Abstract
Background
Although surgeons use many procedures to preserve the femoral head in patients with hip osteonecrosis, there is no consensus regarding the best procedure.
Questions/purposes
We raised the following questions: (1) Is one surgical treatment preferred based on published data? (2) What are the rates of radiographic progression or conversion to THA after treatment of pre- and postcollapse hips? (3) Does lesion size in the femoral head influence progression? And (4) does the extent of involvement of the weightbearing surface of the femoral head influence outcome?
Methods
We searched MEDLINE and Scopus for articles published between 1998 and 2010. We included only articles assessing an operative intervention for hip osteonecrosis and having a level of evidence of I to IV. We included 54 of the 488 reviewed manuscripts.
Results
No procedure was superior to others. In pre- and postcollapse hips, 264 of 864 hips (31%) and 419 of 850 hips (49%), respectively, exhibited radiographic disease progression. There were lower failure rates when the lesion involved less than 15% of the femoral head or had a necrotic angle of less than 200° (14%–25%) and when the osteonecrotic lesion involved only the medial 1/3 of the weightbearing surface (4.6%).
Conclusions
The best treatment of precollapse lesions is difficult to determine due to the limitations of the available literature. However, the data suggest operative intervention prevents collapse of small lesions of the femoral head or when there is a limited amount of the weightbearing surface involved. Patients with head collapse have a high progression rate after a femoral head-saving procedure.
Introduction
Osteonecrosis of the hip frequently affects patients between 20 and 50 years of age. Since there are an estimated 10,000 to 20,000 new cases of osteonecrosis per year in the United States [36] and since the disease usually affects young, active patients, it is important that appropriate treatment protocols be established [25, 41]. Although arthroplasty procedures have improved over the past decade, patients in this age group will most likely require multiple revision procedures in their lifetime [25, 32]. Therefore, there is great interest in preserving the femoral head in patients with this diagnosis. Unfortunately, there is no consensus among orthopaedic surgeons regarding the operative management of patients with osteonecrosis of the femoral head.
Numerous procedures have been proposed to treat this condition, including core decompression [1, 6, 18, 19, 24, 29, 47, 49, 58, 63], vascularized grafts [3, 5, 7, 8, 20, 27, 28, 30, 39, 50, 61, 66], and osteotomy [2, 9, 16, 17, 23, 40, 44, 45, 62]. The term “core decompression” represents a spectrum of procedures that may include one large core tract or multiple small tracts [25, 32]. Additionally, core decompression may be supplemented with a vascularized [3, 5, 7, 8, 20, 27, 28, 30, 39, 50, 61, 66] or nonvascularized graft [21, 29, 34, 46, 52, 64] or with electrical stimulation [52]. Marker et al. [33] compared the core decompression procedures before 1992 and between 1992 and 2007 and found patients with collapse of the femoral head often have progression of disease after a femoral head-saving procedure. Their study was, however, limited to core decompression and provided no comparison to other approaches.
We therefore performed a systematic review to address the following questions: (1) Is one surgical treatment preferred based on published data? (2) What are the rates of radiographic progression or conversion to THA after treatment of pre- and postcollapse hips? (3) Does lesion size in the femoral head influence progression? And (4) does the extent of involvement of the weightbearing surface of the femoral head influence outcome?
Search Strategy and Criteria
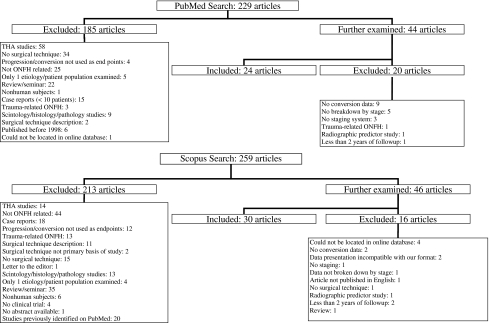
We conducted a search of the electronic databases MEDLINE and Scopus from January 1998 to March 2010 (Fig. 1). For each database, several separate searches were performed. The results were compiled, and duplicate studies were eliminated. Search terms included the phrases “Osteonecrosis of the Femoral Head AND Core Decompression,” “Osteonecrosis of the Femoral Head AND Graft,” “Osteonecrosis of the Femoral Head AND Vascularized Graft,” and “Osteonecrosis of the Femoral Head AND Outcomes.” These terms were selected to provide consistency between search engines and to provide targeted, yet comprehensive search results. We limited the search to original clinical research articles involving human subjects published in the English language and then reviewed the titles and abstracts of the potentially relevant studies obtained from that search. In addition to these searches, the references of all studies deemed relevant by their abstract were reviewed to reveal further studies for possible inclusion. If a review of the abstract suggested the study had the appropriate design and involved human subjects, then we obtained the article and thoroughly evaluated it. This search yielded 488 articles (Fig. 1). From the abstracts, we excluded review articles, case reports, and articles related to management of osteonecrosis or avascular necrosis with THA. We included both prospective and retrospective study designs (level of evidence of I, II, III, or IV) [59]. The inclusion criteria were the following: (1) patients had to be diagnosed with osteonecrosis of the hip; (2) there had to be a surgical intervention to preserve the femoral head that did not include some type of arthroplasty procedure; (3) a classification system needed to be used to evaluate the stage of osteonecrosis of the hip; (4) the mean duration of followup was a minimum of 2 years; and (5) the minimum study size was 10 patients. We excluded any study failing to meet all the inclusion criteria and also if data from the same patients were reported in another study that had longer followup.
Fig. 1.
A flowchart demonstrates the results of our search of the PubMed and Scopus databases. It lists the number of articles initially identified, followed by a list of those excluded by a review of their abstract and a rationale for exclusion. Furthermore, it illustrates which articles were reviewed more thoroughly and those articles that were then excluded or included in the final manuscript on the basis of that analysis. ONFH = osteonecrosis of the femoral head.
Fifty-four of 488 manuscripts met the inclusion criteria for our study (Fig. 1). There was one underpowered prospective randomized controlled trial [12] (Level II, 18 hips) and only eight prospective studies [12, 14, 22, 29, 48, 52, 54, 60] (Table 1).
Table 1.
