Abstract
Background
Severe medial and/or superior defects encountered in revision THA are currently managed with jumbo (≥ 66 mm) acetabular components and modular augments, with reconstruction cages, or with the cup-cage technique. Preoperative planning can indicate when these techniques may not restore vertical and horizontal offset. Failure to restore offset can lead to impingement, leg length inequality, abductor weakness, and dislocation.
Surgical Technique
We developed a “cup-in-cup” technique in which a porous tantalum acetabular shell was impacted into supportive medial host bone. A second tantalum shell was then cemented in, and this shell’s diameter could be selected based on preoperative planning to achieve restoration of horizontal and vertical offset.
Patients and Methods
We implanted porous tantalum hemispheric shells in seven patients undergoing eight revision THAs. The average age was 73 years at the time of the procedure. Preoperative defects per the classification of Paprosky et al. were three IIC, four IIIA, and one IIIB. All patients were followed clinically and radiographically for a minimum of 12 months (average, 28 months; range, 12–50 months).
Results
Abductor strength was either improved by one grade (four hips) or unchanged (four hips). Horizontal offset was increased an average of 10.5 mm (range, 8–16 mm), and vertical offset improved by an average of 18.4 mm (range, 10–29 mm). There was no evidence of loosening or migration at the time of final followup.
Conclusions
At short-term followup, the early experience cautiously supports the use of this construct. Long-term followup and a larger patient experience will be required to determine the durability of this novel technique.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Severe protrusio defects in revision THA present several reconstruction challenges. The strategies employed for treatment have been aided by the classification of Paprosky et al. [14] (Table 1). For smaller medial protrusio Paprosky IIC defects, the use of medially morselized allograft or small structural allograft, or more recently porous augments, combined with a deep-profile acetabular component, can allow restoration of horizontal offset. For more severe IIC defects, these methods may not allow restoration of horizontal offset, possibly resulting in bony impingement. For more severe defects that combine vertical and medial bone loss (Paprosky IIIA), treatment options have included oblong acetabular components [3, 5], use of bulk allograft with a cemented acetabular component, and more recently the combination of jumbo acetabular components cemented to structural porous augments [15, 17]. For Paprosky IIIB defects, these same techniques have been described [17], as well as the use of reconstruction cages [10], custom triflange components [4], and more recently the cup-cage construct described by Nehme et al. [13].
Table 1.
Classification of Paprosky et al. [14]
| Paprosky type | Acetabular rim | Anterior and posterior columns | Osteolysis | Component migration (from original position) | Bony defect | Kohler’s line |
|---|---|---|---|---|---|---|
| I | Intact, supportive | Intact | None | None | Minimal | Intact |
| IIA | Distorted | Intact | Minimal ischial and teardrop | Directly superior < 2 cm | Cavitation of dome, intact superior rim | Intact |
| IIB | Distorted | Intact | Minimal ischial and teardrop | Superolateral migration < 2 cm | Superior rim absent | Intact |
| IIC | Distorted | Intact | Minimal ischial and teardrop | Medial | Destruction of medial wall | Disrupted |
| IIIA | Major destruction | Nonsupportive | Moderate ischial and teardrop | Superior migration > 2 cm | Severe bone loss | Intact |
| IIIB | Major destruction | Nonsupportive | Severe ischial lysis, no teardrop | Superior (and medial) migration > 2 cm | Severe bone loss, possible pelvic discontinuity | Disrupted |
Cementation of a liner into an existing acetabular component in revision hip surgery is an accepted technique. At a mean followup of 5.1 years, no liner debonding has occurred [2]. Mechanical testing has confirmed the strength of this construct compared to a conventional locking mechanism [10].
Fixation of a modern highly porous acetabular component on host bone, if initial stability can be obtained, should result in osseointegration. Cementation of a second modular highly porous acetabular component into this component should allow restoration of horizontal offset or horizontal and vertical offset. The second component may be placed in acceptable component version and allows placement of a modular liner. In certain circumstances, this construct may be preferable to the use of a nonmodular or a “modular” oblong acetabular component (hemispherical shell with porous augments) as the former may increase the area of contact of the porous material against host bone. For severe IIIA and IIIB defects, this construct could possibly exceed the reported lifespan of a reconstruction cage [16].
