Abstract
Background
Initial reports with short-term followup of porous tantalum acetabular components and augments for Paprosky IIIA acetabular defects demonstrate high hip scores, low rates of aseptic loosening, and low rates of complications. However, longer-term followup with a larger cohort is needed to determine the durability of these reconstructions.
Questions/purposes
We therefore determined the functional scores, rates of aseptic loosening, and complications in patients with Paprosky IIIA acetabular defects treated with porous tantalum acetabular components and augments.
Methods
We retrospectively reviewed 37 acetabular revisions in 36 patients (one patient with bilateral revisions) treated with a porous tantalum acetabular component and augment. All patients had defects classified as Type IIIa using the system of Paprosky et al. Harris hip scores were obtained and radiographic examination was performed before surgery and through most recent followup. The minimum followup was 26 months (mean, 60 months; range, 26–106 months).
Results
One patient developed aseptic loosening of the acetabular reconstruction requiring revision; seven other patients required further surgery for periprosthetic femoral fracture (two), acute infection (three), and recurrent dislocation (two). Thirty-five of 37 hips had no or occasional pain at final followup. Mean Harris hip scores improved from 33.0 preoperatively (range, 12.6–58.7) to 81.5 postoperatively (range, 27.0–99.8).
Conclusions
Although the complication rate requiring further surgery was considerable, most patients with these reconstructions had pain relief and reasonable function with low rates of loosening at midterm followup.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Implant loosening with moderate to severe bone loss almost always results in disability for patients and is challenging for arthroplasty surgeons to reconstruct. The senior author (WGP) previously described a classification system and systematic approach for addressing acetabular bone loss in revision THA [1, 13]. A Type III defect is defined by an acetabular rim that is unable to provide adequate initial stability for a standard cementless hemispheric component. Type III defects are further subdivided into IIIa and IIIb. A Type IIIa defect is defined by an “up and out” presentation with superior and lateral migration of the femoral head greater than 3 cm. Cementless acetabular fixation is possible in Type IIIa defects but often requires use of a structural buttress to provide initial stability [13]. Occasionally, if the defect is spherical and if there is adequate column bone stock, sequential reaming can be performed and a jumbo cup can be used [3]. However, using a jumbo cup in Type IIIa defects often results in greater bone loss along the anterior column because the AP dimension is reamed to accommodate the enlarged cephalad-caudal dimension. In these situations, a superior buttress can be placed to bring down the hip to its anatomic center and allow for placement of a smaller hemispheric acetabular component in the appropriate hip center. Structural allografts may also be used to fill the defect and buttress the acetabular component [6, 10, 14, 15]. Although some authors have reported survival rates as high as 86% at average 7-year followup [10], we have previously reported a failure rate resulting from aseptic loosening of 25% using distal femoral allograft with five of 23 patients requiring revision for aseptic loosening at an average 5.3 years from the index surgery [14]. As an alternative, we have reported the use of porous tantalum acetabular components and augments for Type IIIa acetabular defects [18]. The modular nature of the augments allows for a customized acetabular construct to maximize host bone contact and stability. With a high porosity (70%–80%) and a low modulus of elasticity, the acetabular component and augment have propensity for bony ingrowth and biologic fixation (Fig. 1) [4, 9, 11, 12, 16–18, 20, 21]. At a minimum 1-year followup (average, 3 years; range, 1–4 years), we observed no clinical or radiographic evidence of aseptic acetabular component loosening [18]. Only one of 28 hips required further revision surgery (revision to a constrained liner for recurrent instability). Twenty-five patients had none or just slight pain with modified Merle D’Aubigné and Postel hip scores increasing from 6.8 to 10.6 (range, 8–12). Other authors have also reported acceptable postoperative hip scores, low rates of aseptic loosening, and low rates of other complications requiring further surgery using porous tantalum acetabular components and augments at mean followup ranging from 34 to 41 months [9, 20, 21].
