Abstract
Background
While the primary objective of joint arthroplasty is to improve patient quality of life, pain, and function, younger active patients often demand a return to higher function that includes sporting activity. Knowledge of rates and predictors of return to sports will help inform expectations in patients anticipating return to sports after joint arthroplasty.
Questions/purposes
We measured the rate of sports participation at 1 year using the UCLA activity score and explored 11 variables, including choice of procedure/prosthesis, that might predict return to a high level of sporting activity, when controlling for potential confounding variables.
Methods
We retrospectively evaluated 736 patients who underwent primary metal-on-polyethylene THA, metal-on-metal THA, hip resurfacing arthroplasty, revision THA, primary TKA, unicompartmental knee arthroplasty, and revision TKA between May 2005 and June 2007. We obtained UCLA activity scores on all patients; we defined high activity as a UCLA score of 7 or more. We evaluated patient demographics (age, sex, BMI, comorbidity), quality of life (WOMAC score, Oxford Hip Score, SF-12 score), and surgeon- and procedural/implant-specific variables to identify factors associated with postoperative activity score. Minimum followup was 11 months (mean, 12.1 months; range, 11–13 months).
Results
Preoperative UCLA activity score, age, male sex, and BMI predicted high activity scores. The type of operation and implant characteristics did not predict return to high activity sports.
Conclusions
Our data suggest patient-specific factors predict postoperative activity rather than factors specific to type of surgery, implant, or surgeon factors.
Level of Evidence
Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Major joint arthroplasty is undoubtedly one of the surgical success stories of the last 100 years. Incremental improvements in implant design, engineering, and material science continue to promise reduced bearing surface wear, improved implant fixation, and increased component longevity. These improvements have enabled expansion of the indications for joint arthroplasty to include the younger, more active patient. While the primary objectives of joint arthroplasty are to reduce pain and improve patient quality of life and function, younger patients often demand a return to higher function that includes sporting activity. In one recent study, 62% of preoperative sporting participants returned to sporting activity at 1 to 3 years after large joint arthroplasty [45] (Table 1) and several other papers have explored participation in sports after primary THA, hip resurfacing arthroplasty (HRA), TKA, and fixed-bearing unicompartmental knee arthroplasty (UKA) [9, 13, 23, 25, 29, 30, 32]. These reports do not, however, examine the association of implant characteristics on patient activity while controlling for important differences in patient characteristics, preoperative disability and activity, comorbidity, or other important differences.
Table 1.
Comparison of our study and other studies in the literature evaluating sports participation after knee and hip arthroplasty
| Study | Year | Number of patients | Outcome times | UCLA Activity Rating Scale used | Joint and procedure studied | Primary or revision |
|---|---|---|---|---|---|---|
| Amstutz et al. [1] | 2004 | 400 | 3.5 years* | Yes | Hip (HRA) | Primary |
| Bauman et al. [5] | 2007 | 467 | 37–41 months* | Yes | Hip (THA); knee (TKA) | Primary |
| Beaulé et al. [7] | 2004 | 119 | 3 years* | Yes | Hip (HRA) | Primary |
| Bradbury et al. [9] | 1998 | 160 | 5 years* | No | Knee (TKA) | Primary |
| Chatterji et al. [13] | 2004 | 216 | 1–2 years | No | Hip (THA) | Primary |
| Dahm et al. [16] | 2008 | 1630 | 5.7 years* | Yes | Knee (TKA) | Primary |
| Fisher et al. [23] | 2006 | 76 | 18 months* | Yes | Knee (UKA) | Primary |
| Huch et al. [25] | 2005 | 636 | 5 years | No | Hip (THA); knee (TKA) | Primary |
| Mont et al. [29] | 2008 | 33 | 4 years* | No | Knee (TKA) | Primary |
| Naal et al. [30] | 2007 | 83 | 18 months* | No | Knee (UKA) | Primary |
| Naal et al. [32] | 2007 | 112 | 2 years* | No | Hip (HRA) | Primary |
| Sechriest et al. [38] | 2007 | 34 | 6.3 years* | Yes | Hip (THA) | Primary |
| Wylde et al. [45] | 2008 | 2085 | 1–3 years | No | Hip (THA, HRA); knee (TKA, UKA, patellar resurfacing) | Primary |
| Williams et al. | 2012 | 736 | 1 year* | Yes | Hip (THA, HRA); knee (TKA, UKA) | Primary and revision |
* Mean; HRA = hip resurfacing arthroplasty; UKA = unicompartmental knee arthroplasty.