Analysis of prospective studies
| Study/year/design | Technique | Hips | Precollapse | Failures* | Postcollapse | Failures* |
|---|---|---|---|---|---|---|
| Maniwa et al. [29] (2000) (P) | CD w/wo NVG | 26 | 26 | 8 (30.8%) | ||
| Steinberg et al. [52] (2001) (P) | CD/NVG/EStim | 312 | 198 | 63 (31.8%) | 105 | 48 (45.7%) |
| Gangji et al. [12] (2004) (RCT) | CD | 8 | 8 | 2 (25%) | ||
| CD/BMG | 10 | 10 | 0 (0%) | |||
| Hernigou and Beaujean [14] (2002) (P) | CD/BMG | 189 | 136 | 23 (16.9%) | 7 | 7 (100%) |
| Yang et al. [60] (2009) (P) | CD/BLAC | 56 | 48 | 5 (10.4%) | 8 | 4 (50%) |
| Tsao et al. [54] (2005) (P) | CD/TR | 113 | 94 | 18 (19.1%) | 19 | 4 (21%) |
| Shuler et al. [48] (2007) (P) | CD/TR | 22 | 22 | 3 (13.6%) | ||
| Kim et al. [22] (2005) (P) | VFG | 23 | 10 | 1 (10%) | 13 | 7 (53.8%) |
| NVFG | 23 | 10 | 5 (50%) | 13 | 11 (84.6%) |
Mean followup = 4.19 years (minimum followup was used if no mean was provided); * failure was defined as additional surgery or progression of disease; P = prospective study; RCT = randomized clinical trial; CD = core decompression; w/wo NVG = with and without a nonvascularized graft; NVG = nonvascularized graft; EStim = electrical stimulation; BMG = bone marrow graft; BLAC = biomaterial-loaded allograft threaded cage; TR = tantalum rod; VFG = vascularized fibular graft; NVFG = nonvascularized fibular graft.
We assessed each study regarding classification system used, type of surgical intervention, and number of patients lost to followup. We considered a study to be prospective if it started before the first patient was enrolled and considered it to be retrospective if it started after the first patient was enrolled [59].
One of the authors (SME) extracted the relevant data from each study and recorded them on a worksheet. These data included the number of eligible patients, duration of followup, number of patients lost to followup, demographics of patients, surgical technique, classification system used to evaluate the osteonecrosis, results of surgery, and complications. Three of the authors (JRL, RMM, SME) independently assessed each manuscript to confirm whether it was retrospective or prospective in design, number of patients involved, classification system used, and number of patients lost to followup. If there were any discrepancies, they were resolved by conference among the three authors.
Results
We identified no one preferable technique based on the available data. The majority of studies (25 of 43) [1, 3, 9, 12, 14–16, 20, 26–28, 40, 45–48, 50, 54–57, 60, 61, 64, 66] reported success rates of greater than 80% based on no collapse of the joint (range, 40%–100%).
In patients with precollapse hips, 409 of 2163 (19%) hips were converted to THA (Table 2), and 264 of 864 hips (31%) exhibited radiographic progression of disease (Table 3). In patients with postcollapse hips, 442 of 1463 hips (30%) were converted to THA (Table 2), and progression of disease was noted in 419 of 850 hips (49%) (Table 3).
Table 2.
Femoral head-saving procedures analyzed by clinical failure (THA or additional surgery)
| Study/year/design | Technique | Hips | Precollapse | Failures | Postcollapse | Failures |
|---|---|---|---|---|---|---|
| Iorio et al. [18] (1998) (R) | CD | 33 | 33 | 11 (33.3%) | ||
| Bozic et al. [6] (1999) (R) | CD | 54 | 46 | 20 (43.4%) | 8 | 8 (100%) |
| Simank et al. [49] (1999) (R) | CD | 94 | 30 | 12 (40%) | 31 | 20 (64.5%) |
| Lavernia and Sierra [24] (2000)* (R) | CD | 65 | § | (66%) | ||
| Maniwa et al. [29] (2000) (P) | CD w/wo NVG | 26 | 26 | 8 (30.8%) | ||
| Aigner et al. [1] (2002) (R) | CD | 45 | 39 | 1 (2.6%) | 6 | 3 (50%) |
| Wirtz et al. [58] (2003) (R) | CD | 51 | 41 | 9 (22%) | 10 | 9 (90%) |
| Shahrezaee et al. [47] (2008) (R) | CD | 56 | 51 | 0 (0%) | 5 | 0 (0%) |
| Mont et al. [38] (2004)† (R) | CD/SD | 45 | 45 | 13 (28.9%) | ||
| Marker et al. [33] (2008) (R) | CD/SD | 79 | 79 | 27 (34.2%) | ||
| Israelite et al. [19] (2005)* (R) | UCD | 124 | ∥ | ∥ | ||
| BCD | 152 | |||||
| Mont et al. [34] (1998)† (R) | CD/TDBG | 30 | 30 | 8 (26.7%) | ||
| Steinberg et al. [52] (2001) (P) | CD/NVG/EStim | 312 | 198 | 63 (31.8%) | 105 | 48 (45.7%) |
| Yoon et al. [63] (2001) (R) | CD | 39 | 31 | 14 (45.1%) | 8 | 8 (100%) |
| Keizer et al. [21] (2006) (R) | NVFG | 62 | 57 | 21 (36.8%) | 26 | 13 (50%) |
| NVTG | 18 | |||||
