Abstract
Background
Posterior soft tissue repair after posterior THA reportedly decreases the risk of dislocation. Previously described techniques often require drill holes through the greater trochanter, do not include both the short external rotators and the capsule, or require a complex series of multiple sutures. We therefore describe a technique to address these issues.
Description of Technique
The posterior soft tissues were repaired with a single nonabsorbable suture passed through the external rotators and posterior capsule and then through the capsule and posterior border of minimus in a figure-of-eight pattern. This repair remains pliable and obliterates the dead space.
Methods
We retrospectively reviewed 165 patients who underwent 178 primary THAs through a mini-posterior THA and also underwent soft tissue repair using our technique. We determined the rate of dislocation and complications associated with this technique. The minimum clinical followup was 1 year (mean, 23 months; range, 12–37 months).
Results
This repair was associated with a low risk of dislocation at 1 year (one of 178 hips, 0.56%) and no apparent complications related to the technique.
Conclusions
This soft tissue to soft tissue repair technique after posterior-approach THA is technically straightforward and reliable with a low associated dislocation rate.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The posterolateral or posterior approach for THA has the advantages of preserving the hip abductor musculature and providing good visualization during femoral preparation and component insertion. Those advantages have traditionally been offset to some degree by a greater risk of postoperative dislocation after posterior-approach THA as compared to direct lateral- or anterior-approach THA. Historically, as described by Moore, the posterior approach was performed with a complete capsulectomy and the posterior soft tissues (short external rotators) were not repaired [7, 12]. The increased risk of dislocation using a posterior approach is generally attributed to disruption of the posterior soft tissue structures, including the short external rotators of the hip and the posterior capsule [1]. More recently, a variety of surgical techniques have been introduced that repair these posterior structures at the time of THA and the risk of postoperative dislocation appears to have been lowered with each of these [2, 4, 5, 9, 11, 12]. Most techniques describe reapproximation of the capsule and/or short external rotators to the posterior aspect of the greater trochanter through drill holes in the bone [5, 9, 12]. In some patients, passing sutures through the trochanter can weaken the bone and complications including failure of the repair [10] and trochanteric avulsion fracture have been reported [12]. Other techniques for posterior repair include soft tissue capsulorrhaphies [2–4], but the techniques are often complex (involving as many as five separate sutures) or do not include repair of the short external rotators.
We devised a simple surgical technique that involves soft tissue to soft tissue repair of the posterior capsule and the short external rotators using a single nonabsorbable suture passed in a figure-of-eight fashion. This technique was designed to obliterate the dead space adjacent to the posterior aspect of the prosthetic femoral head and to be robust enough to put the hip through a functional ROM without disruption of the repair.
Description of Technique
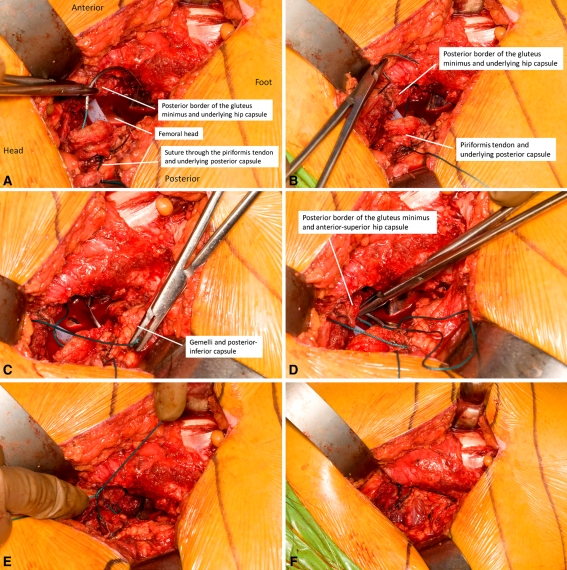
All procedures were performed by the senior author (MWP) using a mini-posterior-incision technique, the details of which have been previously published [8]. During exposure, the external rotators and the underlying posterior hip capsule were incised and preserved as one layer. After insertion of final components, the posterior soft tissue repair was performed. The interval between the gluteus medius and minimus was exposed and the medius muscle was retracted slightly anteriorly to expose the posterior border of the minimus. The hip was internally rotated to best expose the posterior border of the gluteus minimus and the underlying anterior-superior hip capsule. A single Number 5 Ethibond® suture (Ethicon, Inc, Somerville, NJ, USA) was passed twice to reapproximate the piriformis and the posterior capsule back to the anterior-superior capsule and the posterior border of the gluteus minimus (Fig. 1). The suture was passed sequentially from outside-in to inside-out: the first pass was through the piriformis tendon and posterior-superior hip capsule and then from inside the anterior-superior capsule through the posterior-superior edge of the gluteus minimus; the second pass was started 1 cm more distally through the gemelli and posterior-inferior capsule and then from inside the anterior-superior capsule through the posterior-superior edge of the gluteus minimus to form a figure-of-eight pattern. The suture was tied and the hip was placed through a ROM to confirm integrity of the repair. No other sutures were placed through the capsule or external rotators and no sutures were placed through the greater trochanter. The remainder of the wound was closed in layers beginning with the fascia.
