Abstract
Objective
This study sought to examine the age-dependent persistence of attention-deficit/hyperactivity disorder (ADHD) and its predictors in a large sample of girls with and without ADHD followed prospectively for 11 years into young adulthood.
Method
Participants were girls with (N=96) and without (N=91) ADHD 6 –17 years old at the baseline assessment (mean age 11 years) and 15–30 years old at the follow-up assessment (mean: 22 years). Participants were comprehensively and blindly assessed with structured diagnostic interviews and assessments of cognitive, social, school, and family functioning.
Results
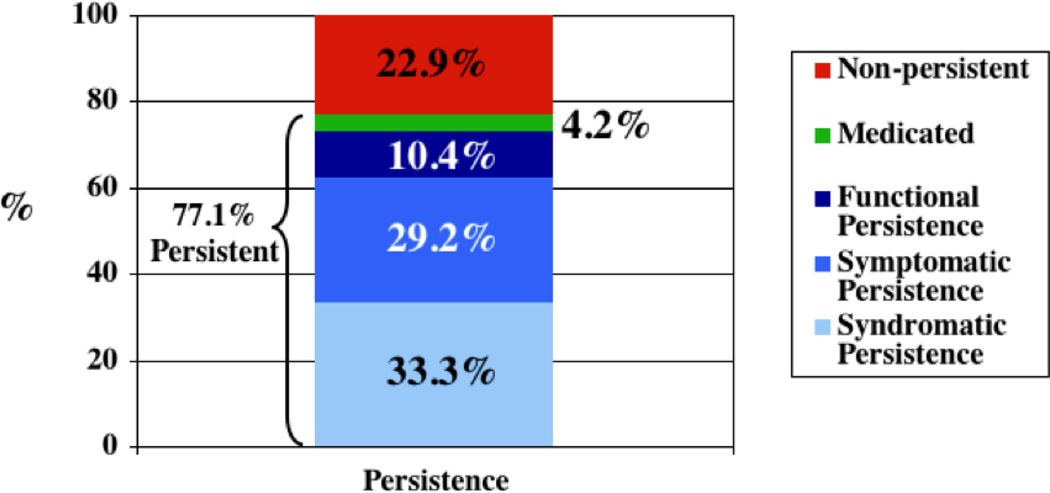
At the 11-year follow-up, 33.3% met full criteria for ADHD, 29.2% showed partial persistence of the disorder, 10.4% had impaired functioning and 4.2% were remitted but treated (77.1% of the sample). Predictors of persistence were psychiatric comorbidity, family history of psychopathology, and family and school functioning at baseline.
Conclusion
These long-term, prospective, follow-up findings extend to girls findings that ADHD is persistent over the long term and can be predicted from psychosocial adversity and psychiatric comorbidity ascertained 11 years earlier.
Keywords: Attention-deficit/hyperactivity disorder, persistence, predictors, longitudinal, young adult
Introduction
While follow-up studies of attention-deficit/hyperactivity disorder (ADHD) have been conducted (1–11), very few have followed girls with ADHD. The first follow-up study of girls reported on the outcome of only 12 DSM-II hyperactive girls compared with 24 hyperactive boys and 24 male controls (12). In a longitudinal community survey, girls identified as hyperactive at baseline were more likely to report academic and interpersonal relationship problems at the adolescent follow-up (13), as well as report using a wide variety of ineffective coping strategies (14).
Hinshaw (15) and Owens (16) reported findings from a prospective sample of girls followed into adolescence, showing that the majority of girls with ADHD continued to struggle with functional impairments across multiple domains. Our group reported similar results from a 5-year prospective follow-up study into mid-adolescent years from a large sample of DSM-III-R defined ADHD girls and controls (17). We found that girls with ADHD were at significantly higher risk than controls for disruptive behavior, mood, anxiety, and addictive disorders in adolescence.
We recently reported results from the 11-year follow-up of the above sample of girls with and without ADHD followed up into young adulthood (mean age 22 years). By young adult years, ADHD girls were at high risk for a wide range of adverse psychiatric outcomes including elevated risks for antisocial, addictive, mood, anxiety, and eating disorders. In another longitudinal report of young adult outcomes of girls with ADHD, Babinski et al. (18) found at the 8-year follow-up that girls with ADHD had more internalizing and externalizing problems, more family conflict, fewer romantic relationships, and poorer academic performance than comparison women. In a longitudinal study of children with ADHD, Dalsgaard et al. (19) found that girls with ADHD had a higher risk of psychiatric admission in adulthood compared to boys with ADHD. Although these reports clearly documented that ADHD in girls is associated with high levels of morbidity and disability into young adult years, they did not detail patterns of persistence and remission, and provided little information regarding predictors of persistence.
There has been a paucity of research about predictors of remission and persistence in girls with ADHD. A few studies of boys with ADHD found that aggression or conduct problems in childhood (20–22) predicted persistence of ADHD into adolescence and young adulthood in boys. Hart et al. (23) reported that the persistence of ADHD in boys at a 4-year follow-up was predicted by hyperactive/impulsive symptoms and by comorbid conduct disorder. Our group identified patterns of psychiatric comorbidity (24) as important risk factors for persistence of ADHD into adolescence in boys. However, whether these risks factors predict outcomes in girls with ADHD remains unknown.
A better understanding of patterns of persistence and remission as well as its predictors of outcome in girls with ADHD over the long term has major clinical, scientific, and public health relevance. Clinically, it may help design appropriate treatment strategies to hasten remission; scientifically, it can help identify more homogeneous subgroups with a higher likelihood of persistent course. From the public health perspective, this knowledge can help focus scarce societal resources on those ADHD children at highest risk for persistent illness.
Aims of the Study
The main aim of this study was to comprehensively evaluate patterns of persistence and remission in girls with attention-deficit/hyperactivity disorder attending to different definitions of persistence and to evaluate predictors of persistence over the long term attending to issues of adversity, familiality, and psychiatric comorbidity. To this end, we used data from an 11-year longitudinal follow-up family study of a large sample of comprehensively assessed referred girls with and without attention-deficit/hyperactivity disorder ascertained from pediatric and psychiatric sources. Based on the literature, we hypothesized that the persistence of attention-deficit/hyperactivity disorder in girls would depend on the definition used and would be predicted by psychiatric comorbidity, familiality and psychosocial adversity.