HRA has recently been advocated as a technique to allow young patients to maintain high activity levels that could not be obtained with conventional THA [7, 32]. The metal-on-metal (MOM) cobalt-chromium bearing surface, reintroduced in the early 1990s, has a surface roughness of less than 0.05 μm Ra (roughness average) and a highly conforming polar bearing geometry that maximizes the potential for fluid film lubrication [2, 10, 11, 33, 36, 40]. In vitro wear tests and clinical retrieval studies reveal 10 to 100 times less wear when compared to conventional metal-on-polyethylene (MOP) surfaces [2, 10, 11, 26, 28, 33, 36, 40], tribologic properties that potentially allow a safe return to high-level sports for patients undergoing MOM HRA and THA. Implant survival rates for both MOM HRA [1, 4, 17, 41, 42] and MOM THA [19–22, 24, 26, 27, 39, 43] reportedly range from 94.1% to 99.8% in the medium term. When looking specifically at participation in sports, 110 of 112 HRA patients participated in an average of 4.6 sporting disciplines at a mean of 23.5 months postsurgery, compared with 105 patients performing an average of 4.8 disciplines preoperatively [32]. Similarly, less invasive UKA has seen more than 90% of patients maintaining or improving their ability to participate in sport or recreational activities at a mean of 18 months [23, 30].
Many studies looking at participation in sports have relied on retrospective patient recall after joint arthroplasty and have been unable to utilize a validated activity score [9, 13, 23, 25, 29, 30, 32, 45]. The UCLA Activity Rating Scale provides qualitative assessment of patients’ level of activity after THA [3, 6] and has been validated for routine activity assessment in a clinical setting [46]. While this score does not account for time spent doing an activity, when compared to the Tegner score and the Activity Rating Scale, it shows the best reliability, provides the highest completion rate, and shows no floor effects [31]. A score of 7 or more defines a return to intense activity [7]. A median UCLA score of 6, indicating a moderate activity level, has been reported at 3 years in 467 patients with THA and TKA [5]. The same mean UCLA score of 6 was observed in 41 THAs at 8 years [38]. A mean score of 7.1 was seen at 5.7 years in 1630 TKAs, with patients older than 70 years having lower scores and men achieving higher scores [16]. Fifty-four percent of 400 HRAs scored more than 7 at 3.5 years [1]. These limited reports, however, require confirmation.
We therefore (1) measured the rate of sports participation at 1 year using the UCLA activity score and (2) explored variables, including choice of procedure/prosthesis, that might independently predict a return to a high level of sporting activity.
Patients and Methods
A search of our longitudinal research database identified 1326 patients who had primary MOP THA, MOM THA, HRA, revision THA, primary TKA, UKA, and revision TKA between May 2005 and June 2007 and had a preoperative UCLA score. During this time, a total of 2873 patients had hip or knee arthroplasty: 1916 patients had hip arthroplasty while 957 had knee arthroplasty. Patients were considered eligible if they had any of these procedures and had both a preoperative and 1-year postoperative UCLA score in our longitudinal research database. Of the 2873 patients who were treated during this time, 1326 (46%) patients were seen in the clinic and had a preoperative UCLA score. Of these 1326 patients, 736 (56%) had completed both preoperative and 1-year followup questionnaires, which were retrieved from our longitudinal research database. There were 360 men and 376 women with a mean age of 64.5 years (range, 25–93 years) (Table 2). Patients undergoing multiple joint arthroplasties were included only once and the first joint to be replaced was assessed. If simultaneous arthroplasties were performed, the side included was chosen at random. Minimum followup was 11 months (mean, 12.1 months; range, 11–13 months). The nonresponders were evaluated preoperatively for demographics and quality of life (including UCLA activity level) and postoperatively for type of procedure and articulation (MOP or MOM). Confidence intervals (CI) will be wider as a result of any missing data. Therefore, finding statistical significance in instances with missing data is actually a stronger result. (This assumes data are missing at random and not related to the variables of interest.) No patients were recalled specifically for this study; all data were obtained from medical records and radiographs. All 1326 patients consented to participate in the study. Institutional Review Board approval had been obtained.
Table 2.
