Abstract
Background
With contemporary canal-filling press-fit stems, there is no adjustability of stem position in the canal and therefore the canal anatomy determines stem version. Stem version will affect head/neck impingement, polyethylene wear from edge loading, and hip stability, but despite this, the postoperative version of a canal-filling press-fit stem is unclear.
Questions/purposes
Is there a difference between the version of the nonoperated femur and the final version of a canal-filling press-fit femoral component? Could a difference create an alignment problem for the hip replacement?
Methods
Sixty-four hips were studied with fluoroscopy and 46 nonarthritic and 41 arthritic hips were studied with MRI. A standardized fluoroscopic technique for determining preoperative and postoperative femoral version was developed with the patient supine on a fracture table undergoing supine total hip arthroplasty. To validate the methods, the results were compared with two selected series of axial MRI views of the hip comparing the version of the head with the version of the canal at the base of the neck.
Results
For the operated hips, the mean anatomic hip version was less than the stem version: 18.9° versus 27.0°. The difference on average was 8.1° of increased anteversion (SD, 7.4°). Both MRI series showed the femoral neck was more anteverted on average than the femoral head, thereby explaining the operative findings.
Conclusion
With a canal-filling press-fit femoral component there is wide variation of postoperative component anteversion with most stems placed in increased anteversion compared with the anatomic head. The surgical technique may need to adjust for this if causing intraoperative impingement or instability.
Introduction
The recommended positioning of the femoral component in THA is to restore the offset and the “natural anteversion” of the femur in the setting of normal femoral anatomy [9]. This natural anteversion can vary, and in a study by Reikeras and Hoiseth [11], the amount of preoperative anteversion correlated with the extent of the degenerative disease, suggesting to the authors that anteversion may be part of the etiology of osteoarthritis of the hip.
With a cemented stem, the surgeon can manipulate the stem to set a desired anteversion, but as has been observed by Dorr et al. [3] for cementless femoral stems, there is much reduced adjustability of stem position for tapered stems and no adjustability for metaphyseal filling stems. If there is no adjustability of the femoral stem anteversion, there are two important questions to be answered: (1) What is the stem anteversion that must be accepted? (2) How does it compare with the anteversion of the preoperative proximal femur?
The first question has been studied. Dorr et al. [4] measured the average postoperative stem anteversion with three-dimensional CT scans using a press-fit stem and noted an average 10.2° ± 7.5° with a range of −8.6°, retroversion, to 27.1°, anteversion. Similarly, Wines and McNicol [16] using CT measurements noted the femoral anteversion to be an average 16.8° (SD, 11.1°) with a range from −15°, retroversion, to 45°, anteversion, for a press-fit stem. Sendtner et al. [13] using intraoperative computer navigation noted femoral stem anteversion of an average of 18° with a range from −13°, retroversion, to 38°, anteversion, with a press-fit stem. Some variation of values may be attributable to the measurement method, but it is clear there is a wide range of postoperative values in all of these studies using press-fit hip stems.
Numerous reports describe the average anteversion of the native unoperated femur. Maruyama et al. [8] reported a mean femoral anteversion of 11.6° (men 11.1°, women 12.2°) from a cadaver study. A CT study of Indian hips reports an anteversion of 8° (range, 6.5°–10°) [7]. Reikas et al. [10] using CT scans measured the anteversion of the proximal femur at 13° ± 7° in normal patients and 20° ± 9° in patients with osteoarthritis. Braten et al. [1] using ultrasound techniques found the average anteversion in normal males to be 14° and females to be 18°.
The unanswered question is how does the anteversion of the preoperative femur compare with the anteversion achieved in the postoperative femur after THA? In other words, does hip arthroplasty restore the natural anteversion of the femur?
Patients and Methods
Sixty-five patients (66 hips) were recruited and 63 sequential patients (64 hips), with sufficient hip rotation for analysis were studied with fluoroscopy at the time of routine unilateral primary THA. Two of the 65 patients were excluded because they lacked enough rotation in the hip to get the necessary preoperative view. There were 31 males and 32 females with an average age of 64.6 years. Institutional Review Board approval was obtained as was informed consent for prospective review of data from each patient.