Material and methods
Participants
Detailed study methodology was previously reported (17, 25). Briefly, participants were derived from a longitudinal case-control family study of girls with and without ADHD ascertained from pediatric and psychiatric sources. At baseline, we ascertained girls aged 6–17 years with (ADHD, N=140) and without (Controls, N=122) DSM-III-R ADHD. We excluded girls who had been adopted, if their nuclear family was not available for study, or if they had major sensorimotor handicaps (paralysis, deafness, blindness), psychosis, autism, inadequate command of the English language, or a Full Scale IQ less than 80. All of the ADHD girls met DSM-III-R diagnostic criteria for ADHD at the time of the clinical referral; at the time of recruitment they all had active symptoms of the disorder.
The present study reports on a mean follow-up of 11 years (range: 8 to 14 years), where 96 ADHD and 91 control girls from the original sample completed a full follow-up assessment. Participants provided written informed consent, and parents also provided consent for offspring under the age of 18 and for their report on their offspring. Adolescents provided written assent to participate. The human research committee at Massachusetts General Hospital approved this study.
Follow-up assessment procedures
We used the Structured Clinical Interview for DSM-IV (SCID) (26) supplemented with modules from the DSM-IV modified Kiddie Schedule for Affective Disorders and Schizophrenia- Epidemiological Version (K-SADS-E) (27) to assess childhood diagnoses. The DSM-IV K-SADS-E was used for participants younger than 18 years of age. We interviewed all participants (direct) and interviewed their mothers about their offspring (indirect). Of the 187 participants with a full diagnostic interview, the proportion that provided direct only, mother only and both types of reports were 89%, 3%, and 8%, respectively (47%, 3%, and 50%, respectively, for the ADHD module). We combined data from direct and indirect interviews by considering a diagnostic criterion positive if it was endorsed in either interview.
In order to assess family history of psychiatric disorders, first-degree relatives of probands were also assessed. This sample comprised mothers (N=187, N=96 ADHD, N=91 controls), fathers (N=180, N=93 ADHD, N=87 controls), and siblings (N=254, N=139 ADHD, N=115 controls). The number of family members did not differ between ADHD and control probands (χ2(1)=0.73, p=0.39). Parents were assessed at baseline only (as they had passed the age of risk for most psychopathology), while the siblings were assessed at baseline (N=206), 5-year follow-up (N=244), and 11-year follow-up (N=252). Parents received direct interviews and siblings received an indirect interview if they were younger than 12 years of age, and both an indirect and a direct interviews if between 12 and 17 years of age, and a direct interview if 18 years of age and older.
Interviewers were blind to baseline ascertainment group, ascertainment site and prior assessments. They had undergraduate degrees in psychology and were extensively trained. Kappa coefficients between interviewers and board certified child and adult psychiatrists and licensed clinical psychologists were previously reported (17) (median kappa for individual disorders=0.98).
We considered a disorder positive if DSM-IV diagnostic criteria were unequivocally met. A committee of board-certified child and adult psychiatrists and child psychologists, blinded to the participant's ADHD status, referral source and all other data, resolved diagnostic uncertainties. Diagnoses presented for review were considered positive only if diagnostic criteria were met to a clinically meaningful degree. We estimated the reliability of the diagnostic review process by computing kappa coefficients of agreement for clinician reviewers. Kappa coefficients between individual clinicians and the review committee were previously reported (17) (median kappa of individual disorders=0.87). To avoid false-positive diagnoses, we diagnosed major depression only if it was associated with severe impairment (28).
Persistent ADHD was defined as meeting full or subthreshold criteria for DSM-IV ADHD in the month prior to the 11-year assessment. A subthreshold ADHD case was defined by more than half but less than full diagnostic criteria (i.e., four or five ADHD symptoms), but meeting all other diagnostic requirements (e.g., age of onset). Socioeconomic status (SES) was measured using the 5-point Hollingshead scale (29). We used the DSM-IV Global Assessment of Functioning (GAF) (27) to assess overall functioning.
Statistical analysis
As proposed by Keck et al. (30), the distinction between different types of remission may clarify components of complex recovery processes. Syndromatic remission refers to the loss of full diagnostic status, symptomatic remission refers to the loss of partial diagnostic status, and functional remission refers to the loss of partial diagnostic status plus functional recovery (full recovery). Consistent with our previous work (31), we defined the following mutually exclusive categories of persistence for the 96 ADHD participants returning at the 11-year follow-up: a) participants meeting full DSM-IV criteria for ADHD (“Syndromatic Persistence”), b) participants meeting subthreshold DSM-IV criteria (more than half of the symptoms required for a full diagnosis, “Symptomatic Persistence”), c) participants not meeting criteria (a) or (b) but who were functionally impaired with a GAF score ≤60 (“Functional Persistence”), and d) participants not meeting criteria (a), (b), or (c) but who were receiving pharmacotherapy for ADHD (“Medicated”) in the month prior to the participant’s 11-year follow-up assessment.
To assess age-specific prevalences of syndromatic, symptomatic, and functional persistence, we graphed the different definitions of persistence as a function of age based on symptoms reported currently (last month) at the 11-year follow-up. Specifically, rates of persistence at follow-up were plotted for different developmental groups in order to easily display observed rates: 15–18 years (high school), 19–21 years (early college), 22–24 years (early young adulthood), and 25–30 years (later young adulthood). Definitions of persistence were modeled as a function of age (continuous) using logistic regression.
Sociodemographic characteristics (age, SES, etc.) among persistent ADHD, remittent ADHD, and controls were compared using linear, logistic, or ordinal logistic regression depending on the distributions of the variable. To assess the functional correlates (e.g., academic functioning) of persistent ADHD, comparisons were made between participants with persistent ADHD, remittent ADHD, and controls using logistic regression. Differences in psychopathology were tested using linear regression for CBCL scores and logistic regression for psychiatric disorders, controlling for any demographic confounders. Positive family history of a disorder was defined as having at least one first-degree relative with a given disorder. All tests were two-tailed with alpha set at 0.05.