We describe the surgical technique and initial results of a novel reconstructive method that requires stable placement of a porous tantalum jumbo acetabular component with adjunctive screw fixation into viable host bone, combined with cementation of a similar tantalum porous acetabular component into the initial shell and placement of a modular liner.
Surgical Technique
The indications for this approach were (1) severe medial (Paprosky IIC) defects, (2) severe medial and superior defects (Paprosky IIIA, IIIB), or (3) severe superior defects (Paprosky IIIA, IIIB) not amenable to previously described techniques (jumbo cups with or without augments, reconstruction cages, cup-cage construct) due to inability to restore offset. The contraindications were (1) ability to reconstruct the deficient acetabulum with the previously described techniques and (2) inability to obtain a stable press-fit of the medial or inner acetabular shell on supportive and adequate bone (estimated 50% or more host bone contact). In all cases, the decision to utilize the described construct was considered as a part of preoperative planning. If the surgeon believed a successful near-anatomic reconstruction of the joint center with a megacup (defined as ≥66 mm) was not likely based on the preoperative radiographs, in addition to planning for the availability of modular augments and reconstruction cages, the surgeon estimated the placement of the inner medial tantalum shell. This was marked on the radiograph, the second lateral shell position was then marked, and determination of the proposed joint center was made. If this allowed restoration of a near-anatomic joint center without excessive lateralization, the technique was preoperatively considered.
A posterolateral approach was used. At the time of surgery, the intraoperative determination to use the cup-in-cup construct was made based on the following factors: determination that insufficient lateral host bone existed to achieve both a near-anatomic placement and adequate stability of a porous megacup with or without augments and that enough medial host bone existed to attempt placement of a tantalum cup. If at any time in the bony preparation the available medial bone was not believed to be either sufficient or supportive or both, this technique was not utilized. Before reaming, an initial trial of the proposed cup-in-cup construct could be made by placement of a larger medial trial shell combined with a smaller lateral trial shell and a trial liner and a careful attempt made at reduction of the hip.
The IIC and IIIA cases were prepared with line-to-line reaming, placement of particulate allograft to fill cavitary defects, and insertion of a jumbo porous tantalum shell (Trabecular Metal® revision shell; Zimmer, Inc, Warsaw, IN). For the IIIB defect, 4 mm underreaming was utilized followed by impaction of the porous shell (Fig. 1). In all cases, the acetabular component had to obtain initial stability against host bone, defined as the ability of the untouched shell to remain in the impacted position during removal of the impaction handle. Adjunctive screw fixation (mean 2.6; range, 1–4) was used in all cases. A smaller trial acetabular component and liner were then placed and used to assess the following variables: the ability to reduce the joint without causing excessive soft tissue tightness or difficulty with fascial closure; sciatic nerve tension; and relative component positioning based on the use of Ranawat’s sign [12]. A second tantalum component usually smaller in diameter by 6 to 10 mm (in one case, implants of the same size were used) was then cemented in. In two cases, secondary to abductor insufficiency, a constrained liner was used, and in two cases, a bipolar head was placed over a nonmodular femoral component (Table 2).
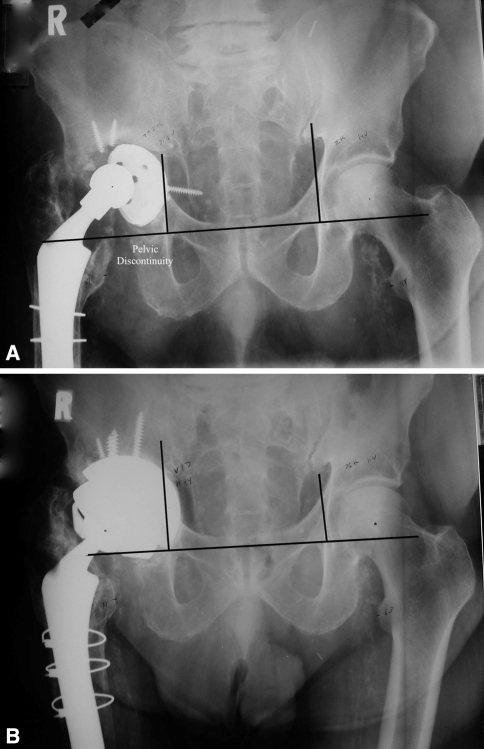
Fig. 1A–B.