| Seyler et al. [46] (2008) (R) | CD/NVG/OP1 | 39 | 22 | 4 (18.2%) | 17 | 9 (52.9%) |
| Mont et al. [35] (2003)† (R) | CD/NVG | 21 | 7 | 2 (28.6%) | 14 | 1 (7.1%) |
| Yuhan et al. [64] (2009) (R) | CD/NVG | 11 | 5 | 0 (0%) | 6 | 3 (50%) |
| Lieberman et al. [26] (2004) (R) | CD/BMP | 17 | 16 | 2 (12.5%) | 1 | 1 (100%) |
| Hernigou and Beaujean [14] (2002) (R) | CD/BMG | 189 | 145 | 9 (6.2%) | 44 | 25 (56.8%) |
| Gangji et al. [12] (2004) (RCT) | CD | 8 | 8 | 2 (25%) | ||
| CD/BMG | 10 | 10 | 0 (0%) | |||
| Hernigou et al. [15] (2009) (R) | CD/BMG | 534 | 534 | 94 (17.6%) | ||
| Wang et al. [56] (2010) (R) | CD/BMMNC | 59 | 50 | 6 (12%) | 9 | 1 (11.1%) |
| Wang et al. [57] (2009) (R) | SEC | 81 | 54 | 8 (14.8%) | 27 | 6 (22.2%) |
| Yang et al. [60] (2010) (P) | CD/BLAC | 56 | 48 | 5 (10.4%) | 8 | 4 (50%) |
| Tsao et al. [54] (2005) (P) | CD/TR | 113 | 94 | 18 (19.2%) | 19 | 4 (21.1%) |
| Veillette et al. [55] (2006) (R) | CD/TR | 58 | 50 | 6 (12%) | 8 | 3 (37.5%) |
| Shuler et al. [48] (2007) (P) | CD/TR | 22 | 22 | 3 (13.6%) | ||
| Louie et al. [27] (1999) (R) | FVFG | 59 | 5 | 0 (0%) | 53 | 16 (30.2%) |
| Soucacos et al. [50] (2001) (R) | VFG | 184 | 39 | 0 (0%) | 145 | 14 (9.7%) |
| Berend et al. [5] (2003) (R) | FVFG | 224 | 224 | 73 (32.6%) | ||
| Dailiana et al. [8] (2007) (R) | FVFG p failed CD | 54 | 5 | 3 (60%) | 49 | 17 (34.7%) |
| FVFG | 32 | 3 | 1 (33.3%) | 29 | 14 (48.3%) | |
| Kawate et al. [20] (2007) (R) | FVFG | 71 | 31 | 1 (3.23%) | 40 | 12 (30%) |
| Yoo et al. [61] (2008) (R) | VFG | 124 | 59 | 7 (11.9%) | 65 | 6 (9.2%) |
| Lowrie et al. [28] (2010) (R) | FVFG | 10 | 7 | 1 (14.3%) | 3 | 0 (0%) |
| Zhao et al. [65] (2010) (R) | VGTG | 195 | 81 | 17 (21%) | 116 | 23 (19.8%) |
| Zhao et al. [66] (2006) (R) | VIG | 226 | 91 | 2 (2.2%) | 135 | 12 (8.9%) |
| Chen et al. [7] (2009) (R) | VIG | 33 | 33 | 25 (75.8%) | ||
| Babhulkar [3] (2009) (R) | VIG | 39 | 9 | 0 (0%) | 22 | 1 (4.5%) |
| Fuchs et al. [11] (2003) (R) | ITO/VIG | 44 | 11 | 4 (36.4%) | 33 | 11 (33.3%) |
| Sakano et al. [45] (2004) (R) | CVO | 20 | 14 | 0 (0%) | 6 | 0 (0%) |
| Langlais et al. [23] (2004) (R) | RO | 19 | 11 | 4 (36.4%) | 8 | 6 (75%) |
| Hisatome et al. [16] (2004) (R) | SO | 25 | 15 | 2 (13.3%) | 10 | 0 (0%) |
| Onodera et al. [40] (2005) (R) | TTRO | 37 | 1 | 0 (0%) | 36 | 15 (41.7%) |
| Rijnen et al. [44] (2005) (R) | SO | 25 | 9 | 5 (56.6%) | 15 | 7 (46.7%) |
| Ikemura et al.‡ [17] (2009) (R) | TTRO | 27† | 27 | 2 (7.4%) | ||
| Drescher et al. [9] (2003) (R) | FO | 70 | 31 | 4 (12.9%) | 32 | 14 (43.8%) |
| Total | 3626 | 2163 | 409 | 1463 | 442 |
Mean followup = 5.96 years (minimum followup was used if no mean was provided); * exact number of hips not indicated in article; data not included in totals; †data presented as clinical failure indicating THA or Harris hip score of less than 70/80; numbers in these studies may not accurately represent total number of revisions; ‡all patients younger than 20 years; §Stage I hips: 0% failures; Stage II hips: 17% failures (not included in total); ∥Stage I: 28% failures; Stage II hips: 34% failures; Stage III hips: 23% failures; Stage IV hips: 49% failures (not included in total); P = prospective study; R = retrospective study; RCT = randomized clinical trial; CD = core decompression; w/wo NVG = with and without a nonvascularized graft; SD = multiple small-diameter drillings; UCD = unilateral core decompression; BCD = bilateral core decompression; TDBG = trap door bone graft; NVG = nonvascularized graft; EStim = electrical stimulation; NVFG = nonvascularized fibular graft; NVTG = nonvascularized tibial graft; NVG/OP-1 = nonvascularized graft enriched with OP-1; NVG = nonvascularized graft; BMP = graft enriched with bone morphogenic protein; BMG = bone marrow graft; BMMNC = bone marrow mononuclear cell graft; SEC = superelastic cage implantation; BLAC = biomaterial-loaded allograft threaded cage; TR = tantalum rod; VFG = vascularized fibular graft; FVFG = free vascularized fibular graft; FVFG p failed CD = free vascularized fibular graft after failed core decompression; VGTG = vascularized greater trochanter graft; VIG = vascularized iliac graft; ITO = intertrochanteric osteotomy; CVO = curved varus osteotomy; RO = rotational osteotomy; SO = Sugioka osteotomy; TTRO = transtrochanteric rotational osteotomy; FO = flexion osteotomy.
Table 3.