Results
Of the 140 ADHD and 122 control girls recruited at baseline, 96 (69%) and 91 (75%), respectively, were re-assessed at the 11-year follow-up. The average follow-up time was 10.6±1.3 years; ages at follow-up ranged from 15–30 years (mean=22.1±3.3, 93% were ≥18 years). The rate of follow-up did not differ between the groups (χ2(1)=1.16, p=0.28). There were no significant differences between girls successfully followed up and those lost to follow-up on SES, age, race, GAF score, familial intactness (i.e., mother and father married and living together), ascertainment source, or psychiatric outcomes (32).
Age-specific prevalence of different definitions of persistence
Of the 96 ADHD participants at the 11-year follow-up, 32 (33.3%) had syndromatic persistence, 28 (29.2%) had symptomatic persistence, 10 (10.4%) had functional persistence, 4 (4.2%) were not symptomatic, syndromatic, or functionally impaired but were medicated for ADHD, and 22 (22.9%) were fully remitted (77.1% (74/96) of ADHD girls). Using only ADHD participants who had reached adulthood (at least 18 years of age), 75% (62/83) met one of our definitions of persistence.
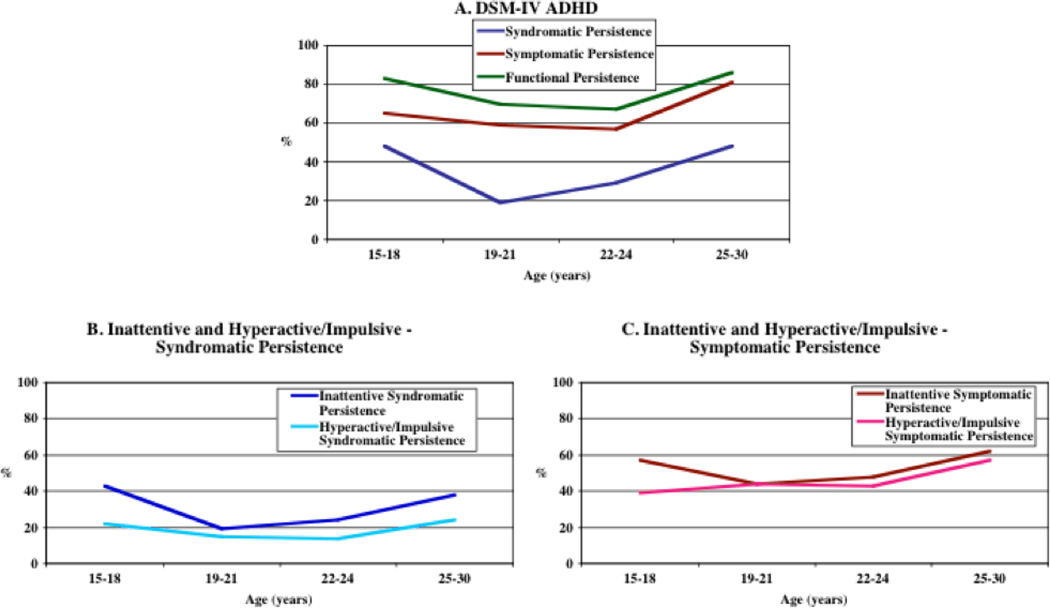
The prevalence estimate of persistence varied considerably depending on the definition used for individual symptomatic clusters. Inattention was slightly more persistent than hyperactivity/impulsivity for both syndromatic (Figure 2B) and symptomatic (Figure 2C) persistence. Increasing age (continuous) was not significantly associated with any definition of persistence (all p>0.20). However, there was a significant curvilinear effect for syndromatic persistence (p=0.03). Figure 2 shows a large drop in syndromatic persistence from ages 15–18 to 19–21 years, but then an increase in persistence in the ages 22–30 years. There were no significant curvilinear effects for any other definition of persistence (all p>0.05).
Fig. 2.
Age-specific prevalence of persistence of ADHD at the 11-year follow-up by definition of persistence and symptom type (N=92). The prevalence of persistence varied considerably depending on the definition used. Age was not significantly associated with any definition of persistence (all p>0.20).
Comparisons between ADHD participants with any form of persistent ADHD (syndromatic, symptomatic, functional persistence and medicated for ADHD [persistent ADHD, N=74] vs. remitted ADHD [Remittent ADHD, N=22], and controls [N=91]) showed that the groups did not differ in age (baseline or follow-up), ascertainment source, or baseline family SES (Table 1). Because the rate of intactness of the family at baseline was significantly lower in the persistent ADHD group (Table 1), all subsequent analyses adjusted for intactness of the family.
Table 1.
Sociodemographic characteristics
| Persistent ADHD(N=74) |
Remittent ADHD(N=22) |
Controls(N=9 1) |
Test statistic |
p-value | |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | |||
| Age at baseline (years) | 11.0 ± 3.2 | 11.1 ± 3.3 | 12.0 ± 2.8 | F(2,184)=2.34 | 0.10 |
| Age at follow-up (years) | 21.7 ± 3.8 | 21.5 ± 3.2 | 22.7 ± 2.9 | F(2,184)=2.30 | 0.10 |
| Socioeconomic status | 1.9 ± 1.0 | 1.9 ± 0.8 | 1.7 ± 0.8 | χ2(2)=3.34 | 0.07 |
| N (%) | N (%) | N (%) | |||
| Intact family | 50 (68) | 20 (91)* | 77 (85)* | χ2(2)=9.30 | 0.01 |
| Ascertainment status (psychiatric) | 40 (44) | 7 (32) | 37 (50) | χ2(2)=2.33 | 0.31 |
p<0.05 versus Persistent ADHD
The two ADHD groups had similar rates of direct and indirect interviews (persistent ADHD: direct=44%, indirect=3%, both=53%; remittent ADHD: direct=68%, indirect=5%, both=27%; χ2(2)=4.41, p=0.11). The persistent ADHD group was significantly more likely to have received pharmacotherapy for ADHD at some point in their lifetime compared to the remittent ADHD group (96% versus 77%, z=2.51, p=0.01). Only 39% (27/70) of the persistent ADHD group was currently (last month) receiving pharmacotherapy for ADHD (excluding n=4 participants classified as persistent ADHD by virtue of being on medication).
