Abstract
Background
Intraarticular hip disease is commonly acknowledged as a cause of ipsilateral knee pain. However, this is based primarily on observational rather than high-quality evidence-based studies, and it is unclear whether ipsilateral knee pain improves when hip disease has been treated.
Questions/purposes
We asked whether (1) hip disease was associated with preoperative ipsilateral knee pain and (2) ipsilateral knee pain would improve after hip arthroplasty.
Patients and Methods
We retrospectively assessed knee pain in 255 patients who underwent hip arthroplasties between 2006 and 2008. The WOMAC pain score of each joint was the primary outcome measure, which was obtained prospectively before surgery and at 3 months and 1 year postoperatively. Of the 255 patients, 245 (96%) had followup data obtained at 3 months or 1 year.
Results
Preoperatively, ipsilateral knee pain was observed more frequently than contralateral knee pain (55% versus 18%). Preoperative ipsilateral knee pain scores were worse than contralateral knee pain scores (mean, 80 versus 95). Ipsilateral knee pain improved at 3 months and 1 year. When compared with the scores for contralateral knee pain at 3 months (95) and 1 year (96), there were no differences between knees.
Conclusions
Our observations suggest hip disease is associated with ipsilateral knee pain and that it improves after hip arthroplasty. This should be considered during preoperative evaluation for patients with hip and knee pain.
Level of Evidence
Level III, diagnostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Ipsilateral knee pain (IKP) is commonly associated with intraarticular hip disease [11, 14, 20, 21, 24, 26] and other sources of pain referred from the lumbar spine and pelvic area. Osteoarthritis (OA) of the knee is not an uncommon cause of IKP [28]. Referred pain to the knee from hip disease is particularly common in the pediatric population and has been identified as a cause for delayed diagnosis of hip problems such as developmental dysplasia of the hip, Perthes’ disease, slipped capital femoral epiphysis, septic arthritis, and others [14, 18, 27]. Others have reported a similar referred pain in adult patients with hip OA [8, 21, 24]. The accepted explanation of this phenomenon is that hips and knees get innervation from the femoral and obturator nerves. Additionally, there is a subgroup of patients with radiographic degenerative changes in both joints (ipsilateral hip and knee). In these patients, determining the primary source of the knee pain and treatment strategy can be challenging. Crockarell and Guyton argued knee surgery should be delayed until other possible sources of knee and leg pain are systematically excluded [9]. Patients also likely will be concerned regarding whether IKP will resolve after hip surgery. Although the notion of hip disease causing ipsilateral knee pain is widely accepted, this presumption is based primarily on observational studies rather than high-quality evidence.
We therefore asked whether (1) hip disease was associated with preoperative IKP, and (2) IKP would improve after hip arthroplasty.
Patients and Methods
Between November 2006 and November 2008, 415 hip reconstructions were performed at our center by the two surgeons (WM, JAG). All data were entered in an institutional review board-approved joint registry. We included patients undergoing unilateral elective hip reconstruction including primary and revision total THAs, metal-on-metal hip resurfacing (MOMHR), and conversion THA. We excluded 160 patients having bilateral hip reconstructions, ipsilateral or contralateral knee arthroplasty within 2 years, and lack of complete baseline data. This left 255 patients (61%) who fulfilled the inclusion criteria and were included in this study. Patients were predominantly male (143 of 255; 62%), with a mean age of 59 ± 15 years (range, 15–87 years), and a mean BMI of 28.8 ± 6.1 kg/m2. The majority of the patients were white (195, 76%), followed by black (23, 9%), Hispanic (16, 6%), Asian (four, 2%), and other (17, 7%). The primary preoperative diagnosis was OA (178; 70%), followed by osteonecrosis (31; 12%), implant loosening (18; 7%), dysplasia (13; 5%), and other (15; 6%). One hundred forty-two patients (56%) underwent primary THAs, 90 (35%) underwent MOMHR, 18 (7%) underwent revision THAs, and five (2%) underwent conversion THAs. The left hip was involved in 118 patients (46%) and the right hip was involved in 137 patients (54%).
Of the original 255 patients, 245 (96%) had at least one followup data point at 3 months or 1 year; 197 patients had 3-month (mean ± SD, 95 ± 28 days) data and 227 had 1-year (380 ± 40 days) data.