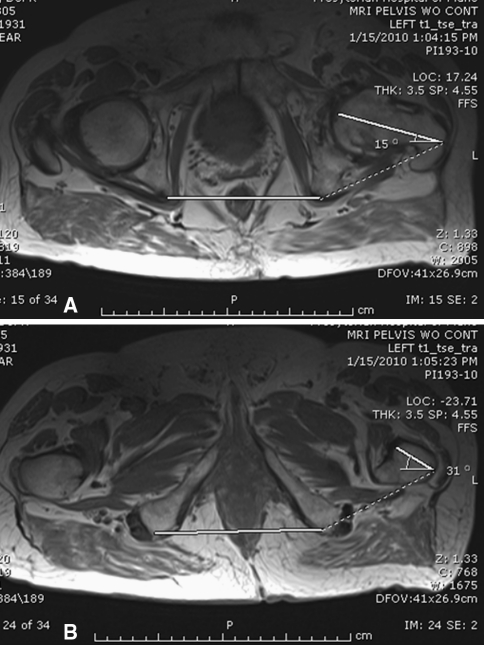
Because the postoperative stem version was determined by the shape of the endosteal canal, two series of axial MRI scans (axial T2 images) were studied to compare the shape of the canal at the femoral head level and the lower neck level at the lesser trochanter to further corroborate the operative data (Fig.1A–B). The first MRI series (MRI-1, n = 46) consisted of selected nonarthritic patients undergoing MRI of the pelvis for nonorthopaedic reasons; the second series (MRI-2, n = 41) was collected and studied chronologically after the fluoroscopy series, in which an MRI was ordered as part of the preoperative planning. This imaging included views of the knee.
Fig. 1A–B.
(A) T2 axial view hip showing anteversion of femoral head. (B) T2 axial CT view showing anteversion of femoral neck.
A standardized fluoroscopic technique was developed for routine use with all primary hip arthroplasties with the patient supine on a fracture table. All stems were the Microplasty Taperloc (Biomet, Inc, Warsaw IN), a press-fit, metaphyseal-filling blade-shaped wedge stem approved by the FDA. The stems were prepared with a broach-only technique. The final stem chosen was the largest stem that could be placed into the femoral canal. The rotation of the stem was determined by the shape of the endosteal canal and no attempt was made to change this.
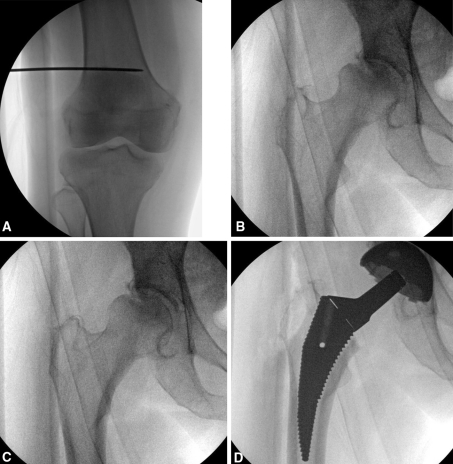
The fluoroscope was used to determine a true AP view of the knee. A small percutaneous unicortical pin was placed laterally above the knee to mark this position. An AP image of the hip was taken in this same position and designated the neutral view. The femur was then internally rotated until there was a single view of the greater trochanter, designated as the anteverted image. The degree of rotation measured from the pin with a long-armed goniometer was recorded as the preoperative anteversion angle of the proximal femur. The interobserver reliability for the use of a long-armed goniometer has been studied by Rothstein et al. and is high (r = 0.88 to 0.99) [12] (Fig. 2A–E). After placement of the final femoral broach, a true AP image of the broach was taken facilitated by a circular hole in the broach. The femur is rotated until this hole is a perfect circle and the rotation of the pin measured again with a long-armed goniometer and designated as the postoperative stem anteversion.
Fig. 2A–D.
(A) AP view of the knee with a unicortical Kirschner wire placed. (B) AP of the hip corresponding to AP view of the knee in A. (C) Internally rotated view of the hip until a single profile of the greater trochanter; degree of rotation designated the anteversion angle of the hip. (D) True AP of the rasp, noted by a perfect circle for the hole in the rasp, with rotation measured from the Kirschner wire designating the stem anteversion.