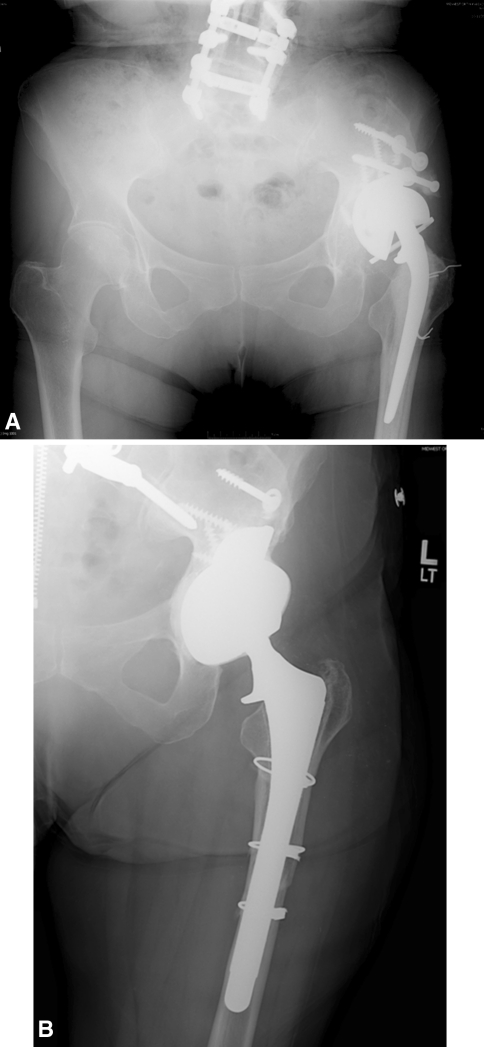
Fig. 1A–B.
(A) Preoperative and (B) 63-month postoperative radiographs of a 73-year-old woman with reconstruction of a Paprosky IIIA defect after failed shelf allograft. The patient is currently pain-free and ambulating without the use of an assistive device.
Given the relatively small size and short followup of these initial studies, further study is required to determine (1) maintained improvement in pain and function; (2) longer-term rates of aseptic loosening; and (3) the presence of additional postoperative complications requiring further surgery.
Patients and Methods
We retrospectively reviewed the charts and radiographs of 43 patients who underwent acetabular revision for a Type IIIA acetabular defect with a porous tantalum acetabular shell and augment from January 1, 2002, to January 1, 2009. All surgeries were performed by the two senior authors (SMS, WGP) at Central Dupage Hospital (Winfield, IL, USA) or the Rush University Medical Center (Chicago, IL, USA). We identified patients from an operating room database retrieval system using the standard current procedural terminology codes for revision THA. Forty-three hips (42 patients) underwent acetabular revision with porous tantalum acetabular components and modular augments for Type IIIA acetabular defects during the aforementioned time period. This approach was indicated for (1) acetabular defects with severe superior and lateral bone loss; (2) compromising stability of a standard hemispherical component; and where (3) preparation of a large or jumbo cup would result in excessive bone loss from the anterior column and loss of stability. A relative contraindication of this approach during the study period was very young (< 35 years old) age in which multiple future revision surgeries are anticipated. In these patients, to preserve and possibly restore acetabular bone, a distal femoral allograft reconstruction was considered. Four patients died from diseases unrelated to THA before the minimum 2-year followup. Three patients were lost to followup. This left 36 patients with 37 hip revisions. The mean age at the time of surgery was 60 years (range, 36–80 years). The reason(s) for revision were aseptic loosening of the acetabular component (31), second-stage reconstruction after infection (five), and revision of a failed chronically dislocated hemiresurfacing arthroplasty (one). Four patients had pelvic discontinuity that was treated with distraction as previously described by the senior authors (WGP, SMS). Minimum followup of the cohort was 26 months (mean, 60 months; range, 26–106 months). We had prior Institutional Review Board approval.