At the time of database enrollment, all patients completed a preoperative questionnaire containing WOMAC [4] outcome measures. The WOMAC is a self-administered health questionnaire. It has three subcomponents including pain, stiffness, and physical function [3, 4]; each subcomponent was validated individually and used in research studies [3, 4, 23]. WOMAC pain scores of bilateral hips and knees were collected for each patient (Table 1). Each item was scored using a five-point Likert scale, (extreme pain = 0, severe pain = 5, moderate pain = 10, mild pain = 15, no pain = 20), and aggregate scores for joint-specific pain with five items were calculated. A score for each joint was transformed to a range from 0 to 100 points, with a score of 100 indicating no pain. The WOMAC pain score was the primary outcome measure. IKP or contralateral knee pain (CKP) was defined as a WOMAC knee pain score less than 100. We did not routinely obtain knee imaging for patients having hip arthroplasties. Followup data (via patient-completed questionnaire) were collected at routine followups at 3 months and 1 year postoperatively. For patients who did not comply with routine followup schedules, data collection was accomplished via mail or telephone. Data collection and maintenance were performed using the Patient Analysis and Tracking System (PATS 4.0) software (Axis Clinical Software, Portland, OR, USA).
Table 1.
WOMAC pain score as assessed at our institution
| Location of pain | Level of pain | ||||
|---|---|---|---|---|---|
| Left hip pain walking on a flat surface? | None | Mild | Moderate | Severe | Extreme |
| Left hip pain up or down stairs? | None | Mild | Moderate | Severe | Extreme |
| Left hip pain at night in bed? | None | Mild | Moderate | Severe | Extreme |
| Left hip pain sitting or lying? | None | Mild | Moderate | Severe | Extreme |
| Left hip pain standing upright? | None | Mild | Moderate | Severe | Extreme |
| Right hip pain walking on a flat surface? | None | Mild | Moderate | Severe | Extreme |
| Right hip pain up or down stairs? | None | Mild | Moderate | Severe | Extreme |
| Right hip pain at night in bed? | None | Mild | Moderate | Severe | Extreme |
| Right hip pain sitting or lying? | None | Mild | Moderate | Severe | Extreme |
| Right hip pain standing upright? | None | Mild | Moderate | Severe | Extreme |
| Left knee pain walking on a flat surface? | None | Mild | Moderate | Severe | Extreme |
| Left knee pain up or down stairs? | None | Mild | Moderate | Severe | Extreme |
| Left knee pain at night in bed? | None | Mild | Moderate | Severe | Extreme |
| Left knee pain sitting or lying? | None | Mild | Moderate | Severe | Extreme |
| Left knee pain standing upright? | None | Mild | Moderate | Severe | Extreme |
| Right knee pain walking on a flat surface? | None | Mild | Moderate | Severe | Extreme |
| Right knee pain up or down stairs? | None | Mild | Moderate | Severe | Extreme |
| Right knee pain at night in bed? | None | Mild | Moderate | Severe | Extreme |
| Right knee pain sitting or lying? | None | Mild | Moderate | Severe | Extreme |
| Right knee pain standing upright? | None | Mild | Moderate | Severe | Extreme |
We used a paired t-test to determine the differences in WOMAC pain scores between preoperative IKP and preoperative CKP, preoperative IKP and postoperative IKP, and postoperative IKP and postoperative CKP respectively. Chi square was used to determine the differences in the percentages between reported IKP and CKP preoperatively, and at 3 months and 1 year postoperatively. The t-test and chi square test were performed using Microsoft Office Excel 2007 (Microsoft Corporation, Redmond, WA, USA) and SAS 9.1 software (SAS Institute, Cary, NC, USA) respectively. When performing the paired t-test, patients with incomplete data were not included.
