Abstract
Background
Use of the Ilizarov technique for limb lengthening in patients with achondroplasia is controversial, with a high risk of complications balancing cosmetic gains. Although several articles have described the complications of this procedure and satisfaction of patients after surgery, it remains unclear whether lengthening improves the quality of life (QOL) of these patients.
Questions/purposes
We asked whether bilateral lower limb lengthenings with deformity correction in patients with achondroplasia would improve QOL and investigated the correlation between complication rate and QOL.
Patients and Methods
We retrospectively reviewed 22 patients (average age, 12.7 years) diagnosed with achondroplasia who underwent bilateral lower limb lengthenings between 2002 and 2005. These patients were compared with 22 patients with achondroplasia for whom limb lengthening was not performed. The two groups were assessed using the American Academy of Orthopaedic Surgeons (AAOS) lower limb, SF-36, and Rosenberg self-esteem scores. Minimum followup was 4.5 years (range, 4.5–6.9 years).
Results
Among the lengthening group, the average gain in length was 10.21 ± 2.39 cm for the femur and 9.13 ± 2.12 cm for the tibia. A total of 123 complications occurred in these 88 segments. The surgical group had higher Rosenberg self-esteem scores than the nonsurgical group although there were no differences in the AAOS and the SF-36 scores. The self-esteem scores decreased with the increase in the number of complications.
Conclusions
Our data suggest that despite frequent complications, bilateral lower limb lengthening increases patients’ QOL. We believe lengthening is a reasonable option in selected patients.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Achondroplasia is the most frequently encountered form of nonlethal skeletal dysplasia [4] and is characterized by defective enchondral ossification owing to defective gene encoding for fibroblast growth factor receptor 3 [6, 14, 20]. It is a type of rhizomelic dwarfism with an incidence of approximately one in 10,000 live births [6]. In addition to short stature, individuals with achondroplasia often have substantial angular deformities of the limbs, spinal problems, and other neurologic and craniofacial abnormalities develop [5, 9].
Achondroplastic dwarfism results in considerable physical and psychologic handicaps owing to the disproportionate stature of the body and difficulty in performing routine activities of daily living [1, 6]. These individuals often feel ‘different’ from their families and circle of friends, often suffer from emotional disturbances, and are prone to have inferiority complexes [6]. They also have major musculoskeletal problems including symptomatic malalignment of the lower limbs. Some patients eventually undergo surgical correction of their malalignment to decrease pain and prevent early-onset degenerative arthritis [12, 14].
Limb lengthening by the Ilizarov method has been used in patients with achondroplasia by many authors during the past few decades, but with varying amounts of success [2, 3, 6, 8, 13, 16, 18, 20]. Cattaneo et al. [6] reported a considerable increase in length (14–18 cm) without major risk. Lavini et al. [13] and Aldegheri and Dall’Oca [2] reported 85% to 95% of the patients were satisfied with the surgery and perceived an improved psychologic and emotional state, even when complications delayed the completion of treatment [2]. Owing to its modularity and versatility, the Ilizarov method can simultaneously address limb shortening and angular deformities in these individuals [20]. Although these reports describe the technique and the concerns with the use of the Ilizarov technique, none has described whether this operation enhances QOL for these patients.
Therefore, we reviewed the complications associated with bilateral lower limb lengthening in patients with achondroplasia and asked the following questions: (1) Does QOL increase in terms of the AAOS lower extremity, SF-36, and Rosenberg self-esteem scores after surgery as compared with QOL for patients not surgically treated? (2) Does the QOL correlate with the complications experienced by the patients?
