Abstract
The present investigation examined the main and interactive effects of anxiety sensitivity and behavioral distress tolerance, indexed using the breath-holding task, in relation to PTSD symptom severity among trauma-exposed adults. Participants were 88 adults (63.6% women; Mage = 22.9, SD = 9.1, Range = 18-62), recruited from the community, who met DSM-IV-TR PTSD Criterion A for lifetime trauma exposure. Covariates included number of potentially traumatic events, nonclinical panic attack history, and participant sex. Anxiety sensitivity was significantly incrementally associated with PTSD total symptom severity, as well as Avoidance and Hyperarousal symptom severity (p's < .01). Breath-holding duration was not significantly related to PTSD symptom severity (p's > .05). However, breath-holding duration emerged as a significant moderator of the association between anxiety sensitivity and PTSD Avoidance symptom severity, such that lower breath-holding duration exacerbated the effect of heightened anxiety sensitivity with regard to PTSD Avoidance symptom severity.
Keywords: PTSD, trauma, distress tolerance, anxiety sensitivity
There has been increasing scholarly attention on the investigation of malleable cognitive-affective factors underlying risk and maintenance for posttraumatic stress disorder (PTSD) that may be targeted in intervention efforts (Ehring, Ehlers, & Glucksman, 2008; Elwood, Hahn, Olatunji, & Williams, 2009; Tull, Barrett, McMillan, & Roemer, 2007). Yet, only a small percentage of this work has focused on sensitivity to, and tolerance of, distressing stimuli (Vujanovic, Bernstein, & Litz, 2011). This limitation is unfortunate, as there is a larger psychopathology literature suggesting how one reacts to distressing internal and external stimuli may play a formative role in the etiology and maintenance of anxiety and stress disorders (Leyro, Zvolensky, & Bernstein, 2010; Zvolensky, Vujanovic, Bernstein, & Leyro, 2010).
Anxiety sensitivity, defined as the fear of anxiety and related consequences (McNally, 2002), is one promising cognitive risk and maintenance factor relevant to PTSD. Past cross-sectional studies have shown that higher levels of anxiety sensitivity are related to greater levels of PTSD symptoms among both children and adults (e.g., Leen-Feldner, Feldner, Reardon, Babson, & Dixon, 2008; Lang, Kennedy, & Stein, 2002; Taylor, Koch, & McNally, 1992). Longitudinal investigations also have found that greater levels of anxiety sensitivity predict greater PTSD symptom severity and vice versa (Marshall, Miles, & Stewart, 2010; Simpson, Jakupcak, & Luterek, 2006). Theoretically, individuals who catastrophize about the implications of interoceptive cues (i.e., those high in anxiety sensitivity) may experience enhanced negative emotional learning to trauma-relevant stimuli and early PTSD-relevant symptoms, which may in turn serve to exacerbate such symptoms (Bernstein et al., 2005). Additionally, increased levels of PTSD symptoms may exacerbate an individual's sensitivity to trauma-related interoceptive cues (e.g., Marshall et al., 2010). Furthermore, among trauma-exposed individuals, higher levels of anxiety sensitivity are related to the experience of post-trauma panic attacks, suggesting potentially enhanced interoceptive conditioning among these individuals (Nixon & Bryant, 2003). Finally, neuroimaging work has found that nonclinical individuals high in anxiety sensitivity evidence increased amygdala activation in response to emotional stimuli (Stein, Simmons, Feinstein, & Paulus, 2007), providing further evidence that anxiety sensitivity plays an important role in emotional processing.
A second construct of relevance to bridging our understanding of PTSD symptom expression is distress tolerance (Vujanovic et al., 2011). Distress tolerance reflects the perceived and/or actual behavioral capacity to withstand exposure to aversive or threatening experiential states (e.g., negative emotions, uncomfortable physical sensations; Leyro et al., 2010). Past work indicates distress tolerance may be an important factor related to emotional reactivity to interoceptive distress (Schmidt, Mitchell, Keough, & Riccardi, 2011). For example, lower levels of perceived distress tolerance for emotional distress and physical stress, and a lesser ability to withstand acute episodes of emotional stress, are significantly related to an increased risk of anxiety symptoms and panic attacks (Boelen & Reijntjes, 2009; Bonn-Miller, Zvolensky, & Bernstein, 2009; Daughters et al., 2009; Marshall et al., 2008) as well as escape behavior in response to somatic arousal (Asmundson & Stein, 1994; Marshall et al., 2008; Telch, Jacquin, Smits, & Powers, 2003). Preliminary work suggests that lower levels of perceived emotional distress tolerance are related to greater PTSD symptom severity (Vujanovic, Bonn-Miller, Potter, Marshall, & Zvolensky, 2011; Marshall-Berenz, Vujanovic, Bonn-Miller, Bernstein, & Zvolensky, 2010); however, behavioral distress tolerance has not been extensively studied in relation to PTSD. Moreover, there has not yet been a direct test of the relative explanatory value of distress tolerance and anxiety sensitivity in the context of one another with regard to PTSD symptoms. This limitation impairs the ability to discern the unique and overlapping roles of anxiety sensitivity and distress tolerance in terms of PTSD symptoms.
