Abstract
Background
Acetabular component position is associated with joint function and bearing wear. Current techniques for determining acetabular component version on standard radiographs lack reliability. Other, more consistent techniques are time-consuming and require additional equipment or software.
Questions/purposes
We compared three methods of acetabular component position assessment: (1) Einzel-Bild-Roentgen-Analyse (EBRA), (2) Woo and Morrey, and (3) the new ischiolateral method.
Patients and Methods
We assessed axial component position for 52 hips, with at least three radiographic series, using EBRA, and on true lateral radiographs using the Woo and Morrey method and a new method that uses the ischium as a skeletal landmark, the ischiolateral method.
Results
The mean SDs of the ischiolateral (2.15°) and EBRA (2.06°) methods were lower than that of the Woo and Morrey method (3.65°) but were not different from one another. We observed a SD of greater than 4° in 19 (36.5%) hip series using the Woo and Morrey method, compared to six series (11.5%) for both the ischiolateral and EBRA methods. Twenty-four (12.6%) Woo and Morrey measurements were greater than 4° from the mean for the hip series, compared to seven (3.8%) for ischiolateral and nine (4.7%) for EBRA. The intraclass correlation coefficients for intra- and interobserver reliability for the ischiolateral method and EBRA were the same (0.9).
Conclusions
Referencing the ischium standardizes pelvic position on each lateral radiograph and provides a simple and reliable means to assess axial component position, which is a surrogate for the planar anteversion measured by EBRA.
Introduction
For all bearings, both the acetabular component lateral opening angle and the acetabular component version have been related to multiple clinical outcome measures, including ROM, stability, wear, squeaking of ceramic-ceramic bearings, ion levels in metal-metal bearings, and clinical failure [2, 7–11, 18, 19]. Plain radiographs remain the primary skeletal imaging modality for arthritis and the postoperative assessment of total joint arthroplasty. Surgeons commonly measure the acetabular component abduction or lateral opening angle on an AP projection as the angle between the interteardrop line (a skeletal reference on the image) and the line tangent to the opening of the acetabular component [12]. The method and validity of edge detection software (Einzel-Bild-Roentgen-Analyse [EBRA]; University of Innsbruck, Innsbruck, Austria) have been previously reported [8]. EBRA is a valid method of acetabular component position assessment (abduction angle and version) on digital AP films but is not available to all practitioners and is relatively time-consuming. Further, it is difficult to distinguish a small degree of anteversion from a small degree of retroversion with EBRA, but it is obvious on a true lateral radiograph [9].
Murray [14] defined three types of anteversion: anatomic, radiographic, and direct observation at surgery. True lateral radiographs, as described by Johnson [5] and Danelius and Miller [3], display the hip and pelvis at 90° from the AP radiograph and are used to assess the anterior (or posterior) opening angle of the acetabular component, which is a surrogate for version [8, 12, 20]. This projection shows the component position in the axial plane and the potential for femoral-acetabular impingement, which influences ROM and joint stability [3, 5, 6]. Further, this projection shows femoral-acetabular meeting at 90° from the AP radiograph for the assessment of the bearing contact area [9].
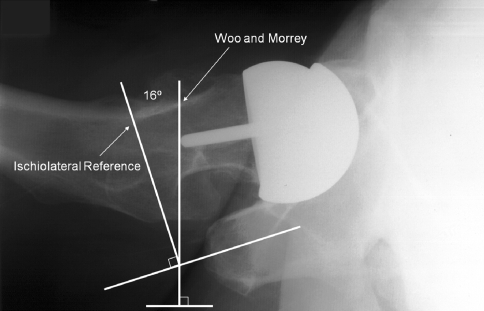
The Woo and Morrey [20] method measures component position on true lateral radiographs as the angle formed when a tangential line to the opening of the acetabulum and a line drawn perpendicular to the horizontal edge of the radiograph intersect (Fig. 1). Pulos et al. [16] demonstrate, similar to what is commonly done with the interteardrop line on AP films, the long axis of the ischial tuberosity is used as a skeletal landmark on a true lateral radiograph. The ischiolateral method improves measurement consistency by reducing variation due to pelvic position of the radiograph.
Fig. 1.
