery until full extension and 90° flexion are attained | Poor motion postoperative | Aggressive physical therapy; manipulation under anesthesia +/− arthroscopy |
| Performing surgery too late [6, 28] | Damage to the meniscus and articular cartilage may result from persistent instability | Patient education regarding limited activities; informed consent for nonoperative treatment; bracing | MRI may detect disorder if recurrent instability has occurred | Treat lesions as they arise |
| Incorrect diagnosis: MRI or preoperative examination is falsely positive [24] | Removing an intact ACL and replacing it is clearly harmful to the patient | Careful history and examination; consider differential diagnosis (ie, quadriceps insufficiency); high resolution MRI with musculoskeletal radiologist | Thorough examination under anesthesia (ie, pivot shift, Lachman test); intraoperative observation and assessment of integrity | Abort reconstruction and treat the underlying diagnosis |
| Missed additional diagnosis: MCL/medial capsule injury [30] | Persistent pain and valgus instability may result with ultimate failure of the ACL reconstruction | Careful history and examination with valgus stress at 0° and 30° flexion and anterior drawer with external rotation;scrutinize MRI | Persistent valgus laxity at 0° and 30° flexion; presence of anteromedial rotatory instability; ACL reconstruction failure | Bracing MCL injuries early to promote healing; surgical repair versus reconstruction, capsular plication |
| Missed additional diagnosis: posterolateral corner injury [23] | Persistent varus instability and development of a varus thrust with ultimate failure of the ACL reconstruction | Careful history and examination with varus stress at 0° and 30° flexion; scrutinize MRI | Varus laxity at 0° and 30° flexion; presence of posterolateral rotatory instability with dial test | Surgical repair versus reconstruction of the damaged structures |
| Missed additional diagnosis: meniscal tear [12] | Persistent posterior joint line pain after ACL reconstruction | Careful history and examination; MRI to assess coronal and sagittal sequences; posteromedial portal for complete observation and Gillquist view (Fig. 1) | Postoperatively noted by persistent joint line pain and mechanical symptoms | Meniscal repair for red-red and red-white tears versus meniscectomy for complex/ irreparable tears |
ACL = anterior cruciate ligament; MCL = medial collateral ligament.
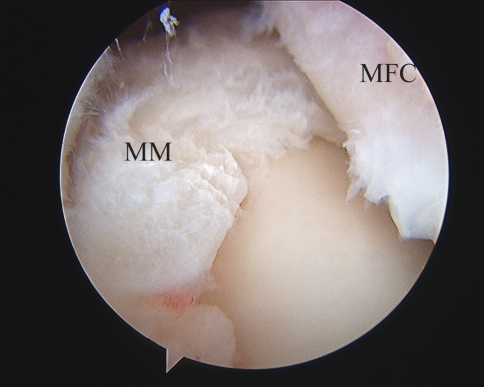
Fig. 1.
The posterior horn and root attachment of the medial meniscus are seen with the arthroscope positioned under the posteromedial bundle of the PCL, along the lateral aspect of the medial femoral condyle in this Gillquist view [10]. Meniscal root tears and far posterior horn tears can be missed if a detailed arthroscopic examination is not performed. (MFC = medial femoral condyle; MM = posterior horn attachment of medial meniscus).
Table 2.