We determined the difference between the preoperative head anteversion and the postoperative stem anteversion using the Student’s t-test for paired samples assuming equal variance. The statistical analysis was done using Microsoft Office Excel 2007 (Redmond WA, USA).
Results
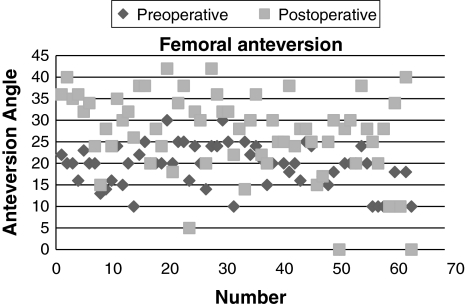
For the operated hips, the preoperative hip version was less than (p < 0.001) the postoperative hip stem version: 18.9° (range, 0°–30°) versus 27.0° on average (range, 0°–42°) (Fig. 3). The difference on average was 8.1° of increased femoral anteversion (SD, 7.4°) after the hip arthroplasty. The range is from −11° to 22°.
Fig. 3.
Scatterplot of the anteversion values for the study series that shows the increase (p > 0.001) in femoral anteversion for the postoperative femur compared with the preoperative femur.
For the MRI series 1, the average head anteversion was less than (p < 0.001) the average neck anteversion: 20.0° versus 35.4°. The difference was 15.4° of increased anteversion on average for the femoral neck compared to the femoral head (SD, 6.3).
For the MRI series 2, the average head anteversion was less than (p < 0.001) the average neck anteversion: 13.4° versus 24.6°. The difference was 11.7° of increased anteversion on average for the femoral neck compared with the femoral head (SD, 6.5). Correcting for the rotation of the knee, the version of the neck was 14.8° and the head was 3.6° on average.
Discussion
The best amount of femoral anteversion for the total hip stem has not been determined, although it is generally agreed to be between 10° to 20° [4] and 10° to 30° [2]. It is generally appreciated, as noted by Dorr et al. [3], that the stem position using press-fit techniques is predetermined by the canal shape with the implication that this has restored “natural anteversion” of the femur [9] with anterior tilt leading to increased anteversion. Very little has been written about the relationship between the native anteversion of the unoperated femur and the anteversion actually achieved by surgical stem placement. Unless the femoral stem component is inserted with the femoral head in place [6], there is no means of directly comparing the femoral stem anteversion achieved with the preoperative femoral head anteversion. Therefore, indirect methods must be used, which ideally allow for adjustments of component position at the time of surgery.
With no adjustability of the femoral stem version, there are two important questions to be answered: (1) What is the stem anteversion that must be accepted? (2) How does it compare with the anteversion of the preoperative proximal femur?
This study is subject to certain limitations. First, this is a study using only one femoral design, a broach-only metaphyseal-filling blade-shaped wedge. In the past, with cemented femoral stems, there was a range of anteversion adjustability available to the surgeon, as much as 10° to 20° according to Dorr et al. [3]. With a canal-filling bone ingrowth stem, there is less adjustability depending on the design and instrumentation used. A stem that uses intramedullary reaming will logically fit differently than a stem that is prepared by broaches only, and a blade-shaped stem will fit differently from a rounded design. Broach-only stems of the study design are commonly in use and favored by many surgeons because of the simplicity of the preparation and diminished trauma to the femur. Therefore, the findings of this study pertain to a large number of current THAs. Second, femoral anteversion can be determined in several ways, ie, CT scan [4, 12, 16], anatomic dissection [8], computer-assisted techniques [14], and intraoperative fluoroscopy as done here, which may each give somewhat different values depending on how the neutral point (0° of anteversion) and the final end point are determined. This may explain in part the difference in values determined by the intraoperative technique and the MRI technique used in this study. Because this study is looking at the differences between the preoperative and postoperative angles, the actual angles are not important. Of importance is how the two compare and whether “natural anteversion” has been restored. Third, all of these cases were done through the direct anterior approach, which uses the fluoroscope and fracture table. Logically, the fit of a canal-filling stem should be independent of the approach because the position of the stem is determined by the shape of endosteal canal. This is the whole point of the study. Studies have shown that surgeons are not good at estimating the anteversion of the femoral component [4] without a quantitative method.