This radiograph shows the Woo and Morrey method for determining component position using the horizontal film edge as the reference. The ischiolateral method uses the long axis of the ischium. Reproduced from Pulos N, Tiberi JV 3rd, Schmalzried TP. Measuring acetabular component position on lateral radiographs: ischio-lateral method. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S84–S89. With permission.
While the ischiolateral method is reportedly more consistent than the Woo and Morrey method [16], it has not been compared to modern measurement tools, such as EBRA. Similarly, while the validity of EBRA has been reported in the literature [8], it has not been directly compared to other methods. We therefore compared three methods of acetabular component position assessment: (1) EBRA, (2) the Woo and Morrey method [20], and (3) the ischiolateral method [16].
Patients and Methods
We analyzed all 52 hips in 51 patients implanted with the same cobalt-chromium alloy hip resurfacing prosthesis with a cementless acetabular component (ASRTM; DePuy, Leeds, UK) implanted between November 8, 2004, and June 25, 2007. Each hip had at least three postoperative radiograph series, including an AP pelvis and a Danelius-Miller [3] true lateral, taken at different times (approximately 6 weeks, 6 months, and 1 year postoperatively). Thirty-four of the 52 hips had a fourth examination at about 2 years postoperatively. There were 31 men and 20 women.
The EBRA software package determines acetabular component position via edge detection on the AP pelvis radiograph. Using multiple points from the peripheral surfaces of the femoral and acetabular components, EBRA creates an acetabular component ellipse with a center that overlaps the center of rotation. The software calculates a measurement for both acetabular inclination and version.
For the Woo and Morrey method, we drew two lines on a Danelius-Miller lateral radiograph. We drew the reference line perpendicular to the horizontal plane or border of the radiograph and drew the second line as a tangent to the opening of the acetabular component. Then, we measured the angle between these lines to determine axial acetabular component position (Fig. 1) [20].
For the ischiolateral method, we drew the reference line perpendicular to the long axis of the ischial tuberosity on the Danelius-Miller [3] lateral radiograph. We drew the tangent to the opening of the acetabular component the same as the Woo and Morrey method [20] described and measured the angle between these lines to determine axial acetabular component position (Fig. 1) [16].
We analyzed a total of 190 lateral and 190 AP radiographs. A single observer (NP) measured acetabular component position for each of the three methods for each radiographic series. For each hip, the observer calculated a mean component position angle and SD for each method using the corresponding radiograph taken at different times. In seven (3.7%) films, the ischiolateral method could not be used to measure the angle. For five (2.6%) of these, the ischial tuberosity was outside the image. For the other two (0.5%), we could not clearly see the ischial tuberosity due to insufficient contrast. For each projection, we randomly selected 50 radiographs, which were reevaluated by the original observer at a separate setting and then assessed in the same way by a different observer (MK). We evaluated intra- and interobserver reliability for each method using the intraclass correlation coefficient (ICC) [17]. Three separate linear regression analyses were performed to evaluate corresponding measurements between techniques.
We used a paired two-sample t test with a hypothesized mean difference of zero to compare each method to the two other methods.