Beyond the individual significance of anxiety sensitivity and distress tolerance in terms of PTSD, there is apt to be clinically-relevant interplay between these factors. Indeed, trauma-exposed persons with higher levels of anxiety sensitivity and lower tolerance for interoceptive distress (e.g., physical sensations) may be more likely to manifest greater PTSD symptom severity. That is, lower levels of tolerance for internal stress (e.g., bodily petrubation) may moderate the relation between anxiety sensitivity and PTSD symptoms among trauma-exposed persons. Namely, trauma-exposed individuals experiencing greater levels of anxiety sensitivity who cannot as effectively tolerate such distress may interpret distressing symptoms as more severe, thereby increasing reactivity to and severity of such symptoms. Conversely, higher levels of tolerance for emotionally or physically distressing or uncomfortable states may attenuate relative risk for heightened PTSD symptoms.
Together, the aim of the current study was to investigate the main and interactive effects of anxiety sensitivity and behavioral distress tolerance in relation to PTSD symptom severity among trauma-exposed adults. Specifically, it was hypothesized that: (1) higher levels of anxiety sensitivity would be related to higher levels of PTSD symptom severity; (2) lower levels of behavioral distress tolerance (defined here as shorter latency to termination of a breath-holding challenge; Hajek, Belcher, & Stapleton, 1987) would be related to higher levels of PTSD symptom severity; and (3) behavioral distress tolerance would moderate the relationship between anxiety sensitivity and PTSD symptom severity, such that anxiety sensitivity-PTSD relations would be particularly relevant among individuals low in distress tolerance. All effects were expected above and beyond the variance accounted for by the theoretically relevant covariates of number of potentially traumatic events (PTEs), panic attack history, and participant sex, for those variables exhibiting significant zero-order relationships with the criterion variables. Panic attacks have demonstrated robust associations with PTSD symptoms (e.g., Falsetti & Resnick, 2000; Resnick, Falsetti, Kilpatrick, & Foy, 1994); therefore, it is important to ensure that associations between the variables of interest and PTSD symptoms in the current sample are not better accounted for by panic reactivity. Furthermore, significant differences in men's and women's abilities to hold their breath have been detected (Hajek et al., 1987); therefore, it is important to ensure that participant sex does not better account for distress tolerance-PTSD relations.
Method
Participants
Participants were 88 adults (63.6% women; Mage = 22.9, SD = 9.1, Range = 18-62) from the community who met DSM-IV-TR Criterion A (American Psychiatric Association [APA], 2000) for lifetime trauma exposure on the Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995). The ethnic distribution was consistent with the overall recruitment environment: 96.5% Caucasian, 1.2% Hispanic/Latino, 1.2% Asian, and 1.2% Biracial/Other.
The current study data were collected as part of a larger laboratory investigation examining cognitive risk factors among individuals with and without a recent history of nonclinical panic attacks. Inclusionary criteria for the primary investigation were: (a) being between the ages of 18-65 years; and (b) either meeting criteria for a past 2-year history of nonclinical, unexpected panic attacks or having no lifetime history of panic attacks. To be included in the current analyses, individuals had to meet DSM-IV-TR Criterion A for trauma exposure (APA, 2000). Exclusionary criteria were: (a) current psychotropic medication use; (b) alcohol or substance dependence in the last 6 months; (c) lifetime panic disorder diagnosis; (d) current psychosis or suicidal ideation; and (e) limited mental competency or the inability to provide informed, written consent. An initial 154 participants were enrolled after a brief phone screen, of which 5 (3.2%) participants were ruled out at the baseline session due to not meeting the panic attack criteria outlined above. Of the 149 eligible participants, 88 (59%) met DSM-IV-TR criteria for trauma exposure and were included in the current data analysis.
Measures
Structured Clinical Interview for DSM-IV
Non-patient Version (SCID-I/NP; First, Spitzer Gibbon, & Williams, 1995). The SCID-I/NP was administered: (1) to assess whether participants met criteria for a recent (past two years) history of panic attacks, as well as current (past month or past six months for substance dependence) psychopathology, and (2) to assess for current suicidal ideation (see exclusionary criteria). Approximately 20% of the SCID-I/NP administrations were observed and reviewed by the P.I. (EMB) to ensure inter-rater reliability, with no cases of diagnostic disagreement noted.
Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995)
The CAPS was employed to measure the frequency and intensity of current (past month) PTSD symptoms, as well as to assess current (past month) PTSD diagnostic status. All individuals met the DSM-IV-TR PTSD Criteria A1 and A2 (APA, 2000, p. 467). The CAPS Life Events Checklist was used to index number of PTEs; all degrees of exposure (i.e., “happened to me,” “witnessed it,” “learned about it”) were included to comprise a comprehensive index of perceived past life traumatic stressors (i.e., number of PTEs variable). This index of PTEs does not represent Criterion A events necessarily, given that the majority of events were not assessed for Criterion A status. Only the “most bothersome” event indicated on the Life Events Checklist was assessed for Criterion A1 and A2 status on the CAPS, with the most bothersome event meeting Criterion A status being referenced for the CAPS administration. Past work has found that the Life Events Checklist has good test-retest reliability, good convergent validity with the Traumatic Life Events Checklist (Kubany et al., 2000), and significant relations with PTSD symptom severity (Gray, Litz, Hsu, & Lombardo, 2004). Consistent with prior research (Monson et al. 2006; Weathers, Ruscio, & Keane 1999), symptom severity was defined as the sum of the frequency and intensity ratings. Twenty percent of the CAPS administrations were observed and reviewed by the P.I. (EMB) to ensure inter-rater reliability, with no cases of diagnostic disagreement noted.