(A) A Paprosky IIIB defect is seen. Note the heterotopic ossification superior to the greater trochanter and the well-fixed cementless femoral component. (B) At 4-year followup, the implants are stable. Vertical offset has been restored compared to the contralateral normal joint. Horizontal offset has been increased.
Table 2.
Implants used
| Patient | Paprosky type | Medial shell (mm) | Lateral shell (mm) | Allograft bone (mL) | Liner used |
|---|---|---|---|---|---|
| 1 | IIC | 80 | 74 | 120 | Constrained |
| 2 | IIC | 76 | 68 | 90 | 10° |
| 3 | IIC | 72 | 66 | 90 | Constrained |
| 4 | IIIA | 64 | 64 | 90 | 10° |
| 5 | IIIA | 70 | 60 | 30 | Neutral |
| 6 | |||||
| Right | IIIA | 68 | 58 | 45 | Bipolar |
| Left | IIIA | 68 | 58 | 30 | Bipolar |
| 7 | IIIB | 80 | 70 | 90 | Constrained |
Postoperatively, patients were instructed in the use of a walker to limit weightbearing to 10% for the first 12 weeks and 50% for the next 12 weeks; then advancement to full weightbearing was allowed. At the 6-week followup, gentle stretching exercises were started, and at 12 weeks, active straight-leg raising and abduction exercises were begun. No patient attended formal physical therapy.
Patients and Methods
From August 2006 to March 2010, seven patients (one bilateral) with an average age of 73 years at the time of the procedure underwent eight isolated acetabular reconstructions for severe bony defects using porous tantalum acetabular components (Table 3). Three patients (four hips) had mild pain, one had moderate pain, and three had severe pain. Five patients (six hips) walked fewer than two blocks, all requiring assistive devices; one patient walked two to three blocks using two crutches; and two patients walked an unlimited distance using a cane. All surgical procedures were performed by the authors. All patients were followed clinically and radiographically for a minimum of 12 months (average, 28 months; range, 12–50 months). No patients were lost to followup. Per our Institutional Review Board, approval is not required for case reports. We have contacted the patients, however, and they have given consent for submission.
Table 3.
Patient demographics
| Patient | Age (years) | Gender | Height (inches) | Weight (pounds) | Initial diagnosis | Prior surgeries |
|---|---|---|---|---|---|---|
| 1 | 83 | Male | 74 | 185 | Posttraumatic osteoarthritis | 1971 cup arthroplasty, 1971 revision cup arthroplasty, 1981 THA, 1989 revision THA |
| 2 | 77 | Male | 70 | 186 | Osteoarthritis | 1977 THA, revision THA × 3 (1979, early 1990s, 2005) |
| 3 | 71 | Male | 68 | 200 | Osteonecrosis | 1965 hemiarthroplasty, 1973 bilateral THAs, 1992 bilateral revision THAs |
| 4 | 87 | Male | 68 | 197 | Osteoarthritis | 1989 THA |
| 5 | 57 | Male | 63 | 200 | Osteonecrosis | 2006 THA, 2007 revision THA (acetabulum) |
| 6 | 60 | Male | 73 | 305 | Posttraumatic osteoarthritis | 1978 bilateral THAs |
| 7 | 75 | Male | 67 | 201 | Posttraumatic osteoarthritis | 1977 hemiarthroplasty, THA, 1988 revision THA, 1996 revision THA |
Acetabular bone loss was classified according to the criteria of Paprosky et al. [14]. On the basis of preoperative and intraoperative assessment, there were three Paprosky IIC, four Paprosky IIIA, and one Paprosky IIIB defect reconstructions.