We used a posterior approach to the hip in all cases and antibiotics were withheld until definitive cultures were obtained. On removal of fibrous tissue and complete exposure of the acetabular defect, we sequentially used hemispheric reamers at the native hip center until both the anterior and posterior columns were engaged. With a trial acetabular component in place, trial augments were positioned, usually in the posterior superior quadrant as is typically required for Type IIIa defects. We then contoured the bone and/or the tantalum augment with a reamer and/or barrel burr to optimize the surface contact area. With a trial acetabular component in place, the tantalum augment was secured to the bone with multiple 6.5-mm screws. We then packed the augment with morselized fresh-frozen cancellous allograft mixed with viable autograft reamings if available. The portion of the augment to contact the acetabular component was coated with polymethylmethacrylate (PMMA). The acetabular component (either a modular or revision porous tantalum metal shell) was then firmly impacted against the native bone and the PMMA-covered portion of the augment. The revision porous tantalum shell offers the theoretical advantages over the modular component of a lower modulus of elasticity, increased ability to obtain screw fixation by drilling directly through the tantalum shell, and locked screws with greater pull out strength through cementation of the screw holes. The revision acetabular shell was used in 15 reconstructions when the surgeon believed the bone quality was particularly poor, additional screw fixation was required, and in all of the patients with pelvic discontinuity. We placed multiple screws (a minimum of two but as many as five depending on the quality of bone and availability of fixation) through the acetabular component into host bone. The largest femoral head possible for the size of the acetabular component was used to minimize the risk of instability (usually 36 or 40 mm). Even in the setting of abductor deficiency, in which the benefits of a larger femoral head are not as appreciated, we avoided placing constrained liners to minimize stress at the host bone-component interface before ingrowth [2, 8].
Postoperatively, we placed all patients in an abduction brace and followed posterior THA precautions with touch-down weightbearing for 12 weeks before being advanced to weightbearing as tolerated without a brace. Patients were mobilized on postoperative Day 1. Physiotherapy was directed to concentrate on simple ambulation, activities of daily living, and maintaining posterior hip precautions for the first 12 weeks. At 12 weeks, the therapists began weaning the patient from assisted ambulatory devices and initiated more aggressive strengthening of core musculature, hip abductors, and hip flexors. All patients were counseled preoperatively that they may always have some limp and require a cane for balance. At 6 months postoperatively, patients were cleared to return to most activities with recommendations to avoid repetitive impact (jumping), heavy lifting, and deep/exaggerated hip positions.
Routine followup consisted of clinic visits at 2, 6, and 12 weeks followed by 3, 6, 12 months, and then annual afterward. An AP pelvis, AP hip, and Lowenstein lateral hip radiographs were obtained at every followup visit. Our radiology technicians are well trained and experienced at standardizing hip and pelvic radiographs. All films are printed to true size and then evaluated by the technician and the treating surgeon. The printed radiographs are superimposed with prior films to evaluate for gross deviation in sizing and rotation. Evaluation of the appearance of radiographic landmarks such as the obturator foramen or measurements such as the distance of the pubic symphysis to the coccyx allow for estimation and consistency of pelvic rotation in multiple planes. Measurement of the known size of the prosthetic femoral head confirms appropriate and consistent sizing of the radiographs. Beginning at the 6 months postoperatively, Harris hip scores (HHS) are obtained through the history and physical examination performed by the treating surgeon.
Radiographs were reviewed and the results documented by the treating surgeon (WGP, SMS) at each clinic visit in the medical records. For the purpose of this study an additional investigator (DJD) also reviewed the immediate postoperative and the most recent available radiographs for each patient. Loosening was defined radiographically as a change in the component abduction angle of greater than 10° or a change in the horizontal or vertical position of greater than 6 mm after correcting for magnification. These parameters are based on previously published studies from our and other institutions and allow for some variance in xray rotation and magnification to minimize a false-positive diagnosis of aseptic loosening [4, 9, 11, 14, 18]. There was no interobserver variability in the radiographic diagnosis of aseptic loosening of the acetabular components.
Results
The majority, 35 of 37 hips, have none or occasional slight pain. A patient with severe juvenile rheumatoid arthritis and spine degeneration had severe lower extremity radicular pain likely unrelated to her hip reconstruction. The mean HHS increased from preoperative 33.0 (range, 12.6–58.7) to postoperative 81.5 (range, 27.0–99.8). Twenty-eight hips had a HHS greater than 80, five had a score from 70–80, and four had a score less than 70. All but one of the poor results had multiple medical comorbidities unrelated to their hip markedly limiting their ambulatory capacity.
Of the 37 acetabular reconstructions (including four patients with pelvic discontinuity; Fig 2), one reconstruction had radiographic evidence of loosening. The patient, a 54-year-old woman with a history of multiple epiphyseal dysplasia and three prior acetabular revisions (two for aseptic loosening and one for malpositioned components/recurrent dislocations) is currently 97 months from the most recent acetabular revision performed for aseptic loosening. At approximately 72 months postoperatively, she had slight occasional pain and used a cane only for long walks. She had approximately 1 year of increasingly severe groin and thigh pain and now has evidence of greater than 6-mm component migration on radiographic examination. She is currently waiting to undergo revision to a custom triflange component at another institution.