Results
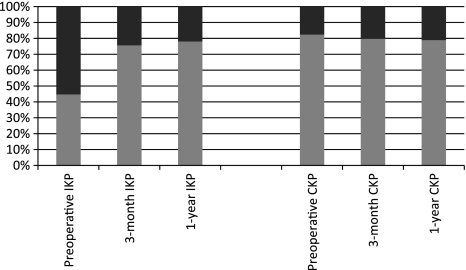
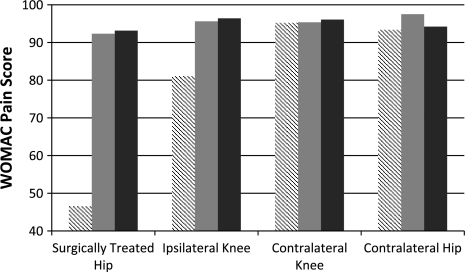
Preoperatively, 141 of 255 patients (55%) reported IKP, which occurred more frequently (p < 0.001) than CKP (45 of 255; 18%) (Fig. 1). Preoperatively, the mean ipsilateral knee WOMAC pain scores (80 ± 27) were lower (p < 0.001) than those reported for the contralateral side (95 ± 15) (Fig. 2).
Fig. 1.
The percentages of ipsilateral knee pain (IKP) and contralateral knee pain (CKP) preoperatively and at 3 months and 1 year postoperatively are shown. Preoperatively, 141 of 255 patients (55%) had IKP, which occurred more frequently than CKP (45 of 255; 18%). At 3 months postoperatively, 48 of 197 patients (24%) had IKP, which was similar to the rate of CKP (40 of 197; 20%). At 1 year, 50 of 227 patients (22%) had IKP, which also was similar to the rate for CKP (48 of 227; 21%). Black = reported pain; gray = no pain.
Fig. 2.
A graph shows improvement in the joint-specific WOMAC pain score from preoperatively to 3 months and 1 year postoperatively. Preoperatively, ipsilateral knee WOMAC pain scores (80 ± 27) were lower than those for the contralateral side (95 ± 15). Postoperatively, ipsilateral knee WOMAC pain scores improved to 96 ± 12 and 96 ± 13 at 3 months and 1 year, respectively. When compared with the contralateral WOMAC knee pain scores at 3 months (96 ± 14) and 1 year (96 ± 12), there were no differences between knees. Preoperatively, the WOMAC hip pain score for the entire cohort was 44 ± 23, which improved to 92 ± 14 and 92 ± 16 at 3 months and 1 year, respectively. The WOMAC pain scores for the contralateral hip and knee did not change. Hatched bar = preoperative; gray bar = 3 months; black bar = 1 year.
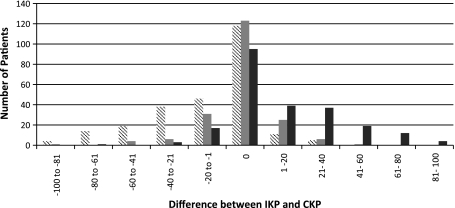
At 3 months postoperatively, 24% reported IKP, which was similar (p = 0.33) to the 20% rate for patients with CKP. At 1 year, 22% reported IKP, which also was similar (p = 0.82) to the 21% rate reported for CKP (Fig. 1). Postoperatively, ipsilateral knee WOMAC pain scores improved (p < 0.001) to 96 ± 12 and 96 ± 13 at 3 months and 1 year, respectively (Fig. 2). When compared with the contralateral WOMAC knee pain scores at 3 months (96 ± 14) and 1 year (96 ± 12), there were no differences between knees (p = 0.84 and p = 0.87, respectively). We observed no differences (p = 0.102) among subgroups of patients with different diagnoses. At 3 months and 1 year, the reported IKP and CKP were similar for patient number and severity (Fig. 3).
Fig. 3.
A graph shows the differences between ipsilateral knee pain (IKP) preoperatively and at 3 months and 1 year postoperatively. Before hip reconstruction, the ipsilateral knee WOMAC pain score was worse than that of the contralateral knee (CKP) in 121 patients (48%); it was the same in 118 patients (46%), but better than that of the contralateral knee for only 16 patients (6%). At 3 months, 31 of 197 patients (16%) had an ipsilateral knee WOMAC pain score worse than that of the contralateral side, 139 (70%) had the same score, and 27 (14%) had a score less than that of the contralateral side. At 1 year, 32 of 227 patients (14%) had ipsilateral knee WOMAC pain scores worse than those of the contralateral side, 171 patients (75%) had the same scores, and 24 patients (11%) had scores less than those of the contralateral knee. Hatched bar = preoperative; gray bar = 3 months; black bar = 1 year.