Fig. 1A–F.
(A) The repair begins by passing a Number 5 Ethibond® suture from outside to inside through the piriformis tendon and posterior-superior hip capsule. (B) The suture is then passed from the inside of the anterior-superior capsule through the posterior-superior edge of the gluteus minimus tendon. (C) The second pass is started 1 cm more distally and passed from outside to inside through the gemelli and posterior-inferior capsule. (D) The final pass is from the inside of the anterior-superior capsule through the posterior-superior edge of the gluteus minimus tendon. (E) The suture forms a figure-of-eight pattern and is tied. (F) The final repair demonstrates elimination of any dead space between the metal prosthetic head and the posterior capsule.
Patients and Methods
From November 2006 to December 2009, 165 patients (178 hips) underwent uncomplicated primary THA with a mini-posterior approach. The group was comprised of 96 women (104 hips) and 79 men (74 hips) with an average age of 64 years (range, 22–93 years). The preoperative diagnosis was osteoarthritis in 162 hips, rheumatoid arthritis in six hips, avascular necrosis in six hips, posttraumatic degenerative joint disease in three hips, and fracture nonunion in one hip. We excluded from this study any patients with any of the following: severe bone deformity about the hip, such as Crowe Type III or IV dysplasia; osteomyelitis or prior intraarticular infection of the hip; substantial neurologic or musculoskeletal disorders that would adversely affect gait or early weightbearing after surgery; evidence of abnormal abductor function or gluteus medius tears preoperatively; acute trauma with proximal femoral fracture; metastatic cancer; congenital, developmental, or other bone disease; and arthrodesis of the affected hip. The minimum clinical followup was 1 year (mean, 23 months; range, 12–37 months). No patients were lost to followup. No patients were recalled specifically for this study; all data were obtained from medical records and radiographs.
All patients received uncemented acetabular and femoral components. The majority of patients received a metal-on-highly crosslinked polyethylene articulation with femoral head sizes of 28 mm (five hips), 32 mm (71 hips), 36 mm (72 hips), or 40 mm (seven hips). For 23 hips, a metal-on-metal bearing surface with jumbo femoral heads (43–53 mm) was used.
All patients were managed with the same comprehensive perioperative pain management and rapid rehabilitation protocol. Traditional total hip dislocation precautions were not used; the only warning was to avoid the combination of flexion of greater than 100° and marked internal rotation of the hip during the first 8 weeks after surgery. Patients were otherwise encouraged to proceed with activities as tolerated, allowing their hip symptoms to be their guide.
Results
This soft tissue-to-soft tissue repair technique was performed successfully in all patients who met the inclusion criteria. The repair was associated with a low risk of dislocation. At 16 months postoperatively, one patient (0.6%) sustained a posterior hip dislocation. The patient had a 36-mm head with a metal-on-polyethylene bearing surface. The dislocation occurred because of a fall and was successfully treated with closed reduction. There were no complications related to the posterior soft tissue repair technique.