The answer to the question posed about the relationship between preoperative and postoperative femoral anteversion in the setting of a bone ingrowth canal-filling broach-only stem is that the postoperative femoral stem is consistently more anteverted on average than the native femoral head, on average 8.1°, and there is great variability of postoperative anteversion, from −11° (retroverted) to 22° (anteverted) compared with preoperative version. It cannot be concluded that a press-fit stem of the type studied restores “natural anteversion” of the femur.
The data suggest the explanation is that the anatomic shape of the femoral canal determines the anteversion of the stem in the setting of a canal-filling stem, and the canal is more anteverted at the level of the lower neck and intertrochanteric area than the head. There are other studies using different methods, which have documented similar increased anteversion of a press-fit femoral stem (Table 1).
Table 1.
Review of literature pertaining to postoperative press-fit stem position in the femur
| Authors | Technique | Imaging | Stem | Postoperative anteversion* |
|---|---|---|---|---|
| Suh et al. [14] | Postoperative | CT | Press-fit | 3.8° ± 2.6 ° |
| Eckrich et al. [5] | Laboratory apparatus | Plane radiograph | Press-fit | 7.5° ± 6.3° |
| Emerson (current study) | Intraoperative | Fluoroscopy | Press-fit | 8.2° ± 7.4° |
* Degrees of increased anteversion relative to the preoperative femur.
The clinical implications of this observation are important. Femoral offset and anteversion, in conjunction with acetabular abduction and anteversion, are important implant-related factors contributing to impingement free ROM after THA. Computer simulation studies by Patel et al. [9] showed that for each combination of acetabular abduction and femoral anteversion, there is an optimum range of acetabular anteversion that will minimize impingement. In clinical practice, with both components subject to positioning constraints, cup orientation by osseous coverage, and femoral anteversion by the shape of the canal, the importance of looking at a combined component anteversion has become appreciated and increasingly used at surgery. The concept is that overall anteversion, the sum of the two values, allows for adjusting the individual component positions to achieve the best combination [2]. Dorr et al. [3] write that the safe zone of combined anteversion is 25° to 50° (Table 2).
Table 2.
Review of the literature pertaining to combined femoral anteversion with and without a femoral stem
| Author | Technique | Imaging | Stem | Combined anteversion |
|---|---|---|---|---|
| Maruyama et al. [8] | Cadaver | None | None | 29.6° M, 33.5° F |
| Widmer and Zurfluh [15] | Mathematical | None | None | 37° |
| Dorr et al.* [3] | Intraoperative | CT | Press-fit | 37.6° ± 7° |
* Safe zone determined to be 25° to 50°; M = male; F = female.
Component orientation outside of this safe range will lead to impingement and eccentric loading with implications for bearing wear and joint stability. Where there is excessive femoral anteversion, the cup will need to be adjusted with less anteversion and where the stem is less anteverted, the cup will need to more anteverted. This need has caused some surgeons to recommend a workflow that positions the acetabular component only after the femoral version has been determined [3]. The anteversion of the femoral component is generally assessed at surgery by the surgeon’s visual assessment of the stem position relative to the condylar plane of the distal femur. One study suggests the surgeon’s estimation of the femoral anteversion achieved at surgery has low precision (reproducibility) [4], making it difficult to set a corresponding acetabular position. The advantage of the fluoroscopic technique described here is that a consistent neutral position is established and the postoperative anteversion is quantifiable.
For surgeons who find it difficult to assess the intraoperative version of the femoral stem, the data in this study do demonstrate some value for a preoperative CT or MRI scan to determine the probable anteversion of the postoperative stem. If preoperative planning raises the concern for an unacceptable version of the femoral component, the surgeon may want to use a surgical technique that allows for intraoperative adjustment of the femoral stem version.
Footnotes
The author has received funding from Biomet, Inc Warsaw, IN.
The author certifies that his institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
The author certifies that he, or a member of this immediate family, has no commercial associations that might pose a conflict of interest in connection with the submitted article.