Discussion
Although widely understood that intraarticular hip disease is a potential cause for IKP, no high-quality evidence-based study has documented this association in adults or documented the pattern of improvement when the hip disease has been treated. Most previous studies have been case reports [8, 10–13, 15, 16]. Only several observational reports describe the distribution of the referral pain of hip disease [21, 24, 32]. We therefore asked: (1) if hip disease was associated with preoperative IKP and (2) does IKP improve after hip arthroplasty?
We note limitations to our study. First is the use of a retrospective study design. However, all data in our study were collected prospectively; therefore, recall bias has been avoided. Second, 98 patients who did not give consent to be enrolled in the database were excluded; this potentially could cause selection bias. Third, 62 patients who had multiple surgeries were excluded to eliminate patients whose source of CKP might be unclear and create a more homogeneous population. There also is some selection bias in that all patients had hip disease sufficiently severe to warrant THA, and therefore might not reflect a population with less severe disease. Fourth, we used the WOMAC pain score as the only way to assess pain. However, the WOMAC pain score is a reliable and valid instrument that has been used extensively to measure disability of patients with hip and knee OA [3, 4]. It is patient-centric and self-reported, helping to minimize researcher bias. Fifth, we had a short followup period. We chose 3 months and 1 year based on the length of time we expected hip arthroplasty to affect a change in perceived pain and return patients to their highest anticipated function without waiting long enough to witness progression of OA in other joints. Some authors have reported OA might develop or deteriorate at other joints within 5 years after unilateral THA [25, 30, 31]; therefore, we studied pain at 3 months and 1 year postoperatively. Because contralateral hip and CKP scores remained constant during our relatively short study period, OA did not seem to develop or progress. Sixth, we did not routinely obtain imaging of the knee, even in patients with symptoms, therefore, we cannot evaluate the effect of knee disease on knee pain.
We found IKP is common in patients who have end-stage hip disease. Our observations suggest 55% of our patients undergoing hip arthroplasties had IKP, which was high compared with 17.6% for the contralateral knee. Khan et al. [21] suggested a similar phenomenon with 68.6% and 50.9% of patients scheduled to undergo hip arthroplasties reporting anterior and posterior knee pain, respectively, before surgery. Although IKP is frequent in patients with severe hip disease, the direct cause remains unknown.
One possible explanation for this finding is that OA in the ipsilateral knee may play a role. Knee and hip OA reportedly occur concurrently in approximately 30% of patients [4]. However, we found IKP improved without any treatment for the ipsilateral knee. Another possible explanation for relief of pain is that gait change after the hip arthroplasty might play a role in the dissolution of IKP. However, in a weightbearing study, an alteration in functional movement patterns was observed in patients with OA, which was characterized by compensation to reduce loading of the affected limb [6]. After hip arthroplasty, patients tend to increase use of the ipsilateral knee for ambulation [29]. Therefore the pressure in the ipsilateral knee will increase, which cannot explain the improvement of the IKP. Although referred IKP has been studied in the pediatric population [34], numerous case reports and qualitative studies report an association of hip disease and IKP in adults [8, 10–13, 15, 16, 20, 21, 24] (Table 2). In one study, Lesher et al. [24] reported pain from hip disease could refer to the groin, thigh, buttock, knee, leg, and foot. In another study, Street et al. [33] reported preoperative pain referral patterns of hip arthritis affect patient outcome and satisfaction after THA. Crawford et al. [7, 8] used intraarticular injection of local anesthetics to the hip to study the pattern of referred hip pain and believed it was a simple and useful method to clarify if the hip is the source of pain and the knee pain is relieved after injection to the hip. However, their patient population represented less than 1% of all patients in their arthroplasty unit [7, 8]. Furthermore, routinely injecting intraarticular anesthetics is neither practical nor necessary. As such, it may be difficult to adopt this method to study referred IKP in the general population of patients with hip disease. However, as with these reports, all previous studies attempt to show the pattern of referral pain without quantitatively evaluating IKP before and after treatment of the problem. Tracking both knee outcomes after hip arthroplasty, our study shows reported IKP improved from baselines of 80 ± 27 to 96 ± 12 and 96 ± 13 at 3 months and 1 year, respectively, to plateau at comparable levels to the contralateral knee. Fully understanding this phenomenon is critical for clinical practice and patient care.