Femoral head-saving procedures analyzed by radiographic progression of disease
| Study/year/design | Technique | Hips | Precollapse | Progression | Postcollapse | Progression |
|---|---|---|---|---|---|---|
| Iorio et al. (1998) [18] (R) | CD | 33 | 33 | 18 (54.5%) | ||
| Bozic et al. (1999) [6] (R) | CD | 54 | 46 | 26 (56.5%) | 8 | 8 (100%) |
| Simank et al. (1999) [49] (R) | CD | 94 | 30 | 13 (43.3%) | 31 | 19 (61.3%) |
| Lavernia and Sierra (2000) [24] (R) | CD | 65 | ||||
| Aigner et al. (2002) [1] (R) | CD | 45 | 39 | 5 (12.8%) | 6 | 3 (50%) |
| Keizer et al. (2006) [21] (R) | NVFG | 62 | 57 | 44 (77.2%) | 13 | 8 (61.5%) |
| NVTG | 18 | |||||
| Hernigou and Beaujean (2002) [14] (P) | CD/BMG | 189 | 136 | 23 (16.9%) | 7 | 7 (100%) |
| Gangji et al. (2004) [12] (RCT) | CD | 8 | 8 | 5 (62.5%) | ||
| CD/BMG | 10 | 10 | 1 (10%) | |||
| Baksi et al. (2009) [4] (R) | CD/MPG | 187 | 79 | 14 (17.7%) | 68 | 29 (42.6%) |
| Louie et al. (1999) [27] (R) | FVFG | 59 | 5 | 4 (80%) | 52 | 25 (48.1%) |
| Soucacos et al. (2001) [50] (R) | VFG | 184 | 39 | 2 (5.1%) | 145 | 70 (48.3%) |
| Marciniak et al. (2005) [30] (R) | FVFG | 101 | 14 | 7 (50%) | 87 | 52 (59.8%) |
| Zhao et al. (2010) [65] (R) | VGTG | 195 | 81 | 0 (0%) | 114 | 60 (52.6%) |
| Kawate et al. (2007) [20] (R) | FVFG | 71 | 31 | 10 (32.2%) | 40 | 25 (62.5%) |
| Zhao et al. (2006) [66] (R) | VIG | 226 | 89 | 11 (12.4%) | 123 | 49 (39.8%) |
| Nagoya et al. (2004) [39] (R) | VIG | 35 | 28 | 12 (42.9%) | 7 | 7 (100%) |
| Fuchs et al. (2003) [11] (R) | ITO/VIG | 44 | 17 | 7 (41.2%) | 22 | 13 (59.1%) |
| Hisatome et al. (2004) [16] (R) | SO | 25 | 15 | 6 (40%) | 10 | 4 (40%) |
| Atsumi et al. (2006) [2] (R) | PRO | 35 | 35 | 2 (5.7%) | ||
| Yoon et al. (2008) [62] (R) | TTRO | 43 | 17 | 1 (5.9%) | 26 | 2 (7.7%) |
| Plakseychuk et al. (2003) [42] (R) | VFG | 50 | 35 | 6 (17.1%) | 15 | 7 (46.7%) |
| NVFG | 50 | 35 | 25 (71.4%) | 15 | 11 (73.3%) | |
| Kim et al. (2005) [22] (P) | VFG | 23 | 10 | 1 (10%) | 13 | 7 (53.8%) |
| NVFG | 23 | 10 | 5 (50%) | 13 | 11 (84.6%) | |
| Total | 1714 | 864 | 264 | 850 | 419 |
Mean followup = 7.12 years (minimum followup was used if no mean was provided); P = prospective study; R = retrospective study; RCT = randomized clinical trial; CD = core decompression; NVFG = nonvascularized fibular graft; NVTG = nonvascularized tibial graft; BMG = bone marrow graft; MPG = muscle pedicle graft; FVFG = free vascularized fibular graft; VFG = vascularized fibular graft; VGTG = vascularized greater trochanter graft; VIG = vascularized iliac graft; ITO = intertrochanteric osteotomy; SO = Sugioka osteotomy; PRO = posterior rotational osteotomy; TTRO = transtrochanteric rotational osteotomy.
We identified six studies assessing the results of core decompression based on lesion size (Table 4). Four of these six [19, 33, 38, 63] (439 hips) evaluated patients with osteonecrosis treated with core decompression alone (Table 4). A lesion was classified as small if less than 15% of the femoral head was affected or the total necrotic angle was less than 200°, medium if 15% to 30% of the femoral head was affected, and large if greater than 30% of the femoral head was affected or the total necrotic angle was greater than 200°. The failure rates among small lesions ranged between 14% and 25%, and the failure rate in patients with large lesions ranged between 42% and 84%. Two studies (51 hips) assessed core decompression with nonvascularized grafts [34, 35] and classified lesions as small (necrotic angle < 200°) or large (necrotic angle > 200°) (Table 5). The failure rates in the small lesion group were 14% (three of 21 hips) and 0% (zero of seven hips), and the failure rates in the large lesion groups were 56% (five of nine hips) and 21% (three of 14 hips). Three studies (419 hips) assessed the outcome of core decompression with vascularized grafts [5, 20, 61] and classified lesions as small (< 25% of the femoral head), medium (25%–50% of the femoral head), or large (> 50% of the femoral head). Hips with small lesions had an average failure rate of 24.6% (range, 0%–52.6%) and hips with large lesions had an average failure rate of 42.8% (range, 16.9%–73.3%).
Table 4.
Failure (clinical or radiographic) based on lesion size
| Study/year/design | Technique | Hips | Small (<15%) | Medium (15%–30%) | Large (>30%) | |||
|---|---|---|---|---|---|---|---|---|
| Hips | Failures | Hips | Failures | Hips | Failures | |||
| Yoon et al. [63] (2001) (R) | CD | 39 | 14 | 2 (14.3%) | 7 | 4 (57.1%) | 19 | 16 (84.2%) |
| Steinberg et al. [52] (2001) (P) | CD/NVG/EStim | 312 | 14% | 48% | 42% | |||
| Israelite et al. [19] (2005) (R) | UCD | 124 | 14%† | 48%† | 42%† | |||
| BCD | 152 | |||||||
| Mont et al. [38] (2004) (R) | CD/SD | 45 | ‡ | 12 | 7 | |||
| Yoo et al. [61] (2008) (R) | VFG | 124 | 27 | 0 (0%) | 38 | 3 (7.89%) | 59 | 10 (16.9%) |
| Kawate et al. [20] (2007) (R) | FVFG | 71 | 19 | 10 (52.6%) | 15 | 11 (73.3%) | ||
| Berend et al. [5] (2003)* (R) | FVFG | 224 | (21.1%) | (38.2%) | (38.2%) | |||
Mean followup = 4.89 years (minimum followup was used if no mean was provided); * in this study, small was defined as less than 25%; medium as 25% to 50%, and large as greater than 50%; †only Stage I and II hips included; ‡in the small and medium-sized groups: six failures in 33 hips (18.2%); P = prospective study; R = retrospective study; CD = core decompression; NVG = nonvascular graft; EStim = electrical stimulation; UCD = unilateral core decompression; BCD = bilateral core decompression; SD = multiple small-diameter drillings; VFG = vascularized fibular graft; FVFG = free vascularized fibular graft.
Table 5.
Failure (clinical or radiographic) based on necrotic angle
| Study/year/design | Technique | Hips | Small angle (<200°) | Large angle (≥200°) | ||
|---|---|---|---|---|---|---|
| Hips | Failures | Hips | Failures | |||
| Mont et al. [34] (1998) (R) | CD/TDBG | 30 | 21 | 3 (14%) | 9 | 5 (56%) |
| Mont et al. [35] (2003) (R) | CD/NVG | 21 | 7 | 0 (0%) | 14 | 3 (21%) |
R = retrospective study; CD = core decompression; TDBG = trap door bone graft; NVG = nonvascularized graft.
We found five studies (163 hips) evaluating five different operative procedures that analyzed outcomes based on extent of involvement of the weightbearing surface of the femoral head (Table 6) [26, 39, 40, 46]. The location of the lesion was described according to the Japanese Investigation Committee’s 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head [53]. One of 22 Type A hips (4.6%), six of 39 Type B (15.4%), 15 of 48 Type C1 (31.3%), and 26 of 43 Type C2 (60.5%) failed. One study combined Types C1 and C2 and reported two of four failed hips in that group.