Patients and Methods
We retrospectively reviewed all 22 patients (88 segments) with achondroplasia who underwent bilateral tibial lengthenings with the Ilizarov ring fixator and bilateral femoral lengthenings with the monolateral external fixator between January 2002 and December 2005. The patients were derived from those who were referred to our institution through the Little People Society of Korea. These patients and their parents were counseled regarding the surgical process and its complications and only those willing were prepared for surgery. The indication for this primarily cosmetic surgery was any patient of clinically and/or genetically proved achondroplasia who was willing to undergo surgery for limb lengthening. The contraindications for surgery were: (1) patients and parents who were unwilling to have surgery, (2) patients with a medical contraindication (eg, heart disease, restrictive or obstructive lung diseases, and neurologic issues like cervicomedullary compression) for surgery, and (3) patients with the possibility of intramedullary infection. The average age of the patients at the time of surgery was 12.7 years (range, 8–25 years). There were seven males and 15 females. The average preoperative height was 121.8 cm (range, 104–132.8 cm). All the patients underwent bilateral tibial lengthenings first, after which bilateral femoral lengthenings were performed 6 to 22 months later. Minimum followup was 4.5 years (average, 4.9 years; range, 4.5–6.9 years). Preoperative QOL assessment was not performed because the age of the patients at the time of surgery was too young for validated questionnaires. Instead, the patients who underwent surgical lengthening were compared with 22 patients with the same diagnosis but who did not have surgical lengthening. For analysis, an equivalent number of control subjects who were case-matched according to age at the time of surgery, gender, and height were asked, through the Little People Society, to return for followup and were given questionnaires for measurement of QOL. Accordingly the average age of the patients who had surgery was 12.72 years and that of the patients without surgery was 12.54 years. The average height of the patients who had surgery was 121.81 cm whereas that of the patients without surgery was 120.09 cm. The number of patients who had surgery for all six bone lengthenings (humerus, femur, and tibia) was too small to consider in a separate analysis. No patient was lost to followup. No patients died and all were asked to return specifically for this study. All data were obtained from medical records and radiographs. Informed parental consent was obtained for children 16 years or younger for the procedure.
We used the Ilizarov ring fixator (U & I Co, Ltd, Seoul, Korea) for tibial lengthening and deformity correction. Three or four rings were used depending on whether unifocal or bifocal osteotomies were performed at the center of rotation of angulation (CORA) for gradual correction of the deformity and lengthening. Paired hinges were aligned with the apex of the deformity and a single lengthening rod was placed opposite them. We used two wires each at the proximal and distal rings. The proximal and distal tibiofibular joints were transfixed with a wire each to prevent distal or proximal migration of the fibula, respectively. We inserted two additional half pins at the proximal and middle rings. The osteotomy using the multiple drill hole method was performed at the level of the CORA. A monolateral external fixator was used for femoral lengthening. The reason for using the monolateral fixator for the femur instead of the Ilizarov ring fixator for the tibia was that the monolateral fixator is much more comfortable for patients without compromising much stability. Three or four Schanz screws were inserted in the proximal and distal ends of the femur perpendicular to the anatomic axis. A transverse osteotomy was performed at the middiaphyseal region in all cases after longitudinally incising the periosteum.
Lengthening with or without gradual correction of the deformity was started after 7 days at a rate of 1 mm/day (0.25 mm every 6 hours). The rate was adjusted during followups according to morphologic features of the callus as observed on radiographs. We removed the fixator when we observed three continuous cortices on the radiographs. A long leg cast was applied after fixator removal and was removed at 4 to 6 weeks. Postoperative radiographic angular measurements were based on immediate postremoval radiographs. All the radiographs were taken using StarPACS PiView STAR 5.0.6.0 software (Infinitt Healthcare Co, Seoul, Korea) with xray beams perpendicular to the center of the distraction site.
Patients underwent supervised daily physiotherapy including active and passive ROM of the knee and ankle beginning 2 days after surgery. Physiotherapy was performed twice per day for 2 hours during 2 weeks of admission and 1 hour per day after discharge until the end of the distraction phase. Partial weightbearing with two crutches for 4 hours a day was allowed during the distraction phase.