Table 2.
Review of the literature
| Study | Number of cases | Quantity evaluation of IKP | Diagnosis | Symptoms | Followup after treatment |
|---|---|---|---|---|---|
| Crawford et al. [8] | 1 | No | OA | No hip pain, only IKP | Knee pain relieved after injection to hip |
| Emms et al. [10] | 1 | No | OA | No hip pain, only IKP | Knee pain relieved after injection to hip, and THA |
| Flatman [12] | 1 | No | Tuberculosis | No hip pain, only IKP | No treatment |
| Guss [13] | 1 | No | Hip fracture | No hip pain, only IKP | Pain relieved after THA |
| Hammer [15] | 1 | No | Hip fracture | No hip pain, only IKP | Hemiarthroplasty, pain relieved |
| Hetsroni & Weigl [16] | 1 | No | Posterior hip dislocation | Hip and knee pain | Closed reduction, pain relieved |
| Khan et al. [21] | 60 | No | OA | 68.6% had anterior knee pain, 50.9% had posterior knee pain | No treatment |
| Lesher et al. [24] | 51 | No | Awaiting hip arthroplasty, no details | Most common site is buttock, 2% to the knee | Pain relieved after injection to the hip |
| Street et al. [33] | 236 | No | Awaiting hip arthroplasty, no details | 32% had IKP | No IKP data after hip arthroplasty |
| Current study | 255 | Yes | OA, osteonecrosis, implant loosening, dysplasia, other | 55.3% had IKP which is more than CKP (17.6%), IKP score (79.7) is lower than CKP score (94.8). | IKP improved after hip arthroplasty to the same level of the CKP |
IKP = ipsilateral knee pain; CKP = contralateral knee pain; OA = osteoarthritis.
It seems plausible referred pain from hip disease plays a central role in IKP. Referred pain is a term used to describe the phenomenon of pain perceived at a site adjacent to or distant from the site of an injury’s origin. Physicians have known about referred pain since at least the late 1860s [17]. However the true mechanism of referred pain remains unknown. Although there are several proposed mechanisms for referred pain, there currently is no definitive consensus. The most widely accepted explanation of referred pain is Ruch’s convergence-projection theory [32]. Deep structures, such as the hip, although sparsely innervated, send off afferent neurons that converge on spinothalamic cells, which also receive impulses from segmentally innervated somatic structures, eg, cutaneous pain receptors. The spinothalamic tract is more commonly innervated by these somatic structures, and the brain begins to associate activity in the spinothalamic tract with the cutaneous receptors. Therefore, when deep afferents activate the spinothalamic tract, the brain misinterprets the message and mislocalizes the source of activity to the cutaneous region [12]. The hip is innervated by branches of the femoral nerve, obturator nerve, sciatic nerve, accessory obturator nerve, and the nerve to the quadratus femoris and inferior gemellus, of which the femoral and obturator nerves contribute the majority of sensation. These two nerves, derived from lumbar nerve roots 2, 3, and 4 [5, 19, 22], have dermatomal sensory distributions that include the groin, medial thigh, knee, leg, and foot. This pattern of distribution may be the link that results in hip disease giving rise to referred pain to the ipsilateral knee. Identifying and treating the source of concurrent hip and knee pain can be difficult. Not only do a majority of patients with hip OA report preoperative IKP but 30% to 40% of patients with knee OA have concomitant hip OA [28]. Diagnosis of hip and knee OA should not be based on radiographs alone as many patients have symptoms of hip and knee OA early in its course without radiographic changes and 40% of patients with typical radiographic changes may be asymptomatic [1, 2]. In all such cases, diagnosis and treatment can be challenging. We recommend a thorough physical examination of the knees, hips, posterior pelvis, and lumbar spine, when examining patients reporting hip or knee pain. For controversial cases, further radiographic evaluation of the hips and knees should be performed. If the symptoms can be explained by hip disease, we give consideration to treating the hip first, with careful followup on the ipsilateral knee after surgery. If the source of pain cannot be identified, we consider injection of an intraarticular local anesthetic. Among patients who have preoperative IKP, we found the IKP improved after hip surgery in approximately 90% of patients without any specific treatment of the knee (89% and 91% at 3 months and 1 year respectively).