Results
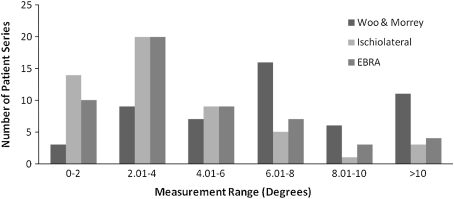
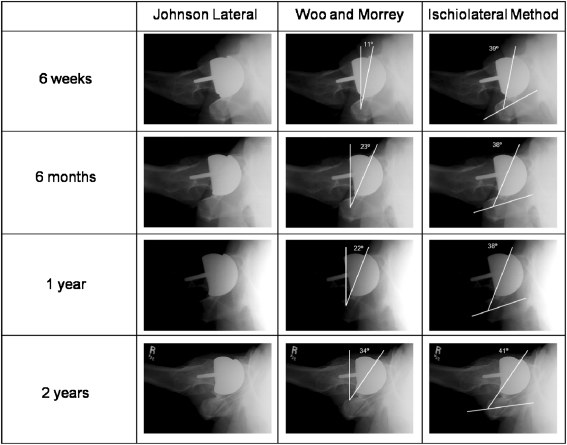
The Woo and Morrey method had a higher (p < 0.001) mean SD of the anteversion measurements than both the ischiolateral and EBRA methods. The mean SDs of the ischiolateral and EBRA methods, however, were similar (p = 0.78) (Table 1). Using the Woo and Morrey method, there were far more radiographic series with anteversion measurement SDs of greater than 4° compared to both the ischiolateral (p = 0.003) and EBRA (p = 0.003) methods. Similarly, there were more angles measured greater than 4° from the mean using the Woo and Morrey method than using either the ischiolateral (p < 0.001) or EBRA (p < 0.001) method. None of the comparisons between the ischiolateral and EBRA methods differed (Table 1). While the ischiolateral and EBRA methods were similarly precise, the Woo and Morrey method had more patient series with measurement ranges of greater than 6° (Fig. 2). For example, the acetabular component anteversion measured in one patient’s hip was 27°, 37°, and 36° at 6-week, 6-month, and 1-year followup, respectively, using the Woo and Morrey method whereas anteversion measured 53°, 53°, and 55° for the same times using the ischiolateral method on the same set of films (Fig. 3). Linear regression showed all three measurements were correlated with the ischiolateral measurements nominally about 26° higher than EBRA and 2° lower than Woo and Morrey. The ICCs for intra- and interobserver reliability for the ischiolateral method (0.9 and 0.9, respectively) and EBRA (0.9 and 0.9, respectively) were the same (Table 1).
Table 1.
Statistical comparisons for the Woo and Morrey, ischiolateral, and EBRA methods
| Variable | Woo and Morrey | Ischiolateral | EBRA | p Value | ||
|---|---|---|---|---|---|---|
| Woo and Morrey versus ischiolateral | Woo and Morrey versus EBRA | Ischiolateral versus EBRA | ||||
| Mean SD of anteversion measurements | 3.7° | 2.2° | 2.1° | < 0.001 | < 0.001 | 0.78 |
| Number of hips with SD > 4° (n = 52 hips) | 19 (36.5%) | 6 (11.5%) | 6 (11.5%) | 0.003 | 0.003 | 1 |
| Number of measurements > 4° from mean (n = 190 radiographs) | 24 (12.6%) | 7 (3.8%) | 9 (4.7%) | < 0.001 | < 0.001 | 0.66 |
| ICC for intraobserver reliability | 0.9 | 0.9 | ||||
| ICC for interobserver reliability | 0.9 | 0.9 | ||||
EBRA = Einzel-Bild-Roentgen-Analyse; ICC = intraclass correlation coefficient.
Fig. 2.
This graph demonstrates the distribution of the range of angles measured for each hip series.
Fig. 3.
This figure compares the Woo and Morrey and ischiolateral methods performed on radiographs taken at different periods in the postoperative care from the same patient. Reproduced from Pulos N, Tiberi JV 3rd, Schmalzried TP. Measuring acetabular component position on lateral radiographs: ischio-lateral method. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S84–S89. With permission.
Discussion
The importance of acetabular component position in the outcomes of hip arthroplasty, including ROM, stability, wear, squeaking of ceramic-ceramic bearings, ion levels in metal-metal bearings, and overall implant survival, has been previously described [2, 7–11, 18, 19]. The ideal method for evaluating acetabular component position would be one that is readily available, consistent and reproducible, inexpensive, quick, and easy to interpret. Such a technique is frequently employed for measuring abduction by referencing the interteardrop line; however, previously described methods for anteversion utilize external references, sacrificing reproducibility, or sophisticated equipment or software, sacrificing time, availability, and cost. We compared three methods for measuring acetabular component anteversion, one new and two previously described, to determine whether a method using readily available tools could be comparable in precision and validity to an advanced research tool such as EBRA.