Complications related to graft harvest
| Complication | Clinical effect | Prevention | Detection | Remedy |
|---|---|---|---|---|
| Graft dropped during surgery [5] | Contaminated graft and risk of infection | Careful intraoperative technique with suture fixation and clamps to secure grafts to field | Easily detected during surgery | Sterilize the graft with chlorhexidine 2%; harvest contralateral graft (BTB versus hamstring); use allograft if available and patient amenable |
| Patellar graft or quadriceps tendon graft: bone cuts not beveled during harvest [8] | Patella fracture can occur after harvest | Trapezoidal cut can help to minimize a steep cut angle and prevent a stress riser at the harvest site | Examine the cut edge of the graft and the harvest site | Bevel the remaining cut edge of the patella; bone graft the donor site with plug trimmings if a large defect is present; protected weightbearing |
| Hamstring graft: tendons not adequately released [21] | Can lead to proximal transection of the tendon and inadequate length of the graft for reconstruction | The tendons should be released from the sartorial fascia and all gastrocnemius attachments should be transected; the stripper should be seated and constant pressure, in line with the harvested tendon, should be applied | The graft is examined after muscle removal and the length checked. Minimal length is typically 18 cm (9 cm when double looped); the surgeon can detect an impending inadequate release if she or he cannot deliver at least 3 cm of tendon through the skin wound with traction and knee flexion before stripping | Augment with allograft; harvest ipsilateral patellar tendon or contralateral hamstrings (if consented); abort procedure |
| Hamstring graft: excessive removal of muscle tissue [27] | Knee flexion weakness, particularly at high flexion angles. | Avoid plunging at time of harvest; avoid hamstring graft in athletes who require maximal power at high flexion angles (ie, hurdlers) | Excessive muscle tissue noted when graft is prepared for insertion | Physical therapy directed at hamstring strengthening |
| Saphenous nerve injury [25] | Injury to either the sartorial (terminal) or infrapatellar branch of the saphenous nerve during harvest or skin incision | Careful intraoperative technique, blunt retraction | Hyperesthesia and numbness on medial aspect of the knee | Observation, patient counseling, or desensitization therapy. |
BTB = bone-tendon-bone.
Table 3.
Complications related to graft sizing
| Complication | Clinical effect | Prevention | Detection | Remedy |
|---|---|---|---|---|
| Patellar tendon: graft tunnel length mismatch [3, 14] | When a BTB graft is too long, interference screw fixation cannot be used; when it is short, the fixation is not cortical | Careful measurement of bone plugs and tendon length after harvest; planning tunnels accordingly | The graft is seen protruding out of the tibial tunnel with the knee in extension | If long, recess the graft in the femoral tunnel to achieve more length on the femoral side; or shorten the bone plugs (if enough remains); if too short, consider supplementary fixation (staple, suture (with post), or nonaperture suspensory fixation (eg, EndoButtonTM; Smith and Nephew, Andover, MA, USA) |
| Patellar tendon: graft width mismatch [7] | Bone plugs that are too wide will not pass into the tunnels; plugs that are too small are susceptible to loose fixation; excess soft tissue may cause lack of motion and impingement | Measure the bone plugs before tunnel drilling | Detect before passage with sizers, otherwise it will be detected less optimally when passage is attempted | If too big, remove graft from knee and trim accordingly; soft tissue can be trimmed or the notch can be widened (notchplasty); if too small, alternative fixation method can be used in place of interference screw (staple, suture and post, EndoButtonTM), and the tunnel can be bone grafted |
BTB = bone-tendon-bone.
Table 4.