Acknowledgments
We thank Todd Morrison and Leslie Fink MD for help with data collection.
Footnotes
One of the authors (WW) received funding from the Orthopaedic Research and Education Foundation (OREF).
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Altman R, Alarcón G, Appelrouth D, Bloch D, Borenstein D, Brandt K, Brown C, Cooke TD, Daniel W, Feldman D, et al. The American College of Rheumatology criteria for the classification and reporting of osteoarthritis of the hip. Arthritis Rheum. 1991;34:505–514. doi: 10.1002/art.1780340502. [DOI] [PubMed] [Google Scholar]
- 2.Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, Christy W, Cooke TD, Greenwald R, Hochberg M, et al. Development of criteria for the classification and reporting of osteoarthritis: classification of osteoarthritis of the knee. Diagnostic and Therapeutic Criteria Committee of the American Rheumatism Association. Arthritis Rheum. 1986;29:1039–1049. doi: 10.1002/art.1780290816. [DOI] [PubMed] [Google Scholar]
- 3.Bellamy N. WOMAC: a 20-year experiential review of a patient-centered self-reported health status questionnaire. J Rheumatol. 2002;29:2473–2476. [PubMed] [Google Scholar]
- 4.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 5.Birnbaum K, Prescher A, Hessler S, Heller KD. The sensory innervation of the hip joint: an anatomical study. Surg Radiol Anat. 1997;19:371–375. doi: 10.1007/BF01628504. [DOI] [PubMed] [Google Scholar]
- 6.Christiansen CL, Stevens-Lapsley JE. Weight-bearing asymmetry in relation to measures of impairment and functional mobility for people with knee osteoarthritis. Arch Phys Med Rehabil. 2010;91:1524–1528. doi: 10.1016/j.apmr.2010.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Crawford RW, Ellis AM, Gie GA, Ling RS. Intra-articular local anaesthesia for pain after hip arthroplasty. J Bone Joint Surg Br. 1997;79:796–800. doi: 10.1302/0301-620X.79B5.7644. [DOI] [PubMed] [Google Scholar]
- 8.Crawford RW, Gie GA, Ling RS, Murray DW. Diagnostic value of intra-articular anaesthetic in primary osteoarthritis of the hip. J Bone Joint Surg Br. 1998;80:279–281. doi: 10.1302/0301-620X.80B2.8299. [DOI] [PubMed] [Google Scholar]
- 9.Crockarell JR, Guyton JL. Arthroplasty of the knee. In: Canale ST, Beaty JH, eds. Campbell’s Operative Orthopaedics. Philadelphia, PA: Mosby Elsevier; 2008:241–313.
- 10.Emms NW, O’Connor M, Montgomery SC. Hip pathology can masquerade as knee pain in adults. Age Ageing. 2002;31:67–69. doi: 10.1093/ageing/31.1.67. [DOI] [PubMed] [Google Scholar]
- 11.Flatman JG. Hip diseases with referred pain to the knee. JAMA. 1975;234:967–968. doi: 10.1001/jama.1975.03260220071028. [DOI] [PubMed] [Google Scholar]
- 12.Gannon JM, Gustilo RB. Treat the hip and not the knee: a report of four cases. Orthopedics. 1992;15:474–477. doi: 10.3928/0147-7447-19920401-13. [DOI] [PubMed] [Google Scholar]
- 13.Guss DA. Hip fracture presenting as isolated knee pain. Ann Emerg Med. 1997;29:418–420. doi: 10.1016/S0196-0644(97)70357-3. [DOI] [PubMed] [Google Scholar]
- 14.Hamer AJ. Pain in the hip and knee. BMJ. 2004;328:1067–1069. doi: 10.1136/bmj.328.7447.1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammer SG. Hip fracture presenting as knee pain in an elderly patient. Am Fam Physician. 1996;54:872. [PubMed] [Google Scholar]
- 16.Hetsroni I, Weigl D. Referred knee pain in posterior dislocation of the hip. Clin Pediatr (Phila) 2006;45:93–95. doi: 10.1177/000992280604500117. [DOI] [PubMed] [Google Scholar]