All patients were followed prospectively at 6 weeks, 3 months, 6 months, and 12 months postoperatively and annually thereafter. Harris hip scores (HHSs) were obtained at each visit. Abduction strength, tested with the patients lying on their side (graded 1–5), was initially tested at the 3-month visit and at scheduled followups.
Preoperative and postoperative standardized radiographs taken at each followup visit (AP pelvis, AP and table down lateral with magnification markers) were assessed for evidence of component migration, initial and progressive radiolucencies [6], and change in the prosthetic head center. Migration was assessed as a change in head center position when comparing the initial 6-week AP pelvis to the latest AP pelvis. The head center was measured according to the method of DeBoer and Christie [5]. After the interteardrop line was drawn on the preoperative AP pelvis, a vertical perpendicular line was drawn at the intersection of the teardrop line and the ilioischial line. On the operative side, a vertical measurement with a magnified ruler was made from the interteardrop line to the prosthetic head center and was recorded as vertical offset; a horizontal measurement was then made from the ilioischial line to the prosthetic head center and recorded as horizontal offset. We defined an improvement or decrease in the vertical offset pre- to postsurgery (describing the joint center moving closer to the interteardrop line) as a negative (−) number; similarly, an improvement or increase in the horizontal offset, representing joint center lateralization, was a positive (+) number. If we could not visualize the teardrop, then we marked out the most superior lateral point seen on both obturators. For the patient with bilateral failed THAs (IIIA), the deviations were measured as follows: after drawing the above lines, the current prosthetic head center was measured as above. Postoperative measurements were made in a similar fashion and recorded.
Results
The preoperative HHS was 51 (range, 30–71) and improved at latest followup to 78 (range, 52–94), a mean improvement of 27 points. At latest followup, six patients (seven hips) had no pain and one patient had mild pain. Four patients (five hips) improved in ambulatory distance after surgery, one patient noted no change, and two patients walked less (due to worsening of underlying medical conditions; HHS, 52 and 62). Pre- to postoperative abductor function improved by one grade in four hips and was unchanged in four hips.
Horizontal offset was increased an average of +10 mm (range, 8–16 mm), and vertical offset decreased by an average of −18.4 mm (range, 10–29 mm) (Table 4). Average abduction was 43° (range, 29°–50°) for the inner (medial) shell and 43° (range, 34°–49°) for the outer shell. In only one case was the measured abduction angle the same for both shells.
Table 4.
Joint center pre- to postrevision
| Patient | Paprosky type | Joint center vertical (mm) | Joint center horizontal (mm) | Contralateral normal hip | |||||
|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Change (− = inferior) | Preoperative | Postoperative | Change (+ = lateral) | Joint center vertical (mm) | Joint center horizontal (mm) | ||
| 1 | IIC | 30 | 18.5 | −11.5 | 35 | 43 | +8 | 14 | 37 |
| 2 | IIC | 19 | 9 | −10 | 39 | 47 | +8 | 9 | 42 |
| 3 | IIC | 35 | 20 | −15 | 34 | 47 | +13 | NA | NA |
| 4 | IIIA | 38 | 7 | −21 | 40 | 50 | +10 | NA | NA |
| 5 | IIIA | 48 | 19 | −29 | 33 | 41 | +8 | NA | NA |
| 6 | |||||||||
| Right | IIIA | 37 | 18 | −19 | 28 | 44 | +16 | NA | NA |
| Left | IIIA | 42 | 19 | −23 | 39 | 54 | +15 | NA | NA |
| 7 | IIIB | 36 | 17 | −19 | 38 | 44 | +6 | 14 | 36 |
NA = not available.
At latest followup, there was no evidence for component migration as compared to the initial postoperative views (Fig. 2). In two cases, there were less than 1 mm radiolucencies seen in Zone C at latest followup (Fig. 3). At the time of surgery, all femoral components were retained, and none showed any radiographic changes at the time of latest followup.