Complications related to graft placement and fixation
| Error | Clinical effect | Prevention | Detection | Remedy |
|---|---|---|---|---|
| Tibial tunnel placed too anterior [1, 11] | Loss of extension; higher tensile loads on graft in full extension could lead to failure |
Careful tibial guide placement using PCL and meniscus as references; intraoperative fluoroscopy to make sure that the tunnel is posterior to Blumensaat’s line in full extension | Intraoperative, graft impinges in the intercondylar notch in full extension (Fig. 2). Postoperative, lateral radiograph/MRI shows anterior tunnel placement; physical examination reveals limited knee extension | Consider expanding the tunnel and filling in the anterior aspect with graft and using supplemental fixation |
| Tibial tunnel placed too posterior [15, 16] | May result in a vertical tunnel with poor rotational stability of the graft; may result in PCL impingement and early failure | Careful tibial guide placement avoiding placement against the PCL; intraoperative fluoroscopy to make sure that the tunnel is not beyond the middle of the tibial plateau | Intraoperative, graft impinges against the PCL during range of motion. Postoperative, lateral radiograph/MRI shows posterior tunnel placement; physical examination may reveal laxity or a pivot shift | Consider expanding the tunnel and filling in the posterior aspect with graft and using supplemental fixation |
| Femoral tunnel placed too anterior [13] | Loss of knee flexion; graft impingement which can result in early failure | Ensure adequate observation of back wall with soft tissue notchplasty | Intraoperative observation shows graft is near or anterior to ‘resident’s ridge’; lateral knee radiograph or MRI can detect anterior placement | If detected early, consider dilating the tunnel and using nonaperture fixation (eg, EndoButtonTM [Smith and Nephew, Andover, MA, USA]); revision ACL reconstruction may be warranted to achieve normal knee motion |
| Femoral tunnel placed too posterior [19] | Blowout of the femoral tunnel which can compromise graft fixation if not recognized | Ensure adequate observation of the back wall and place graft in anatomic position; Over-the-top guides can help to prevent back wall compromise | Femoral tunnel has no posterior wall on inspection; interference screw does not achieve purchase | Revision tunnel drilling at least one diameter away, if possible, or use alternative femoral fixation and maintain tunnel |
| Femoral tunnel placed too vertical [4] | Poor rotational stability, leading to failure of the surgery | Medial tibial tunnel placement can allow for transtibial drilling lower on the condylar wall; anteromedial portal drilling allows for more anatomic graft placement | The graft or tunnel is noted to be in the 12 o’ clock position at 90o flexion; radiographs show vertical tunnel placement | Tibial guides that allow for lower placement for transtibial drilling are commercially available; anteromedial portal drilling can eliminate this hazard (Fig. 3) |
| Graft fixed in excessive knee flexion [18, 22] | Loss of knee extension and patellofemoral pain. | Fixing ACL grafts in terminal extension can eliminate excessive graft tension | Physical examination shows flexion contracture of the knee; MRI is used to exclude soft tissue impingement (ie, cyclops lesion) | Aggressive physical therapy focusing on active quadriceps extension. Extension casting or dynamic splinting; arthroscopic removal of cyclops lesion if present (without sacrificing graft) |
| Excessive notchplasty [2] | Pain secondary to detrimental effects on articular cartilage and patellofemoral dysfunction. | Consider limited or no notchplasty; consider accessory medial portal viewing to obviate the need for excessive notchplasty | Excessively wide notch; patella maltracking | Place graft in correct spot and hope fibrocartilage grows in. |
| Graft-screw divergence [9] | Divergence of screw by greater than 15o-30o from trajectory of tunnel may lead to failure of fixation and ACL failure | Insert screw and drill from same portal (no divergence at all); hyperflex the knee when inserting the screw if the femoral tunnel was drilled through the tibial tunnel; use guide wire to help gauge mismatch | Postoperative radiograph can detect divergence. Suspicion should be raised if there is difficulty inserting the screw | Readjust screw if noticed intraoperatively; consider supplemental fixation with suture and post; modify postoperative protocol |
PCL = posterior cruciate ligament; ACL = anterior cruciate ligament.
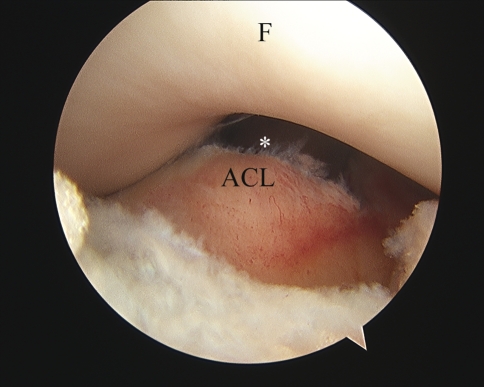
Fig. 2.