Patients were seen for followup at 2, 4, 6, and 8 weeks and then every month thereafter, with clinical and radiographic evaluations (ROM, deformity, and AP, lateral, and long leg standing radiographs). All patients were seen by the senior author (HRS) and examined for any signs of pin tract infection, ROM of adjoining joints, angulation or translation of the osteotomy site, and other complications that can occur during lengthening. We reviewed the medical records of all patients to obtain demographic data and other factors related to the treatment, including age at surgery, height, scheme of lengthening used, number of days of distraction, number of days required for maturation of the callus, and total duration of treatment. We calculated the lengthening percentage, fixator index, and bone healing index. We recorded any secondary operations. The complications were recorded according to the classification of Paley [15] (problems, obstacles, sequelae). Standard radiographs of both lower limbs were taken and were compared with the preoperative and immediate postoperative images. For QOL assessment, we used four validated questionnaires: (1) AAOS lower limb outcomes [11], (2) Rosenberg self-esteem [17], (3) SF-36 [10], and (4) Pediatric Quality of Life (PedsQL) [7] (for children between 8 and 12 years of age). The Rosenberg self-esteem scale is one of the most widely used measures of global self-esteem in social science research and has a set of 10 questions which are easy to complete, require just 1 to 2 minutes to complete, and are linked to self-competence and self-liking, both features that are very important in patients with achondroplasia. The AAOS lower limb score measures the ability of the patient to walk on flat surfaces, lower limb stiffness, swelling and pain, and the ability to ambulate with or without support. This score ranges from 0 to 44, with the QOL being worse as the score increases. The score is reportedly reliable, sensitive to changes in patient status, and comprehensively reflects the QOL in patients with various lower limb conditions [11]. The SF-36 score has eight sets of questions included in two groups: the Physical component summary (PCS) and Mental component summary (MCS), which together give a composite score. Thus this score effectively gives an idea regarding the physical and the mental QOL of the patients.
Three of us (SJK, GCB, HRS) independently measured the conventional mechanical axis deviation (MAD-C) or ground mechanical axis deviation (MAD-G) and tibia-femur angle on standard weightbearing full-length lower extremity radiographs to determine angular deformities of the knee. The MAD-C was measured as the distance between the center of the knee and a line drawn from the center of the femoral head to the center of the talus. The MAD-G was measured as the distance between the center of the knee and a line drawn from the center of the femoral head to that of the heel when in contact with the ground on long leg standing radiographs [20]. The difference between MAD-C and MAD-G is the result of inclusion of heel varus in the measurement of MAD-G. Heel varus or valgus was measured with the tibiocalcaneal angle on standing radiographs. We defined neutral alignment when the mechanical axis line drawn from the center of the femoral head to the center of the calcaneus (MAD-G line) passed through the 30%-lateral or medial plateau region measured between the center of the knee and medial or lateral edges of the medial or lateral plateau. Valgus or varus was defined as when the MAD-G line passed through greater than 30% of the lateral or medial plateau region. Valgus or varus ankle was defined when the tibiocalcaneal angle on standing radiographs was greater than ± 5°. The average gain in length as measured on radiographs was 10.2 ± 2.4 cm in the femur and 9.1 ± 1.98 cm in the tibia. The mean lengthening percentage was 35.5% (range, 14%–65%) in the femur and 37.2% (range, 15%–67%) in the tibia. The mean external fixator index was 33 days/cm (range, 21–84 days/cm) in the femur and 28 days/cm (range, 11–80 days/cm) in the tibia. The mean healing index was 34 days/cm (range, 17–80 days/cm) in the femur and 35 days/cm (range, 15–90 days/cm) in the tibia. Radiographic parameters were tested for reproducibility by interobserver studies using Pearson correlation coefficients; the correlation coefficients ranged from 0.871 to 0.969.
The lengthening and various indices were described by a mean ± SD. The differences in the mean AAOS lower extremity scores between preoperatively and postoperatively were analyzed using the Mann-Whitney test. Rosenberg self-esteem scores, PedsQL scores, and SF-36 scores were analyzed using the two-tailed test. The patients who had surgery also were divided into two groups for statistical analysis: Group I (nine patients) who had four or fewer complications and Group II (13 patients) who had more than four complications. Two additional groups were created for those with complications without sequelae (Group A, seven patients) or complications with sequelae (Group B, 15 patients). The data were recorded using Microsoft® Excel® 2007 version (Microsoft Corp, Redmond, WA, USA) and analyzed using SPSS® software (SPSS Inc, Chicago, IL, USA).
Results
The mean AAOS scores were similar (p = 0.645) for the two groups: 17.3 ± 8.2 for the surgical group and 16.95 ± 5.75 for the nonsurgical group. The Rosenberg score was higher (p < 0.001) for the surgical than for the nonsurgical group: 22.1 ± 2.5 versus 19 ± 1.6, respectively (Table 1). The nonsurgical group had higher (p = 0.051) SF-36 scores than the surgical group in the PCS score: 45.04 ± 16.8 for the surgical group and 55.63 ± 15.38 for the nonsurgical group. However the mean overall SF-36 scores were similar ((p = 0.307): 52.77 ± 17.43 for the surgical group and 57.81 ± 16.82 for the nonsurgical group (Table 2).
Table 1.