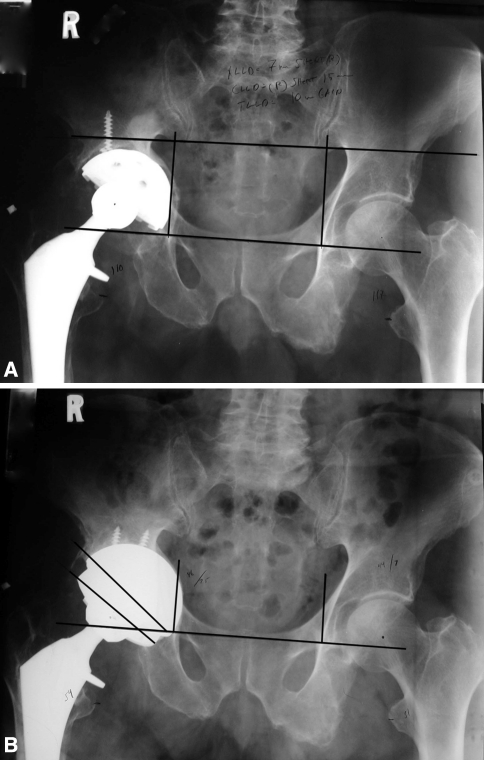
Fig. 2A–B.
(A) A Paprosky IIC defect is seen. The medial wall has remodeled. The inferior to superior distance is too great for a megacup. (B) Postoperatively, the joint center is anatomic.
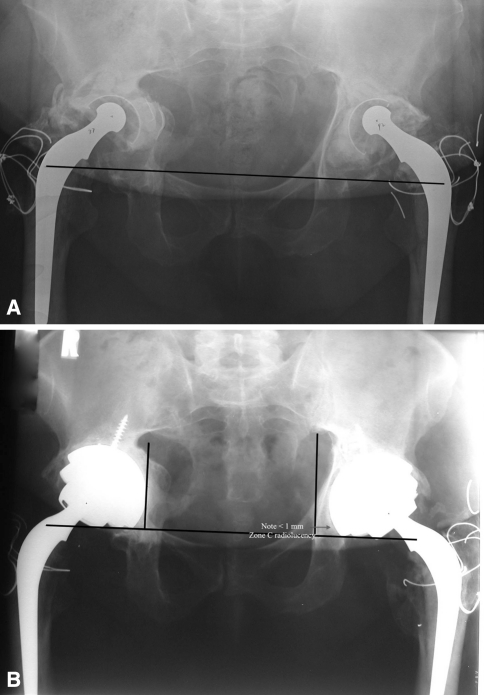
Fig. 3A–B.
(A) Bilateral IIIA defects are seen. The THAs were performed in 1978 when the patient was 32 years old. (B) The right hip is 4 years postoperative, and the left 3 years. Note the use of bipolar heads over the retained nonmodular femoral component. The less than 1 mm gap in Zone C of the left acetabulum (arrow) is being monitored.
One patient developed an early postoperative infection, treated with irrigation, débridement, head and liner exchange, and placement of antibiotic-laden cement beads, followed by 6 weeks of intravenous antibiotics. At 13-month followup, the patient was asymptomatic, with a normal C-reactive protein and erythrocyte sedimentation rate. There were no dislocations.
Discussion
Severe protrusio defects occurring either medially or medially and vertically represent a reconstructive challenge. After reconstruction, if the joint center remains medialized, bony impingement and instability may occur. We determined the initial results obtained with a novel “cup-in-cup” technique utilizing two porous tantalum acetabular shells, one placed onto supportive host bone in a cementless fashion and the other cemented into this shell.
Readers should be aware of the limitations of this report and our observations must be interpreted cautiously. First, we had a small number of reconstructions as the majority of acetabular reconstructions seen in our practice are performed with hemispherical shells with or without augments. Second, our followup is short and the longer-term durability of this specific construct is unknown.