Patient characteristics (n = 736)
| Characteristic | Primary (n = 425) | Revision THA | Overall: hip | Primary (n = 211) | Revision TKA | Overall: knee | |||
|---|---|---|---|---|---|---|---|---|---|
| MOP THA | MOM THA | MOM HRA | TKA | UKA | |||||
| Number of patients | 284 | 59 | 82 | 62 | 487 | 194 | 17 | 38 | 249 |
| Age at surgery (years) | |||||||||
| Mean | 65.7 | 58.4 | 54.2 | 67.3 | 63.0 | 67.1 | 63.4 | 71.2 | 67.5 |
| SD | 12.2 | 8.8 | 7.4 | 12.2 | 12.1 | 10.1 | 8.4 | 8.6 | 9.9 |
| Range | 25–92 | 31–76 | 42–74 | 31–89 | 25–92 | 45–93 | 46–75 | 51–86 | 45–93 |
| Male:female (number of patients) | 123:161 | 42:17 | 68:14 | 33:29 | 266:221 | 66:128 | 6:11 | 22:16 | 94:155 |
| BMI (kg/m2) | 27.9 | 27.4 | 27.8 | 28.1 | 27.8 | 31.2 | 29.0 | 32.0 | 31.2 |
| Charnley class (number of patients) | |||||||||
| A | 89 | 27 | 40 | 24 | 180 | 43 | 6 | 14 | 63 |
| B1 | 36 | 11 | 21 | 3 | 71 | 43 | 4 | 1 | 48 |
| B2 | 32 | 1 | 7 | 10 | 50 | 25 | 3 | 4 | 32 |
| C | 127 | 20 | 14 | 25 | 186 | 83 | 4 | 19 | 106 |
MOP = metal-on-polyethylene; MOM = metal-on-metal; HRA = hip resurfacing arthroplasty; UKA = unicompartmental knee arthroplasty.
Procedures were performed by four participating surgeons (BAM, NVG, CPD, DSG) at our institution. Surgical details and comorbidities were recorded prospectively. The Charnley classification [12] was used for the assessment of comorbidity: Class A patients have an ipsilateral joint arthroplasty; Class B1 have an ipsilateral joint arthroplasty with degenerative change in the contralateral hip; Class B2 have both hips replaced; and Class C have multiple-joint disease or other disabilities leading to difficulties in walking (Table 2).
Patients completed a WOMAC [8], an Oxford Hip Score (OHS) [18], an SF-12 [44], and a UCLA activity questionnaire [3, 6] at the time of admission and at 1-year followup. The WOMAC is a self-administered multidimensional index containing five dimensions for pain, two for stiffness, and 17 for function. Each item is represented by a Likert scale between 0 (best health state) and 4 (worst state). Each total raw score was normalized into a 0 to 100 scale, with 0 being the worst quality of life and 100 the best [8]. The OHS is a 12-item patient-based questionnaire developed and validated specifically to assess function and pain after THA [18] and was again normalized to a total best score out of 100. The SF-12 mental component score is a subscale of the SF-36 and is calculated on a 0- to 100-point, worst to best, scale [44]. The UCLA Activity Rating Scale has 10 descriptive activity levels, ranging from wholly inactive and dependent on others (Level 1), to moderate activities such as unlimited housework and shopping (Level 6), to regular participation in cycling (Level 7) and participation in impact sports such as jogging or tennis (Level 10) [3].
An ordinal regression model was used to assess predictors of activity level [37]. The dependent variable was UCLA activity. This model calculated a single odds ratio (OR) and 95% CI for each covariate, independent of the rank of the response category. The assumptions of proportionality across thresholds were tested [14]. Summary proportional ORs and CIs were then calculated for selected independent variables, which included various demographic and surgical parameters. The covariates tested in all analyses included patient characteristics, such as age, sex, BMI, and Charnley [12] comorbidity class (A, B1, B2, C); preoperative quality-of-life scores, such as preoperative WOMAC function score (continuous), WOMAC pain score (continuous), OHS (continuous), and SF-12 mental component score (continuous); the surgeon (one of four participating fellowship-trained surgeons [BAM, NVG, DSG who perform both hip and knee arthroplasty and CPD who performs only hip arthroplasty]); the type of operation (primary MOP THA, MOM THA, HRA, revision THA, primary TKA, UKA, revision TKA); and the bearing surface diameter. We did not include the use of cement (cementless versus cemented implants) as a covariate since previous studies have shown this factor does not affect quality of life [15, 34, 35]. A separate similar analysis was run excluding all knee arthroplasties. The difference between preoperative and followup scores was used to demonstrate improvements in WOMAC function and pain, OHS, and SF-12 mental component scores. This analysis utilized a t-test. In the proportional odds model for each covariate, outputs included an estimate of the regression coefficient, its standard error, Wald chi-square statistic, p value, and the corresponding OR and CI. We performed the statistical analysis using the SAS® Version 9.1 software package (SAS Institute, Inc, Cary, NC, USA).