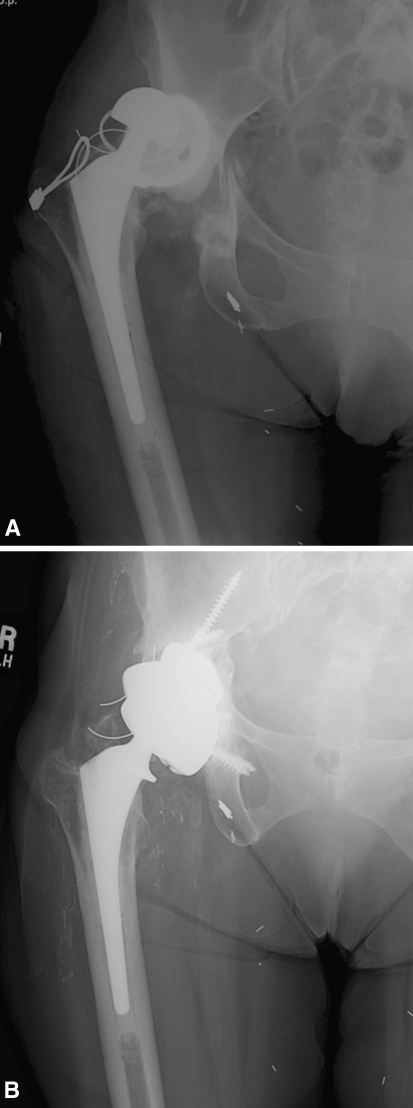
Fig. 2A–B.
(A) Preoperative and (B) 105-month postoperative radiograph of a 69-year-old woman who underwent reconstruction of a Paprosky IIIA defect with discontinuity after failed revision THA. The patient is currently pain-free with a Harris hip score of 91.
Seven of the 36 patients (19%) required at least one additional surgery. One patient underwent open reduction internal fixation of a periprosthetic femur fracture. He developed recurrent instability, which was treated with a constrained liner. He then had failure of the constrained liner that was treated with complete revision of all components at an outside institution. He had further instability and recently underwent revision with another constrained liner also performed at an outside institution (current HHS 66 at 106-month followup). One patient underwent revision of her femoral component after a periprosthetic fracture. She subsequently developed recurrent instability and underwent placement of a constrained liner (current HHS 90 at 45-month followup). Two additional patients had recurrent instability. Both of these patients underwent revision surgery for placement of constrained liners. One of these patients did well without further complications (HHS 80 at 44-month followup). The other patient developed an infection after placement of the constrained liner that was treated with irrigation and débridement and chronic antibiotic suppression therapy (HHS 85 at 94-month followup). Finally, three patients required irrigation and débridement with 6 weeks of intravenous antibiotics in the early postoperative period for what was believed to be acute infections. All three patients are currently off antibiotics and without evidence of recurrent infection. One of the three patients had two dislocations, which were treated nonoperatively with closed reductions (HHS 95 at 43-month followup, 86 at 79-month followup, and 70 at 39-month followup).
Discussion
Paprosky Type IIIA acetabular defects present a unique reconstructive challenge. Severe bone loss makes acceptable stability with a standard hemispherical acetabular component alone unobtainable. A variety of techniques have been used to address this problem. These include the use of bulk structural allograft and reconstruction cages, shelf/buttress allograft, and more recently porous tantalum augments [4, 6, 9–11, 14, 15, 18, 20–22]. The porous tantalum augments offer theoretical advantages of ease of use, modularity, and lack of resorption. Initial studies with small enrollment and short followup demonstrated encouraging results. With this study we sought to determine pain relief and function, rate of radiographic evidence of aseptic loosening, and incidence of complications requiring further surgery at midterm followup.