Anxiety Sensitivity Index - III (ASI-III; Taylor et al., 2007)
The ASI-III is an 18-item self-report measure, which assesses sensitivity to, and discomfort with, physical sensations. Participants are instructed to rate the degree to which they believe the 18 statements apply to them (e.g., “It scares me when my heart beats rapidly”) on a Likert-type scale from 0 (“very little”) to 4 (“very much”). The ASI-III was developed to improve upon the factor structure of the original 16-item ASI (Reiss et al., 1986), which evidenced good internal consistency, test-retest reliability, and convergent validity with other measures of psychiatric symptoms (Peterson & Reiss, 1992; Zinbarg, Mohlman, & Hong, 1999), but which evidenced inconsistent findings with regard to the fit of its established three-factor model (Taylor et al., 2007). Internal consistency of the ASI-III total score in the current sample was excellent (α = .94).
Breath-Holding Task (Hajek et al., 1987)
The breath-holding task has been administered as a behavioral index of physical distress tolerance. The task requires participants to hold their breath as long as they can. In the present study, participants completed two breath-holding trials, during which they were instructed to inhale deeply, exhale, and then inhale and hold their breath as long as they could. Similar to past work (Hajek et al., 1987), distress tolerance on the breath-holding task was defined as the average duration (in seconds) across the two trials that participants were able to hold their breath.
Procedure
All study procedures were approved by the Institutional Review Board at the University of Vermont. Recruitment materials describing a study on “emotion” were circulated in the community, via flyers placed in high traffic areas (e.g., downtown bulletin boards and restaurants, university campuses) and advertisements placed in local newspapers. Community members who responded to advertisements were scheduled for a session in the laboratory to determine eligibility and collect study data. Upon arrival to the laboratory, interested participants first provided informed consent. The SCID-I/NP and CAPS were then administered by a clinical psychology doctoral candidate to determine eligibility based on the criteria identified above. Eligible participants then completed a battery of self-report measures and the breath-holding task. Eligible participants were compensated $30 for their involvement with all elements of the study, which also included a final laboratory component (not discussed here); ineligible participants were compensated $10 for participating in the SCID-N/P and CAPS administration.
Data-Analytic Plan
Analyses were conducted in PASW Statistics 18.0. First, zero-order relations were evaluated among the predictor and criterion variables. Second, a series of hierarchical linear regression analyses was conducted to evaluate whether the main and interactive effects of anxiety sensitivity and behavioral distress tolerance (i.e., breath-holding duration) were significantly related to CAPS - PTSD total (and symptom cluster) severity. The covariates of number of PTEs endorsed on the CAPS Life Events Checklist and panic attack group were entered into step one of the regression equations. The main effects (mean-centered) of ASI-III total score and breath-holding duration (seconds) were entered simultaneously as a block into step two. The interaction term, computed from mean-centered main effects, was entered at step three. The criterion variables were past month CAPS – PTSD Total, Re-experiencing, Avoidance, and Hyperarousal symptom severity (corrected using logarithmic transformation). All tests were two-tailed with an alpha level set at .05.
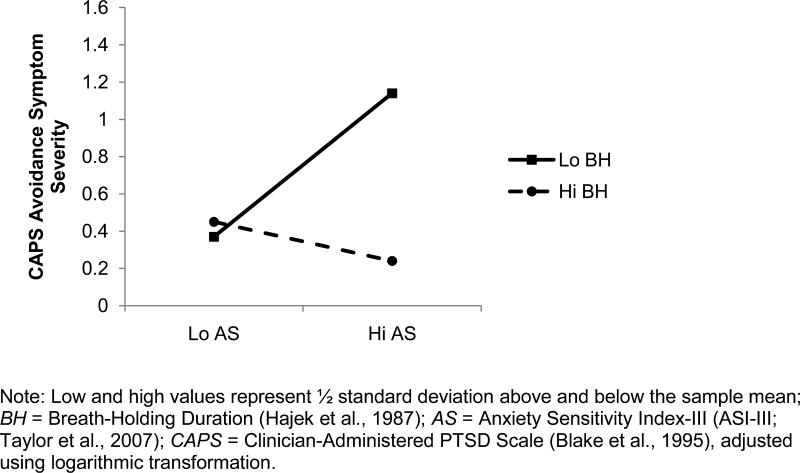
The forms of any significant interactions were subsequently examined both graphically, as per recommendations from Cohen and Cohen (1983), and statistically (Holmbeck, 2002). First, on the basis of recommendations of Cohen and Cohen (pp. 323, 419), we examined the form of these interactions by inserting specific values for each predictor variable (0.5 SD above and below the mean) into the regression equation associated with the described analysis. Furthermore, on the basis of recommendations of Holmbeck (2002), we conducted post hoc probing analyses on the data to examine the significance of the simple slopes and interactions.