Results of the questionnaire
| Variable | Patients who had surgery | Patients without surgery | p Values |
|---|---|---|---|
| Age | 12.72 ± 4.68 years | 12.54 ± 4.55 years | p = 0.898 |
| Preoperative height | 121.84 ± 8.24 cm | 120.09 ± 7.43 cm | p = 0.463 |
| Rosenberg score | 22.1 ± 2.5 | 19 ± 1.6 | p < 0.001 |
| AAOS score | 17.27 ± 8.16 | 16.95 ± 5.75 | p = 0.645 |
| SF-36 score | 52.77 ± 17.43 | 57.81 ± 16.82 | p = 0.307 |
Table 2.
Summary of the Short Form-36 scores
| Component | Patients who had surgery | Patients without surgery |
|---|---|---|
| Physical component summary | ||
| Mean | 45.04 | 55.63 |
| Standard deviation | 16.8 | 15.38 |
| Standard error of the mean | 3.58 | 3.27 |
| p Value | 0.0508 | |
| Mental component summary | ||
| Mean | 56.86 | 55.18 |
| Standard deviation | 14.33 | 14.53 |
| Standard error of the mean | 3.05 | 3.09 |
| p Value | 0.6444 | |
| Total component summary | ||
| Mean | 52.77 | 57.81 |
| Standard deviation | 17.43 | 16.82 |
| Standard error of the mean | 3.71 | 3.58 |
| p Value | 0.3078 | |
Group I with four or fewer complications had a higher (p = 0.001) Rosenberg self-esteem score (23) than Group II with more than four complications (20), suggesting fewer complications could improve QOL after surgery. Group A without sequelae had a higher (p < 0.001) Rosenberg self-esteem score (22) than Group B with one or more sequelae (19.5). There was no difference between the two groups in PedsQL scores.
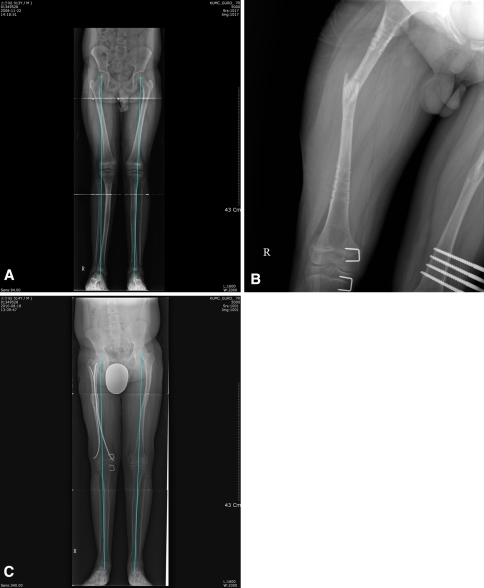
A total of 123 complications were encountered in 88 segments. Joint complications were seen in 70 (57%) segments (including hip flexion contractures in 68% of patients who had surgery for femoral lengthening, but the patients recovered considerably with minor muscle releases and physiotherapy), and bony complications in 47 (38%) segments (Fig. 1). The hip flexion contractures and increased lumbar lordosis were not severe enough to warrant any more bony procedures, such as subtrochanteric extension osteotomy. The contractures were treated with minor soft tissue releases with minimal morbidity to the patients without any effect on their activities. Other minor complications (problems) were seen in six (5%) segments and properly dealt with in the outpatient clinic.
Fig. 1A–C.
(A) A standing full-length lower extremity radiograph of a 10-year-old boy with achondroplasia shows genu valgum deformity on the left side after tibia lengthening. (B) A radiograph shows refracture of the femur after lengthening. (C) The latest radiograph after hemiepiphysiodesis shows the malalignment was corrected, but a 2.5-cm limb length discrepancy remained. A flexible nail was inserted owing to refracture of the femur.
Discussion
The ability of the Ilizarov technique to lengthen both lower limbs in patients with achondroplasia and other causes of short stature has been confirmed in several studies [3, 8, 16, 18]. However, the basic concept of lengthening in patients with achondroplasia is a contentious issue. Although there is no doubt the total height of the patient can be increased, it is unclear whether the lengthening influences patient function or QOL. Further, the long arduous nature of the treatment and considerable potential for immediate and long-term complications make it a controversial technique [19]. We therefore asked the following questions: (1) Does QOL increase after surgery in parameters such as the AAOS lower extremity, SF-36, and Rosenberg self-esteem scores? (2) Is there any correlation between the complication rate and QOL of the patients?