Table 6.
Failure (clinical or radiographic) based on lesion location
| Study/year/design | Technique | Hips | Lesion location | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C1 | C2 | |||||||
| Hips | Failures | Hips | Failures | Hips | Failures | Hips | Failures | |||
| Lieberman et al. [26] (2004) (R) | CD/BMP | 17 | 3 | 0 (0%) | 7 | 1 (14.3%) | ||||
| Nagoya et al. [39] (2004) (R) | VIG | 35 | 17 | 4 (23.5%) | 18 | 15 (83.3%) | ||||
| Onodera et al. [40] (2005) (R) | TTRO | 37 | 19 | 9 (47.4%) | 18 | 6 (33.3%) | ||||
| Atsumi et al. [2] (2006) (R) | PRO | 35 | 11 | 0 (0%) | 20 | 0 (0%) | 4 hips, 2 failures* | |||
| Seyler et al. [46] (2008) (R) | CD/NVG/OP1 | 39 | 8 | 1 (12.5%) | 12 | 5 (41.7%) | 12 | 2 (16.7%) | 7 | 5 (71.4%) |
| Total | 163 | 22 | 1 (4.6%) | 39 | 6 (15.4%) | 48 | 15 (31.2%) | 43 | 26 (60.4%) | |
* Not included in totals; A: ≤ medial 1/3 weightbearing; B: ≤ medial 2/3 weightbearing; C1: > 2/3 not extending to acetabular ridge; C2: > 2/3 extending to acetabular ridge; P = prospective study; R = retrospective study; CD = core decompression; BMP = bone morphogenic protein; VIG = vascularized iliac graft; TTRO = transtrochanteric rotational osteotomy; PRO = posterior rotational osteotomy; NVG/OP-1 = nonvascularized graft enriched with OP-1.
Discussion
Although surgeons use many procedures to preserve the femoral head in patients with hip osteonecrosis, there is no consensus regarding the best procedure. The purposes of this systematic review were to answer the following critical questions associated with surgical management of osteonecrosis of the hip: (1) Is one surgical treatment preferred based on published data? (2) What are the rates of radiographic progression or conversion to THA after treatment of pre- and postcollapse hips? (3) Does lesion size in the femoral head influence progression? And (4) does the extent of involvement of the weightbearing surface of the femoral head influence outcome?
The literature and our specific search are subject to limitations. First, there are no appropriately powered randomized trials comparing different surgical techniques and these studies are necessary to determine which operative technique is most effective in preventing collapse of the femoral head. Second, the studies tended to include patients with different diagnoses associated with osteonecrosis (ie, steroid induced, trauma, sickle cell disease), but the natural history of osteonecrosis in these cases may differ. In addition, patients need to be evaluated using the same classification system. Six different classification systems were used to evaluate the extent of the disease in the femoral head [10, 31, 37, 43, 51, 53]. Third, the use of time to arthroplasty as an outcome will clearly underestimate the number of failures, especially if followup is short. Patients may be reluctant to undergo a THA and surgeons may delay in performing an arthroplasty soon after a failed femoral head-saving procedure. In addition, a number of studies did not report complete data on the outcome of each hip. For example, 32 studies [3, 5, 7–9, 15, 17, 19, 23, 26, 28, 29, 33–35, 38, 40, 44–48, 52, 54–58, 60, 61, 63, 64] reported data only in terms of conversion to THA, and seven reported only in terms of progression of disease [2, 4, 22, 30, 39, 42, 62]. Only 15 studies reported data in terms of both conversion to THA and progression of disease [1, 6, 11, 12, 14, 16, 18, 20, 21, 24, 27, 49, 50, 65, 66]. Fourth, most of the studies in this review did not use a validated patient-oriented questionnaire to evaluate outcomes. A majority of the studies used the Harris hip score [13], which has two major limitations: (1) the hip score is generated by the physician, and (2) only a limited number of activities are assessed. This is a major problem in evaluating femoral head-saving procedures if one chooses to use pain and function rather than time to arthroplasty to determine the success or failure of the procedure. Fifth, while we assessed each study for the presence or absence of certain types of information and level of evidence, we had no formal assessment of study quality. Finally, we limited our selection of papers to those in the English language. We cannot confirm whether these are representative of the whole or whether individual non-English manuscripts might have contained crucial information where there were few studies.
The data do not demonstrate any particular procedure is superior with respect to operative treatment of osteonecrosis of the hip in terms of conversion to THA (Table 2) or radiographic progression of disease (Table 3). There were only eight prospective studies [12, 14, 22, 29, 48, 52, 54, 60] and one randomized trial in the literature [12]. Our systematic review revealed 15 different operative procedures were used to treat osteonecrosis of the hip.
The data demonstrate operative procedures designed to save the femoral head do not prevent progression of disease in hips that have already collapsed. The results with postcollapse hips demonstrate 50% had radiographic progression of disease (Table 3). In contrast, only 19% of precollapse hips (409 of 2163) were converted to THA (Table 2) and only 31% (264 of 864) demonstrated radiographic progression of disease (Table 3).
Core decompression, with or without grafting, is effective in patients with small lesions involving less than 15% of the femoral head or with a necrotic angle less than 200° (failure rates: 14%–25%). The failure rates are even lower (4.5%) when the osteonecrotic lesion occupies less than 30% of the medial weightbearing surface. However, core decompression alone demonstrates more variable failure rates in patients with large lesions (42%–84%).
We identified three studies [5, 20, 61] (419 hips) that assessed the influence of lesion size on outcomes of core decompression combined with a vascularized bone graft, and these studies reported wide variability in results with both small and large lesions. For small lesions, the three studies reported failure rates of 0% [61], 21.1% [5], and 53% [20] respectively. Two studies reported reasonable failure rates for large lesions (16.9% [61] and 38. 2% [5]), but the third study reported a failure rate of 73% [20]. These results suggest patient selection and technical expertise have an important impact on the results of vascularized grafts for the treatment of precollapse lesions. Clearly, randomized clinical trials are needed to determine whether the use of a vascularized graft enhances outcomes compared to core decompression alone or with a nonvascularized graft.
Five studies [2, 26, 39, 40, 46] evaluated the results of different procedures based on location of the osteonecrotic lesion. In lesions comprising less than 30% of the medial weightbearing surface, only one of 22 hips (4.5%) failed. In contrast, in hips with lesions occupying greater than 60% of the medial weightbearing surface, 41 of 91 hips failed (45%). Furthermore, when these large lesions extend beyond the acetabular ridge, 26 of 43 hips failed (60.5%). These findings suggest, when attempting to predict outcome, the overall size of the lesion and its location related to the medial weightbearing surface may be just as important as the type of operative procedure selected.