Results
Participant Characteristics
As assessed by the SCID-I/NP (First et al., 1995), 45.5% of the sample met criteria for current (past month) axis I psychopathology. Participants endorsing current psychopathology met criteria for an average of 2.1 (SD = 1.5) diagnoses. Specifically, 15.9% of the total sample met criteria for Social Anxiety Disorder, 12.5% met criteria for Generalized Anxiety Disorder, 11.4% met criteria for Specific Phobia, 9.1% met criteria for Cannabis Abuse, 8.0% met criteria for Dysthymia, 6.9% met criteria for Alcohol Abuse, 5.7% met criteria for Major Depressive Disorder, 4.5% met criteria for Obsessive-Compulsive Disorder, 2.3% met criteria for Eating Disorder NOS, and 1.1% met criteria for Bipolar Disorder. Additionally, due to study entry criteria, 50.0% of the sample met criteria for past two-year nonclinical, unexpected panic attacks.
Participants in the current study endorsed at least one Criterion A traumatic event and reported an average of 7.7 (SD = 5.7) PTEs. Participants completed the CAPS with reference to their reported “worst” traumatic event that met DSM-IV-TR PTSD Criterion A (APA, 2000). In terms of participants’ report of “worst” traumatic event, 21.8% of the sample endorsed a sudden unexpected death, 14.9% endorsed a transportation accident, 12.6% endorsed a sexual assault, 12.6% endorsed a life-threatening illness or injury, 8.0% endorsed an “other” traumatic event, 6.9% endorsed a sudden violent death, 5.7% endorsed a physical assault, 5.7% endorsed a serious accident at home or work, 4.6% endorsed an unwanted sexual experience, 3.4% endorsed a natural disaster, 2.3% endorsed an assault with a weapon, and 1.1% endorsed a fire or explosion. Participants scored an average of 12.9 (SD = 15.9) on CAPS severity ratings (frequency + intensity), indicating generally low levels of PTSD symptoms (e.g., minimum score of 45 reliably corresponds to PTSD diagnosis; Weathers et al., 1999), with 4.5% meeting criteria for a current (past month) PTSD diagnosis. With regard to the symptom clusters, 50.0% of the sample met criteria for 1 or more Re-experiencing symptoms, 10.2% for 3 or more Avoidance symptoms, and 17.0% for 2 or more Hyperarousal symptoms.
Descriptive Statistics and Zero-Order Correlations
See Table 1 for descriptive statistics and zero-order correlations among the variables studied. Due to issues of normality in the CAPS criterion variables, all CAPS variables underwent logarithmic transformation. Number of PTEs and participant sex were significantly negatively correlated, with men reporting more lifetime traumas compared to women. Panic attack group was significantly positively related to ASI-III total scores, with individuals endorsing a positive panic attack history reporting greater levels of anxiety sensitivity. The covariate of participant sex was not significantly related to any criterion variables; therefore, sex was not included as a covariate in the regression analyses. ASI-III and breath-holding duration were not significantly related to one another (p = .88).
Table 1.
Descriptive Statistics and Zero-Order Correlations of Sample (n=88)
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | Mean or % | SD | Observed Range |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Number of PTEs | 1 | 7.7 | 5.7 | 1 – 37 | ||||||||
| 2. Panic Attack Group (% positive) | .01 | 1 | 50.0% | |||||||||
| 3. Participant Sex (% women) | -.21* | .12 | 1 | 63.6% | ||||||||
| 4. ASI-III | .13 | .39** | -.12 | 1 | 18.2 | 13.0 | 0 – 66 | |||||
| 5. Breath-Holding Duration (seconds) | .20* | -.10 | -.41** | -.02 | 1 | 48.9 | 21.0 | 15 – 130 | ||||
| 6. CAPS – Totala | .19 | .32** | -.08 | .35** | -.17 | 1 | 12.9 | 15.9 | 0 – 66 | |||
| 7. CAPS – Re-experiencinga | .21* | .20 | -.03 | .26* | -.17 | .88** | 1 | 4.3 | 5.3 | 0 – 27 | ||
| 8. CAPS – Avoidancea | .12 | .25* | -.13 | .31** | -.11 | .81** | .66** | 1 | 4.6 | 6.9 | 0 – 27 | |
| 9. CAPS – Hyperarousala | .14 | .33** | -.14 | .43** | -.17 | .80** | .64** | .53** | 1 | 4.0 | 6.2 | 0 – 32 |
Note:
p < .05
p < .01
Log-adjusted for correlations, unaltered for descriptive statistics to allow for interpretation of scores
Number of PTEs = Number of potentially traumatic events endorsed on the CAPS – Life Events Checklist (Blake et al., 1995); Panic Attack Group = Past 2 year history of nonclinical, unexpected panic attacks (1 = no history, 2 = positive history) as assessed by the Structured Clinical Interview for DSM-IV Non-Patient Version (SCID-I/NP; First et al., 1995); Participant Sex (1 = male, 2 = female); ASI-III = Anxiety Sensitivity Index – III (Taylor et al., 2007); Breath-Holding Duration = Average latency to termination of breath-holding task in seconds (Hajek et al., 1987); CAPS = Clinician-Administered PTSD Scale (Blake et al., 1995).
Regression Results
See Table 2 for regression output. The proposed model accounted for 21.2% of variance in CAPS total symptom severity (F(5, 87) = 4.41, p = .001). Step one of the model accounted for 11.4% of variance (p < .01), with panic group being the only significant predictor at that step. Step two of the model accounted for a unique 8.1% of variance (p < .05), with the main effect of ASI-III being a significant predictor and breath-holding duration trending towards statistical significance (p = .09). The interaction at step three of the model was not significant
Table 2.