An arthroscopic view shows the intercondylar notch during an ACL reconstruction with the knee positioned in full extension. An intercondylar notch is evident after a tunnel dilator (unseen) is placed in the tibial tunnel. Because the dilator is in the position of the ACL graft, a frontal view such as this one can be used to determine if the tunnel is well placed. Positioned correctly, the dilator (and therefore the graft) is not seen when the knee is in full extension. In this view, only the tibia and femur are seen with the knee in full extension; the tunnel dilator (position marked by *) is obscured by the distal femur, indicating proper tibial tunnel placement and absence of graft impingement. (F = femoral trochlea; ACL = ACL stump).
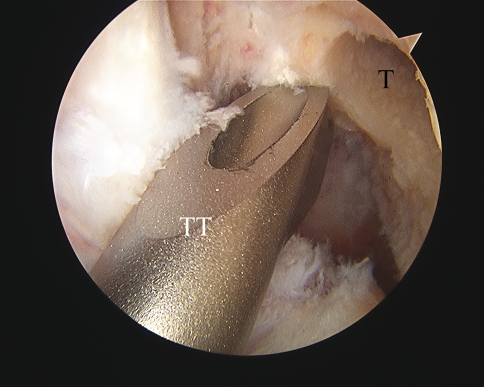
Fig. 3.
An arthroscopic view shows the intercondylar notch during a left ACL reconstruction with the knee positioned in flexion. The arthroscope is in the anterolateral portal. The femoral tunnel in this left knee was drilled via a medial portal and is in the correct 2 o’clock position. By contrast, the point selected by a transtibial guide would orient the graft too vertically. (T = femoral tunnel; TT = transtibial guide).
Table 5.
Postoperative complications
| Postoperative course | Clinical effect | Prevention | Detection | Remedy |
|---|---|---|---|---|
| Infection [17, 29] | Pain, swelling, stiffness that could necessitate removal of the graft | In addition to the usual, with knee arthroscopy, be mindful of the foot going on and off the table; use waterproof drapes to prevent convection of contaminants; use trusted donor sources when allograft is used | Knee aspiration and cultures | Aggressive treatment with lavage, débridement, and intravenous antibiotic therapy; do not remove the graft and fixation on the basis of cell count (use cultures for that) |
| Stiffness [22] | Lack of full ROM in either flexion or extension (or both) | Proper placement of tibial and femoral tunnels; tensioning of the graft at or near terminal extension to prevent over-constraining the knee | Identified at the postoperative appointment by lack of terminal extension (within 2 weeks, typically) or flexion (typically by 6 weeks) | Aggressive postoperative rehabilitation; drop-out casting or arthroscopic lysis of adhesions for refractory cases; manipulation under anesthesia may help restore lost flexion |
| Patella fracture | Pain, articular cartilage injury, further disability that may require surgery | Use of allograft or hamstring autograft for ACL reconstruction; limiting postoperative contact or collision sports for an extended time; proper harvest technique | Typically as a result of impact on a bent knee; radiographs reveal the diagnosis | Protected weightbearing; surgery if the fracture is displaced |
Footnotes
Each author certifies that he or she, or a member of their immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
An erratum to this article can be found at http://dx.doi.org/10.1007/s11999-012-2270-2.