Despite the limitations of the quality of the literature, our analysis suggests core decompression, with or without bone grafting, is effective in treating small lesions and a variety of surgical procedures can be used to treat lesions that occupy less than 30% of the medal weightbearing surface of the hip. The results of treatment of large lesions are variable and require further study to determine the optimal operative management strategy. Finally, once the hip has collapsed, attempts at head preservation are associated with high failure rates and operative intervention cannot be recommended for these patients.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the University of Connecticut School of Medicine.
References
- 1.Aigner N, Schneider W, Eberl V, Knahr K. Core decompression in early stages of femoral head osteonecrosis—an MRI-controlled study. Int Orthop. 2002;26:31–35. doi: 10.1007/s00264-001-0311-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Atsumi T, Kajiwara T, Hiranuma Y, Tamaoki S, Asakura Y. Posterior rotational osteotomy for nontraumatic osteonecrosis with extensive collapsed lesions in young patients. J Bone Joint Surg Am. 2006;88(Suppl 3):42–47. doi: 10.2106/JBJS.F.00767. [DOI] [PubMed] [Google Scholar]
- 3.Babhulkar S. Osteonecrosis of femoral head: treatment by core decompression and vascular pedicle grafting. Indian J Orthop. 2009;43:27–35. doi: 10.4103/0019-5413.45320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baksi DP, Pal AK, Baksi DD. Long-term results of decompression and muscle-pedicle bone grafting for osteonecrosis of the femoral head. Int Orthop. 2009;33:41–47. doi: 10.1007/s00264-007-0455-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berend KR, Gunneson EE, Urbaniak JR. Free vascularized fibular grafting for the treatment of postcollapse osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85:987–993. doi: 10.2106/00004623-200306000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Bozic KJ, Zurakowski D, Thornhill TS. Survivorship analysis of hips treated with core decompression for nontraumatic osteonecrosis of the femoral head. J Bone Joint Surg Am. 1999;81:200–209. doi: 10.2106/00004623-199902000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Chen CC, Lin CL, Chen WC, Shih HN, Ueng SW, Lee MS. Vascularized iliac bone-grafting for osteonecrosis with segmental collapse of the femoral head. J Bone Joint Surg Am. 2009;91:2390–2394. doi: 10.2106/JBJS.H.01814. [DOI] [PubMed] [Google Scholar]
- 8.Dailiana ZH, Toth AP, Gunneson E, Berend KR, Urbaniak JR. Free vascularized fibular grafting following failed core decompression for femoral head osteonecrosis. J Arthroplasty. 2007;22:679–688. doi: 10.1016/j.arth.2006.12.042. [DOI] [PubMed] [Google Scholar]
- 9.Drescher W, Furst M, Hahne HJ, Helfenstein A, Petersen W, Hassenpflug J. Survival analysis of hips treated with flexion osteotomy for femoral head necrosis. J Bone Joint Surg Br. 2003;85:969–974. doi: 10.1302/0301-620X.85B7.14155. [DOI] [PubMed] [Google Scholar]
- 10.Ficat RP. Idiopathic bone necrosis of the femoral head. Early diagnosis and treatment. J Bone Joint Surg Br. 1985;67:3–9. doi: 10.1302/0301-620X.67B1.3155745. [DOI] [PubMed] [Google Scholar]
- 11.Fuchs B, Knothe U, Hertel R, Ganz R. Femoral osteotomy and iliac graft vascularization for femoral head osteonecrosis. Clin Orthop Relat Res. 2003;412:84–93. doi: 10.1097/01.blo.0000071756.07450.76. [DOI] [PubMed] [Google Scholar]
- 12.Gangji V, Hauzeur JP, Matos C, Maertelaer V, Toungouz M, Lambermont M. Treatment of osteonecrosis of the femoral head with implantation of autologous bone-marrow cells: a pilot study. J Bone Joint Surg Am. 2004;86:1153–1160. doi: 10.2106/00004623-200406000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 14.Hernigou P, Beaujean F. Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res. 2002;405:14–23. doi: 10.1097/00003086-200212000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Hernigou P, Poignard A, Zilber S, Rouard H. Cell therapy of hip osteonecrosis with autologous bone marrow grafting. Indian J Orthop. 2009;43:40–45. doi: 10.4103/0019-5413.45322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hisatome T, Yasunaga Y, Takahashi K, Ochi M. Progressive collapse of transposed necrotic area after transtrochanteric rotational osteotomy for osteonecrosis of the femoral head induces osteoarthritic change: mid-term results of transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2004;124:77–81. doi: 10.1007/s00402-003-0610-0. [DOI] [PubMed] [Google Scholar]
- 17.Ikemura S, Yamamoto T, Nakashima Y, Mawatari T, Motomura G, Iwamoto Y. Transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head in patients 20 years or younger. J Pediatr Orthop. 2009;29:219–223. doi: 10.1097/BPO.0b013e31819bc746. [DOI] [PubMed] [Google Scholar]
- 18.Iorio R, Healy WL, Abramowitz AJ, Pfeifer BA. Clinical outcome and survivorship analysis of core decompression for early osteonecrosis of the femoral head. J Arthroplasty. 1998;13:34–41. doi: 10.1016/S0883-5403(98)90073-0. [DOI] [PubMed] [Google Scholar]
- 19.Israelite C, Nelson CL, Ziarani CF, Abboud JA, Landa J, Steinberg ME. Bilateral core decompression for osteonecrosis of the femoral head. Clin Orthop Relat Res. 2005;441:285–290. doi: 10.1097/01.blo.0000192365.58958.84. [DOI] [PubMed] [Google Scholar]
- 20.Kawate K, Yajima H, Sugimoto K, Ono H, Ohmura T, Kobata Y, Murata K, Shigematsu K, Kawamura K, Kawahara I, Maegawa N, Tamai K, Takakura Y, Tamai S. Indications for free vascularized fibular grafting for the treatment of osteonecrosis of the femoral head. BMC Musculoskelet Disord. 2007;8:78. doi: 10.1186/1471-2474-8-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keizer SB, Kock NB, Dijkstra PD, Taminiau AH, Nelissen RG. Treatment of avascular necrosis of the hip by a non-vascularised cortical graft. J Bone Joint Surg Br. 2006;88:460–466. doi: 10.1302/0301-620X.88B4.16950. [DOI] [PubMed] [Google Scholar]