Anxiety Sensitivity, Breath-Holding Duration, and PTSD Symptom Severity
| Criterion Variable: PTSD Total Symptom Severity | ||||
|---|---|---|---|---|
| R2 | t | β | sr2 | |
| Step 1 | .11** | |||
| Number of PTEs | 1.69 | .17 | .03 | |
| Panic Attack Group | 2.89** | .30 | .09 | |
| Step 2 | .08* | |||
| ASI-III | 2.31* | .25 | .05 | |
| Breath-Holding Duration | -1.71 | -.18 | .03 | |
| Step 3 | .02 | |||
| Interaction Term | -1.30 | -.13 | .02 | |
| Criterion Variable: PTSD Re-experiencing Symptom Severity | ||||
|---|---|---|---|---|
| R2 | t | β | sr2 | |
| Step 1 | .07* | |||
| Number of PTEs | 1.90 | .20 | .04 | |
| Panic Attack Group | 1.66 | .17 | .03 | |
| Step 2 | .07* | |||
| ASI-III | 1.76 | .20 | .03 | |
| Breath-Holding Duration | -1.89 | -.20 | .04 | |
| Step 3 | .01 | |||
| Interaction Term | -.92 | -.10 | .01 | |
| Criterion Variable: PTSD Avoidance Symptom Severity | ||||
|---|---|---|---|---|
| R2 | t | β | sr2 | |
| Step 1 | .07* | |||
| Number of PTEs | .99 | .11 | .01 | |
| Panic Attack Group | 2.28* | .24 | .06 | |
| Step 2 | .06* | |||
| ASI-III | 2.17* | .24 | .05 | |
| Breath-Holding Duration | -1.14 | -.12 | .01 | |
| Step 3 | .05* | |||
| Interaction Term | -2.15* | -.23 | .05 | |
| Criterion Variable: PTSD Hyperarousal Symptom Severity | ||||
|---|---|---|---|---|
| R2 | t | β | sr2 | |
| Step 1 | .11** | |||
| Number of PTEs | .95 | .10 | .01 | |
| Panic Attack Group | 3.11** | .32 | .10 | |
| Step 2 | .12** | |||
| ASI-III | 3.38** | .36 | .11 | |
| Breath-Holding Duration | -1.15 | -.12 | .01 | |
| Step 3 | .02 | |||
| Interaction Term | -1.61 | -.16 | .02 | |
Note:
p < .05
p < .01
Number of PTEs = Number of potentially traumatic events endorsed on the CAPS – Life Events Checklist (Blake et al., 1995); Panic Attack Group = Past 2 year history of nonclinical, unexpected panic attacks (1 = no history, 2 = positive history) as assessed by the Structured Clinical Interview for DSM-IV Non-Patient Version (SCID-I/NP; First et al., 1995); Participant Sex (1 = male, 2 = female); ASI-III = Anxiety Sensitivity Index – III (Taylor et al., 2007); Breath-Holding Duration = Average latency to termination of breath-holding task in seconds (Hajek et al., 1987); CAPS = Clinician-Administered PTSD Scale (Blake et al., 1995).
The proposed model accounted for 14.7% of variance in CAPS Re-experiencing symptom severity (F(5, 87) = 2.83, p < .05). Step one of the model accounted for 6.8% of variance (p = .05), with number of traumas evidencing a statistical trend (p = .06) at that step. Step two of the model accounted for 7.0% of unique variance (p < .05), with ASI-III (p = .08) and breath-holding duration (p = .06) evidencing statistical trends at that step. Step three of the model was not significant.
The proposed model accounted for 17.7% of variance in CAPS Avoidance symptom severity (F(5, 87) = 3.52, p < .01). Step one of the model accounted for 6.7% of variance (p = .05), with panic group being the only significant predictor at that step. Step two of the model accounted for an additional 6.4% of variance (p = .05), with the main effect of ASI-III being a significant predictor at that step. The interaction at step three of the model accounted for an additional 4.6% of variance (p < .05).
The proposed model accounted for 25.3% of variance in CAPS Hyperarousal symptom severity (F(5, 87) = 5.55, p < .001). Step one of the model accounted for 10.9% of variance (p < .01), with panic group being the only significant predictor at that step. Step two of the model accounted for an additional 12.0% of variance (p < .01), with the main effect of ASI-III being the only significant predictor at that step. Step three of the model was not significant.
Examination of Significant Interaction
Please see Figure 1 for a graphical representation of the significant interaction between ASI-III and breath-holding duration in relation to CAPS Avoidance symptom severity. As shown in the figure, the relationship between anxiety sensitivity and PTSD Avoidance symptoms was greatest among those low in behavioral distress tolerance, such that individuals high in anxiety sensitivity who exhibited low breath-holding duration reported the greatest levels of Avoidance symptoms. Post hoc probing analyses of the simple slopes and interactions supported that breath-holding duration significantly moderated the relationship between ASI-III and CAPS Avoidance symptom severity. The relationship between ASI-III and CAPS Avoidance symptom severity was statistically significant when breath-holding duration was low (t = 3.39, β = .57, p = .001), such that symptom severity was higher among those with elevated levels of anxiety sensitivity. However, the relation between ASI-III and CAPS total symptom severity was not statistically significant when breath-holding duration was high (t = -.75, β = -.16, p = .46).