Results
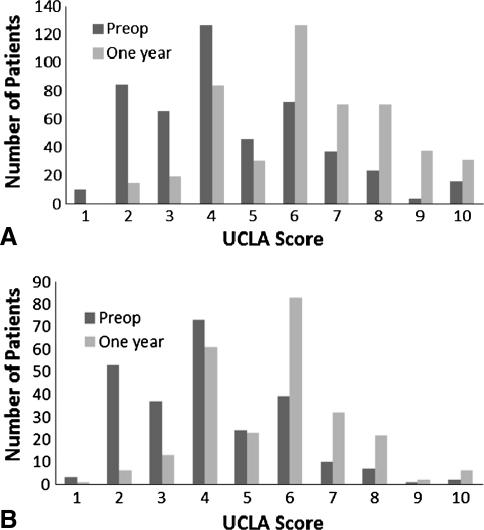
Ninety-one (12.3%) patients achieved a UCLA score of 7 or more at baseline increasing to 274 (37.2%) patients at 1-year followup (Table 3). The distributions of preoperative UCLA activity scores increased for hip and knee arthroplasty at 1 year (Fig. 1). We observed an improvement (p < 0.001) in all patients’ 1-year quality-of-life scores from the preoperative scores, as evidenced by the 95% CIs for these improvements, for all types of hip and knee arthroplasty (Table 4).
Table 3.
Percentage of patients with a UCLA activity score of 7 or more
| Time of assessment | % of patients | |
|---|---|---|
| Overall: hip | Overall: knee | |
| Preoperative | 16.6 | 8.0 |
| Postoperative | 43.3 | 24.9 |
Fig. 1A–B.
Graphs show the preoperative and 1-year UCLA scores for all patients with (A) hip and (B) knee arthroplasties. Preop = preoperative.
Table 4.
Quality-of-life scores preoperatively and at 1-year followup
| Scoring system | Overall: hip | Overall: knee |
|---|---|---|
| WOMAC function score (points) | ||
| Preoperative | 49.2 (20; 0–99) | 50.5 (19; 9–97) |
| One year | 88.0 (14; 5–100) | 81.5 (17; 11.8–100) |
| Difference | 37–41 | 26–32 |
| WOMAC pain score (points) | ||
| Preoperative | 49.7 (19; 0–100) | 47.9 (20; 0–100) |
| One year | 90.0 (15; 0–100) | 83.7 (18; 15–100) |
| Difference | 38–43 | 33–38 |
| Oxford Hip Score (points) | ||
| Preoperative | 45.1 (18; 6–100) | 43.0 (18; 4–98) |
| One year | 86.5 (16; 14–100) | 78.9 (18; 17–100) |
| Difference | 39–44 | 34–39 |
| SF-12 mental component score (points) | ||
| Preoperative | 46.8 (12; 18–69) | 47.2 (12; 21–69) |
| One year | 54.9 (8; 16–68) | 53.1 (10; 17–68) |
| Difference | 7–10 | 4–8 |
| UCLA activity score | ||
| Preoperative | 4.5 (2.1; 1–10) | 4.1 (1.7; 1–10) |
| One year | 6.3 (2.0; 2–10) | 5.6 (1.7; 1–10) |
| Difference | 1.5–2.0 | 1.3–1.7 |
Values are expressed as mean, with SD and range in parentheses; differences between preoperative and 1-year scores are expressed as 95% CIs.
The preoperative UCLA activity score, younger patient age, male sex, and BMI independently predicted a postoperative UCLA activity score of 7 or more for all operation types (Table 5). Additionally, a better preoperative WOMAC pain score was also a factor for predicting a UCLA score of 7 or more when considering hip arthroplasty alone (Table 6). Thus, with each unit increase in preoperative UCLA score, the OR for achieving a 1-year UCLA score of 7 or more was 1.64 (95% CI, 1.47–1.83). The other covariates, mainly Charnley class, preoperative WOMAC function score, OHS, SF-12 mental component score, the operating surgeon, and interestingly the type of operation and the bearing surface diameter, did not predict a 1-year UCLA score of 7 or more.
Table 5.
Overall predictors of UCLA activity score of 7 or more
| Predictor | Odds ratio | 95% CI | p value (chi-square test) |
|---|---|---|---|
| Preoperative UCLA score | 1.64 | 1.47–1.83 | < 0.001 |
| Age | 0.95 | 0.93–0.97 | < 0.001 |
| Sex | 4.25 | 2.86–6.31 | < 0.001 |
| BMI | 0.91 | 0.87–0.95 | < 0.001 |
Table 6.