- 22.Kim SY, Kim YG, Kim PT, Ihn JC, Cho BC, Koo KH. Vascularized compared with nonvascularized fibular grafts for large osteonecrotic lesions of the femoral head. J Bone Joint Surg Am. 2005;87:2012–2018. doi: 10.2106/JBJS.D.02593. [DOI] [PubMed] [Google Scholar]
- 23.Langlais F, Fourastier J, Gedouin JE, Ropars M, Lambotte JC, Thomazeau H. Can rotation osteotomy remain effective for more than ten years? Orthop Clin North Am. 2004;35:345–351, ix. [DOI] [PubMed]
- 24.Lavernia CJ, Sierra RJ. Core decompression in atraumatic osteonecrosis of the hip. J Arthroplasty. 2000;15:171–178. doi: 10.1016/S0883-5403(00)90132-3. [DOI] [PubMed] [Google Scholar]
- 25.Lieberman JR, Berry DJ, Mont MA, Aaron RK, Callaghan JJ, Rajadhyaksha AD, Urbaniak JR. Osteonecrosis of the hip: management in the 21st century. Instr Course Lect. 2003;52:337–355. [PubMed] [Google Scholar]
- 26.Lieberman JR, Conduah A, Urist MR. Treatment of osteonecrosis of the femoral head with core decompression and human bone morphogenetic protein. Clin Orthop Relat Res. 2004;429:139–145. doi: 10.1097/01.blo.0000150312.53937.6f. [DOI] [PubMed] [Google Scholar]
- 27.Louie BE, McKee MD, Richards RR, Mahoney JL, Waddell JP, Beaton DE, Schemitsch EH, Yoo DJ. Treatment of osteonecrosis of the femoral head by free vascularized fibular grafting: an analysis of surgical outcome and patient health status. Can J Surg. 1999;42:274–283. [PMC free article] [PubMed] [Google Scholar]
- 28.Lowrie AG, Rao K, Nanu A, Erdmann MW. Reversed flow lateral circumflex femoral vessels as recipients for free fibular grafting in treatment of femoral head osteonecrosis. Microsurgery. 2010;30:19–23. doi: 10.1002/micr.20695. [DOI] [PubMed] [Google Scholar]
- 29.Maniwa S, Nishikori T, Furukawa S, Kajitani K, Iwata A, Nishikawa U, Ochi M. Evaluation of core decompression for early osteonecrosis of the femoral head. Arch Orthop Trauma Surg. 2000;120:241–244. doi: 10.1007/s004020050456. [DOI] [PubMed] [Google Scholar]
- 30.Marciniak D, Furey C, Shaffer JW. Osteonecrosis of the femoral head: a study of 101 hips treated with vascularized fibular grafting. J Bone Joint Surg Am. 2005;87:742–747. doi: 10.2106/JBJS.D.02004. [DOI] [PubMed] [Google Scholar]
- 31.Marcus ND, Enneking WF, Massam RA. The silent hip in idiopathic aseptic necrosis: treatment by bone-grafting. J Bone Joint Surg Am. 1973;55:1351–1366. [PubMed] [Google Scholar]
- 32.Marker DR, Seyler TM, McGrath MS, Delanois RE, Ulrich SD, Mont MA. Treatment of early stage osteonecrosis of the femoral head. J Bone Joint Surg Am. 2008;90(Suppl 4):175–187. doi: 10.2106/JBJS.H.00671. [DOI] [PubMed] [Google Scholar]
- 33.Marker DR, Seyler TM, Ulrich SD, Srivastava S, Mont MA. Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin Orthop Relat Res. 2008;466:1093–1103. doi: 10.1007/s11999-008-0184-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mont MA, Einhorn TA, Sponseller PD, Hungerford DS. The trapdoor procedure using autogenous cortical and cancellous bone grafts for osteonecrosis of the femoral head. J Bone Joint Surg Br. 1998;80:56–62. doi: 10.1302/0301-620X.80B1.7989. [DOI] [PubMed] [Google Scholar]
- 35.Mont MA, Etienne G, Ragland PS. Outcome of nonvascularized bone grafting for osteonecrosis of the femoral head. Clin Orthop Relat Res. 2003;417:84–92. doi: 10.1097/01.blo.0000096826.67494.38. [DOI] [PubMed] [Google Scholar]
- 36.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77:459–474. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 37.Mont MA, Marulanda GA, Jones LC, Saleh KJ, Gordon N, Hungerford DS, Steinberg ME. Systematic analysis of classification systems for osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88(Suppl 3):16–26. doi: 10.2106/JBJS.F.00457. [DOI] [PubMed] [Google Scholar]
- 38.Mont MA, Ragland PS, Etienne G. Core decompression of the femoral head for osteonecrosis using percutaneous multiple small-diameter drilling. Clin Orthop Relat Res. 2004;429:131–138. doi: 10.1097/01.blo.0000150128.57777.8e. [DOI] [PubMed] [Google Scholar]
- 39.Nagoya S, Nagao M, Takada J, Kuwabara H, Wada T, Kukita Y, Yamashita T. Predictive factors for vascularized iliac bone graft for nontraumatic osteonecrosis of the femoral head. J Orthop Sci. 2004;9:566–570. doi: 10.1007/s00776-004-0841-0. [DOI] [PubMed] [Google Scholar]
- 40.Onodera S, Majima T, Abe Y, Ito H, Matsuno T, Minami A. Transtrochanteric rotational osteotomy for osteonecrosis of the femoral head: relation between radiographic features and secondary collapse. J Orthop Sci. 2005;10:367–373. doi: 10.1007/s00776-005-0906-8. [DOI] [PubMed] [Google Scholar]
- 41.Petrigliano FA, Lieberman JR. Osteonecrosis of the hip: novel approaches to evaluation and treatment. Clin Orthop Relat Res. 2007;465:53–62. doi: 10.1097/BLO.0b013e3181591c92. [DOI] [PubMed] [Google Scholar]
- 42.Plakseychuk AY, Kim SY, Park BC, Varitimidis SE, Rubash HE, Sotereanos DG. Vascularized compared with nonvascularized fibular grafting for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am. 2003;85:589–596. doi: 10.2106/00004623-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 43.Plakseychuk AY, Shah M, Varitimidis SE, Rubash HE, Sotereanos D. Classification of osteonecrosis of the femoral head: reliability, reproducibility, and prognostic value. Clin Orthop Relat Res. 2001;386:34–41. doi: 10.1097/00003086-200105000-00005. [DOI] [PubMed] [Google Scholar]