We acknowledge limitations of our study. First is the retrospective design. Ideally a randomized controlled trial would be performed comparing this type of reconstruction with other techniques such as a distal femoral allograft buttress. Given the established relatively high rates of failure resulting from aseptic loosening with distal femoral allograft and low rates of loosening with porous tantalum augments, we do not believe this study would be ethical [11, 14]. Second, the radiographic analysis was not blinded and we used parameters to define loosening that have not been radiographically validated and that may have some degree of inconsistent rotation and/or magnification. There are no well accepted three-dimensional criteria to radiographically diagnose aseptic loosening or a fibrous stable fixation in complex revision constructions with severe bone loss. Clearly, there will be radiolucent lines present where the construct does not contact host bone. Imaging and interpreting radiolucent lines in this setting are difficult. Further, we used the following criteria for migration: abduction angle of greater than 10° or a change in the horizontal or vertical position of greater than 6 mm, criteria that reflect substantial amounts of migration. It is possible that one or more of the acetabular constructs were fibrous stable but did not migrate beyond these criteria. However, we presume the clinical importance would be limited given 35 of 37 hips had minimal if any pain and we would not advise rerevision if a hip were minimally painful and the reconstruction stable even if multiple radiolucent lines were present. The parameters for radiographic evidence of loosening chosen for this study have been published in prior studies performed at our institution and others [4, 9, 11, 14, 18]. Roentgen stereophotogrammetric analysis (RSA) allows accurate measurement of small (0.25 mm) amounts of implant migration corresponding to aseptic loosening [5]. Unfortunately, during this study we did not have RSA capabilities. We have subsequently started using RSA for implant migration and acknowledge that RSA of this cohort would more effectively measure implant migration than a plain radiograph protocol. Third, the physical examination portion of the HHS was performed by unblinded investigators. Although this may have introduced bias, the majority of the data points obtained for the HHS were derived from questions on a form filled out by the patient without coaching from an investigator.
The clinical status of our patients based on function and pain measured by the HHS are encouraging given the complex nature of the surgeries and the multiple comorbidities of many of the patients. We believe a direct comparison these hip scores to those of other studies evaluating complex acetabular reconstruction is of limited use given potential confounding variables. Nonetheless, the hip scores of this study stand alone in demonstrating a HSS above 80 in 33 of the 37 patients at mid-term followup.
At a mean 60-month followup, only one of 37 hips (2.7%) failed as a result of aseptic loosening. These results compare favorably with those from studies using alternative techniques and to those with shorter-term studies reporting porous acetabular components and augments (Table 1). Garbuz et al. reviewed the results of 33 acetabular reconstructions with severe bone loss treated with bulk allograft and cage reconstruction [6]. There was a 44% failure rate resulting from aseptic loosening at a mean 85-month followup. A study performed at our institution as well as another performed by Woodgate et al. demonstrated a 22% incidence of aseptic loosening with the use of a superior lateral buttress allograft [15, 22]. The benefits of porous tantalum augments compared with structural allograft have been well described and include relative ease of insertion, minimized soft tissue stripping, and inability to resorb [4, 11, 15, 18]. Given the encouraging results presented in this study, we recommend using structural allograft for Type IIIa defects only in the “very young” patient in whom multiple subsequent acetabular revisions are anticipated and restoration and conservation of bone stock is a priority. Although aseptic loosening was rare in this series, potential areas of failure in the long term include failure at the augment/cement/acetabular component interface and fatigue failure of the tantalum components themselves. Further study and continued monitoring are needed to determine the long-term results of the use of porous tantalum acetabular components and augments for complex acetabular reconstruction.
Table 1.