Readers should be aware of limitations to our study. First, we used a series of radiographs made at different points in time for each patient, which assumes component position has not changed over time. To minimize confounding factors, one would analyze several different radiographs made at the same point in time; however, such a study would not be possible due to the unjustified radiation exposure for each patient. Further, all radiographs were within the 2-year postoperative period, an early timeframe for hip arthroplasty, and each patient had no identifiable sign or symptom of loosening. Second, there are also limitations to each of the three methods evaluated by this study. For the Woo and Morrey method, decreased reliability due to the use of an external reference was confirmed by our results. The availability, cost, and time consumption limitations of the EBRA method have been previously discussed. A specific limitation of the ischiolateral method identified during our study is that the ischium must be clearly visible on the lateral radiograph. All of the radiographs were taken before the initiation of this study and the technicians had not received any specific instructions regarding inclusion of the ischium. Despite this, only seven (3.7%) films did not include the ischium. Inclusion of the ischium on the radiograph is not technically demanding. Discussion with technicians regarding the importance of including the ischium on this view can reduce or eliminate the number of unusable films.
The most common way to evaluate acetabular component position on a lateral radiograph is to use the horizontal film edge as a reference [20]. The mean SD of this method in our study was 3.7°. Using the same method, Pollard et al. [15] found a mean SD of 4°. In this study, the ischiolateral method, using an internal skeletal landmark, had a mean SD of 2.2°. The reproducibility of the ischiolateral method compares well to the previously validated EBRA digital edge detection method [8].
In another radiographic study, Hing et al. [4] used an ICC of greater than 0.6 to represent substantial agreement and an ICC of greater than 0.9 to represent excellent agreement, while an ICC equaling 1.0 represented perfect agreement. On this basis, the intra- and interobserver reliabilities of the ischiolateral method are excellent and equivalent to EBRA. Thus, the ischiolateral method is an equally reliable way of measuring component position.
The absolute value of the angle measured with the ischiolateral method was larger than that obtained using the Woo and Morrey method, larger than the planar anteversion measured by EBRA, and larger than the surgical anteversion of that hip. Surgical anteversion is the angle between the frontal plane of the patient and the perpendicular to the face of the acetabular component [13]. When a patient lies supine, the ischial tuberosity points slightly downward into the table (rather than parallel to it), creating a larger measurement angle with the ischiolateral method. Linear regression analysis of our data demonstrated ischiolateral measurements of our data are approximately 26° higher than corresponding EBRA measurements.
Practically, the ischiolateral method is analogous to what is commonly done on AP radiographs, where the interteardrop line is a pelvic reference for the measurement of the acetabular component abduction angle [12]. Similarly, using the long axis of the ischium as a pelvic reference on the lateral radiograph decreases variability of the measurement due to differences in pelvic tilt, which can vary temporally [1]. The ischiolateral method provides a more consistent measurement by decreasing the number of outlier angles (Fig. 2). It is as consistent and has intra- and interobserver reliability equivalent to EBRA.
In conclusion, the ischiolateral measurement has precision and validity equivalent to EBRA and is more precise and valid for multiple observers than the historical method of Woo and Morrey. Although the nominal angles of component position measured on the true lateral and AP films are different, they correlate. The ischiolateral measure minus 26° closely approximates the planar anteversion measured by EBRA. The benefits of the ischiolateral method are that it requires no special software, can be performed on a conventional film or a digital image, and is simple and quick. With an increased appreciation for the importance of anteversion, the ischiolateral method provides a quick, low-cost, consistent, and reliable means to assess axial component position, which is a surrogate for the planar anteversion measured with EBRA.
Acknowledgment
The authors thank Mylene dela Rosa, BS, CCRP, for her assistance in the collection of data and materials on this project.
Footnotes
The institution of one or more of the authors (TPS) has received funding from DePuy Orthopaedics Inc (Warsaw, IN). One or more of the authors (TPS) have received royalties and consultant fees from DePuy Orthopaedics.
This study was approved and qualified as exempt by the Institutional Review Board of St Vincent Medical Center, where all study participants were evaluated.
This work was performed at the Joint Replacement Institute at St Vincent Medical Center.
An erratum to this article can be found at http://dx.doi.org/10.1007/s11999-012-2249-z.