Figure 1.
Interaction of Anxiety Sensitivity and Breath-Holding Duration in Relation to CAPS Avoidance Symptom Severity
Discussion
The present investigation examined the main and interactive effects of anxiety sensitivity and behavioral distress tolerance in relation to PTSD symptom severity among trauma-exposed adults. Results were partially consistent with hypotheses. Anxiety sensitivity was significantly incrementally associated with PTSD total symptom severity as well as with Avoidance and Hyperarousal symptom severity. Interestingly, despite a significant zero-order correlation (r = .39, p < .01), anxiety sensitivity was not significantly incrementally associated with Re-Experiencing symptom severity, perhaps due to the relatively low levels of PTSD symptoms reported in this non-clinical sample. Taken together, the anxiety sensitivity-PTSD associations documented here add to the growing literature focused upon the clinical relevance of anxiety sensitivity as a risk and maintenance factor for PTSD (e.g., Marshall et al., 2010).
Behavioral distress tolerance, operationally defined in the current study as breath-holding duration, evidenced a trend towards statistical significance in relation to PTSD total and Re-experiencing symptoms. It may be the case that behaviorally observed distress tolerance does not evidence similar relations to PTSD as perceived (i.e., self-report) distress tolerance indices (Marshall-Berenz et al., 2010; Vujanovic et al., 2011; Vujanovic, Bonn-Miller et al., 2011). It is possible that individuals’ perceptions of their ability to tolerate distress are more important in relation to PTSD symptoms than one's actual ability to tolerate distress. However, further work in clinical populations is needed to better understand distress tolerance-PTSD relations.
Finally, a significant interactive effect of anxiety sensitivity by breath-holding duration emerged with regard to PTSD Avoidance symptom severity, contributing 4.6% of unique variance to the model. Post hoc analyses documented that breath-holding duration significantly moderated anxiety sensitivity-PTSD Avoidance symptom associations, such that lower levels of breath-holding duration exacerbated the effects of heightened anxiety sensitivity on PTSD Avoidance symptom severity. This novel, albeit preliminary, model presents clinically useful information about the potential interplay of two prominent cognitive-affective factors in relation to PTSD. Although replication and extension of this work is necessary to facilitate more sophisticated theory-building in this regard, this investigation puts forth an integrative conceptual model for advancing our understanding of the roles of cognitive-affective vulnerability factors in PTSD symptom expression. To move this literature forward, more advanced studies (e.g., laboratory manipulation) of the factors underlying trauma-related psychopathology are needed to refine our understanding of not only risk and maintenance for PTSD, but also the etiology and manifestation of co-occurring disorders (e.g., PTSD and panic disorder) among trauma-exposed individuals (e.g., Vujanovic, Zvolensky, & Bernstein, 2008). Also important to consider and test in future research is whether anxiety sensitivity and behavioral distress tolerance represent general risk factors for psychopathology, or whether under certain conditions, they evidence unique relations to PTSD specifically.
The present findings should be considered in the context of several noteworthy study limitations. First, the investigation was based on a relatively small, racially homogeneous sample of community-recruited trauma-exposed participants. It is important for future work to extend these findings with larger more diverse samples in order to gain confidence in the present findings. Second, the participants in the study evidenced low levels of PTSD symptoms. It is possible that the current sample possesses particular resiliency factors, given that they have been exposed to trauma but the vast majority has not developed PTSD. It is necessary to replicate the current study in clinical populations with moderate to high levels of PTSD symptoms. Third, the study utilized a cross-sectional design, impeding the examination of temporal relations among variables studied. This line of inquiry could be strengthened by the implementation of prospective designs and experimental paradigms, such as trauma-relevant cue reactivity protocols (e.g., script-driven imagery; Coffey et al., 2002). Fourth, the current study did not assess past history of PTSD, which is typically considered a risk factor for future PTSD symptoms. Future work would benefit from lifetime PTSD assessment. Fifth, the current investigation examined the interplay of two theoretically-relevant factors, anxiety sensitivity and behavioral distress tolerance, with regard to PTSD symptom severity. It is important for future work to advance this line of inquiry by also examining the interplay of other cognitive-affective factors (e.g., mindfulness) within this framework to promote a more multi-faceted understanding of PTSD symptom expression and maintenance. Furthermore, as alternative behavioral and self-report measures of distress tolerance exist (e.g., Paced Auditory Serial Addition Task-Computerized; Lejuez, Kahler, & Brown, 2003), future work would benefit from investigating the interactive effects of a variety of distress tolerance measures in relation to anxiety sensitivity and other pertinent factors in terms of PTSD symptom expression.
Highlights.