Predictors of persistence
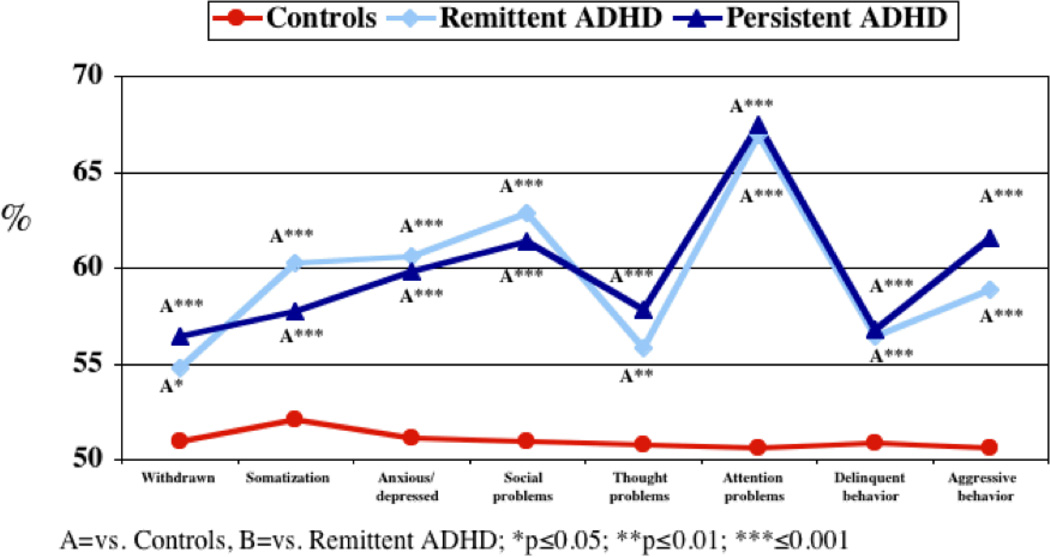
No baseline characteristics of ADHD (age of onset, number of symptoms, impairment, treatment history) were significantly associated with persistence (all p>0.05). Both ADHD groups had significantly higher rates of ODD, major depressive disorder, and multiple (≥2) anxiety disorders at baseline compared to controls (Table 2). However, only the persistent ADHD group had significantly higher rates of conduct and bipolar disorder vs. controls. Both ADHD groups had significantly higher T-scores at baseline for all Child Behavior Checklist (CBCL) subscales vs. controls (Figure 3) but did not differ from each other.
Table 2.
Psychiatric disorders and functional variables at baseline and 11-year follow-up
| Persistent ADHD (N=74) |
Remittent ADHD (N=22) |
Controls (N=91) |
Test statistic |
p- value |
|
|---|---|---|---|---|---|
| Lifetime Psychiatric Disorders at Baseline | |||||
| N (%) | N (%) | N (%) | |||
| Oppositional defiant disorder | 27 (36) a*** | 9 (41) a*** | 4 (4) | χ2(2)=22.34 | <0.001 |
| Conduct disorder | 8 (11) a** | 1 (5) | 0 (0) | Exact | 0.002 |
| Major depressive disorder | 15 (20) a** | 3 (14) a* | 1 (1) | χ2(2)=8.12 | 0.02 |
| Bipolar disorder | 9 (12) a** | 1 (5) | 0 (0) | Exact | 0.002 |
| Multiple (≥2) anxiety disorders | 27 (36) a*** | 7 (32) a*** | 5 (5) | χ2(2)=19.99 | <0.001 |
| School Functioning | |||||
| Repeated grade | 16 (22) a*** | 1 (5) | 2 (2) | χ2(2)=11.88 | 0.003 |
| Special class | 13 (18) a** | 2 (9) | 2 (2) | χ2(2)=17.50 | <0.001 |
| Tutoring | 53 (72) a*** | 13 (59) a*** | 14 (15) | χ2(2)=7.78 | 0.02 |
| Family Environment Scale at Baseline | |||||
| Mean ± SD | Mean ± SD | Mean ± SD | |||
| Cohesion | 39.2 ± 19.9 a*** | 48.3 ± 15.9 | 52.1 ± 16.9 | F(2,179)=7.39 | <0.001 |
| Expression | 43.8 ± 13.1 | 51.2 ± 13.3 | 45.9 ± 14.5 | F(2,179)=1.87 | 0.16 |
| Conflict | 59.6 ± 11.7 a*** | 55.7 ± 10.2 | 52.0 ± 12.6 | F(2,179)=7.65 | <0.001 |
| One-year Prevalence of Psychiatric Disorders at the 11-year Follow-up | |||||
| N (%) | N (%) | N (%) | |||
| Oppositional defiant disorder | 14 (19) | 2 (9) | 4 (4) | χ2(2)=5.70 | 0.06 |
| Conduct/antisocial personality disorder | 9 (12) a** | 0 (0) | 0 (0) | Exact | 0.002 |
| Major depressive disorder | 17 (23) a** | 2 (9) | 6 (7) | χ2(2)=6.58 | 0.04 |
| Bipolar disorder | 8 (11) | 0 (0) | 2 (2) | Exact | 0.15 |
| Multiple (≥2) anxiety disorder | 22 (30) a*** | 3 (14) a*** | 6 (7) | χ2(2)=12.66 | 0.002 |
| Psychoactive substance use disorder | 25 (34) | 7 (32) | 21 (23) | χ2(2)=1.63 | 0.44 |
| Smoking | 11 (15) | 5 (23) a** | 4 (4) | χ2(2)=6.95 | 0.03 |
| Lifetime School Functioning at the 11-year Follow-up | |||||
| Repeated grade | 25 (34) a*** | 5 (23) a** | 3 (3) | χ2(2)=15.71 | <0.001 |
| Special class | 26 (35) a*** | 6 (27) a** | 4 (4) | χ2(2)=17.50 | <0.001 |
| Tutoring | 67 (91) a*** | 19 (86) a*** | 36 (40) | χ2(2)=41.13 | <0.001 |
| Detention^ | 30 (62) | 9 (75) | 34 (45) | χ2(2)=5.43 | 0.07 |
| Suspension^ | 14 (30) a** | 4 (33) a* | 6 (8) | χ2(2)=9.10 | 0.01 |
| Expulsion^ | 2 (4) | 0 (0) | 0 (0) | Exact | 0.57 |
| Graduated high school^‡ | 43 (91) a** | 14 (100) | 73 (100) | Exact | 0.002 |
vs. Controls,
vs. Remittent ADHD;
p≤0.05,
p≤0.01,
p≤0.001
Missing data (Persistent ADHD, N=49; Remittent ADHD, N=14; Controls, N=76)
Limited to participants over 18 years of age
Fig. 3.