References
- 1.Arai N, Nakamura S, Matsushita T. Difference between 2 measurement methods of version angles of the acetabular component. J Arthroplasty. 2007;22:715–720. doi: 10.1016/j.arth.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 2.Barrack RL, Schmalzried TP. Impingement and rim wear associated with early osteolysis after a total hip replacement. J Bone Joint Surg Am. 2002;84:1218–1220. doi: 10.2106/00004623-200207000-00021. [DOI] [PubMed] [Google Scholar]
- 3.Danelius G, Miller LF. Lateral view of the hip. AJR Am J Roentgenol. 1936;35:282–284. [Google Scholar]
- 4.Hing CB, Back DL, Bailey M, Young DA, Dalziel RE, Shimmin AJ. The results of primary Birmingham hip resurfacings at a mean of five years: an independent prospective review of the first 230 hips. J Bone Joint Surg Br. 2007;89:1431–1438. doi: 10.1302/0301-620X.89B11.19336. [DOI] [PubMed] [Google Scholar]
- 5.Johnson CR. A new method for roentgenographic examination of the upper end of the femur. J Bone Joint Surg. 1932;14:859–866. [Google Scholar]
- 6.Laage H, Barnett JC, Brady JM, Dulligan PJ, Jr, Fett HC, Gallagher TF, Schneider BA. Horizontal roentgenography of the hip in children. J Bone Joint Surg Am. 1953;35:387–398. [PubMed] [Google Scholar]
- 7.Langton DJ, Jameson SS, Joyce TJ, Hallab NJ, Natu S, Nargol AV. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg Br. 2010;92:38–46. doi: 10.1302/0301-620X.92B1.22770. [DOI] [PubMed] [Google Scholar]
- 8.Langton DJ, Jameson SS, Joyce TJ, Webb J, Nargol AV. The effect of component size and orientation on the concentrations of metal ions after resurfacing arthroplasty of the hip. J Bone Joint Surg Br. 2008;90:1143–1151. doi: 10.1302/0301-620X.90B9.20785. [DOI] [PubMed] [Google Scholar]
- 9.Langton DJ, Joyce TJ, Jameson SS, Lord J, Orsouw M, Holland JP, Nargol AV, Smet KA. Adverse reaction to metal debris following hip resurfacing: the influence of component type, orientation and volumetric wear. J Bone Joint Surg Br. 2011;93:164–171. doi: 10.1302/0301-620X.93B2.25099. [DOI] [PubMed] [Google Scholar]
- 10.Langton DJ, Sprowson AP, Mahadeva D, Bhatnagar S, Holland JP, Nargol AV. Cup anteversion in hip resurfacing: validation of EBRA and the presentation of a simple clinical grading system. J Arthroplasty. 2010;25:607–613. doi: 10.1016/j.arth.2009.08.020. [DOI] [PubMed] [Google Scholar]
- 11.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217–220. [PubMed] [Google Scholar]
- 12.Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration: an experimental study. J Arthroplasty. 1989;4:245–251. doi: 10.1016/S0883-5403(89)80020-8. [DOI] [PubMed] [Google Scholar]
- 13.McKee GK. Development of total prosthetic replacement of the hip. Clin Orthop Relat Res. 1970;72:85–103. [PubMed] [Google Scholar]
- 14.Murray DW. The definition and measurement of acetabular orientation. J Bone Joint Surg Br. 1993;75:228–232. doi: 10.1302/0301-620X.75B2.8444942. [DOI] [PubMed] [Google Scholar]
- 15.Pollard JA, Daum WJ, Uchida T. Can simple radiographs be predictive of total hip dislocation? J Arthroplasty. 1995;10:800–804. doi: 10.1016/S0883-5403(05)80078-6. [DOI] [PubMed] [Google Scholar]
- 16.Pulos N, Tiberi JV, 3rd, Schmalzried TP. Measuring acetabular component position on lateral radiographs: ischio-lateral method. Bull NYU Hosp Jt Dis. 2011;69(Suppl 1):S84–S89. [PubMed] [Google Scholar]
- 17.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037/0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- 18.Walter WL, O’toole GC, Walter WK, Ellis A, Zicat BA. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty. 2007;22:496–503. doi: 10.1016/j.arth.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 19.Wan Z, Boutary M, Dorr LD. The influence of acetabular component position on wear in total hip arthroplasty. J Arthroplasty. 2008;23:51–56. doi: 10.1016/j.arth.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 20.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]