Hip arthroplasty predictors of UCLA activity score of 7 or more
| Predictor | Odds ratio | 95% CI | p value (chi-square test) |
|---|---|---|---|
| Preoperative UCLA score | 1.61 | 1.40–1.86 | < 0.001 |
| Age | 0.96 | 0.94–0.98 | < 0.001 |
| Sex | 4.84 | 2.93–7.99 | < 0.001 |
| BMI | 0.93 | 0.88–0.97 | < 0.001 |
| Preoperative WOMAC pain score | 1.02 | 1.001–1.029 | 0.029 |
When assessing for possible selection bias, we noted responders had higher (better) health-related quality-of-life scores (including UCLA activity level) preoperatively than nonresponders. Type of surgical procedure did not differ between patients who were followed versus those who were not followed. In hips only, revisions, women, and those with MOP articulations (compared to MOM) were less likely to be followed. However, since surgical procedure itself did not differ between those followed or not followed, the effects of loss to followup on comparisons between procedures would at least be partly mitigated.
Discussion
While the primary objective of joint arthroplasty is to improve patient quality of life, pain, and function, younger active patients often demand a return to higher function that includes sporting activity. This study (1) measured the rate of sports participation at 1 year and (2) explored 11 variables that might predict a return to a high level of sporting activity, including whether procedure/prosthesis is an independent predictor.
We acknowledge limitations to our study. First, only 46% of patients undergoing lower limb arthroplasty during the study period had a preoperative score and only 56% of these patients returned a 1-year score. It is, therefore, possible that patients who returned the 1-year questionnaire could be more active and/or motivated than the nonresponders. The study does however measure UCLA activity, a score that is validated for use in a clinical setting [46], with 7 or more defining a return to intense activity [7], in a large cohort of patients undergoing primary MOP THA, MOM THA, HRA, revision THA, primary TKA, UKA, and revision TKA. We therefore believe our conclusions can be used to confirm or refute the findings of previous studies.
In this study, 91 (12.3%) patients achieved a UCLA score of 7 or more at preoperative baseline increasing to 274 (37.2%) patients at 1-year followup. Wylde et al. [45] analyzed the responses of a cross-sectional postal survey to describe the effect of a range of hip and knee arthroplasty procedures on sports participation. While type of sport was recorded in Wylde et al. [45], a validated activity score was not used to grade participation and therefore comparison with our study must be interpreted carefully. In the 3 years before THA, HRA, TKA, UKA, or patellar resurfacing, 726 of 2085 (35%) patients were participating in sports [45]. A total of 446 (21% of the total group and 61% of preoperative participants) returned to their sporting activities by 1 to 3 years postoperatively; 192 participants (26%) were unable to do so after lower limb arthroplasty [45]. The largest declines in participation were seen in high-impact sports, including badminton, tennis, and dancing [45]. Patient participation in sports after primary THA [13, 25], HRA [32], TKA [9, 25, 29], and UKA [23, 30] has been described (Table 1). The proportion of 636 patients performing sporting activities increased from 36% preoperatively to 52% at 5 years after THA, but participation declined from 42% to 34% at 5 years after TKA [25]. In a study of 235 THAs in 216 patients, the total number of patients performing a sport also increased at 1 to 2 years postoperatively, but the total amount of sports played decreased [13]. One hundred ten of 112 patients with HRA participated in an average of 4.6 sporting disciplines at a mean of 23.5 months after surgery, compared with 105 patients preoperatively performing an average of 4.8 disciplines [32]. Thirty-two of 33 patients with TKA partaking in high-impact sports enjoyed an excellent activity level at a minimum of 4 years [29]. Forty-three of 56 (77%) patients with TKA who had participated in regular exercise in the year before surgery had returned to sports at a mean of 5 years [9]. UKA has seen more than 90% of patients maintaining or improving their ability to participate in sports or recreational activities at a mean of 18 months [23, 30]. Comparison of our study with these papers must be interpreted carefully, since most did not use the validated UCLA activity score to grade participation (Table 1). In studies that do utilize the validated UCLA activity score, a median UCLA score of 6 was reported at 3 years in 467 patients with 47% of patients with THA and 53% of patients with TKA achieving a score of 7 or more [5]. The same mean UCLA score of 6 was observed in 41 THAs at 8 years [38]. A mean score of 7.1 was seen at 5.7 years in 1630 TKAs [16], and 54% of 400 HRAs scored more than 7 at 3.5 years [1]. These papers [1, 16, 38] do not however report the distribution of UCLA scores of 7 or more that defines a return to intense activity [7].