References
- 1.Allum R. Complications of arthroscopic reconstruction of the anterior cruciate ligament. J Bone Joint Surg Br. 2003;85:12–16. doi: 10.1302/0301-620X.85B1.13956. [DOI] [PubMed] [Google Scholar]
- 2.Asahina S, Muneta T, Ezura Y. Notchplasty in anterior cruciate ligament reconstruction: an experimental animal study. Arthroscopy. 2000;16:165–172. doi: 10.1016/S0749-8063(00)90031-8. [DOI] [PubMed] [Google Scholar]
- 3.Barber FA. Flipped patellar tendon autograft anterior cruciate ligament reconstruction. Arthroscopy. 2000;16:483–490. doi: 10.1053/jars.2000.4384. [DOI] [PubMed] [Google Scholar]
- 4.Bedi A, Raphael B, Maderazo A, Pavlov H, Williams RJ., 3rd Transtibial versus anteromedial portal drilling for anterior cruciate ligament reconstruction: a cadaveric study of femoral tunnel length and obliquity. Arthroscopy. 2010;26:342–350. doi: 10.1016/j.arthro.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Burd T, Conroy BP, Meyer SC, Allen WC. The effects of chlorhexidine irrigation solution on contaminated bone-tendon allografts. Am J Sports Med. 2000;28:241–244. doi: 10.1177/03635465000280021601. [DOI] [PubMed] [Google Scholar]
- 6.Church S, Keating JF. Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. J Bone Joint Surg Br. 2005;87:1639–1642. doi: 10.1302/0301-620X.87B12.16916. [DOI] [PubMed] [Google Scholar]
- 7.Dargel J, Schmidt-Weithoff R, Bruggemann GP, Koebke J. The effect of bone tunnel dilation versus extraction drilling on the initial fixation strength of press-fit anterior cruciate ligament reconstruction. Arch Orthop Trauma Surg. 2007;127:801–807. doi: 10.1007/s00402-006-0206-6. [DOI] [PubMed] [Google Scholar]
- 8.DuMontier TA, Metcalf MH, Simonian PT, Larson RV. Patella fracture after anterior cruciate ligament reconstruction with the patellar tendon: a comparison between different shaped bone block excisions. Am J Knee Surg. 2001;14:9–15. [PubMed] [Google Scholar]
- 9.Fineberg MS, Zarins B, Sherman OH. Practical considerations in anterior cruciate ligament replacement surgery. Arthroscopy. 2000;16:715–724. doi: 10.1053/jars.2000.8951. [DOI] [PubMed] [Google Scholar]
- 10.Gillquist J, Hagberg G, Oretorp N. Arthroscopic examination of the posteromedial compartment of the knee joint. Int Orthop. 1979;3:13–18. doi: 10.1007/BF00266321. [DOI] [PubMed] [Google Scholar]
- 11.Goble EM, Downey DJ, Wilcox TR. Positioning of the tibial tunnel for anterior cruciate ligament reconstruction. Arthroscopy. 1995;11:688–695. doi: 10.1016/0749-8063(95)90111-6. [DOI] [PubMed] [Google Scholar]
- 12.Gold DL, Schaner PJ, Sapega AA. The posteromedial portal in knee arthroscopy: an analysis of diagnostic and surgical utility. Arthroscopy. 1995;11:139–145. doi: 10.1016/0749-8063(95)90058-6. [DOI] [PubMed] [Google Scholar]
- 13.Hame SL, Markolf KL, Hunter DM, Oakes DA, Zoric B. Effects of notchplasty and femoral tunnel position on excursion patterns of an anterior cruciate ligament graft. Arthroscopy. 2003;19:340–345. doi: 10.1053/jars.2003.50040. [DOI] [PubMed] [Google Scholar]
- 14.Herz A, Tjoumakaris F. A novel solution for graft tunnel-mismatch in ACL reconstruction. Tech Knee Surg. 2009;8:242–245. doi: 10.1097/BTK.0b013e3181b57f87. [DOI] [Google Scholar]
- 15.Howell SM. Principles for placing the tibial tunnel and avoiding roof impingement during reconstruction of a torn anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 1998;6(suppl 1):S49–S55. doi: 10.1007/s001670050223. [DOI] [PubMed] [Google Scholar]
- 16.Howell SM, Clark JA. Tibial tunnel placement in anterior cruciate ligament reconstructions and graft impingement. Clin Orthop Relat Res. 1992;283:187–195. [PubMed] [Google Scholar]