References
- 1.Braten M, Terjesen T, Rossvoll I. Femoral anteversion in normal adults. Ultrasound measurements in 50 men and 50 women. Acta Orthop Scand. 1992;63:29–32. doi: 10.3109/17453679209154844. [DOI] [PubMed] [Google Scholar]
- 2.D’Lima DD, Urguart AG, Buehler KO, Walker RH, Colwell CW. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82:315–321. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Dorr LD, Malik A, Dastane M, Zhinian W. Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res. 2009;467:1132–1528. doi: 10.1007/s11999-008-0598-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dorr LD, Wan Z, Malik A, Dastane M, Deshmane P. A comparison of surgeon estimation and computed tomographic measurement of femoral component anteversion in cementless total hip arthroplasty. J Bone Joint Surg Am. 2009;91:2598–2604. doi: 10.2106/JBJS.H.01225. [DOI] [PubMed] [Google Scholar]
- 5.Eckrich SG, Noble PC, Tullos HS. Effect of rotation on the radiographic. Appearance of the femoral canal. J Arthroplasty. 1994;9:419–426. doi: 10.1016/0883-5403(94)90053-1. [DOI] [PubMed] [Google Scholar]
- 6.Kamizis IA. A technique for accurate reproduction of the femoral anteversion during primary total hip arthroplasty. Arch Orthop Trauma Surg. 2001;121:343–345. doi: 10.1007/s004020000237. [DOI] [PubMed] [Google Scholar]
- 7.Maheshwari AV, Zlowodzki MP, Siram G, Jain AK. Femoral neck anteversion, acetabular anteversion and combined anteversion in the normal Indian adult population: a computed tomographic study. Indian J Orthop. 2010;44:277–282. doi: 10.4103/0019-5413.65156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maruyama M, Feinberg JR, Capello WN, D’Antonio JA. The Frank Stinchfield Award: Morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res. 2001;393:52–65. doi: 10.1097/00003086-200112000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Patel AB, Wagle RR, Usrey MM, Thompson MT, Incavo SJ, Noble PC. Guidelines for implant placement to minimize impingement during activities of daily living after total hip arthroplasty. J Arthroplasty. 2010;25:1275–1281. doi: 10.1016/j.arth.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 10.Reikeras O, Bjerkreim I, Kolbenstvedt A. Anteversion of the acetabulum and femoral neck in normals and in patients with osteoarthritis of the hip. Acta Orthop Scand. 1983;54:18–23. doi: 10.3109/17453678308992864. [DOI] [PubMed] [Google Scholar]
- 11.Reikeras O, Hoiseth A. Femoral neck angles in osteoarthritis of the hip. Acta Orthop Scand. 1982;53:781–784. doi: 10.3109/17453678208992292. [DOI] [PubMed] [Google Scholar]
- 12.Rothstein JM, Miller PJ, Roettger RF. Goniometric reliability in a clinical setting. Elbow and knee measurements. Phys Ther. 1983;63:1611–1615. doi: 10.1093/ptj/63.10.1611. [DOI] [PubMed] [Google Scholar]
- 13.Sendtner E, Müller M, Winkler R, Wörner M, Grifka J, Renkawitz T. Femur first in hip arthroplasty—the concept of combined anteversion. Z Orthop Unfall. 2010;148:185–190. doi: 10.1055/s-0029-1240969. [DOI] [PubMed] [Google Scholar]
- 14.Suh KT, Kang JH, Roh HL, Moon KP, Kim HJ. True femoral anteversion during primary total hip arthroplasty: use of postoperative computed tomography-based sections. J Arthroplasty. 2006;21:599–605. doi: 10.1016/j.arth.2005.04.042. [DOI] [PubMed] [Google Scholar]
- 15.Widmer KH, Zurfluh B. Compliant positioning of total hip components for optimal range of motion. J Orthop Res. 2004;22:815–821. doi: 10.1016/j.orthres.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 16.Wines AP, McNicol D. Computed tomography measurement of the accuracy of component version in total hip arthroplasty. J Arthroplasty. 2006;21:696–701. doi: 10.1016/j.arth.2005.11.008. [DOI] [PubMed] [Google Scholar]