- 44.Rijnen WH, Gardeniers JW, Westrek BL, Buma P, Schreurs BW. Sugioka’s osteotomy for femoral-head necrosis in young Caucasians. Int Orthop. 2005;29:140–144. doi: 10.1007/s00264-005-0639-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sakano S, Hasegawa Y, Torii Y, Kawasaki M, Ishiguro N. Curved intertrochanteric varus osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br. 2004;86:359–365. doi: 10.1302/0301-620X.86B3.14383. [DOI] [PubMed] [Google Scholar]
- 46.Seyler TM, Marker DR, Ulrich SD, Fatscher T, Mont MA. Nonvascularized bone grafting defers joint arthroplasty in hip osteonecrosis. Clin Orthop Relat Res. 2008;466:1125–1132. doi: 10.1007/s11999-008-0211-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shahrezaee M, Navab I, Keshtkari S, Khatibi A, Motaghi A, Farrokhi A. Efficacy of core decompression plus bone graft with minimal incision in 41 patients with osteonecrosis of the femoral head. Int J Rheum Dis. 2008;11:274–278. doi: 10.1111/j.1756-185X.2008.00362.x. [DOI] [Google Scholar]
- 48.Shuler MS, Rooks MD, Roberson JR. Porous tantalum implant in early osteonecrosis of the hip: preliminary report on operative, survival, and outcomes results. J Arthroplasty. 2007;22:26–31. doi: 10.1016/j.arth.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 49.Simank HG, Brocai DR, Strauch K, Lukoschek M. Core decompression in osteonecrosis of the femoral head: risk-factor-dependent outcome evaluation using survivorship analysis. Int Orthop. 1999;23:154–159. doi: 10.1007/s002640050335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Soucacos PN, Beris AE, Malizos K, Koropilias A, Zalavras H, Dailiana Z. Treatment of avascular necrosis of the femoral head with vascularized fibular transplant. Clin Orthop Relat Res. 2001;386:120–130. doi: 10.1097/00003086-200105000-00016. [DOI] [PubMed] [Google Scholar]
- 51.Steinberg ME, Hayken GD, Steinberg DR. A quantitative system for staging avascular necrosis. J Bone Joint Surg Br. 1995;77:34–41. [PubMed] [Google Scholar]
- 52.Steinberg ME, Larcom PG, Strafford B, Hosick WB, Corces A, Bands RE, Hartman KE. Core decompression with bone grafting for osteonecrosis of the femoral head. Clin Orthop Relat Res. 2001;386:71–78. doi: 10.1097/00003086-200105000-00009. [DOI] [PubMed] [Google Scholar]
- 53.Sugano N, Atsumi T, Ohzono K, Kubo T, Hotokebuchi T, Takaoka K. The 2001 revised criteria for diagnosis, classification, and staging of idiopathic osteonecrosis of the femoral head. J Orthop Sci. 2002;7:601–605. doi: 10.1007/s007760200108. [DOI] [PubMed] [Google Scholar]
- 54.Tsao AK, Roberson JR, Christie MJ, Dore DD, Heck DA, Robertson DD, Poggie RA. Biomechanical and clinical evaluations of a porous tantalum implant for the treatment of early-stage osteonecrosis. J Bone Joint Surg Am. 2005;87(Suppl 2):22–27. doi: 10.2106/JBJS.E.00490. [DOI] [PubMed] [Google Scholar]
- 55.Veillette CJ, Mehdian H, Schemitsch EH, McKee MD. Survivorship analysis and radiographic outcome following tantalum rod insertion for osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88(Suppl 3):48–55. doi: 10.2106/JBJS.F.00538. [DOI] [PubMed] [Google Scholar]
- 56.Wang BL, Sun W, Shi ZC, Zhang NF, Yue DB, Guo WS, Xu SQ, Lou JN, Li ZR. Treatment of nontraumatic osteonecrosis of the femoral head with the implantation of core decompression and concentrated autologous bone marrow containing mononuclear cells. Arch Orthop Trauma Surg. 2010;130:859–865. doi: 10.1007/s00402-009-0939-0. [DOI] [PubMed] [Google Scholar]
- 57.Wang Y, Chai W, Wang ZG, Zhou YG, Zhang GQ, Chen JY. Superelastic cage implantation: a new technique for treating osteonecrosis of the femoral head with mid-term follow-ups. J Arthroplasty. 2009;24:1006–1014. doi: 10.1016/j.arth.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 58.Wirtz DC, Rohrig H, Neuss M. Core decompression for avascular necrosis of the femoral head. Oper Orthop Traumatol. 2003;15:288–303. doi: 10.1007/s00064-003-1077-4. [DOI] [Google Scholar]
- 59.Wright JG. A practical guide to assigning levels of evidence. J Bone Joint Surg Am. 2007;89:1128–1130. doi: 10.2106/JBJS.F.01380. [DOI] [PubMed] [Google Scholar]
- 60.Yang S, Wu X, Xu W, Ye S, Liu X, Liu X. Structural augmentation with biomaterial-loaded allograft threaded cage for the treatment of femoral head osteonecrosis. J Arthroplasty. 2010;25:1223–1230. doi: 10.1016/j.arth.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 61.Yoo MC, Kim KI, Hahn CS, Parvizi J. Long-term followup of vascularized fibular grafting for femoral head necrosis. Clin Orthop Relat Res. 2008;466:1133–1140. doi: 10.1007/s11999-008-0204-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Yoon TR, Abbas AA, Hur CI, Cho SG, Lee JH. Modified transtrochanteric rotational osteotomy for femoral head osteonecrosis. Clin Orthop Relat Res. 2008;466:1110–1116. doi: 10.1007/s11999-008-0188-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Yoon TR, Song EK, Rowe SM, Park CH. Failure after core decompression in osteonecrosis of the femoral head. Int Orthop. 2001;24:316–318. doi: 10.1007/s002640000186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yuhan C, Hu CC, Chen DW, Ueng SW, Shih CH, Lee MS. Local cancellous bone grafting for osteonecrosis of the femoral head. Surg Innov. 2009;16:63–67. doi: 10.1177/1553350608330398. [DOI] [PubMed] [Google Scholar]
- 65.Zhao D, Wang B, Guo L, Yang L, Tian F. Will a vascularized greater trochanter graft preserve the necrotic femoral head? Clin Orthop Relat Res. 2010;468:1316–1324. doi: 10.1007/s11999-009-1159-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zhao D, Xu D, Wang W, Cui X. Iliac graft vascularization for femoral head osteonecrosis. Clin Orthop Relat Res. 2006;442:171–179. doi: 10.1097/01.blo.0000181490.31424.96. [DOI] [PubMed] [Google Scholar]