- 17.Judd D, Bottoni C, Kim D, Burke M, Hooker S. Infections following arthroscopic anterior cruciate ligament reconstruction. Arthroscopy. 2006;22:375–384. doi: 10.1016/j.arthro.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Logerstedt D, Sennett BJ. Case series utilizing drop-out casting for the treatment of knee joint extension motion loss following anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 2007;37:404–411. doi: 10.2519/jospt.2007.2466. [DOI] [PubMed] [Google Scholar]
- 19.Markolf KL, Hame S, Hunter DM, Oakes DA, Zoric B, Gause P, Finerman GA. Effects of femoral tunnel placement on knee laxity and forces in an anterior cruciate ligament graft. J Orthop Res. 2002;20:1016–1024. doi: 10.1016/S0736-0266(02)00035-9. [DOI] [PubMed] [Google Scholar]
- 20.Mohtadi NG, Webster-Bogaert S, Fowler PJ. Limitation of motion following anterior cruciate ligament reconstruction: a case control study. Am J Sports Med. 1991;19:620–624; discussion 624–625. [DOI] [PubMed]
- 21.Pagnani MJ, Warner JJ, O’Brien SJ, Warren RF. Anatomic considerations in harvesting the semitendinosus and gracilis tendons and a technique of harvest. Am J Sports Med. 1993;21:565–571. doi: 10.1177/036354659302100414. [DOI] [PubMed] [Google Scholar]
- 22.Petsche TS, Hutchinson MR. Loss of extension after reconstruction of the anterior cruciate ligament. J Am Acad Orthop Surg. 1999;7:119–127. doi: 10.5435/00124635-199903000-00005. [DOI] [PubMed] [Google Scholar]
- 23.Ricchetti ET, Sennett BJ, Huffman GR. Acute and chronic management of posterolateral corner injuries of the knee. Orthopedics. 2008;31:479–488. doi: 10.3928/01477447-20110414-05. [DOI] [PubMed] [Google Scholar]
- 24.Sampson MJ, Jackson MP, Moran CJ, Shine S, Moran R, Eustace SJ. Three Tesla MRI for the diagnosis of meniscal and anterior cruciate ligament pathology: a comparison to arthroscopic findings. Clin Radiol. 2008;63:1106–1111. doi: 10.1016/j.crad.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 25.Sanders B, Rolf R, McClelland W, Xerogeanes J. Prevalence of saphenous nerve injury after autogenous hamstring harvest: an anatomic and clinical study of sartorial branch injury. Arthroscopy. 2007;23:956–963. doi: 10.1016/j.arthro.2007.03.099. [DOI] [PubMed] [Google Scholar]
- 26.Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction: the effect of timing of reconstruction and rehabilitation. Am J Sports Med. 1991;19:332–336. doi: 10.1177/036354659101900402. [DOI] [PubMed] [Google Scholar]
- 27.Tashiro T, Kurosawa H, Kawakami A, Hikita A, Fukui N. Influence of medial hamstring tendon harvest on knee flexor strength after anterior cruciate ligament reconstruction: a detailed evaluation with comparison of single- and double-tendon harvest. Am J Sports Med. 2003;31:522–529. doi: 10.1177/31.4.522. [DOI] [PubMed] [Google Scholar]
- 28.Tayton E, Verma R, Higgins B, Gosal H. A correlation of time with meniscal tears in anterior cruciate ligament deficiency: stratifying the risk of surgical delay. Knee Surg Sports Traumatol Arthrosc. 2009;17:30–34. doi: 10.1007/s00167-008-0622-y. [DOI] [PubMed] [Google Scholar]
- 29.Wang C, Ao Y, Wang J, Hu Y, Cui G, Yu J. Septic arthritis after arthroscopic anterior cruciate ligament reconstruction: a retrospective analysis of incidence, presentation, treatment, and cause. Arthroscopy. 2009;25:243–249. doi: 10.1016/j.arthro.2008.10.002. [DOI] [PubMed] [Google Scholar]
- 30.Zaffagnini S, Bignozzi S, Martelli S, Lopomo N, Marcacci M. Does ACL reconstruction restore knee stability in combined lesions? An in vivo study. Clin Orthop Relat Res. 2007;454:95–99. doi: 10.1097/BLO.0b013e31802b4a86. [DOI] [PubMed] [Google Scholar]