Comparisons of studies reporting reconstructions for severe acetabular bone loss
| Author | Number and severity of acetabular reconstructions | Reconstruction technique for IIIA defects | Mean followup | Mean postoperative hip score | Failure resulting from aseptic loosening | Other complications requiring reoperation |
|---|---|---|---|---|---|---|
| Garbuz et al. [6] | 33 hips with “major” (> 50% of cup support by graft) bone loss | Cage and structural allograft | 85 months (range, 60–132) | Not specified; 55% of patients obtained 20 points or greater increase in Harris hip score | 14 (42%) 8 graft failures and 6 loose cups | Sciatic nerve palsy requiring exploration (1) |
| Woodgate et al. [22] | 51 hips requiring superior/lateral allograft buttress (all with > 50% cup/host bone contact) | Porous coated acetabular component with allograft buttress | 119 months (range, 68–195) | Not specified | 11 (22%) | Not specified |
| Sporer et al. [14] | 23 IIIA | Porous-coated acetabular component with distal femoral allograft buttress | 10.3 years | Modified Merle D’Aubigne and Postel 10 | 5 (22%) | Not specified |
| Weeden and Schmidt [21] | 43 acetabular reconstructions; 33 IIIA and 10 IIIB | Porous tantalum cup in all cases, 13/33 IIIA with porous tantalum augments | 34 months (range, 24–48) | Harris hip score 84 (range, 28–100) | 0 | Infection requiring component resection (1) |
| Flecher et al. [4] | 23 acetabular reconstructions; 17 IIIA and 6 IIIB | Porous tantalum cup in all cases, 11/17 IIIA with porous tantalum augments | 35 months (range, 24–50) | Modified Merle D’Aubigne and Postel 10.6 (range, 8–12) | 0 | Recurrent instability (1) |
| Lingaraj et al. [9] | 23 acetabular reconstructions; 17 IIIA and 6 IIIB | Porous tantalum cup and augments in all cases | 41 months (range, 24–62) | Harris hip score 75.7 (range, 53–00) | 0 | Recurrent instability (2), Infection requiring irrigation and débridement (1) |
| Van Kleunen et al. [20] | 97 acetabular reconstructions; 24 IIA, 19 IIB, 19 IIC, 19 IIIA, and 16 IIIB | Porous tantalum cup in all cases and 23 cases (not specified) with augments | 45 months (range, 24–79) | Harris hip score 76 (range, 25–100) | 0 | Infection component removal (8), recurrent instability (2), hematoma (4), liner failure (3) |
| Current study | 37 IIIA acetabular reconstructions | Porous tantalum cup and augments in all cases | 60 months (range, 26–106) | Harris hip score 81.5 (range, 27.0–99.8) | 1 (2.7%) | Recurrent instability (5), infection requiring irrigation and débridement (4), periprosthetic femoral fracture (2) |
We observed a relatively high complication rate requiring further surgery. With seven patients having undergone at least one additional procedure and one patient with aseptic loosening awaiting complete acetabular revision, the overall complication rate requiring further surgery was 21.6%. Although there were more complications in our study compared with previously published reports of short-term followup of porous tantalum acetabular components and augments, the incidence of complication is consistent with other series of longer-term followup after complex revision THA [7, 9, 11, 18, 19, 21]. Further work is required to address issues of infection, periprosthetic fracture, and instability after revision THA.
Footnotes
One of the authors (SMS) receives institutional research support from Zimmer (Warsaw, IN, USA) and is a paid consultant for and receives payment for development of educational programs for Smith and Nephew (Memphis, TN, USA). One of the authors (WGP) receives institutional research support, is a paid consultant, a paid lecturer/instructor/developer of educational presentations, receives royalty payments from Zimmer, and is a paid consultant and a paid lecturer/instructor/developer of educational presentations for Biomet (Warsaw, IN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
The authors certify that their institutions approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent was obtained.
This work was performed at Rush University Medical Center, Chicago IL, and Central Dupage Hospital, Winfield, IL, USA.
Contributor Information
Daniel J. Del Gaizo, Email: ddelgaizo@gmail.com.
Scott M. Sporer, Email: scottsporer@gmail.com.