- Higher levels of anxiety sensitivity are related to greater total, Avoidance and Hyperarousal PTSD symptom severity
- Main effect of behavioral distress tolerance was not related to PTSD symptoms
- Distress tolerance moderates the relationship between anxiety sensitivity and PTSD Avoidance symptom severity
Acknowledgements
This research was supported by a National Institute on Mental Health National Research Service Award (1 F31 MH080453-01A1) awarded to Erin C. Berenz. This research was also supported by grants (1 R01 DA027533-01; 1 R01 MH076629-01) awarded to Dr. Michael Zvolensky. The views expressed here are the authors’ and do not necessarily represent those of the United States Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed., text revision Author; Washington, DC: 2000. [Google Scholar]
- Asmundson GG, Stein MB. Vagal attenuation in panic disorder: An assessment of parasympathetic nervous system function and subjective reactivity to respiratory manipulations. Psychosomatic Medicine. 1994;56:187–193. doi: 10.1097/00006842-199405000-00002. [DOI] [PubMed] [Google Scholar]
- Bernstein A, Zvolensky MJ, Feldner MT, Lewis SF, Fauber AL, Leen-Feldner EW, Vujanovic AA. Anxiety sensitivity taxon and trauma: Discriminant associations for posttraumatic stress and panic symptomatology among young adults. Depression and Anxiety. 2005;22:138–149. doi: 10.1002/da.20091. doi:10.1002/da.20091. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. doi:10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Boelen PA, Reijntjes A. Intolerance of uncertainty and social anxiety. Journal of Anxiety Disorders. 2009;23:130–135. doi: 10.1016/j.janxdis.2008.04.007. doi:10.1016/j.janxdis.2008.04.007. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller MO, Zvolensky MJ, Bernstein A. Discomfort intolerance: Evaluation of incremental validity for panic-relevant symptoms using 10% carbon dioxide-enriched air provocation. Journal of Anxiety Disorders. 2009;23:197–203. doi: 10.1016/j.janxdis.2008.06.007. doi:10.1016/j.janxdis.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Saladin ME, Drobes DJ, Brady KT, Dansky BS, Kilpatrick DG. Trauma and substance use cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug and Alcohol Dependence. 2002;65:115–127. doi: 10.1016/s0376-8716(01)00157-0. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2nd edition Erlbaum; Hillsdale, NJ: 1983. [Google Scholar]
- Daughters SB, Reynolds EK, McPherson L, Kahler CW, Danielson CK, Zvolensky M, Lejuez CW. Distress tolerance and early adolescent externalizing and internalizing symptoms: The moderating role of gender and ethnicity. Behaviour Research and Therapy. 2009;47:198–205. doi: 10.1016/j.brat.2008.12.001. doi:10.1016/j.brat.2008.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehring T, Ehlers A, Glucksman E. Do cognitive models help in predicting the severity of posttraumatic stress disorder, phobia, and depression after motor vehicle accidents? A prospective longitudinal study. Journal of Consulting and Clinical Psychology. 2008;76:219–230. doi: 10.1037/0022-006X.76.2.219. doi:10.1037/0022-006X.76.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwood LS, Hahn KS, Olatunji BO, Williams NL. Cognitive vulnerabilities to the development of PTSD: A review of four vulnerabilities and the proposal of an integrative vulnerability model. Clinical Psychology Review. 2009;29:87–100. doi: 10.1016/j.cpr.2008.10.002. doi:10.1016/j.cpr.2008.10.002. [DOI] [PubMed] [Google Scholar]
- Falsetti SA, Resnick HS. Cognitive behavioral treatment for PTSD with comorbid panic attacks. Journal of Contemporary Psychotherapy. 2000;30:163–179. doi:10.1023/A:1026522931013. [Google Scholar]
- First M, Spitzer R, Gibbon M, Williams J. Structured clinical interview for DSM-IV (nonpatient edition) Biometrics Research Department, New York State Psychiatric Institute; New York: 1995. [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341. doi: 10.1177/1073191104269954. doi:10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- Hajek P, Belcher M, Stapleton J. Breath-holding endurance as a predictor of success in smoking cessation. Addictive Behaviors. 1987;12:285–288. doi: 10.1016/0306-4603(87)90041-4. doi:10.1016/0306-4603(87)90041-4. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and meditational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Leisen M, Kaplan AS, Watson SB, Haynes SN, Owens JA, Burns K. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The traumatic life events questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. doi:10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Lang AJ, Kennedy CM, Stein MB. Anxiety sensitivity and PTSD among female victims of intimate partner violence. Depression and Anxiety. 2002;16:77–83. doi: 10.1002/da.10062. doi:10.1002/da.10062. [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Reardon LE, Babson KA, Dixon L. Anxiety sensitivity and posttraumatic stress among traumatic event-exposed youth. Behaviour Research and Therapy. 2008;46:548–556. doi: 10.1016/j.brat.2008.01.014. doi:10.1016/j.brat.2008.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lejuez CW, Kahler CW, Brown RA. A modified computer version of the paced auditory serial addition task (PASAT) as a laboratory-based stressor. The Behavior Therapist. 2003;26:290–293. doi:10.1002/da.20091. [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin. 2010;136:576–600. doi: 10.1037/a0019712. doi:10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall EC, Zvolensky MJ, Vujanovic AA, Gregor K, Gibson LE, Leyro TM. Panic reactivity to voluntary hyperventilation challenge predicts distress tolerance to bodily sensations among daily cigarette smokers. Experimental and Clinical Psychopharmacology. 