We found age, male sex, BMI, and the preoperative UCLA activity level independently predicted a 1-year postoperative UCLA score of 7 or more. In addition, a better preoperative WOMAC pain score predicted a UCLA score in the 7 to 10 range when considering hip arthroplasty alone. Others have found higher scores at followup in young male patients [16]. Wylde et al. [45] also found men were 1.8 times more likely than women to return to sports but did not find age predicted return. Charnley class, preoperative WOMAC function and pain score, preoperative OHS, preoperative SF-12 mental component score, operating surgeon, and bearing surface diameter did not predict a 1-year UCLA score of 7 or more. Type of operation also did not predict a 1-year UCLA score of 7 or more; primary hip arthroplasty (all categories) showed no advantage over revision THA, and the large MOM bearing surface, whether HRA or THA, showed no advantage over MOP. The same was true when comparing primary with revision TKA and UKA with TKA, although numbers in the UKA group were small. Our findings therefore support those reported by Wylde et al. [45], who found no difference in return to sports according to type of operation undertaken.
Of 11 preoperative variables, we found four (age, male sex, BMI, and preoperative activity level) predicted a 1-year UCLA activity score of 7 or more, equivalent to a return to cycling. Our observations suggest patient-specific factors predict postoperative activity rather than factors specific to type of surgery, implant, or surgeon. Expectations regarding the ability of new bearing surface technologies to enable a return to sports should be tempered. The ability of different implants to maintain activity level beyond 1 year into the medium and long term however requires further study. These data may be useful in further informing the surgeon-patient discussion as to expectations regarding return to sporting activities after hip and knee arthroplasty.
Acknowledgments
The authors thank Daphné Savoy for her assistance in the preparation of this manuscript and Eric Sayre, PhD, for his assistance with the statistical analysis.
Footnotes
The institution of one or more of the authors (DSG, NVG, BAM) has received, in any 1 year, funding from Zimmer, Inc (Warsaw, IN, USA), DePuy Orthopaedics Inc (Warsaw, IN, USA), and Stryker Canada (Hamilton Ontario, Canada). One or more of the authors (DSG, BAM, CPD) certify that he or she, or a member of his or her immediate family, has consultancies at Zimmer, Inc. One or more of the authors (CPD) certify that he or she, or a member of his or her immediate family, has a consultancy at Smith & Nephew, Inc (Memphis, TN, USA).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amstutz HC, Beaulé PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39. [PubMed] [Google Scholar]
- 2.Amstutz HC, Campbell P, McKellop H, Schmalzreid TP, Gillespie WJ, Howie D, Jacobs J, Medley J, Merritt K. Metal on metal total hip replacement workshop consensus document. Clin Orthop Relat Res. 1996;329(suppl):S297–S303. doi: 10.1097/00003086-199608001-00027. [DOI] [PubMed] [Google Scholar]
- 3.Amstutz HC, Thomas BJ, Jinnah RF, Kim WF, Grogan TF, Yale C. Treatment of primary osteoarthritis of the hip: a comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed] [Google Scholar]
- 4.Back DL, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings: an independent prospective study of the first 230 hips. J Bone Joint Surg Br. 2005;87:324–329. doi: 10.1302/0301-620X.87B3.15556. [DOI] [PubMed] [Google Scholar]
- 5.Bauman S, Williams DF, Petruccelli DF, Elliott WF, Beer J. Physical activity after total joint replacement: a cross-sectional survey. Clin J Sport Med. 2007;17:104–108. doi: 10.1097/JSM.0b013e3180379b6a. [DOI] [PubMed] [Google Scholar]
- 6.Beaulé PE, Dorey FJ, Hoke RF, Leduff MF, Amstutz HC. The value of patient activity level in the outcome of total hip arthroplasty. J Arthroplasty. 2006;21:547–552. doi: 10.1016/j.arth.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Beaulé PE, Dorey FJ, LeDuff M, Gruen T, Amstutz HC. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93. doi: 10.1097/00003086-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Bellamy NF, Buchanan WW, Goldsmith CH, Campbell JF, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 9.Bradbury NF, Borton DF, Spoo GF, Cross MJ. Participation in sports after total knee replacement. Am J Sports Med. 1998;26:530–535. doi: 10.1177/03635465980260041001. [DOI] [PubMed] [Google Scholar]