CBCL at baseline
Both ADHD groups had significantly higher rates of tutoring at baseline vs. controls (Table 2). The persistent ADHD group had significantly higher rates of repeated grades and placement in a special class, higher family environment scale (FES) conflict and lower FES cohesion scores vs. controls.
Persistent ADHD in girls was associated with significantly higher rates of +FH (at least one first-degree relative affected) of ADHD (69% [51/74]) and multiple (≥2) anxiety disorders (61% [45/74]) vs. controls (35% [32/91] and 38% [35/91], z=4.17 and z=2.76, p<0.001 and p=0.006, respectively). Remittent ADHD girls had a significantly higher rate of +FH of conduct/antisocial personality vs. controls (50% [11/22] vs. 20% [18/91], z=2.79, p=0.005). Persistent ADHD girls had a significantly higher rate of +FH of multiple anxiety disorders vs. Remittent ADHD girls (61% [45/74] vs. 36% [8/22], z=1.97, p=0.049).
Correlates of persistence
Persistent ADHD was significantly associated with higher rates of conduct disorder and major depressive disorder at follow-up versus controls (Table 2). Independent of ADHD persistence status, ADHD was associated with significant educational impairments. Participants with persistent ADHD had a significantly lower rate of high school graduation compared with controls.
Discussion
Using a prospective, longitudinal design, as well as comprehensive measures, and blind assessments, our 11-year follow-up found that patterns of persistence in girls with ADHD were highly dependent on the definition used. While 23% of the girls attained full remission in young adult years, the other 77% showed evidence of some form of persistence. Persistence of ADHD in girls was associated with higher baseline and follow- up rates of disruptive behavior, mood and anxiety disorders, school dysfunction, family conflict, and higher rates of positive family history of ADHD and anxiety disorders. These findings document that ADHD in girls is a persistent disorder and persistence and remission can be predicted over the long term based on patterns of comorbidity, familiality and adversity.
The rate of syndromatic remission is highly consistent with that observed by young adult years in our sample of boys with ADHD and with the meta-analysis of ADHD outcome studies (33) which estimated that 65% of ADHD youth continue to have ADHD or impairing symptoms of ADHD into young adulthood. However, in contrast to prior findings in boys (34), symptoms of inattention and hyperactivity/impulsivity remained relatively stable from adolescence through young adult years in girls with ADHD, indicating that ADHD continues to affect all components of the symptomatic picture of the disorder in girls in a relatively similar fashion. While the reasons for these differences between the sexes remain unclear, it is possible that ADHD symptoms in boys may be more sensitive to developmental changes in which maturation mitigates symptom expression making them less conspicuous (35). This latter idea predicts that the male predominance of ADHD seen among youth should diminish with age. In fact, studies of clinically referred adults suggest that ADHD is equally common among males and females (36). More work is needed to further evaluate this issue. The reason for the curvilinear pattern found for syndromatic persistence is also unclear. The constant rate of symptomatic persistence across age groups indicates that the lower rate of syndromatic persistentce in participants 19–21 year old age group is accompanied by a higher rate of symptomatic persistence compared to the other age groups.
Our findings that persistence of ADHD in girls was associated with greater psychiatric comorbidity are consistent with our previous study of boys (37), and work by others showing that conduct/aggressive symptoms predicted persistence of ADHD (23, 38, 39) and that adult ADHD was associated with impulsive aggression (40).
Persistent ADHD in girls was associated with being raised in non-intact families and in families showing high levels of family conflict and diminished levels of family cohesion. While these findings support our hypothesis that adversity is a predictor of persistence in girls with ADHD, we do not know the direction of this effect. More work is needed to disentangle whether family conflict leads to a persistent course or whether a persistent course is associated with increasing severity, which in turn could lead to family conflict. Irrespective of the direction of effect, efforts directed at improving family functioning could mitigate the course of the disorder.
Our finding that persistence of ADHD in girls was associated with higher rates of family history of ADHD is consistent with previous findings by our group showing that persistent ADHD impart a greater familial risk for ADHD to parents and siblings than do non-persistent cases (41) and with findings (39) showing that adult ADHD (by definition, a persistent form of the disorder) is a highly familial disorder.
Persistent ADHD in girls was also associated with significantly higher rate of a +FH of anxiety disorders vs. remittent cases. This finding may explain the higher personal risk for anxiety disorders in girls with ADHD. They also suggest that previous family studies linking these disorders (42) with ADHD may have been driven by persistent cases of ADHD.
The finding that persistence of ADHD in girls was associated with lower rates of high school graduation vs. controls is consistent with a large literature documenting impaired educational outcomes in participants with ADHD (43, 44). However, it is important to note that similarly impaired educational deficits were observed in the remitting cases. This finding stresses the critical importance of aggressively addressing ADHD during formative years irrespective of the fact that some cases will remit.
Our treatment history findings revealed that participants with persistent ADHD were more likely to receive pharmacotherapy for ADHD at some point in their lives compared to participants with remittent ADHD. This is consistent with Langley et al.’s (45) longitudinal findings that adolescents currently medicated with ADHD had more ADHD symptoms and a higher rate of ADHD diagnosis compared to adolescents no longer using medication. Longitudinal findings of Molina et al. (38) and retrospective findings of Lara et al. (46) found that treatment for ADHD in childhood did not predict functioning and was not associated with persistent ADHD.
Our results must be interpreted in the context of some methodological limitations. Our persistent ADHD group comprised participants meeting various definitions of persistence, and we lacked sufficient sample sizes to compare these different definitions individually. Our inclusion of symptomatic persistence in our definition is consistent with the proposed revision for DSM-V ADHD criteria for older adolescents and adults, namely, that four symptoms be required instead of six for inattention or hyperactivity/impulsivity. Although the vast majority of our participants (93%) were > 18 years, a small proportion of our sample had not yet reached adulthood. Another limitation of this longitudinal study is the broad age range of the sample (6 to 17 years at baseline). However, we did not find a significant difference in age at baseline or follow-up between participants who had persistent and remittent ADHD. Likewise, we found little relationship between age at follow-up and persistence (Figure 1).