2008;16:313–321. doi: 10.1037/a0012752. doi:10.1037/a0012752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall GN, Miles JV, Stewart SH. Anxiety sensitivity and PTSD symptom severity are reciprocally related: Evidence from a longitudinal study of physical trauma survivors. Journal of Abnormal Psychology. 2010;119:143–150. doi: 10.1037/a0018009. doi:10.1037/a0018009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall-Berenz EC, Vujanovic AA, Bonn-Miller MO, Bernstein A, Zvolensky MJ. Multi-method study of distress tolerance and PTSD symptom severity in a trauma-exposed community sample. Journal of Traumatic Stress. 2010;23:623–630. doi: 10.1002/jts.20568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. doi:10.1016/S0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- Monson CM, Schnurr PP, Resick PA, Friedman MJ, Young-Xu Y, Stevens SP. Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2006;74:898–907. doi: 10.1037/0022-006X.74.5.898. doi: 10.1037/0022-006X.74.5.898. [DOI] [PubMed] [Google Scholar]
- Nixon RD, Bryant RA. Peritraumatic and persistent panic attacks in acute stress disorder. Behaviour Research and Therapy. 2003;41:1237–1242. doi: 10.1016/s0005-7967(03)00150-5. doi:10.1016/S0005-7967(03)00150-5. [DOI] [PubMed] [Google Scholar]
- Peterson RA, Reiss S. Anxiety sensitivity index manual. 2nd ed. International Diagnostic Systems; Worthington, OH: 1992. [Google Scholar]
- Reiss S, Peterson RA, Gursky DM, McNally RJ. Anxiety sensitivity, anxiety frequency and the predictions of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. doi:10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Falsetti SA, Kilpatrick DG, Foy DW. Associations between panic attacks during rape assaults and follow-up PTSD or panic attack outcomes.. Presented at the 10th annual meeting of the International Society for Traumatic Stress Studies; Chicago, IL. 1994. [Google Scholar]
- Schmidt NB, Mitchell M, Keough M, Riccardi C. Anxiety and its disorders. In: Zvolensky MJ, Bernstein A, Vujanovic AA, editors. Distress tolerance: Theory, research, and clinical applications. Guilford Press; New York: 2011. pp. 105–125. [Google Scholar]
- Simpson T, Jakupcak M, Luterek JA. Fear and avoidance of internal experiences among patients with substance use disorders and PTSD: The centrality of anxiety sensitivity. Journal of Traumatic Stress. 2006;19:481–491. doi: 10.1002/jts.20128. doi:10.1002/jts.20128. [DOI] [PubMed] [Google Scholar]
- Stein MB, Simmons AN, Feinstein JS, Paulus MP. Increased amygdala and insula activation during emotion processing in anxiety-prone subjects. American Journal of Psychiatry. 2007;164:318–327. doi: 10.1176/ajp.2007.164.2.318. doi:10.1176/appi.ajp.164.2.318. [DOI] [PubMed] [Google Scholar]
- Taylor S, Koch WJ, McNally RJ. How does anxiety sensitivity vary across the anxiety disorders? Journal of Anxiety Disorders. 1992;6:249–259. doi:10.1016/0887-6185(92)90037-8. [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley D, Cardenas S. Robust dimensions of anxiety sensitivity: Development and initial validation of the anxiety sensitivity index-3. Psychological Assessment. 2007;19:176–188. doi: 10.1037/1040-3590.19.2.176. doi:10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Telch MJ, Jacquin K, Smits JJ, Powers MB. Emotional responding to hyperventilation as a predictor of agoraphobia status among individuals suffering from panic disorder. Journal of Behavior Therapy and Experimental Psychiatry. 2003;34:161–170. doi: 10.1016/s0005-7916(03)00037-5. doi:10.1016/S0005-7916(03)00037-5. [DOI] [PubMed] [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, Roemer L. A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy. 2007;38:303–313. doi: 10.1016/j.beth.2006.10.001. doi:10.1016/j.beth.2006.10.001. [DOI] [PubMed] [Google Scholar]
- Vujanovic AA, Bernstein A, Litz BT. Traumatic stress. In: Zvolensky MJ, Bernstein A, Vujanovic AA, editors. Distress tolerance: Theory, research, and clinical applications. Guilford Press; New York: 2011. pp. 126–148. [Google Scholar]
- Vujanovic AA, Bonn-Miller MO, Potter CM, Marshall-Berenz EC, Zvolensky MJ. An evaluation of the association between distress tolerance and posttraumatic stress within a trauma-exposed sample. Journal of Psychopathology and Behavioral Assessment. 2011;33:129–135. doi: 10.1007/s10862-010-9209-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vujanovic AA, Zvolensky MJ, Bernstein A. Posttraumatic stress and panic psychopathology: Clinical import, research advances, and future directions – Introduction to the special issue. Cognitive Behaviour Therapy. 2008;37:63–65. doi: 10.1080/16506070801968981. doi:10.1080/16506070801968981. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio A, Keane TM. Psychometric properties of nine scoring rules for the clinician-administered posttraumatic stress disorder scale. Psychological Assessment. 1999;11:124–133. doi:10.1037/1040-3590.11.2.124. [Google Scholar]
- Zinbarg RE, Mohlman J, Hong NN. Dimensions of anxiety sensitivity. In: Taylor S, editor. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Lawrence Erlbaum Associates Publishers; Mahwah, NJ: 1999. pp. 83–114. [Google Scholar]
- Zvolensky MJ, Vujanovic AA, Bernstein A, Leyro TM. Distress tolerance: Theory, measurement, and relations to psychopathology. Current Directions in Psychological Science. 2010;19:406–410. doi: 10.1177/0963721410388642. doi:10.1177/0963721410388642. [DOI] [PMC free article] [PubMed] [Google Scholar]