Recent reports using tantalum acetabular components, with or without augments, have described both the defect treated and the mean improvement in horizontal and vertical offset (Table 5). Three papers to date have reported on the treatment of Paprosky IIIA and IIIB defects [1, 9, 17]. Combining these papers, 63 IIIA defects and 22 IIIB defects were treated. The mean change in vertical offset was 18 mm and the mean change in horizontal offset was 16 mm. In our five patients (four IIIA, one IIIB), the mean change in vertical offset was 22 mm and the mean change in horizontal offset was 11 mm. Our results in a limited number of patients suggest the cup-in-cup construct allows improvement in vertical offset without excessive lateralization of the joint center.
Table 5.
Comparison of offset change after acetabular reconstruction
| Study | Number of surgeries | Paprosky type (number) | Followup* (months) | Survivorship (%) | Augments required in surgery (total number used) | Mean pre- to postoperative change in prosthetic head center (mm) | |
|---|---|---|---|---|---|---|---|
| Vertical (− = inferior) | Horizontal (+ = lateral) | ||||||
| Ballester Alfaro and Sueiro Fernández [1] | 19 | IIIA 13 IIIB 6 |
26 (18–43) | 100 | 14 (all buttress augments) (5 cup-cages) | −21 | +16 |
| Fernandez-Fairen et al. [8] | 263 | I 20 IIA 73 IIB 82 IIC 39 IIIA 40 IIIB 9 |
73.6 (60–84) | 99.2 | 34 IIB 3 IIIA 22 IIIB 9 |
−22 | +15 |
| Flecher et al. [9] | 23 | IIIA 17 IIIB 6 |
35 (24–50) | 100 | 14 (16) | −15 | +15 |
| Weeden and Schmidt [17] | 43 | IIIA 33 IIIB 10 |
34 (24–48) | 98 | 26 (all 10 IIIB cases used augments) (2 cup-cages) | −19 | Not reported |
| Blumenfeld and Bargar | 8 | IIC 3 IIIA 4 IIIB 1 |
28 (12–50) | 100 | 1 | −18 | +11 |
* Values are expressed as mean, with range in parentheses.
Two mechanical concerns exist with this technique. The femoral head center is displaced laterally from the center of the medial shell. This could produce a moment creating tension stresses at the bone-implant interface that might affect bone ingrowth. The finding in two patients of less than 1 mm radiolucencies in Zone C is possibly a result of this mechanism but is of unclear importance at this time. The second mechanical concern is the durability of cementation of the second porous shell into the first. Published mechanical studies of cementing a liner or a component into a shell would support the validity of this construct [7, 11]. With a 2-mm cement mantle between a cobalt-chromium shell and a titanium alloy shell, the fixation strength exceeded that of commonly used locking mechanisms [7]. As tantalum is more porous than cobalt-chrome, we suspect our fixation strength is adequate in these reconstructions.
Cost is a factor in this reconstruction as two acetabular components are required. Certainly when the defect allows reconstruction with a single shell, we would avoid the cup-in-cup reconstruction. When the reconstruction requires the use of an augment, a reconstruction cage, or a structural allograft, at our institution, the modular tantalum shell is 25% to 40% less expensive than those alternatives. In the appropriate setting, the cup-in-cup technique may be favorable.
For the limited situation where more conventional revision constructs will not restore offset and cementless fixation on host bone is deemed preferable, we believe this technique a reasonable alternative. Our early observations show no obvious implant migration or debonding of the outer shell. We continue to use this technique sparingly and only when indicated as described. We continue to follow the patients.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved or waived approval for the reporting of this case, that all investigations were conducted in conformity with ethical principles of research, and that patient consent for publication of these case reports was obtained.