- 10.Chan FW, Bobyn JD, Medley JB, Krygier JJ, Tanzer M. The Otto Aufranc Award. Wear and lubrication of metal-on-metal hip implants. Clin Orthop Relat Res. 1999;369:10–24. doi: 10.1097/00003086-199912000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Chan FW, Bobyn JD, Medley JB, Krygier JJ, Yue S, Tanzer M. Engineering issues and wear performance of metal on metal hip implants. Clin Orthop Relat Res. 1996;333:96–107. doi: 10.1097/00003086-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br. 1972;54:61–76. [PubMed] [Google Scholar]
- 13.Chatterji U, Ashworth MJ, Lewis PL, Dobson PJ. Effect of total hip arthroplasty on recreational and sporting activity. ANZ J Surg. 2004;74:446–449. doi: 10.1111/j.1445-1433.2004.03028.x. [DOI] [PubMed] [Google Scholar]
- 14.Cleveland WS, Devlin SJ, Grosse E. Regression by local fitting. J Econometrics. 1988;37:87–114. doi: 10.1016/0304-4076(88)90077-2. [DOI] [Google Scholar]
- 15.Corten K, Bourne RB, Charron KD, Au K, Rorabeck CH. What works best, a cemented or cementless primary total hip arthroplasty? Minimum 17-year followup of a randomized controlled trial. Clin Orthop Relat Res. 2011;469:209–217. doi: 10.1007/s11999-010-1459-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dahm DL, Barnes SA, Harrington JR, Sayeed SA, Berry DJ. Patient-reported activity level after total knee arthroplasty. J Arthroplasty. 2008;23:401–407. doi: 10.1016/j.arth.2007.05.051. [DOI] [PubMed] [Google Scholar]
- 17.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 18.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190. [PubMed] [Google Scholar]
- 19.Delaunay CP. Metal-on-metal bearings in cementless primary total hip arthroplasty. J Arthroplasty. 2004;19:35–40. doi: 10.1016/j.arth.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Dorr LD, Wan Z, Longjohn DB, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation: four to seven-year results. J Bone Joint Surg Am. 2000;82:789–798. doi: 10.2106/00004623-200006000-00005. [DOI] [PubMed] [Google Scholar]
- 21.Dumbleton JH, Manley MT. Metal-on-metal total hip replacement: what does the literature say? J Arthroplasty. 2005;20:174–188. doi: 10.1016/j.arth.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 22.Eswaramoorthy V, Moonot P, Kalairajah Y, Biant LC, Field RE. The Metasul metal-on-metal articulation in primary total hip replacement: clinical and radiological results at ten years. J Bone Joint Surg Br. 2008;90:1278–1283. doi: 10.1302/0301-620X.90B10.20378. [DOI] [PubMed] [Google Scholar]
- 23.Fisher N, Agarwal M, Reuben SF, Johnson DS, Turner PG. Sporting and physical activity following Oxford medial unicompartmental knee arthroplasty. Knee. 2006;13:296–300. doi: 10.1016/j.knee.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 24.Grubl A, Marker M, Brodner W, Giurea A, Heinze G, Meisinger V, Zehetgruber H, Kotz R. Long-term follow-up of metal-on-metal total hip replacement. J Orthop Res. 2007;25:841–848. doi: 10.1002/jor.20381. [DOI] [PubMed] [Google Scholar]
- 25.Huch KF, Muller KA, Sturmer TF, Brenner HF, Puhl WF, Gunther KP. Sports activities 5 years after total knee or hip arthroplasty: the Ulm Osteoarthritis Study. Ann Rheum Dis. 2005;64:1715–1720. doi: 10.1136/ard.2004.033266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jacobsson SA, Djerf K, Wahlstrom O. Twenty-year results of McKee-Farrar versus Charnley prosthesis. Clin Orthop Relat Res. 1996;329(suppl):S60–S68. doi: 10.1097/00003086-199608001-00006. [DOI] [PubMed] [Google Scholar]
- 27.Long WT, Dorr LD, Gendelman V. An American experience with metal-on-metal total hip arthroplasties: a 7-year follow-up study. J Arthroplasty. 2004;19:29–34. doi: 10.1016/j.arth.2004.09.018. [DOI] [PubMed] [Google Scholar]