Fig. 1.
Persistence of ADHD at 11- year follow-up.
Because our participants were clinically referred these findings may not generalize to community samples. Because our sample was mostly caucasian, our findings may not generalize to other ethnic groups. Because our sample was originally ascertained according to DSM-III-R criteria, it is possible that our results may not generalize to samples ascertained by DSM-IV criteria. However, considering the very high degree of overlap between the two definitions (93% of DSM-III-R cases received a DSM-IV diagnosis) (47) and our use of DSM-IV criteria in our follow-up assessment, any effect on these results should be minimal. Our attrition rate was high (31% in the ADHD group), highlighting the difficulty of following children into adulthood. However, we did not find any significant differences between participants who were retained and those who were lost to follow-up (32), suggesting that retained participants were representative of the original sample.
Despite these considerations, this 11-year follow-up showed that many girls with ADHD experience persistent symptoms and functional impairment into early adulthood. These findings further highlight the importance of attending to residual ADHD symptoms in order to evaluate patterns of persistence of ADHD in children growing up.
Significant outcomes.
Many girls with attention-deficit/hyperactivity disorder (ADHD) experience persistent symptoms and functional impairment into early adulthood.
ADHD in girls is a persistent disorder and persistence and remission can be predicted over the long term based on patterns of comorbidity, familiality and adversity
Attending to residual ADHD symptoms is important in evaluating patterns of persistence of ADHD in children growing up.
Limitations.
The persistent ADHD group included participants meeting various definitions of persistence.
Participants were clinically referred and mostly caucasian; therefore, these findings may not generalize to community samples and other ethnic groups.
Acknowledgements
This work was supported, in part by a grant from the Eli Lilly and Company Foundation and the Pediatric Psychopharmacology Philanthropy Fund.
Declaration of Interests:
Dr. Joseph Biederman is currently receiving research support from the following sources: Elminda, Janssen, McNeil, Next Wave Pharmaceuticals, and Shire. In 2011, Dr. Joseph Biederman gave a single unpaid talk for Juste Pharmaceutical Spain, and received honoraria from the MGH Psychiatry Academy for a tuition-funded CME course. He also received an honorarium from Cambridge University Press for a chapter publication. Dr. Biederman received departmental royalties from a copyrighted rating scale used for ADHD diagnoses, paid by Eli Lilly, Shire and AstraZeneca; these royalties are paid to the Department of Psychiatry at MGH. In 2010, Dr. Joseph Biederman received a speaker’s fee from a single talk given at Fundación Dr.Manuel Camelo A.C. in Monterrey Mexico. Dr. Biederman provided single consultations for Shionogi Pharma Inc. and Cipher Pharmaceuticals Inc.; the honoraria for these consultations were paid to the Department of Psychiatry at the MGH. Dr. Biederman received honoraria from the MGH Psychiatry Academy for a tuition-funded CME course. In 2009, Dr. Joseph Biederman received a speaker’s fee from the following sources: Fundacion Areces (Spain), Medice Pharmaceuticals (Germany) and the Spanish Child Psychiatry Association. In previous years, Dr. Joseph Biederman received research support, consultation fees, or speaker’s fees for/from the following additional sources: Abbott, Alza, AstraZeneca, Boston University, Bristol Myers Squibb, Celltech, Cephalon, Eli Lilly and Co., Esai, Forest, Glaxo, Gliatech, Hastings Center, Janssen, McNeil, Merck, MMC Pediatric, NARSAD, NIDA, New River, NICHD, NIMH, Novartis, Noven, Neurosearch, Organon, Otsuka, Pfizer, Pharmacia, Phase V Communications, Physicians Academy, The Prechter Foundation, Quantia Communications, Reed Exhibitions, Shire, The Stanley Foundation, UCB Pharma Inc., Veritas, and Wyeth.
In the past year, Dr. Faraone received consulting fees and was on Advisory Boards for Shire Development and received research support from Shire and the National Institutes of Health (NIH). In previous years, he received consulting fees or was on Advisory Boards or participated in continuing medical education programs sponsored by: Shire, McNeil, Janssen, Novartis, Pfizer and Eli Lilly. In previous years he received research support from Eli Lilly, Shire, Pfizer and the NIH. Dr. Faraone receives royalties from a book published by Guilford Press: Straight Talk about Your Child’s Mental Health.
Footnotes
Mr. Carter Petty, Ms. Katherine O’Connor, and Ms. Laran Hyder have no competing interests to report.