References
- 1.Bradford MS, Paprosky WG. Acetabular defect classification: a detailed radiographic approach. Semin Arthroplasty. 1995;2:76–85. [PubMed] [Google Scholar]
- 2.Della Valle CJ, Chang D, Sporer S, Berger RA, Rosenberg AG, Paprosky WG. High failure rate of a constrained acetabular liner in revision total hip arthroplasty. J Arthroplasty. 2005;7(Suppl 3):103–107. doi: 10.1016/j.arth.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Emerson RH, Jr, Head WC. Dealing with the deficient acetabulum in revision hip arthroplasty: the importance of implant migration and use of the jumbo cup. Semin Arthroplasty. 1993;1:2–8. [PubMed] [Google Scholar]
- 4.Flecher X, Sporer S, Paprosky W. Management of severe bone loss in acetabular revision using a trabecular metal shell. J Arthroplasty. 2008;7:949–955. doi: 10.1016/j.arth.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 5.Franzen H, Mjoberg B, Onnerfalt R. Early migration of acetabular components revised with cement. A roentgen stereophotogrammetric study. Clin Orthop Relat Res. 1993;287:131–134. [PubMed] [Google Scholar]
- 6.Garbuz D, Morsi E, Gross AE. Revision of the acetabular component of a total hip arthroplasty with a massive structural allograft. Study with a minimum five-year follow-up. J Bone Joint Surg Am. 1996;5:693–697. doi: 10.2106/00004623-199605000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Jafari SM, Coyle C, Mortazavi SM, Sharkey PF, Parvizi J. Revision hip arthroplasty: Infection is the most common cause of failure. Clin Orthop Relat Res. 2010;8:2046–2051. doi: 10.1007/s11999-010-1251-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kung PL, Ries MD. Effect of femoral head size and abductors on dislocation after revision THA. Clin Orthop Relat Res. 2007;465:170–174. doi: 10.1097/BLO.0b013e318159a983. [DOI] [PubMed] [Google Scholar]
- 9.Lingaraj K, Teo YH, Bergman N. The management of severe acetabular bone defects in revision hip arthroplasty using modular porous metal components. J Bone Joint Surg Br. 2009;12:1555–1560. doi: 10.1302/0301-620X.91B12.22517. [DOI] [PubMed] [Google Scholar]
- 10.Morsi E, Garbuz D, Gross AE. Revision total hip arthroplasty with shelf bulk allografts. A long-term follow-up study. J Arthroplasty. 1996;1:86–90. doi: 10.1016/S0883-5403(96)80165-3. [DOI] [PubMed] [Google Scholar]
- 11.Nehme A, Lewallen DG, Hanssen AD. Modular porous metal augments for treatment of severe acetabular bone loss during revision hip arthroplasty. Clin Orthop Relat Res. 2004;429:201–208. doi: 10.1097/01.blo.0000150133.88271.80. [DOI] [PubMed] [Google Scholar]
- 12.Paprosky WG, O’Rourke M, Sporer SM. The treatment of acetabular bone defects with an associated pelvic discontinuity. Clin Orthop Relat Res. 2005;441:216–220. doi: 10.1097/01.blo.0000194311.20901.f9. [DOI] [PubMed] [Google Scholar]
- 13.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;1:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 14.Sporer SM, O’Rourke M, Chong P, Paprosky WG. The use of structural distal femoral allografts for acetabular reconstruction. Average ten-year follow-up . J Bone Joint Surg Am. 2005;4:760–765. doi: 10.2106/JBJS.D.02099. [DOI] [PubMed] [Google Scholar]
- 15.Sporer SM, O’Rourke M, Chong P, Paprosky WG. The use of structural distal femoral allografts for acetabular reconstruction. Surgical technique. J Bone Joint Surg Am. 2006;8(Suppl 1):92–99. doi: 10.2106/JBJS.E.00903. [DOI] [PubMed] [Google Scholar]
- 16.Sporer SM, O’Rourke M, Paprosky WG. The treatment of pelvic discontinuity during acetabular revision. J Arthroplasty. 2005;4(Suppl 2):79–84. doi: 10.1016/j.arth.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 17.Sporer SM, Paprosky WG. Acetabular revision using a trabecular metal acetabular component for severe acetabular bone loss associated with a pelvic discontinuity. J Arthroplasty. 2006;6(Suppl 2):87–90. doi: 10.1016/j.arth.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 18.Sporer SM, Paprosky WG. The use of a trabecular metal acetabular component and trabecular metal augment for severe acetabular defects. J Arthroplasty. 2006;6(Suppl 2):83–86. doi: 10.1016/j.arth.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Springer BD, Fehring TK, Griffin WL, Odum SM, Masonis JL. Why revision total hip arthroplasty fails. Clin Orthop Relat Res. 2009;1:166–173. doi: 10.1007/s11999-008-0566-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kleunen JP, Lee GC, Lementowski PW, Nelson CL, Garino JP. Acetabular revisions using trabecular metal cups and augments. J Arthroplasty. 2009;6(Suppl):64–68. doi: 10.1016/j.arth.2009.02.001. [DOI] [PubMed] [Google Scholar]
- 21.Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;6(Suppl 2):151–155. doi: 10.1016/j.arth.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 22.Woodgate IG, Saleh KJ, Jaroszynski G, Agnidis Z, Woodgate MM, Gross AE. Minor column structural acetabular allografts in revision hip arthroplasty. Clin Orthop Relat Res. 2000;371:75–85. doi: 10.1097/00003086-200002000-00009. [DOI] [PubMed] [Google Scholar]