- 17.Hilton J. The Classic: On rest and pain: Lecture XIV. Clin Orthop Relat Res. 2009;467:2208–2214. doi: 10.1007/s11999-009-0928-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hodges DL, McGuire TJ. Hip pain in children: an anatomic approach. Orthop Rev. 1988;17:251–256. [PubMed] [Google Scholar]
- 19.Hodges DL, McGuire TJ, Kumar VN. Diagnosis of hip pain: an anatomic approach. Orthop Rev. 1987;16:109–113. [PubMed] [Google Scholar]
- 20.Johnson EW. Location of hip pain. JAMA. 1979;242:1849. doi: 10.1001/jama.1979.03300170015012. [DOI] [PubMed] [Google Scholar]
- 21.Khan AM, McLoughlin E, Giannakas K, Hutchinson C, Andrew JG. Hip osteoarthritis: where is the pain? Ann R Coll Surg Engl. 2004;86:119–121. doi: 10.1308/003588404322827518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khan NQ, Woolson ST. Referral patterns of hip pain in patients undergoing total hip replacement. Orthopedics. 1998;21:123–126. doi: 10.3928/0147-7447-19980201-05. [DOI] [PubMed] [Google Scholar]
- 23.Lavernia CJ, Alcerro JC, Contreras JS, Rossi MD. Patient perceived outcomes after primary hip arthroplasty: does gender matter? Clin Orthop Relat Res. 2011;469:348–354. doi: 10.1007/s11999-010-1503-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lesher JM, Dreyfuss P, Hager N, Kaplan M, Furman M. Hip joint pain referral patterns: a descriptive study. Pain Med. 2008;9:22–25. doi: 10.1111/j.1526-4637.2006.00153.x. [DOI] [PubMed] [Google Scholar]
- 25.Mont MA, Mitzner DL, Jones LC, Hungerford DS. History of the contralateral knee after primary knee arthroplasty for osteoarthritis. Clin Orthop Relat Res. 1995;321:145–150. [PubMed] [Google Scholar]
- 26.Murtagh J. Hip and buttock pain in adults. Aust Fam Physician. 1992;21:848–853. [PubMed] [Google Scholar]
- 27.Murtagh J. Hip pain in children. Aust Fam Physician. 1992;21:1018–1021. [PubMed] [Google Scholar]
- 28.O’Reilly SC, Muir KR, Doherty M. Occupation and knee pain: a community study. Osteoarthritis Cartilage. 2000;8:78–81. doi: 10.1053/joca.1999.0274. [DOI] [PubMed] [Google Scholar]
- 29.Otsuki T, Nawata K, Okuno M. Quantitative evaluation of gait pattern in patients with osteoarthrosis of the knee before and after total knee arthroplasty: gait analysis using a pressure measuring system. J Orthop Sci. 1999;4:99–105. doi: 10.1007/s007760050081. [DOI] [PubMed] [Google Scholar]
- 30.Ritter MA, Carr K, Herbst SA, Eizember LE, Keating EM, Faris PM, Meding JB. Outcome of the contralateral hip following total hip arthroplasty for osteoarthritis. J Arthroplasty. 1996;11:242–246. doi: 10.1016/S0883-5403(96)80073-8. [DOI] [PubMed] [Google Scholar]
- 31.Ritter MA, Carr KD, Keating EM, Faris PM. Long-term outcomes of contralateral knees after unilateral total knee arthroplasty for osteoarthritis. J Arthroplasty. 1994;9:347–349. doi: 10.1016/0883-5403(94)90043-4. [DOI] [PubMed] [Google Scholar]
- 32.Ruch TC. Pathophysiology of pain. In: Ruch TC, Patton HD, eds. Physiology and Biophysics. Philadelphia, PA: Saunders; 1965:345–363.
- 33.Street J, Lenehan B, Flavin R, Beale E, Murray P. Do pain referral patterns determine patient outcome after total hip arthroplasty? Acta Orthop Belg. 2005;71:540–547. [PubMed] [Google Scholar]
- 34.Sty JR, Wells RG, Smith WB. The child with acute leg pain. Semin Nucl Med. 1988;18:137–158. doi: 10.1016/S0001-2998(88)80006-0. [DOI] [PubMed] [Google Scholar]