References
- 1.Mannuzza S, Klein RG, Truong NL, Moulton JL, 3rd, Roizen ER, Howell KH, et al. Age of methylphenidate treatment initiation in children with ADHD and later substance abuse: prospective follow-up into adulthood. Am J Psychiatry. 2008;165:604–609. doi: 10.1176/appi.ajp.2008.07091465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weiss G, Hechtman L, Milroy T, Perlman T. Psychiatric status of hyperactives as adults: a controlled prospective 15-year follow-up of 63 hyperactive children. Journal of the American Academy of Child and Adolescent Psychiatry. 1985;24:211–220. doi: 10.1016/s0002-7138(09)60450-7. [DOI] [PubMed] [Google Scholar]
- 3.Barkley RA, Fischer M. The unique contribution of emotional impulsiveness to impairment in major life activities in hyperactive children as adults. Journal of the American Academy of Child & Adolescent Psychiatry. 2010;49:503–513. doi: 10.1097/00004583-201005000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Satterfield JH, Faller KJ, Crinella FM, Schell AM, Swanson JM, Homer LD. A 30-year prospective follow-up study of hyperactive boys with conduct problems: adult criminality. J Am Acad Child Adolesc Psychiatry. 2007;46:601–610. doi: 10.1097/chi.0b013e318033ff59. [DOI] [PubMed] [Google Scholar]
- 5.Fergusson DM, Boden JM, Horwood LJ. Classification of behavior disorders in adolescence: scaling methods, predictive validity, and gender differences. J Abnorm Psychol. 2010;119:699–712. doi: 10.1037/a0018610. [DOI] [PubMed] [Google Scholar]
- 6.Biederman J, Monuteaux M, Mick E, Spencer T, Wilens T, Silva J, et al. Young Adult Outcome of Attention Deficit Hyperactivity Disorder: A Controlled 10 year Prospective Follow-Up Study. Psychological Medicine. 2006;36:167–179. doi: 10.1017/S0033291705006410. [DOI] [PubMed] [Google Scholar]
- 7.Polderman TJ, Boomsma DI, Bartels M, Verhulst FC, Huizink AC. A systematic review of prospective studies on attention problems and academic achievement. Acta Psychiatr Scand. 2010;122:271–284. doi: 10.1111/j.1600-0447.2010.01568.x. [DOI] [PubMed] [Google Scholar]
- 8.Danckaerts M, Heptinstall E, Chadwick O, Taylor E. A natural history of hyperactivity and conduct problems: self-reported outcome. Eur Child Adolesc Psychiatry. 2000;9:26–38. doi: 10.1007/s007870050113. [DOI] [PubMed] [Google Scholar]
- 9.Rasmussen P, Gillberg C. Natural outcome of ADHD with developmental coordination disorder at age 22 years: a controlled, longitudinal, community-based study. J Am Acad Child and Adolesc Psychiatry. 2000;39:1424–1431. doi: 10.1097/00004583-200011000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Steinhausen HC, Drechsler R, Foldenyi M, Imhof K, Brandeis D. Clinical course of attention-deficit/hyperactivity disorder from childhood toward early adolescence. J Am Acad Child Adolesc Psychiatry. 2003;42:1085–1092. doi: 10.1097/01.CHI.0000070241.24125.A3. [DOI] [PubMed] [Google Scholar]
- 11.Drechsler R, Brandeis D, Foldenyi M, Imhof K, Steinhausen HC. The course of neuropsychological functions in children with attention deficit hyperactivity disorder from late childhood to early adolescence. J Child Psychol Psychiatry. 2005;46:824–836. doi: 10.1111/j.1469-7610.2004.00384.x. [DOI] [PubMed] [Google Scholar]
- 12.Mannuzza S, Gittelman R. The adolescent outcome of hyperactive girls. Psychiatry Research. 1984;13:19–29. doi: 10.1016/0165-1781(84)90115-x. [DOI] [PubMed] [Google Scholar]
- 13.Young S, Heptinstall E, Sonuga-Barke EJ, Chadwick O, Taylor E. The adolescent outcome of hyperactive girls: self-report of psychosocial status. J Child Psychol Psychiatry. 2005;46:255–262. doi: 10.1111/j.1469-7610.2004.00350.x. [DOI] [PubMed] [Google Scholar]
- 14.Young S, Chadwick O, Heptinstall E, Taylor E, Sonuga-Barke EJ. The adolescent outcome of hyperactive girls. Self-reported interpersonal relationships and coping mechanisms. Eur Child Adolesc Psychiatry. 2005;14:245–253. doi: 10.1007/s00787-005-0461-z. [DOI] [PubMed] [Google Scholar]
- 15.Hinshaw SP, Owens EB, Sami N, Fargeon S. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. J Consult Clin Psychol. 2006;74:489–499. doi: 10.1037/0022-006X.74.3.489. [DOI] [PubMed] [Google Scholar]
- 16.Owens EB, Hinshaw SP, Lee SS, Lahey BB. Few girls with childhood attention-deficit/hyperactivity disorder show positive adjustment during adolescence. J Clin Child Adolesc Psychol. 2009;38:132–143. doi: 10.1080/15374410802575313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biederman J, Monuteaux M, Mick E, Spencer T, Wilens T, Klein K, et al. Psychopathology in females with attention-deficit/hyperactivity disorder: A controlled, five-year prospective study. Biological psychiatry. 2006;60:1098–1105. doi: 10.1016/j.biopsych.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 18.Babinski DE, Pelham WW, Jr, Molina BS, Gnagy EM, Waschbusch DA, Yu J, et al. Late adolescent and young adult outcomes of girls diagnosed with ADHD in childhood: an exploratory investigation. J Atten Disord. 2011;15:204–214. doi: 10.1177/1087054710361586. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dalsgaard S, Mortensen P, Frydenberg M, Thomsen P. Conduct problems, gender and adult psychiatric outcome of children with attention-deficit hyperactivity disorder. The British Journal of Psychiatry. 2002;181:416–421. doi: 10.1192/bjp.181.5.416. [DOI] [PubMed] [Google Scholar]
- 20.Gittelman R, Mannuzza S, Shenker R, Bonagura N. Hyperactive boys almost grown up: I. Psychiatric status. Archives of General Psychiatry. 1985;42:937–947. doi: 10.1001/archpsyc.1985.01790330017002. [DOI] [PubMed] [Google Scholar]
- 21.Loney J, Kramer J, Milich RS. The hyperactive child grows up: predictors of symptoms, delinquency and achievement at follow-up. In: Gadow KD, Loney J, editors. Psychosocial Aspects of Drug Treatment for Hyperactivity. Boulder, CO: Westview Press; 1981. pp. 381–416. [Google Scholar]
- 22.Taylor E, Sandberg S, Thorley G, Giles S. The epidemiology of childhood hyperactivity. New York: Oxford University Press; 1991. [Google Scholar]
- 23.Hart E, Lahey B, Loeber R, Applegate B, Frick P. Developmental change in attention-deficit hyperactivity disorder in boys: a four-year longitudinal study. Journal of Abnormal Child Psychology. 1995;23:729–749. doi: 10.1007/BF01447474. [DOI] [PubMed] [Google Scholar]