- 28.McKellop H, Park SH, Chiesa RF, Doorn PF, Lu BF, Normand PF, Grigoris P, Amstutz H. In vivo wear of three types of metal on metal hip prostheses during two decades of use. Clin Orthop Relat Res. 1996;329(suppl):S128–S140. doi: 10.1097/00003086-199608001-00013. [DOI] [PubMed] [Google Scholar]
- 29.Mont MA, Marker DR, Seyler TM, Jones LC, Kolisek FR, Hungerford DS. High-impact sports after total knee arthroplasty. J Arthroplasty. 2008;23:80–84. doi: 10.1016/j.arth.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 30.Naal FD, Fischer MF, Preuss AF, Goldhahn JF, Knoch FF, Preiss S, Munzinger U, Drobny T. Return to sports and recreational activity after unicompartmental knee arthroplasty. Am J Sports Med. 2007;35:1688–1695. doi: 10.1177/0363546507303562. [DOI] [PubMed] [Google Scholar]
- 31.Naal FD, Impellizzeri FM, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res. 2009;467:958–965. doi: 10.1007/s11999-008-0358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Naal FD, Maffiuletti NA, Munzinger UF, Hersche O. Sports after hip resurfacing arthroplasty. Am J Sports Med. 2007;35:705–711. doi: 10.1177/0363546506296606. [DOI] [PubMed] [Google Scholar]
- 33.Rieker CB, Schon RF, Kottig P. Development and validation of a second-generation metal-on-metal bearing: laboratory studies and analysis of retrievals. J Arthroplasty. 2004;19:5–11. doi: 10.1016/j.arth.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 34.Rorabeck CH, Bourne RB, Lewis PL, Nott L. The Miller-Galante knee prosthesis for the treatment of osteoarthrosis: a comparison of the results of partial fixation with cement and fixation without any cement. J Bone Joint Surg Am. 1993;75:402–408. doi: 10.2106/00004623-199303000-00012. [DOI] [PubMed] [Google Scholar]
- 35.Rorabeck CH, Bourne RB, Mulliken BD, Nayak N, Laupacis A, Tugwell P, Feeney D. The Nicolas Andry Award. Comparative results of cemented and cementless total hip arthroplasty. Clin Orthop Relat Res. 1996;325:330–344. doi: 10.1097/00003086-199604000-00044. [DOI] [PubMed] [Google Scholar]
- 36.Schmidt M, Weber H, Schon R. Cobalt chromium molybdenum metal combination for modular hip prostheses. Clin Orthop Relat Res. 1996;329(suppl):S35–S47. doi: 10.1097/00003086-199608001-00004. [DOI] [PubMed] [Google Scholar]
- 37.Scott SC, Goldberg MS, Mayo NE. Statistical assessment of ordinal outcomes in comparative studies. J Clin Epidemiol. 1997;50:45–55. doi: 10.1016/S0895-4356(96)00312-5. [DOI] [PubMed] [Google Scholar]
- 38.Sechriest VF, Kyle RF, Marek DJ, Spates JD, Saleh KJ, Kuskowski M. Activity level in young patients with primary total hip arthroplasty: a 5-year minimum follow-up. J Arthroplasty. 2007;22:39–47. doi: 10.1016/j.arth.2006.02.083. [DOI] [PubMed] [Google Scholar]
- 39.Sharma S, Vassan U, Bhamra MS. Metal-on-metal total hip joint replacement: a minimum follow-up of five years. Hip Int. 2007;17:70–77. doi: 10.1177/112070000701700203. [DOI] [PubMed] [Google Scholar]
- 40.Sieber HP, Rieker CB, Kottig P. Analysis of 118 second-generation metal-on-metal retrieved hip implants. J Bone Joint Surg Br. 1999;81:46–50. doi: 10.1302/0301-620X.81B1.9047. [DOI] [PubMed] [Google Scholar]
- 41.Steffen RT, Pandit HP, Palan J, Beard DJ, Gundle R, McLardy-Smith P, Murray DW, Gill HS. The five-year results of the Birmingham Hip Resurfacing arthroplasty: an independent series. J Bone Joint Surg Br. 2008;90:436–441. doi: 10.1302/0301-620X.90B4.19648. [DOI] [PubMed] [Google Scholar]
- 42.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty: a minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]
- 43.Wagner M, Wagner H. Medium-term results of a modern metal-on-metal system in total hip replacement. Clin Orthop Relat Res. 2000;379:123–133. doi: 10.1097/00003086-200010000-00015. [DOI] [PubMed] [Google Scholar]
- 44.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. doi: 10.1097/00005650-199206000-00002. [DOI] [PubMed] [Google Scholar]
- 45.Wylde VF, Blom AF, Dieppe PF, Hewlett S, Learmonth I. Return to sport after joint replacement. J Bone Joint Surg Br. 2008;90:920–923. doi: 10.1302/0301-620X.90B7.20614. [DOI] [PubMed] [Google Scholar]
- 46.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. doi: 10.1016/S0883-5403(98)90195-4. [DOI] [PubMed] [Google Scholar]