Our study has some limitations. First, the number of patients studied is relatively small, as the number of patients who have had surgery for all four bone lengthenings is limited even in a tertiary care referral institute like ours. Second, although we attempted to make the two groups as equivalent as possible as far as the age-gender structure or the average pretreatment height is concerned, there may be certain dissimilarities in the two groups as far as the severity of the disease is concerned, as the more severely affected individuals are more likely to be willing to undergo lengthening. Third, we have not taken into account other factors that affect QOL in patients with achondroplasia, such as spinal problems and neurologic disorders.
Even with numerous complications, our data show serial lower limb lengthening is a good option for patients with achondroplasia in terms of good QOL scores. The patients who had surgery for lengthening scored well in the mental component of the SF-36 and in the Rosenberg self-esteem questionnaire. The physical and functional scores of the patients who had surgery were equivalent to those of the nonsurgical group as shown by the AAOS lower extremity scores and the physical component of the SF-36. Such a discrepancy was expected as long and complicated procedures such as bilateral limb lengthenings are likely to have some sequelae in the form of decreased ROM and residual deformities and thus will cause a resultant decrease in the functional score. The physical and mental health scores were directly related to the number of complications seen, as the Rosenberg self-esteem and SF-36 scores were reduced as the number of complications increased to more than four.
Various studies have explored the causes of complications of extensive limb lengthening in patients with achondroplasia and have tried to show their effect on patient satisfaction and function, although they have not explained the same in QOL terms. Lavini et al. [13] and Aldegheri and Dall’Oca [2] reported 85% to 95% of the patients were satisfied with the surgery. They reported no major complications and the patients had resumed a normal social life after lower limb lengthening. Similarly, Vargas Barreto et al. [21] showed, in their study of 22 patients with achondroplasia, their procedures in these patients were as good as those for patients with leg length discrepancy, and all patients who had no or only minor complications were satisfied with their results. Although there was a relatively higher number of complications in our patients as compared with those of other studies, the reason for this discrepancy may be that we used the term “complication” in a very strict manner and included even minor complications that did not require any treatment and did not cause any sequelae. Although it is likely that relatively minor complications such as persistent minor malalignments of the joints might cause long-term complications such as early osteoarthritis later in life, we believe better QOL in the productive years was more important than the risk of degenerative joint disease in later years.
Our study thus suggests that bilateral limb lengthening can be a reasonable option for patients with achondroplasia, provided the patients are carefully monitored for complications and they are promptly addressed when they occur. We believe that our study is a valuable addition to the current literature for this subject, which is lacking in QOL and functional assessments of these patients. However, further multicenter studies are needed to establish objective guidelines for proper patient selection or protocols for evaluation of surgical complications and QOL before this method attains widespread use.
Footnotes
This study was supported by a grant of the Korea Healthcare technology R&D Project, Ministry of Health & Welfare, Republic of Korea (A110416).
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
References
- 1.Adelson BM. The Lives of Dwarves: Their Journey From Public Curiosity Toward Social Liberation. New Brunswick, NJ: Rutgers University Press; 2005. [Google Scholar]