Discussion
Dislocation is an infrequent but dramatic and disconcerting complication for patient and surgeon alike after THA. The incidence of dislocation varies in the literature, with rates reported between 1% to greater than 9% in some series. A recent study of the Medicare 5% national dataset from 2007 revealed a 2.1% risk of dislocation at 6 months [6]. The cumulative risk of longer-term dislocation after posterolateral approaches is reportedly more than double that after anterolateral or transtrochanteric approaches, with a 1-year risk of dislocation approaching 4% using this technique [1]. Various techniques to repair the posterior soft tissues have been reported, most commonly through drill holes in the greater trochanter (Table 1). Concerns associated with drilling holes through the greater trochanter, including avulsion fracture and failure of the repair, as well as practical issues related to the expense and added steps of using drill bits and sutures passers, led us to develop a simple soft-tissue-only repair of the posterior capsule and external rotators using a single nonabsorbable suture. We determined using a contemporary posterior-approach THA whether this simple soft-tissue-only repair was associated with a low risk of dislocation at a minimum of 1 year postoperatively.
Table 1.
Published reports in the literature reporting early dislocation rates with various approaches to posterior soft tissue repair
| Study | Posterior soft tissue repair technique | Number of hips | Followup (months)* | Dislocation rate |
|---|---|---|---|---|
| Hedley et al. [5] (1990) | Capsulomuscular flap repaired to bone | 259 | Not reported | 0.7% (2/259) |
| Pellicci et al. [9] (1998) | Capsule and external rotators repaired through drill tunnels | 519 | 6–12 | 0.2% (1/519) |
| Chiu et al. [2] (2000) | Capsulorrhaphy | 96 | 38 (12–60) | 0% (0/96) |
| Goldstein et al. [4] (2001) | Capsulorrhaphy | 500 | 12 | 0.6% (3/500) |
| White et al. [12] (2001) | Capsule repaired through drill holes | 437 | 6 | 0.7% (3/437) |
| Tsai et al. [11] (2008) | Capsular repair | 62 | 14.8 (12–22) | 0% (0/62) |
| Current study (2011) | Single-suture soft tissue repair | 178 | 23 (12–37) | 0.6% (1/178) |
* Values are expressed as mean, range, or mean with range in parentheses.
This study is limited by relatively small numbers of patients and the case series design. As with all such studies, there is no direct control group, although comparison with historical data is possible. In the case of THA dislocation rates, historical results are heterogeneous with respect to femoral head size and other potential confounders, so direct comparison is imperfect. Second, we have assessed the early (1-year) risk of dislocation but not the long-term risk. Historical patterns of dislocation [1], however, suggest the highest risk of dislocation to be within the first several months after THA, with much smaller risks of dislocation after the first postoperative year. However, this series does represent a consecutive series of patients with an objective end point (dislocation) and 100% clinical followup at 1 year. We believe it is appropriate to view this study as a preliminary report and description of a new technique.
Our results suggest this simple soft tissue-to-soft tissue to soft tissue repair is associated with a low rate of early dislocation. This soft tissue repair has several theoretical advantages over a more traditional osseous repair. First, the posterior capsule and external rotators are advanced to lie directly on the femoral head, which obliterates any dead space. Second, the soft tissue-to-soft tissue repair is more pliable than a transosseous repair and seems less likely to pull apart with internal rotation or flexion of the hip in the early postoperative period. Third, the risk of fracture of the greater trochanter, which has been reported [12] after repair through drill holes in the trochanter, is minimized with this technique. Fourth, by suturing the posterior capsule and piriformis to the posterior border of the gluteus minimus (in addition to the anterior-superior capsule), some degree of dynamic stabilization may be conferred when the gluteus minimus muscle fires. Finally, the repair is simple and quick to perform and does not require a drill bit or suture passer.