- 24.Biederman J, Faraone SV, Keenan K, Benjamin J, Krifcher B, Moore C, et al. Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder. Patterns of comorbidity in probands and relatives in psychiatrically and pediatrically referred samples. Archives of General Psychiatry. 1992;49:728–738. doi: 10.1001/archpsyc.1992.01820090056010. [DOI] [PubMed] [Google Scholar]
- 25.Biederman J, Faraone SV, Mick E, Williamson S, Wilens TE, Spencer TJ, et al. Clinical correlates of ADHD in females: findings from a large group of girls ascertained from pediatric and psychiatric referral sources. J Am Acad Child Adolesc Psychiatry. 1999;38:966–975. doi: 10.1097/00004583-199908000-00012. [DOI] [PubMed] [Google Scholar]
- 26.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders. Washington, D.C.: American Psychiatric Press; 1997. [Google Scholar]
- 27.Orvaschel H. Schedule for Affective Disorder and Schizophrenia for School-Age Children Epidemiologic Version. 5th Edition ed. Ft. Lauderdale: Nova Southeastern University, Center for Psychological Studies; 1994. [Google Scholar]
- 28.Weissman MM, Leckman JF, Merikangas KR, Gammon GD, Prusoff BA. Depression and anxiety disorders in parents and children: Results from the Yale Family Study. Archives of General Psychiatry. 1984;41:845–852. doi: 10.1001/archpsyc.1984.01790200027004. [DOI] [PubMed] [Google Scholar]
- 29.Hollingshead AB. Four Factor Index of Social Status. New Haven: Yale Press; 1975. [Google Scholar]
- 30.Keck P, Mcelroy S, Strakowski S, West S, Sax K, Hawkins J, et al. 12-month outcome of patients with bipolar disorder following hospitalization for a manic or mixed episode. American Journal of Psychiatry. 1998;155:646–652. doi: 10.1176/ajp.155.5.646. [DOI] [PubMed] [Google Scholar]
- 31.Biederman J, Mick E, Faraone SV. Age-dependent decline of symptoms of attention deficit hyperactivity disorder: Impact of remission definition and symptom type. American Journal of Psychiatry. 2000;157:816–818. doi: 10.1176/appi.ajp.157.5.816. [DOI] [PubMed] [Google Scholar]
- 32.Biederman J, Petty CR, Monuteaux MC, Fried R, Byrne D, Mirto T, et al. Adult psychiatric outcomes of girls with attention deficit hyperactivity disorder: 11-year follow-up in a longitudinal case-control study. Am J Psychiatry. 2010;167:409–417. doi: 10.1176/appi.ajp.2009.09050736. [DOI] [PubMed] [Google Scholar]
- 33.Faraone S, Biederman J, Mick E. The Age Dependent Decline Of Attention-Deficit/Hyperactivity Disorder: A Meta-Analysis Of Follow-Up Studies. Psychological Medicine. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- 34.Biederman J, Petty CR, Evans M, Small J, Faraone SV. How persistent is ADHD? A controlled 10-year follow-up study of boys with ADHD. Psychiatry Res. 2010;177:299–304. doi: 10.1016/j.psychres.2009.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Barkley R. Age dependent decline in ADHD: True recovery or statistical illusion? The ADHD Report. 1997;5:1–5. [Google Scholar]
- 36.Biederman J, Faraone SV, Spencer T, Wilens T, Mick E, Lapey KA. Gender differences in a sample of adults with attention deficit hyperactivity disorder. Psychiatry Research. 1994;53:13–29. doi: 10.1016/0165-1781(94)90092-2. [DOI] [PubMed] [Google Scholar]
- 37.Biederman J, Faraone SV, Milberger S, Curtis S, Chen L, Marrs A, et al. Predictors of persistence and remission of ADHD: results from a four-year prospective follow-up study of ADHD children. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:343–351. doi: 10.1097/00004583-199603000-00016. [DOI] [PubMed] [Google Scholar]
- 38.Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. MTA at 8 Years: Prospective Follow-up of Children Treated for Combined-Type ADHD in a Multisite Study. J Am Acad Child Adolesc Psychiatry. 2009;48:484–500. doi: 10.1097/CHI.0b013e31819c23d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Faraone SV, Biederman J, Spencer T, Mick E, Murray K, Petty C, et al. Diagnosing adult attention deficit hyperactivity disorder: are late onset and subthreshold diagnoses valid? Am J Psychiatry. 2006;163:1720–1729. doi: 10.1176/ajp.2006.163.10.1720. quiz 859. [DOI] [PubMed] [Google Scholar]
- 40.Dowson JH, Blackwell AD. Impulsive aggression in adults with attention-deficit/hyperactivity disorder. Acta Psychiatr Scand. 2010;121:103–110. doi: 10.1111/j.1600-0447.2009.01460.x. [DOI] [PubMed] [Google Scholar]
- 41.Faraone SV, Biederman J, Feighner JA, Monuteaux MC. Assessing symptoms of attention deficit hyperactivity disorder in children and adults: which is more valid? Journal of Consulting and Clinical Psychology. 2000;68:830–842. [PubMed] [Google Scholar]
- 42.Biederman J, Faraone SV, Keenan K, Steingard R, Tsuang MT. Familial association between attention deficit disorder and anxiety disorders. American Journal of Psychiatry. 1991;148:251–256. doi: 10.1176/ajp.148.2.251. [DOI] [PubMed] [Google Scholar]
- 43.Antshel K, Faraone SV, Stallone K, Nave A, Kaufmann F, Doyle AE, et al. Is Attention Deficit Hyperactivity Disorder a valid diagnosis in the presence of high IQ? Journal of Child Psychology and Psychiatry. 2007;48:687–694. doi: 10.1111/j.1469-7610.2007.01735.x. [DOI] [PubMed] [Google Scholar]
- 44.Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult outcome of hyperactive children: adaptive functioning in major life activities. J Am Acad Child Adolesc Psychiatry. 2006;45:192–202. doi: 10.1097/01.chi.0000189134.97436.e2. [DOI] [PubMed] [Google Scholar]
- 45.Langley K, Fowler T, Ford T, Thapar AK, Van Den Bree M, Harold G, et al. Adolescent clinical outcomes for young people with attention-deficit hyperactivity disorder. Br J Psychiatry. [Multicenter Study] 2010;196:235–240. doi: 10.1192/bjp.bp.109.066274. [DOI] [PubMed] [Google Scholar]
- 46.Lara C, Fayyad J, De Graaf R, Kessler RC, Aguilar-Gaxiola S, Angermeyer M, et al. Childhood predictors of adult attention-deficit/hyperactivity disorder: results from the World Health Organization World Mental Health Survey Initiative. Biol Psychiatry. 2009;65:46–54. doi: 10.1016/j.biopsych.2008.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Biederman J, Faraone SV, Weber W, Russell RL, Rater M, Park K. Correspondence between DSM-III-R and DSM-IV Attention Deficit Hyperactivity Disorder (ADHD) Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1682–1687. doi: 10.1097/00004583-199712000-00016. [DOI] [PubMed] [Google Scholar]