References
- 1.Ballester Alfaro JJ, Sueiro Fernández J. Trabecular Metal buttress augment and the Trabecular Metal cup-cage construct in revision hip arthroplasty for severe acetabular bone loss and pelvic discontinuity. Hip Int. 2010;20(Suppl 7):S119–S127. doi: 10.1177/11207000100200s720. [DOI] [PubMed] [Google Scholar]
- 2.Beaule PE, Ebramzadeh E, LeDuff M, Prasad R, Amstutz HC. Cementing a liner into a stable cementless acetabular shell: the double socket technique. J Bone Joint Surg Am. 2004;86:929–934. doi: 10.2106/00004623-200405000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Berry DJ, Sutherland CJ, Trousdale RT, Colwell CW, Chandler HP, Ayres D, Yashar AA. Bilobed oblong porous coated acetabular components in revision total hip arthroplasty. Clin Orthop Relat Res. 2000;371:154–160. doi: 10.1097/00003086-200002000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Christie MJ, Barrington SA, Brinson MF, Ruhling ME, DeBoer DK. Bridging massive acetabular defects with the Triflange Cup: 2- to 9-year results. Clin Orthop Relat Res. 2001;393:216–227. doi: 10.1097/00003086-200112000-00024. [DOI] [PubMed] [Google Scholar]
- 5.DeBoer DK, Christie MJ. Reconstruction of the deficient acetabulum with an oblong prosthesis: three-to-seven-year results. J Arthroplasty. 1998;13:674–680. doi: 10.1016/S0883-5403(98)80012-0. [DOI] [PubMed] [Google Scholar]
- 6.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 7.Ebramzadeh E, Beaule PE, Culwell JL, Amstutz HC. Fixation strength of an all-metal acetabular component cemented in to an acetabular shell: a biomechanical analysis. J Arthroplasty. 2004;19:45–49. doi: 10.1016/j.arth.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 8.Fernandez-Fairen M, Murcia A, Blanco A, Merono A, Murcia A, Jr, Ballester J. Revision of failed total hip arthroplasty acetabular cups to porous tantalum components: a 5-year follow-up study. J Arthroplasty. 2010;25:865–872. doi: 10.1016/j.arth.2009.07.027. [DOI] [PubMed] [Google Scholar]
- 9.Flecher X, Sporer S, Paprosky W. Management of severe bone loss in acetabular revision using a Trabecular Metal shell. J Arthroplasty. 2008;23:949–955. doi: 10.1016/j.arth.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 10.Goodman S, Saastamoinen H, Nadav S, Gross A. Complications of ilioischial reconstruction rings in revision total hip arthroplasty. J Arthroplasty. 2004;19:436–446. doi: 10.1016/j.arth.2003.11.015. [DOI] [PubMed] [Google Scholar]
- 11.Haft GF, Heiner AD, Dorr LD, Brown TD, Callaghan JJ. A biomechanical analysis of polyethylene liner cementation into a fixed acetabular shell. J Bone Joint Surg Am. 2003;85:1100–1110. doi: 10.1302/0301-620X.85B8.14673. [DOI] [PubMed] [Google Scholar]
- 12.Lucas DH, Scott RD. The Ranawat sign: a specific maneuver to assess component positioning in total hip arthroplasty. J Orthop Tech. 1994;2:59–61. [Google Scholar]
- 13.Nehme A, Lewallen DG, Hanssen AD. Modular porous metal augments for treatment of severe acetabular bone loss during revision hip arthroplasty. Clin Orthop Relat Res. 2004;429:201–208. doi: 10.1097/01.blo.0000150133.88271.80. [DOI] [PubMed] [Google Scholar]
- 14.Paprosky WG, Perona PG, Lawrence MJ. Acetabular defect classification and surgical reconstruction in revision arthroplasty: a 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 15.Sporer SM, Paprosky WG. The use of a Trabecular Metal acetabular component and Trabecular Metal augment for severe acetabular defects. J Arthroplasty. 2006;21(Suppl 6):83–86. doi: 10.1016/j.arth.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 16.Wachtl SW, Jung M, Jakob RP, Gautier E. The Burch-Schneider antiprotrusio cage in acetabular revision surgery: a mean follow-up of 12 years. J Arthroplasty. 2000;15:959–963. doi: 10.1054/arth.2000.17942. [DOI] [PubMed] [Google Scholar]
- 17.Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22(6 Suppl 2):151–155. doi: 10.1016/j.arth.2007.04.024. [DOI] [PubMed] [Google Scholar]