In conclusion, this simple soft tissue-to-soft tissue repair of the posterior capsule and short external rotators appears to be reliable, with a low risk of postoperative dislocation after posterior-approach THA at 1 year. Our dislocation rate compares favorably with other reports in the contemporary literature that show a substantial decrease in the risk of dislocation when some or all of the posterior soft tissue structures are repaired after posterior-approach THA. When compared to a transosseous repair through drill holes, this technique takes less time and is more straightforward. We continue to use this technique after posterior-approach THA.
Footnotes
One of the authors (MWP) has received royalties from DePuy Orthopaedics Inc (Warsaw, IN, USA), MAKO Surgical Corp (Fort Lauderdale, FL, USA), Stryker Orthopaedics (Mahwah, NJ, USA), and Zimmer Inc (Warsaw, IN, USA).
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Mayo Clinic.
References
- 1.Berry DJ, Knoch M, Schleck CD, Harmsen WS. Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2005;87:2456–2463. doi: 10.2106/JBJS.D.02860. [DOI] [PubMed] [Google Scholar]
- 2.Chiu FY, Chen CM, Chung TY, Lo WH, Chen TH. The effect of posterior capsulorrhaphy in primary total hip arthroplasty: a prospective randomized study. J Arthroplasty. 2000;15:194–199. doi: 10.1016/S0883-5403(00)90220-1. [DOI] [PubMed] [Google Scholar]
- 3.Dixon MC, Scott RD, Schai PA, Stamos V. A simple capsulorrhaphy in a posterior approach for total hip arthroplasty. J Arthroplasty. 2004;19:373–376. doi: 10.1016/j.arth.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 4.Goldstein WM, Gleason TF, Kopplin M, Branson JJ. Prevalence of dislocation after total hip arthroplasty through a posterolateral approach with partial capsulotomy and capsulorrhaphy. J Bone Joint Surg Am. 2001;83(suppl 2 pt 1):2–7. doi: 10.2106/00004623-200100021-00002. [DOI] [PubMed] [Google Scholar]
- 5.Hedley AK, Hendren DH, Mead LP. A posterior approach to the hip joint with complete posterior capsular and muscular repair. J Arthroplasty. 1990;5(suppl):S57–S66. doi: 10.1016/S0883-5403(08)80027-7. [DOI] [PubMed] [Google Scholar]
- 6.Malkani AL, Ong KL, Lau E, Kurtz SM, Justice BJ, Manley MT. Early- and late-term dislocation risk after primary hip arthroplasty in the Medicare population. J Arthroplasty. 2010;25(6 suppl):21–25. doi: 10.1016/j.arth.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 7.Moore AT. The Moore self-locking vitallium prosthesis in fresh femoral neck fractures: a new low posterior approach (the southern exposure) Instr Course Lect. 1959;16:309. [Google Scholar]
- 8.Pagnano MW, Trousdale RT, Meneghini RM, Hanssen AD. Slower recovery after two-incision than mini-posterior-incision total hip arthroplasty: surgical technique. J Bone Joint Surg Am. 2009;91(1):50–73. doi: 10.2106/JBJS.H.01531. [DOI] [PubMed] [Google Scholar]
- 9.Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res. 1998;355:224–228. doi: 10.1097/00003086-199810000-00023. [DOI] [PubMed] [Google Scholar]
- 10.Stähelin T, Drittenbass L, Hersche O, Miehlke W, Munzinger U. Failure of capsular enhanced short external rotator repair after total hip replacement. Clin Orthop Relat Res. 2004;420:199–204. doi: 10.1097/00003086-200403000-00028. [DOI] [PubMed] [Google Scholar]
- 11.Tsai SJ, Wang CT, Jiang CC. The effect of posterior capsule repair upon post-operative hip dislocation following primary total hip arthroplasty. BMC Musculoskelet Disord. 2008;9:29. doi: 10.1186/1471-2474-9-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.White RE, Jr, Forness TJ, Allman JK, Junick DW. Effect of posterior capsular repair on early dislocation in primary total hip replacement. Clin Orthop Relat Res. 2001;393:163–167. doi: 10.1097/00003086-200112000-00019. [DOI] [PubMed] [Google Scholar]