- 2.Aldegheri R, Dall’Oca C. Limb lengthening in short stature patients. J Pediatr Orthop B. 2001;10:238–247. doi: 10.1097/00009957-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 3.Aldegheri R, Trivella G, Renzi-Brivio L, Tessari G, Agostini S, Lavini F. Lengthening of the lower limbs in achondroplastic patients: a comparative study of four techniques. J Bone Joint Surg Br. 1988;70:69–73. doi: 10.1302/0301-620X.70B1.3339063. [DOI] [PubMed] [Google Scholar]
- 4.Bulas DI, Fonda JS. Prenatal evaluation of fetal anomalies. Pediatr Clin North Am. 1997;44:537–553. doi: 10.1016/S0031-3955(05)70492-2. [DOI] [PubMed] [Google Scholar]
- 5.Carter EM, Davis JG, Raggio CL. Advances in understanding etiology of achondroplasia and review of management. Curr Opin Pediatr. 2007;19:32–37. doi: 10.1097/MOP.0b013e328013e3d9. [DOI] [PubMed] [Google Scholar]
- 6.Cattaneo R, Villa A, Catagni M, Tentori L. Limb lengthening in achondroplasia by Ilizarov’s method. Int Orthop. 1988;12:173–179. doi: 10.1007/BF00547160. [DOI] [PubMed] [Google Scholar]
- 7.Davis SE, Hynan LS, Limbers CA, Andersen CM, Greene MC, Varni JW, Iannaccone ST. The PedsQL in pediatric patients with Duchenne muscular dystrophy: feasibility, reliability, and validity of the Pediatric Quality of Life Inventory Neuromuscular Module and Generic Core Scales. J Clin Neuromuscul Dis. 2010;11:97–109. doi: 10.1097/CND.0b013e3181c5053b. [DOI] [PubMed] [Google Scholar]
- 8.Bastiani G, Aldegheri R, Trivella G, Renzi-Brivio L, Agostini S, Lavini F. Lengthening of the lower limbs in achondroplastics. Basic Life Sci. 1988;48:353–355. doi: 10.1007/978-1-4684-8712-1_46. [DOI] [PubMed] [Google Scholar]
- 9.Haga N. Management of disabilities associated with achondroplasia. J Orthop Sci. 2004;9:103–107. doi: 10.1007/s00776-003-0729-4. [DOI] [PubMed] [Google Scholar]
- 10.Jenkinson C, Wright L, Coulter A. Criterion validity and reliability of the SF-36 in a population sample. Qual Life Res. 1994;3:7–12. doi: 10.1007/BF00647843. [DOI] [PubMed] [Google Scholar]
- 11.Johanson NA, Liang MH, Daltroy L, Rudicel S, Richmond J. American Academy of Orthopaedic Surgeons lower limb outcomes assessment instruments: reliability, validity, and sensitivity to change. J Bone Joint Surg Am. 2004;86:902–909. doi: 10.2106/00004623-200405000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Kopits SE. Orthopedic aspects of achondroplasia in children. Basic Life Sci. 1988;48:189–197. doi: 10.1007/978-1-4684-8712-1_28. [DOI] [PubMed] [Google Scholar]
- 13.Lavini F, Renzi-Brivio L, Bastiani G. Psychologic, vascular, and physiologic aspects of lower limb lengthening in achondroplastics. Clin Orthop Relat Res. 1990;250:138–142. [PubMed] [Google Scholar]
- 14.Lee ST, Song HR, Mahajan R, Makwana V, Suh SW, Lee SH. Development of genu varum in achondroplasia: relation to fibular overgrowth. J Bone Joint Surg Br. 2007;89:57–61. doi: 10.1302/0301-620X.89B1.18223. [DOI] [PubMed] [Google Scholar]
- 15.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 16.Peretti G, Memeo A, Paronzini A, Marzorati S. Staged lengthening in the prevention of dwarfism in achondroplastic children: a preliminary report. J Pediatric Orthop B. 1995;4:58–64. doi: 10.1097/01202412-199504010-00009. [DOI] [PubMed] [Google Scholar]
- 17.Rosenberg M. Society and the Adolescent Self-Image. Princeton, NJ: Princeton University Press; 1965.
- 18.Saleh M, Hamer AJ. Bifocal limb lengthening: a preliminary report. J Pediatr Orthop B. 1993;2:42–48. doi: 10.1097/01202412-199302010-00008. [DOI] [Google Scholar]
- 19.Trotter TL. Hall JG; American Academy of Pediatrics Committee on Genetics. Health supervision for children with achondroplasia. Pediatrics. 2005;116:771–783. doi: 10.1542/peds.2005-1440. [DOI] [PubMed] [Google Scholar]
- 20.Vaidya SV, Song HR, Lee SH, Suh SW, Keny SM, Telang SS. Bifocal tibial corrective osteotomy with lengthening in achondroplasia: an analysis of results and complications. J Pediatr Orthop. 2006;26:788–793. doi: 10.1097/01.bpo.0000242429.83866.97. [DOI] [PubMed] [Google Scholar]
- 21.Vargas Barreto B, Caton J, Merabet Z, Panisset JC, Pracros JP. Complications of Ilizarov leg lengthening: a comparative study between patients of leg length discrepancy and short stature. Int Orthop. 2007;31:587–591. doi: 10.1007/s00264-006-0236-2. [DOI] [PMC free article] [PubMed] [Google Scholar]